*Components of Adaptive Immunity
1/35
Earn XP
Description and Tags
5A
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
What are the key features of adaptive immunity?
ability to distinguish self from non-self
pathogen specificity — species- or strain-specific
target diversity — designed to respond to vast # of epitopes
immunological memory — specialized long-living lymphocytes will be retained for quicker, more effective future responses
When is the adaptive immune system triggered?
Triggered when innate immunity cannot fully eliminate a pathogen.
Slower initial response compared to innate immunity, but more effective in long-term protection.
What is the flow of body fluids?
circulatory system (blood)
tissue (leaky capillaries) which drain into
lymphatic system
Contrast lymphatic vessels and blood vessels
Lymphatic vessels are similar to veins and arteries, but carry lymphatic fluid (lymphocytes)
Fluid is monitored for evidence of infection before being returned to circulatory system.
What would happen if lymph fluid cannot be returned to the heart?
Swelling, particularly in the legs, as gravity pulls fluid down.
What are the primary lymphoid tissues?
Bone marrow, thymus.
→ Makes the immune cells. Immune cells produced in bone marrow,.
→ T-cells mature in the thymus. B-cells mature in the bone marrow.
What are the secondary lymphoid tissues?
Spleen, lymph nodes.
→ stores immune cells until infection
→ Mucosa-associated lymphoid tissues (MALTs) found in places vulnerable to infection
What is bone marrow’s role in immunity?
site of hematopoiesis
hematopoietic stem cells constantly produce new immune cells
body is always making new B- and T-cells
What is the spleen’s role in immunity?
filters blood, not ECF (lymph nodes filter ECF)
rich in macrophages and dendritic cells that remove pathogens and dying RBCs from bloodstream
splenomegaly — englargement of spleen during infection
What’s the term for microbes entering the bloodstream?
Bacteremia/septicemia
How does the spleen distinguish old RBCs from young RBCs?
Older RBCs are less flexible and get trapped in splenic clefts.
Macrophages also detect signs of damage on RBCs.
Antigen
A substance that is able to react with a product of the adaptive immune response (lymphcyte, antibody).
Has the potential to trigger an immune response (not all do)
Immunogen
A substance that reacts with the immune products and is able to provoke an immune response (immunogenic).
Antigenicity
The intensity of antigen binding; depends largely on the 3D structure of the molecule.
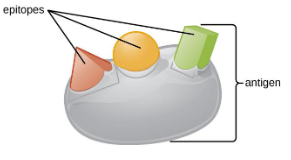
Epitope
The precise part of the molecule where the antibody or lymphocyte receptor attaches.
the 3D shape more important that the amino acid composition
antigenic determinants
Polyclonal antibodies
A single antigen may have multiple epitopes recognized by different antibodies.
Made by different populations of B-cells
Monoclonal antibodies (mAbs)
Molecular biology tools that are produced in labs
Highly specific to a single epitope; used as a therapeutic with minimal side-effects.
Haptens
Extremely small molecules that, by themselves, can bind (antigenic) but poorly trigger an immune response (immunogenic)
When fused with larger carrier complexes, immune response triggered.
Hapten-carrier complex acts as immunogen, where hapten is antigenic determinant. (allergic reactions)
What is the role of haptens in sensitization?
First exposure sensitizes immune system; hapten recognized as antigenic determinant and no longer needs carrier.
Second exposure no longer needs carrier.
→ useful in vaccines
What are downsides of haptens?
Drug allergies — drugs may fuse to larger molecules to cause immune response against them
Anemia — drugs may fuse to RBCs, marking RBCs for destruction
Thrombocytopenia — same but with platelets
Autoantigen
Defects in the generation of immune products could lead to reaction against non-foreign ‘self’ substances. Should NOT be immunogenic.
→ autoimmune diseases
Alloantigen
Target antigens from other members of the same species. Only relevant in the case of tissue transplant (blood/organ)
→ ABO/Rh blood transfusion
Heterophilic antigen
Similar or identical antigens on unrelated organisms can cause abnormal immune function.
→ M protein used to identify Streptococcus is also in heart tissue
Self antigen
During development, lymphocytes are tested for their responsiveness to ‘self antigen’
→ autoreactive lymphocytes are eliminated; self-reactive lymphocytes destroyed
Self antigen is mostly non-immunogenic
How are adaptive immune responses triggered?
Antigen presenting cells (APCs) display potential antigen molecules on their surface to assist in this initiation.
→ macrophages, dendritic cells, B-cells
Human Leukocyte Antigens (HLAs)
aka Major Histocompatibility Complex (MHC)
Cell surface proteins with a role in the adaptive immune system; survey and display antigens to T-cells.
Help distinguish between ‘self’ and ‘non-self’
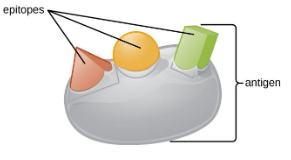
MHC-I
Location: in all nucleated cells
Presents to: cytotoxic T-cells
Shows: antigens from proteins within cell
MHC-II
Location: only on professional APCs (macrophages, DCs, B-cells)
Presents to: helper T-cells
Shows: antigens from the environment (products of phagocytosis)
Describe the structure of MHC-I
Heterodimer made of heavy α-chain and smaller β-microglobulin.
Heavy α-chain has 3 domains α1, α2, α3 (encoded by HLA-A, HLA-B HLA-C)
Peptide binding groove = 3 α domains + β domain
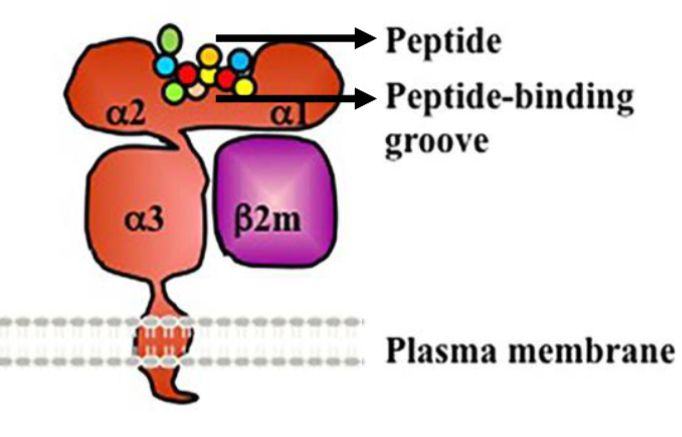
Describe the structure of MHC-II
Heterodimer made of 2 chains: α-chain + β-chain
Encoded by HLA-DP, HLA-DQ, HLA-DR (each with α + β genes)
What is the clinical significance of HLA codominance?
HLA matching is necessary for organs transplants
Parents unlikely to have same haplotypes as one another or child
Identical twins have same HLA haplotypes
Most transplants from unrelated donors, needs immunosupressants to prevent rejections
→better HLA typing = less rejection
Haplotypes
The complete SET of HLA alleles on one chromosome — inherited codominantly from parent.
Isotypes
Each MHC has 3 isotype — the different GENES themselves
MHC-I: HLA-A, HLA-B, HLA-C
MHC-II: HLA-DP, HLA-DQ, HLA-DR
Allotypes
The specific VARIANT (allele) of each gene — what makes each persons HLA unique
HLA-A2
HLA-A24
HLA-A17
Polymorphism
HLA genes are polymorphic — have many versions (alleles) of the each gene within a population.
→ structure of peptide-binding grooves of HLA-I and II will vary greatly among individuals
→ acts as molecular barcode to distinguish individuals
Why do we need such wide variety in MHC complexes?
To be able to respond to a wide variety of pathogens.