unit 3 lymph, immune, resp syst
1/58
Earn XP
Description and Tags
what universe are we in
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
main fxns of lymph syst
return interstitial fluid and leaked plasma proteins back to blood
assists in circulating body fluids (pick up extra fluid)
helps defend body against disease-causing agents
transport dietary lipids and lipid soluble vitamins (A,D,E,K, in GI-tract
lymph
interstitial fluid once entered lymphatic vessels
24 L filtered out of vlood a day; 20.4 L returned to blood; 2.6 L back to lymph vessels
mention fxn of lymph nodes
filtration - macrophages destroy microorganisms and debris
immune syst activation - monitor for antigens and mount an attack against them
*medulla- medullary chords extend from cortex and contain B, T, and plasma cells; macrophages reside on these fibers and phagocytize foreign matter
fxn of thymus
fxns strictly in T lymphocyte maturation
does not directly fight antigens
produces hormones
secretes the hormones (thymopoietin and thymosins) that stim lymphocytes to become immunocompetent
fxn of spleen
site of lymphocyte proliferation
immune surveillance and response
cleanses the blood - macrophages in sinuses remove debris and foreign matter
stores breakdown produces of RBCs for later reuse - spleen macrophages salvage and store iron for later use by bone marrow
site of fetal erythrocyte production (normally ceases after birth)
stores blood platelets
______ are specialized lymphatic capillaries found in the small intestine that pick up digested fats/lipids + assist in transporting chyle (lipids + lymph mixed together) to the bloodstream
lacteals
contrast blood capillaries w lymph capillaries
lymph: mini valves (loosely joined), start at tissue (endothelial); v permiable; withstand interstitial pressure + remain open (thanks to collagen filaments)
can absorb cell debris, pathogens, cancer cells, cells in LN cleanse + “examine” debris
what makes up lymph
interstitial fluid + leaked proteins
name the two lymph ducts and area of the body they drain
thoracic duct: rest of body, L side head, neck, chest and rest of body below diaphragm
R lymphatic duct: R arm, right side of head + neck, R chest
between which veins is lymph drained
R subclavian (?), R internal jugular (might be L, not confident)
what makes thymus diff from all other lymph organs and tissues
prod homrones, no B cells present, fxns strictly in T lymphocyte maturation
what is MALT? give examples of locations
mucosa associated lymphatic tissue: anywhere in mucosa - GI tract, resp syst, urinary,
masses of lymph tissue not surrounded by capsule; protects from foreign matter
what tissues are involved in prod memory
MALT, peyer’s patches, tonsils, appendix, thymus (did i miss any)
what are the two arms of the immune response
innate - 1st: epithelial barriers (skin, mucous mm), 2nd: protections against pathogens that break those external barriers
adaptive - 3rd: grp of mechanisms defeat pathogen + create “memory” for future encounters
what distinguishes innate def from adaptive def syst?
innate - not specific, localized → if cut on arm, that’s where innate response
adaptive - specific, systemic, memory
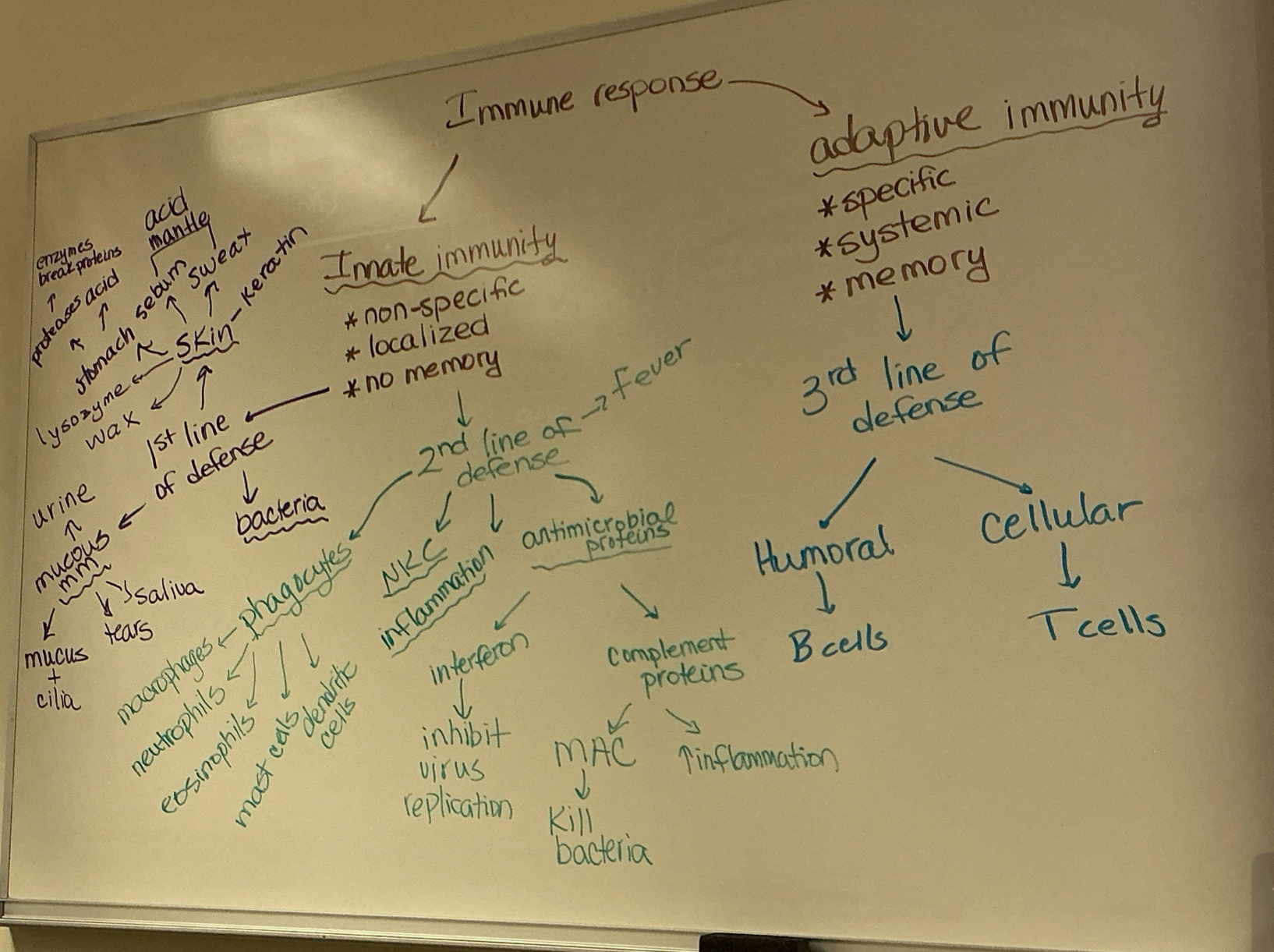
explain 1st line defense weapon fxns
skin - wax, lysozyme, keratin, sebum + sweat (acid mantle), stomach → proteases, acid; enzymes break proteins
mucous mm - urine, mucous + cilia, tears, saliva
bacteria - your natural microbiome
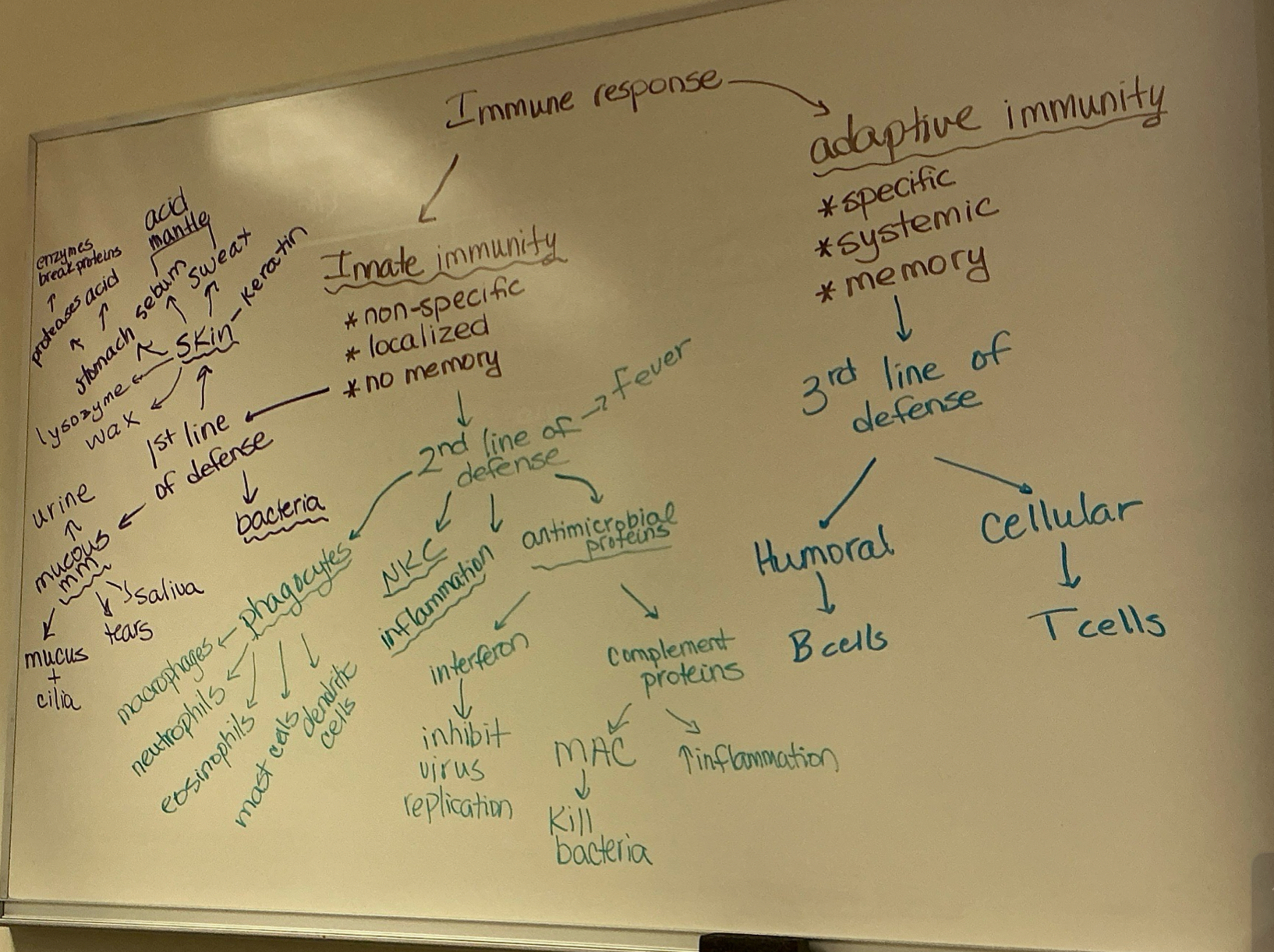
explain 2nd line defense weapon fxns
phagocytes - macrophages, neutrophils, eosinophils, mast cells, dendritic cells
antimicrobial proteins - interferon → inhibit virus replication; complement proteins → MAC: kill bacteria, inflamm
NKC inflamm - small disctinct grp of large granular lymphocytes; react nonspecifically and eliminate cancerous + virus-infected cells; kill targets by releasing perforins and other cytolytic chems; can lyse and kill cancer cells + virus-infected cells by puncturing their mm
fever
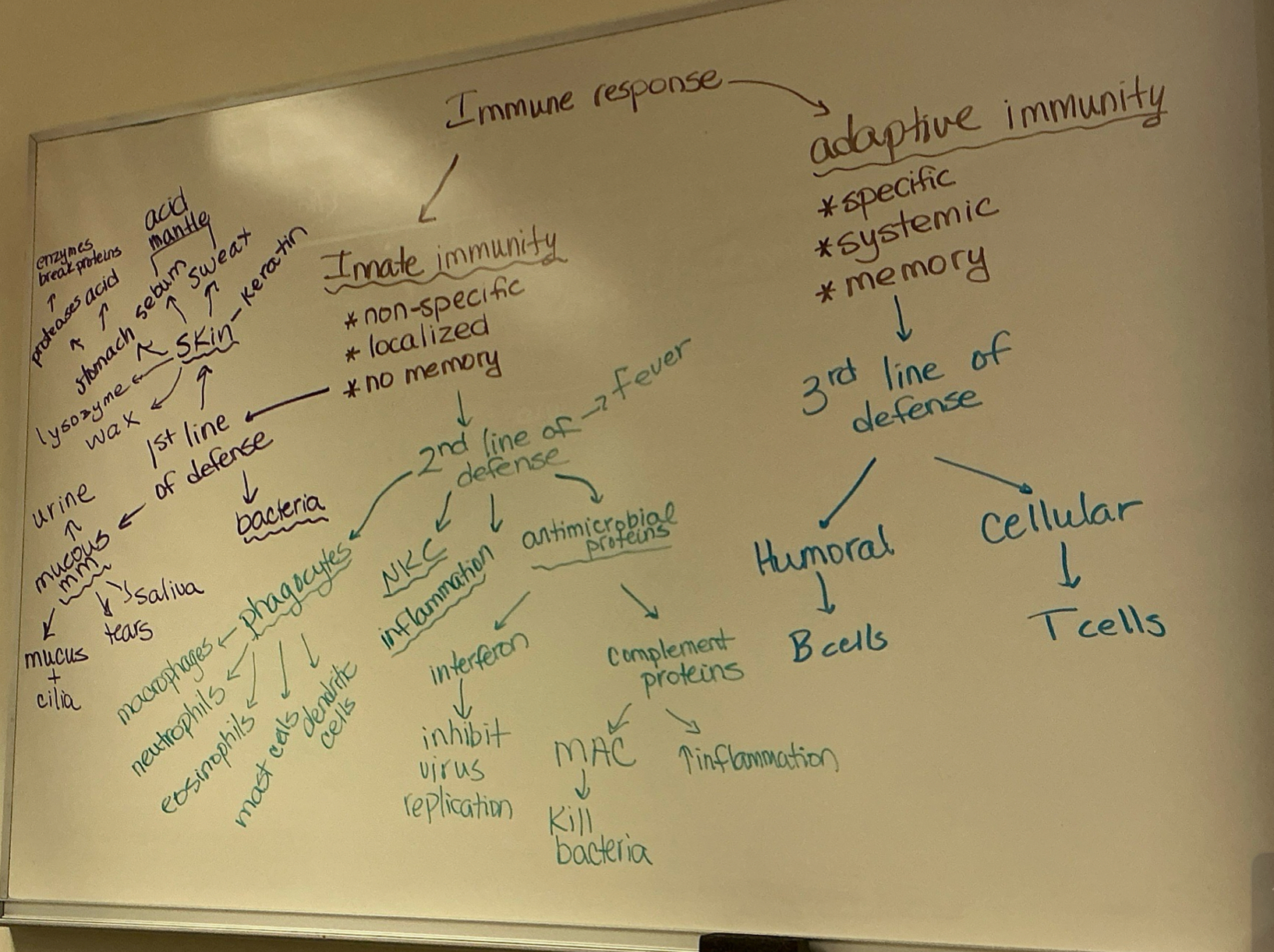
explain 3rd line defense weapon fxns
humoral → antibody-mediated immunity; works mainly against extracellular stages of infectious microorgs; extracell viruses, bacteria, yeast, allergens, toxins, venoms. in event of mismatched blood transfusion, also destroys foreign erythrocytes - B cells prod antibodies to neutralize pathogens
cellular → T cells - directly kill infected/cancerous cells/help coordinate immune response
there are two important antimicrobial proteins:
complements and interferons
what are complement proteins? how does it cause bacterial lysis? what are some of the compliment proteins
amplifies inflamm response, kills bact + destroys foreign substances, circulate in blood in inactive form
causes bact lysis by MAC (membrane attach complex) - MAC inserts into mm of cells and allows ions, water, other molecules to freely pass thru pores
some are C1, C2, C3 (a+b), C4, C5 (a+b), C6, C7, C8, C9
what stims interferon prod, and how they protect uninfected cells
viral infection stims interferon prod (before specific immune syst)
interferons activate macrophages and mobilize NKs (to inhibit virus prod), so
protect by making other cells protect themselves - inter molecules leave infected cell and enter neighbor cells, then stims neighbor cells to activate genes for PKR (antiviral protein), which specifically blocks viral repro in neighboring cells
know steps, fxns, and underlying mechanism of inflamm response
steps: mast cells detect injury to nearby cells + release histamine, initiating inflamm response; histamine increases blood flow to wound sites, bringing in phagocytes and other immune cells that neutralize pathogens. the blood influx causes the wound to swell, redden, and become warm and painful
fxns: prevent spread of damaging agents to nearby tissues, dispose of cell debris + pathogens, set stage for repair processes
mechanism: (? is this not the same as steps? kinda? idrk) stop pathogens from spreading, bring immune cells to location
cardinal signs of inflamm
redness, swelling, pain, heat
what is an antigen? compare and contrast complete and incomplete antigens (haptens)
antigens - illicit immune response; only certain parts of entire antigen are immunogenic (epitopes -specific part of antigen recognized by immune syst)
complete antigens - large (proteins, some lipids, nucleic acid), ultimate targets of immune response; B cells
incomplete antigens (haptens) - small molecules (peptides, nucleotides, many hormones); not immunogenic but reactive when attached to protein carriers (don’t illicit immune responded by themself. bind to protein to become complete and illicit immune response
antigen-presenting cells did i give enough info?
do not respond to specific antigens; play essential auxiliary (supportive) roles in immunity
major role in immunity is to engulf foreign particles and present fragments of antigens on their own surfaces to be recognized by T cells
dendritic cells (usually in CT and epiderm) - major initiator of adaptive immunity; migrate to LN and 2ry lymphoid organs, and present antigens to T and B cells
macrophages - stay at site of infection; similar to dendritic, also secrete soluble proteins that activate T cells
lymphocytes, B cells

what does it mean when a T or B cell becomes immunicompetent
means cells have receptor - can bind to other cells (display unique type of receptor that responds to distinct antigen)
B cells can prod antibodies by binding to antigens (substances that trigger immune response, prompting prod of antibodies)
B cells mature in bone marrow; T cells mature in thymus
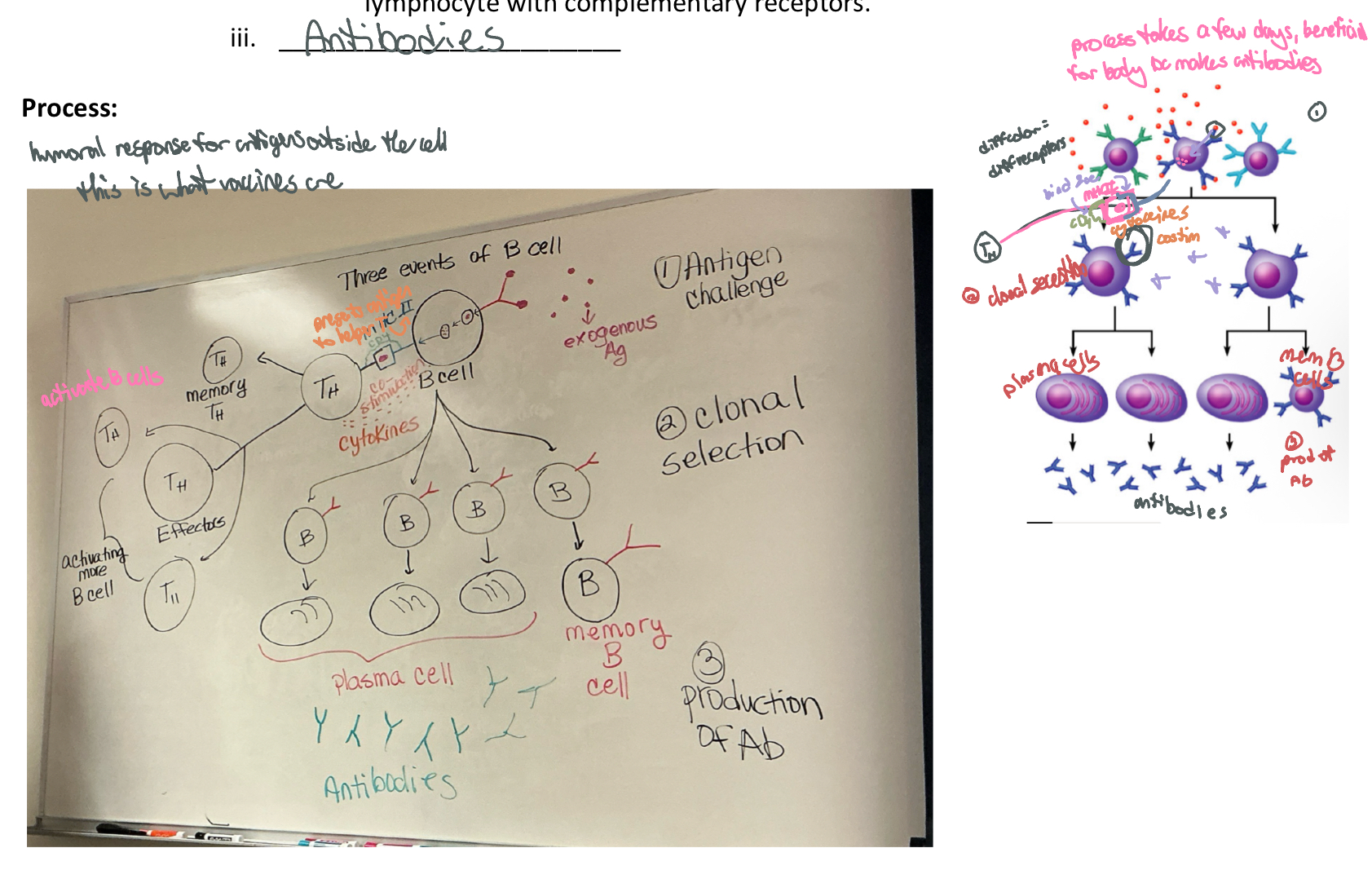
what happens to B cells when activated for the first time? explain clonal selection
when b cell activated, clonal selection begins
a native immunocompetent B cells is activated when antigens bind to its surface receptors and T cell interactions; B cells quickly stimulated then multiply
result is army of cells (all exactly alike) bearing the same antigen-specific receptors; it is the antigen that does the selecting in clonal selection by “choosing” a lymphocyte with complementary receptors
(b cells witness crime (attack), show police sketch of criminal, tell others abt it)
what determines our specificity towards a foreign substance
our genes
why is the secondary response to an antigen so much faster than the primary response
because memory cells generated during the initial exposure to an antigen are ready to react much faster in later encounters
compare and contrast humoral and cellular immunity. Make sure yk when each one is used
humoral: involves B cells + antibodies, deals w exogenous (originating from externals), relies on these to neutralize pathogens in bodily fluids (pleural+peritoneal cavities, after birth)
cellular: cytotoxic T cells fight specific antigen directly; bind to target cell and release perforins into its mm causing cell lysis by creating transmembrane pores, endogenous antigens; attakcs any of our cells infected w virus, parasite, cancer
class II MHC proteins display what kind of antigens? what class of T cell recognizes antigens bound to class II MHC? what types of cells display these proteins?
bind complete antigens to exogenous antigens
CD4 (helper T cells [TH])
antigen-presenting cells (APCs)
contrast active and passive immunity. be able to mention examples
active: make memory+plasma cells → natural - antibodies made after infection; artificial - ab after vaccine
passive: given, not prod by self; go away if given → natural - ab from mother’s milk; artificial - ab from serum shot of antibody itself (ex. IgG, snake venom)
what are the general functions of antibodies
ammunition of humoral imm; capable of binding specifically w certain antigen
“tie up prisoner” until help arrives
Neutralization, Agglutination, Precipitation, Complement, Opsonization (foreign patho coated w opsonins, making susceptible to phagcyto by imm cells), NK cells
a NAP can help you CONcentrate
specific fxn IgM
main antibody of primary responses (first secreted in response to new antigen), best at fixing complement; monomer form of IgM serves as B cell receptor
doesn’t cross placenta
specific fxn IgG
main blood antibody of 2ry responses, neutralizes toxins, opsonization
crosses placenta
specific fxn IgA
secreted into mucus, tears, saliva, colostrum
doesn’t cross placenta
specific fxn IgE
antibody of allergy (histamine) and antiparasitic activity
doesn’t cross placenta
specific fxn IgD
B cell receptor
doesn’t cross placenta
which class of antibody is most abundant in blood? which is secreted first in a primary immune response? which is most abundant in secretion?
IgG, IgM, IgA
what makes up the respiratory and conductive zones of the resp syst
resp: resp bronchi, alveolar ducts, alveoli
conductive: nose, nasal cavity, nasopharynx, larynx, trachea, bronchi, bronchioles
know all fxns of resp syst
exchange CO2 + O2, speech and other vocalizations, sense of smell, influences pH of body fluids by eliminating CO2 (acid-base balance)
BP reg by helping synthesis of angiotensin II (→vasoconstrictor→ADH+aldosterone→inc BP), blood+lymph flow, lungs filter small clots (blood filtration), expulsion of abdominal contents: breath-holding assists in urination, defecation, childbirth (valsalva maneuver)
contrast internal resp, external resp, pulmo ventilation. what is the goal of all 3?
internal - systematic gas exchange (between blood + cells)
external - alveolar gas exchange
pulmo vent - breathing, quiet breathing (at rest, rhythmic); inspiration+expiration; change in vol causes gas pressure changes in thoracic cavity. change in vol causes gas pressure changes in thoracic cavity (do we need to know these details)
be able to answer questions on anat and/or fxns (including types of cells, structure, such as cartilage/smooth musc presence) of all resp structures (from nasal cavity to alveoli)
table in canvas
why pseudostratified ciliated columnar epithelium is common in many resp structures?
has goblet cells that prod mucus to catch bacteria, dust, etc
cilia remove intrusions (idk lol)
which resp structure provides the greatest surface area for gas exchange?
alveolus(i)
what cells would you find in an alveoli and what is the fxn for each cell?
type I - simp squam epi - gas exchange
type II - secrete surfactant (dec surface tension of water in alveoli, keeps open w o collapse)
macrophages - eat bact
simp squam epi - gas exchange
discuss relationship of pleurae to the lungs and thoracic wall, and their fxnal importance
pleurae surround lungs, w visceral layer touching lungs and parietal layer touching thoracic wall
fxnal importance - keep lungs inflated bc pressure
how does alveoli’s surfactant prevent the collapsing of alveoli?
dec surface tension of water
know what steps, muscs, events (such as pressure differences) are involved in breathing:
define intrapulmonary and intrapleural pressure
intrapulmonary - pressure in lungs (alveoli)
intrapleural - pressure between visceral and parietal pleura (pressure around lungs)
know what steps, muscs, events (such as pressure differences) are involved in breathing:
the contraction of the diaphragm and the external intercostals begins inspiration. which nerves are involved in the contraction of these muscles? explain what happens in terms of volume and pressure changes in the lungs when these muscs contract. make sure to include movement of air and pressure diffs inside lungs and pleural pressure. then explain what happens during expiration
diaphragm nerve - phrenic (diaphragm down/flat)
external intercostal nerve - intercostals nerve
volume - 500mL air - tidal volume; vol up, pressure down
pressure - pressure in lungs less than pressure in atmosphere (760mmHg)
movement of air - air in alveoli
pressure diffs in lungs + pleural pressure - intrapulm(in alveoli) begins 760, interpleural is 756. when diaphragm and ext intcosts contract, vol inc intrapulm pressure down to 759 and intrapleural down 754.
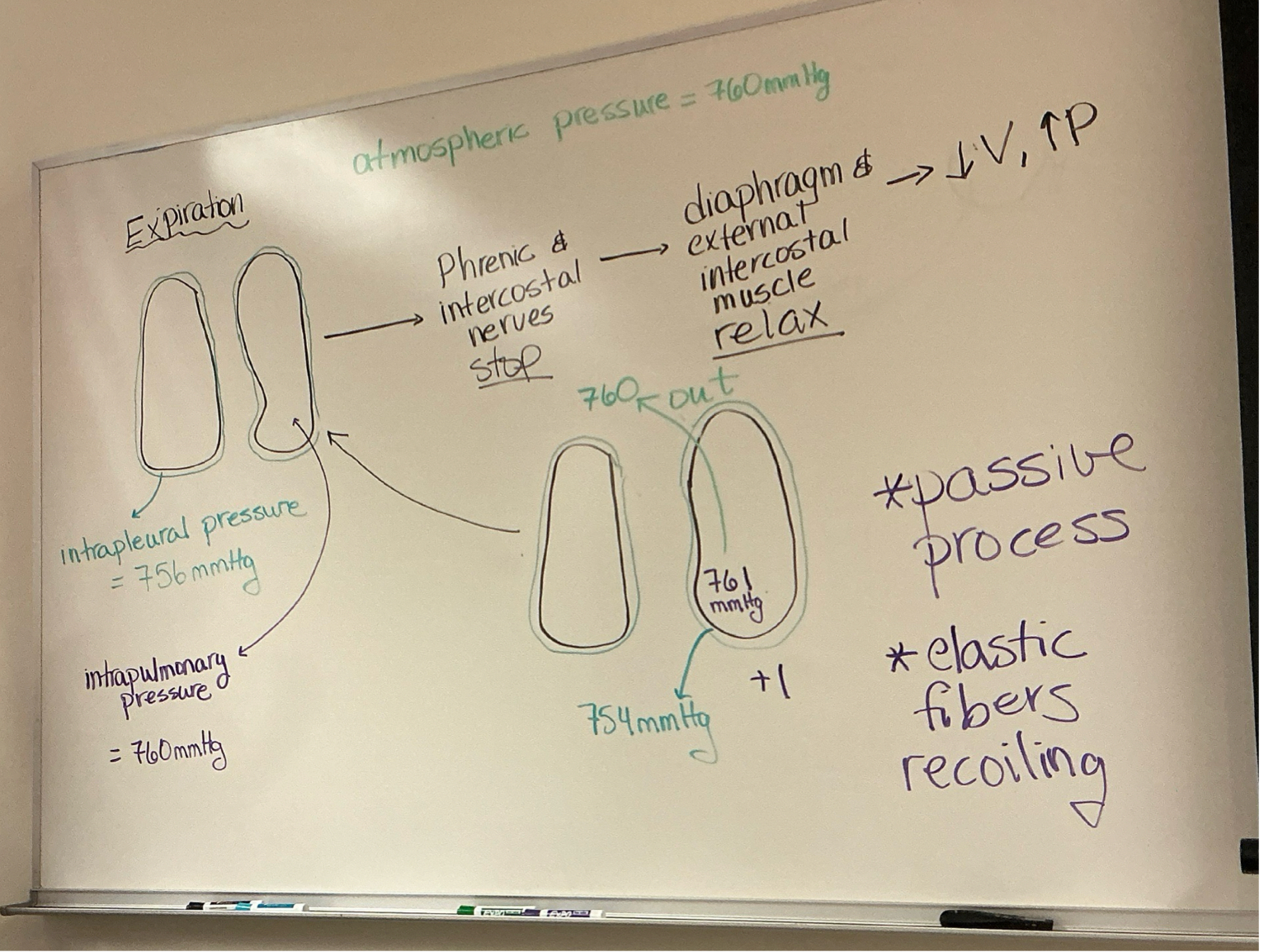
explain what happens during expiration. explain what happens in terms of volume and pressure changes in the lungs when diaphragm and external intercostal muscs contract. make sure to include movement of air and pressure diffs inside lungs and pleural pressure.
volume - 500mL
pressure - vol down, pressure up
movement of air - air moves our alveoli
pressure diffs in lungs + pleural pressure - intrapulm pressure beginning at 760 and interpleural at 754. diaphragm + ect intcosts relax, vol dec intrapulm pressure inc to 761 and intrapleural back to 756
know what steps, muscs, events (such as pressure differences) are involved in breathing:
on the other hand, if you have to force your breathing in what muscs would be involved?
sternocleidomastoid - elevate sternum
scalene - elevating 2 upper ribs
pectoral minor - elevate 3-5 ribs
serratus posterior - ribs 2-5
erector spinae - straighten vertebral column
know what steps, muscs, events (such as pressure differences) are involved in breathing:
on the other hand, if you have to force your breathing out what muscs would be involved?
internal intercostals - depress the ribs
abdominal wall muscles - move abdominal content upward to push diaphragm upward
transversus thoracis - ribs 2-6
serratus posterior inferior - ribs 9-12
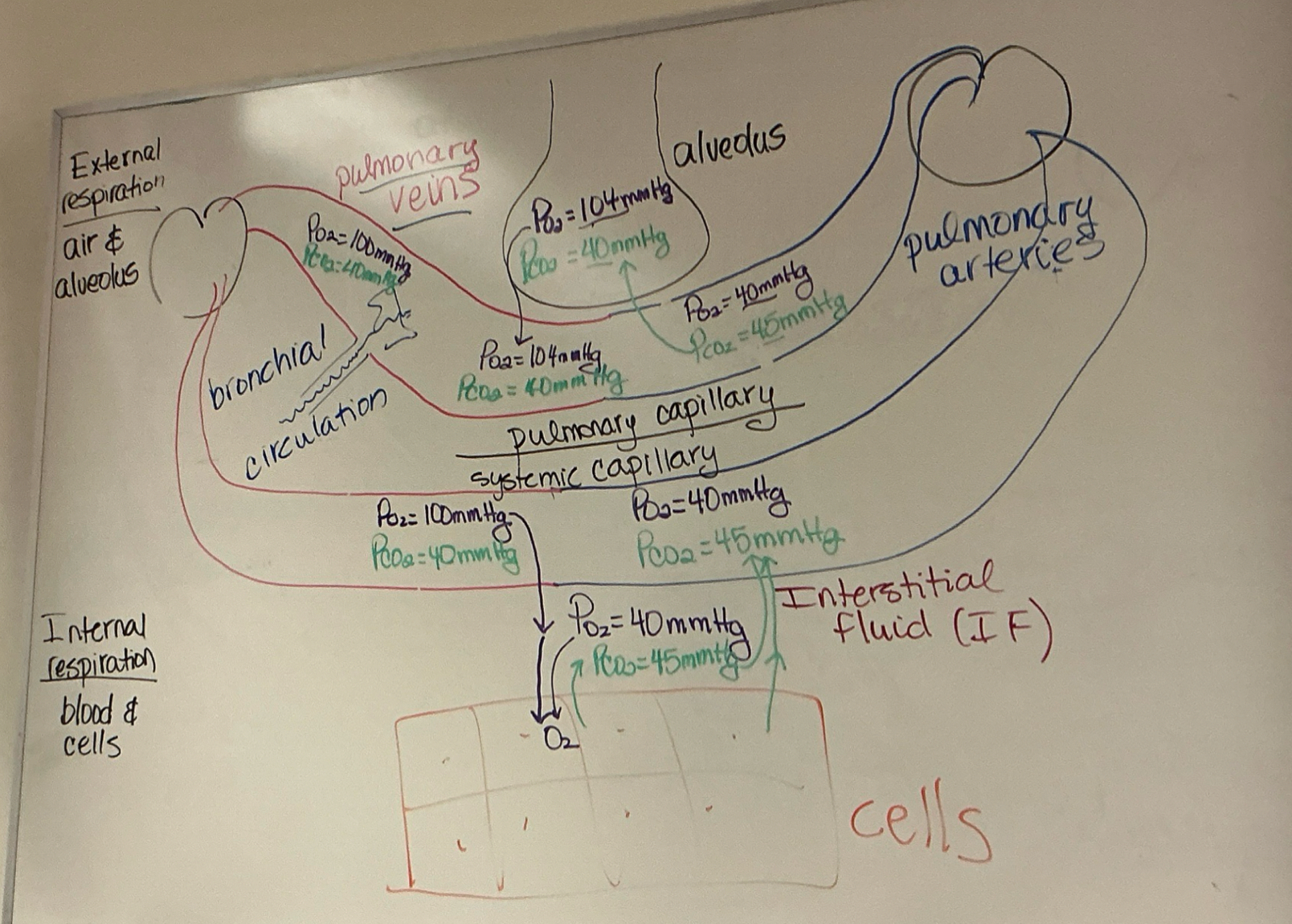
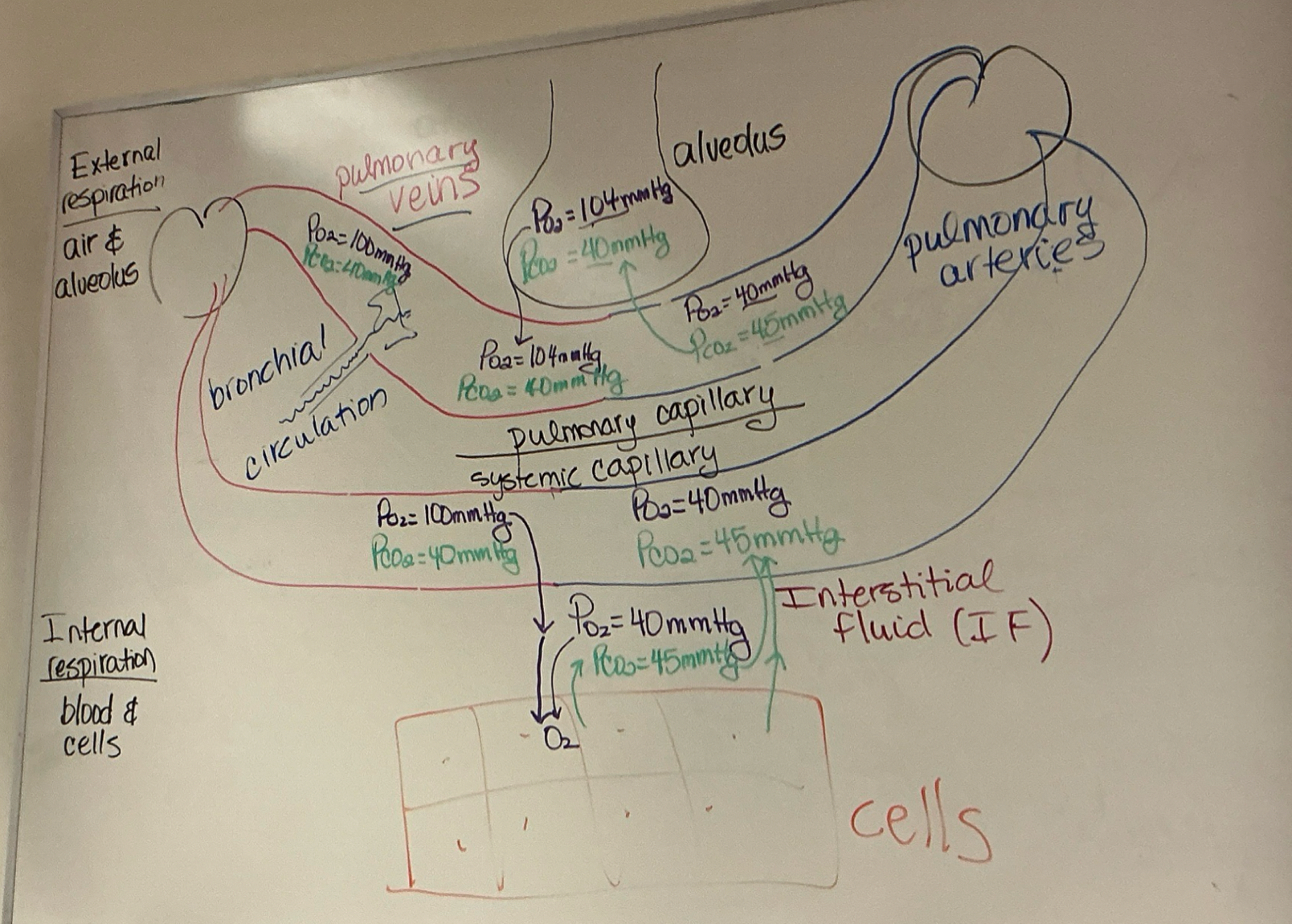
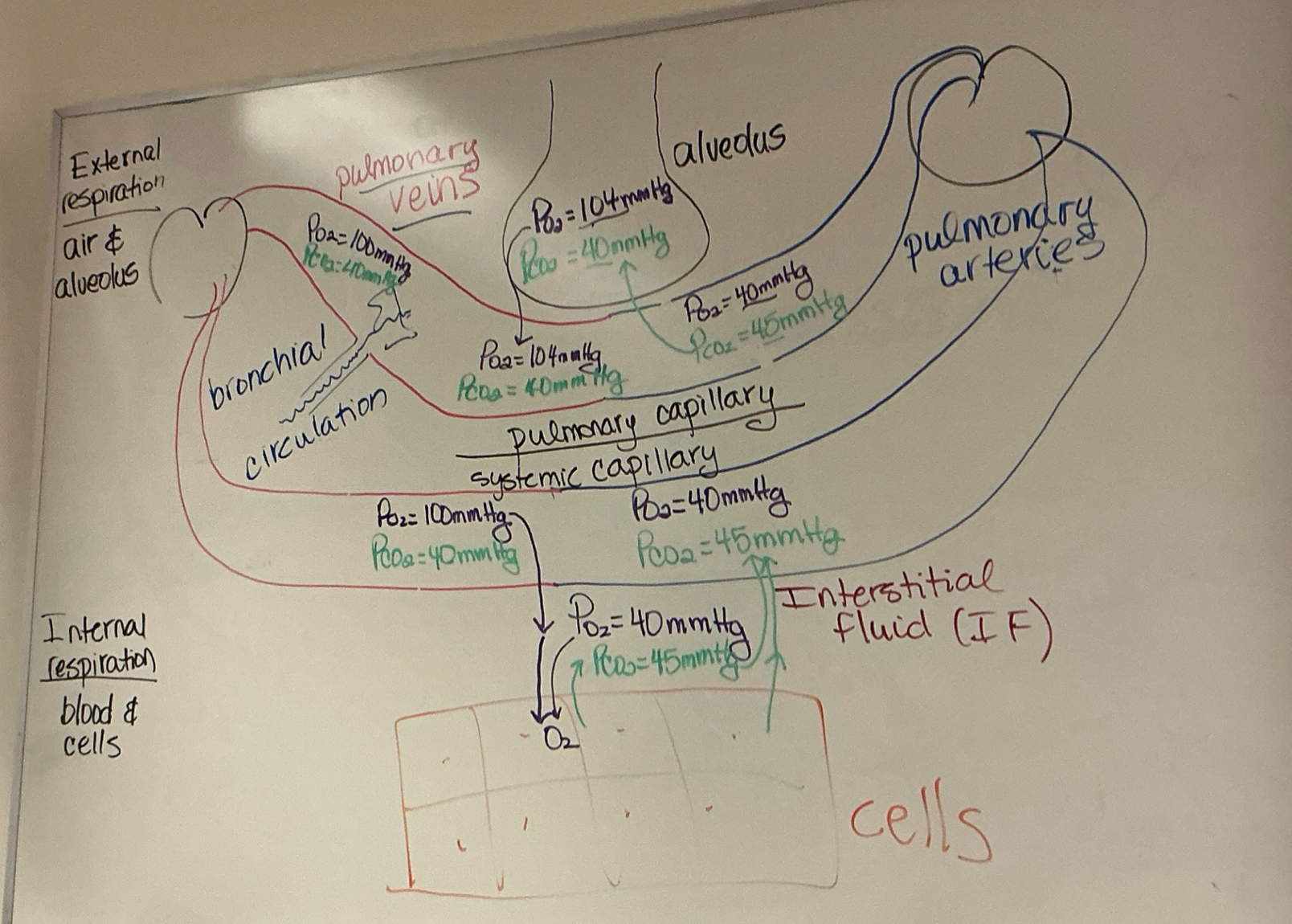
during external resp, where are oxy and CO2 concentrations higher? what drives O2 and CO2 to move from one region to another? dont forget abt mmHg for CO2 and O2
PO2 higher in alveolus until bv pass alveolus, PCO2 higher in bvs until pass alveolus
partial pressure gradient (?) drives O2 and CO2 to move from one region to another
part 1 [deoxy from arteries]: pulmo caps - PO2 = 40mmHg, PCO2 = 45mmHg
part 2: alveolus - PO2 = 104mmHg, PCO2 = 40mmHg → pulmo caps- PO2 = 104mmHg, PCO2 = 40mmHg
part 3 [reoxy in veins]: (bronchial circulation) pulmo caps- PO2 = 100mmHg, PCO2 = 40mmHg
during internal resp, where are oxy and CO2 concentrations higher? what drives O2 and CO2 to move from one region to another? dont forget abt mmHg for CO2 and O2
PO2 higher in bv until pass to cells, PCO2 higher in cells until passed to bvs
pt 1: systemic caps - PO2 = 100mmHg, PCO2 = 40mmHg
pt 2: cells (maybe? i think?) - PO2 = 40mmHg, PCO2 = 45mmHg
pt 3: systemic caps - PO2 = 40mmHg, PCO2 = 45mmHg
know everything abt O2 and CO2 transport. include: where in blood they are transported
hemoglobin
know everything abt O2 and CO2 transport. include: how its transport is affected by factors such as temp, acidity and BPG, etc…
saturation - the higher the PO2 difference, the higher the oxygen dissociation
temp - the higher it is, the higher the oxy dissociation
pH (high H+) - the lower it is, the higher the oxygen dissociation (exercise = lactic acid = lower pH = higher O2 dissociation
PCO2 - inc CO2, inc O2 unloading
BPG - higher BPG, higher oxy dissociation
know diff resp ctrls (resp ctrl center [VRG and DRG] and PRG)
medullary resp centers:
ventral respiratory grp (VRG) - ctrls auto resp; primary generator of resp rhythm; generates gasping during extremely low oxy
dorsal resp syst (DRG) - one of the mechanisms that modifies basic resp rhythm; drg issues output to vrg that modifies resp rhythm to adapt to varying conditions
pons:
pontine resp center - receives input from higher brain centers including hypothalamus, limbic syst, cerebral cortex, and issues output to both DRG and VRG; adapts breathing to special circumstances such as sleep, exercise, vocalization, emotional responses (laugh, cry)
mention diff reasons that could change our breathing pattern and their effect on breathing depth/rate
cerebral cortex - hold breath
hypothalamus + limbic syst - allow emo stim to alter resp, like anticipation of activity/emotional anxiety
central chemoreceptors - PaCO2; medulla oblongata
peripheral chemoreceptors - PaO2 and blood pH; carotid, aortic arch
O2 - must go under 60mmHg in arteries to become major stimulus for increased ventilation
inflation reflex - stretch receptors in walls of bronchi and bronchioles
proprioceptor stim - monitor movement of joints and muscles
temp - inc in temp from fever/exercise inc resp rate
pain - inc in resp rate
airway irritation - ceaces resp followed by coughing/sneezing