Huerta Exam 2 Study Materials on Rheumatic Diseases (Osteoarthritis and Rheumatoid Arthritis)
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
rheumatoid diseases are most commonly referred to as
arthritis
50 mins
arthritis
inflammation of a joint
arthritis is characterized by
- chronic pain
- progressive physical impairment
- affects joints, skin, muscles, ligaments, and/or tendons
arthritis is among the leading causes of
disability
rheumatic diseases
▪Osteoarthritis (OA)
▪Rheumatoid arthritis (RA)
▪Lupus
▪Ankylosing spondylitis
▪Scleroderma
▪Gout
▪Fibromyalgia
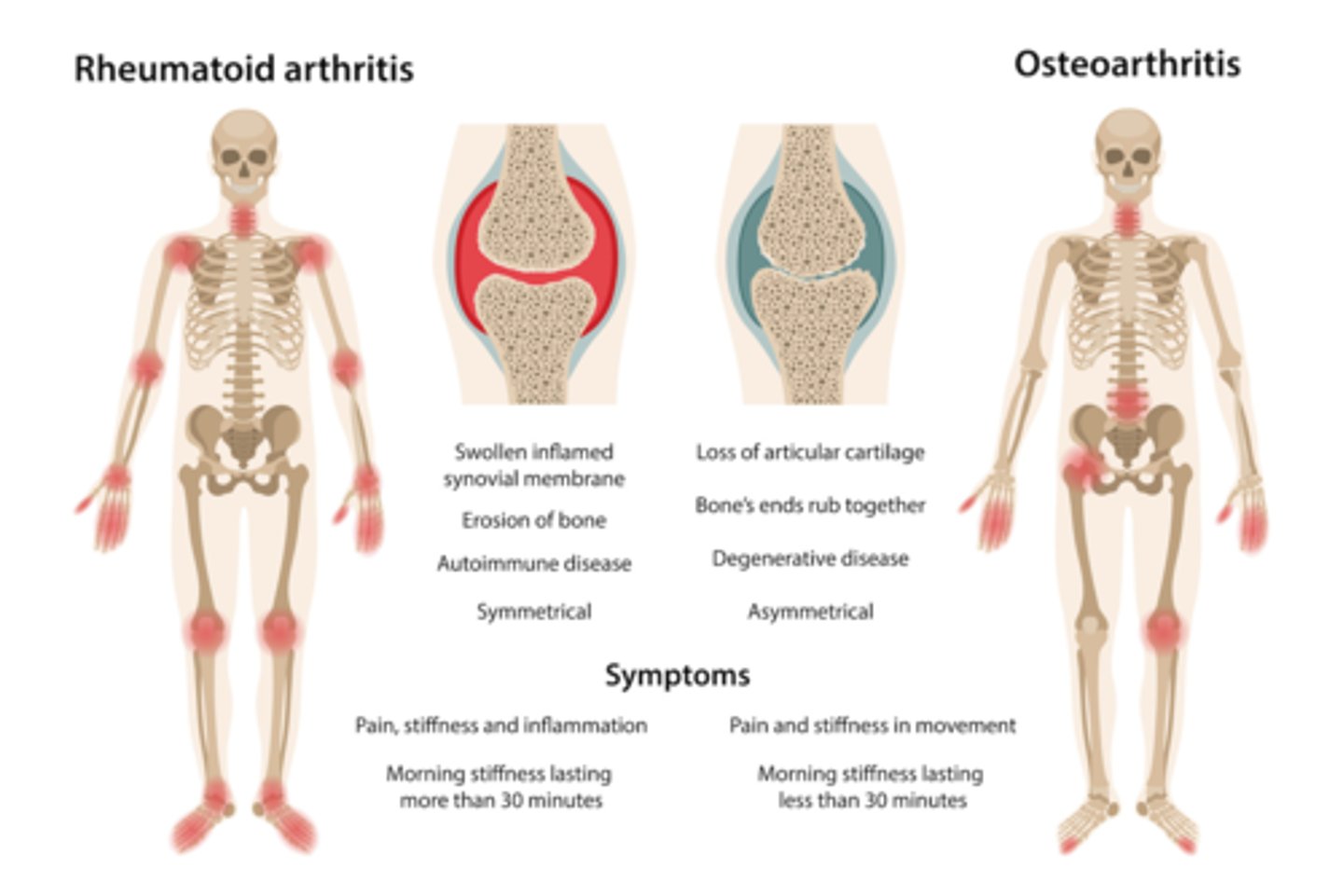
Common wear and tear joint disorder
osteoarthritis - OA
OA is most common in what gender
females
OA risk increases with
age
earlier onset
a) OA
b) RA
RA
develops suddenly or within weeks or months
a) OA
b) RA
RA
many joints affected, including wrists, elbows, and shoulders, mainly smaller joints on both sides of the body
a) OA
b) RA
RA
warmth, swelling, and joint redness are common
a) OA
b) RA
RA
morning stiffness lasts longer
a) OA
b) RA
RA
systemic symptoms present
a) OA
b) RA
RA
individual joints
a) OA
b) RA
OA
non-inflammatory
a) OA
b) RA
OA
body attacking its own structures
a) OA
b) RA
RA
most common
a) OA
b) RA
OA
incidence increases with age
a) OA
b) RA
OA
use heat to tx
a) OA
b) RA
OA - because there is no inflammation
inflammatory disease
a) OA
b) RA
RA
very common in 40-60 year old females
a) OA
b) RA
RA
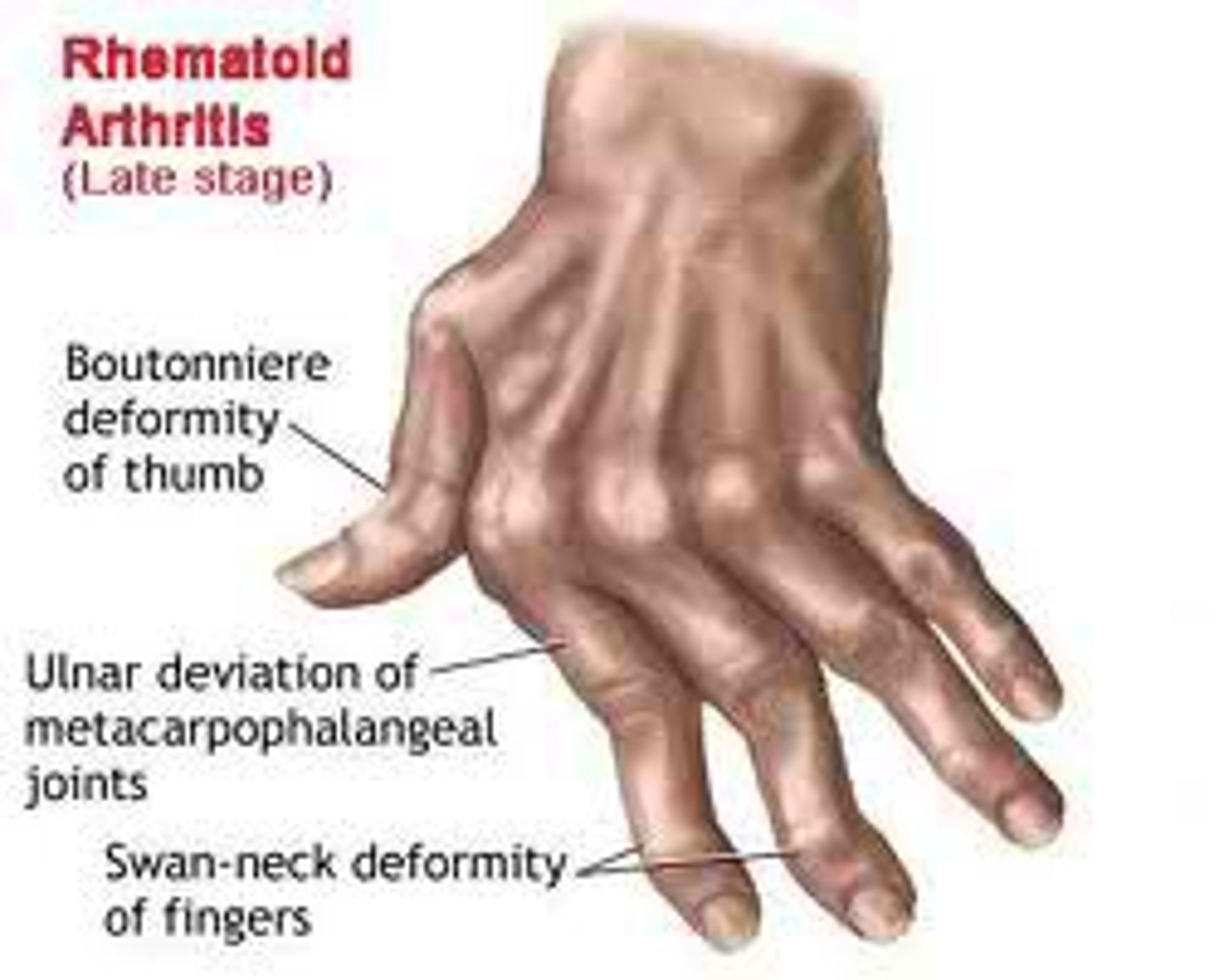
ulnar deviation is most common in
a) OA
b) RA
RA
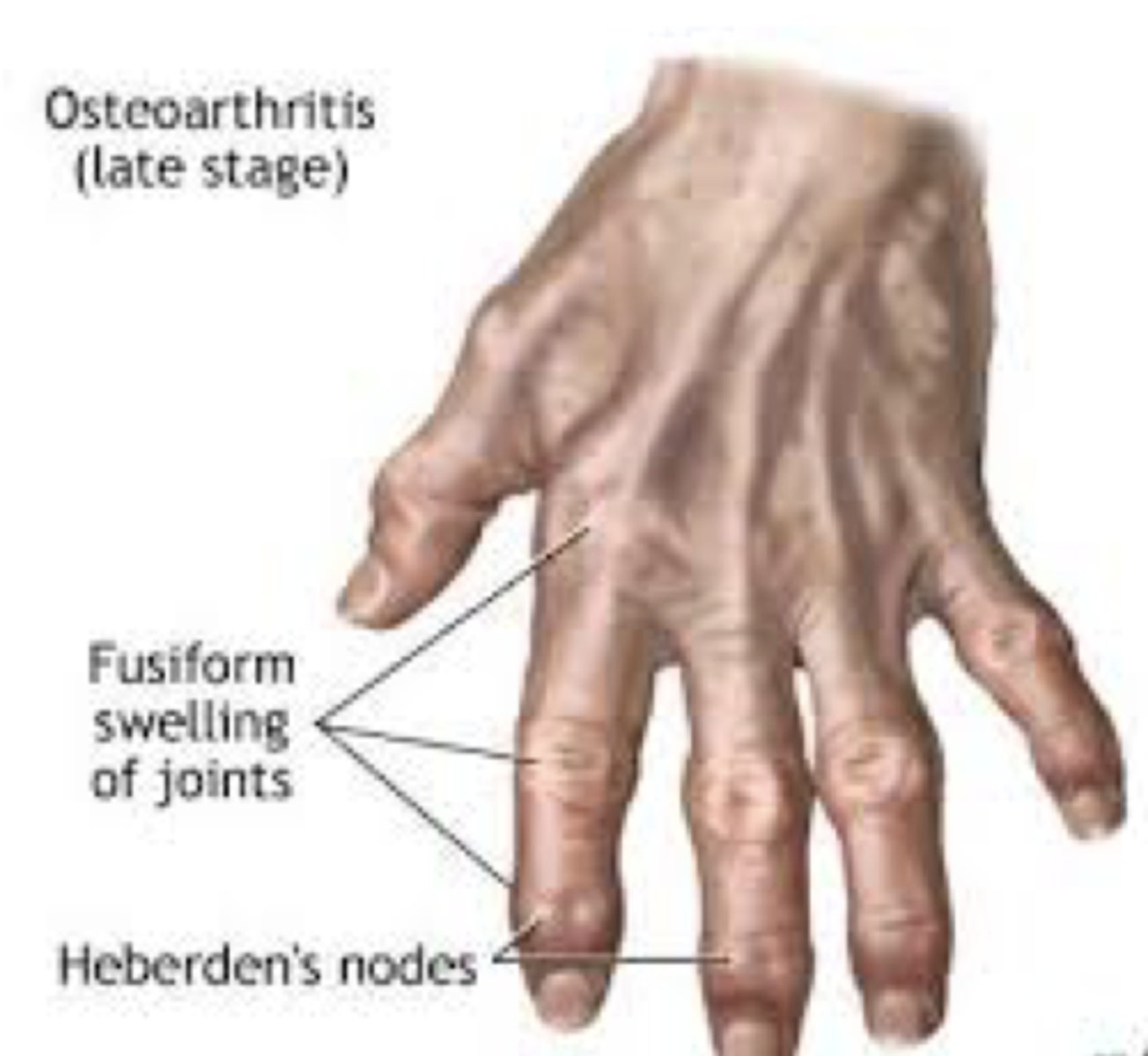
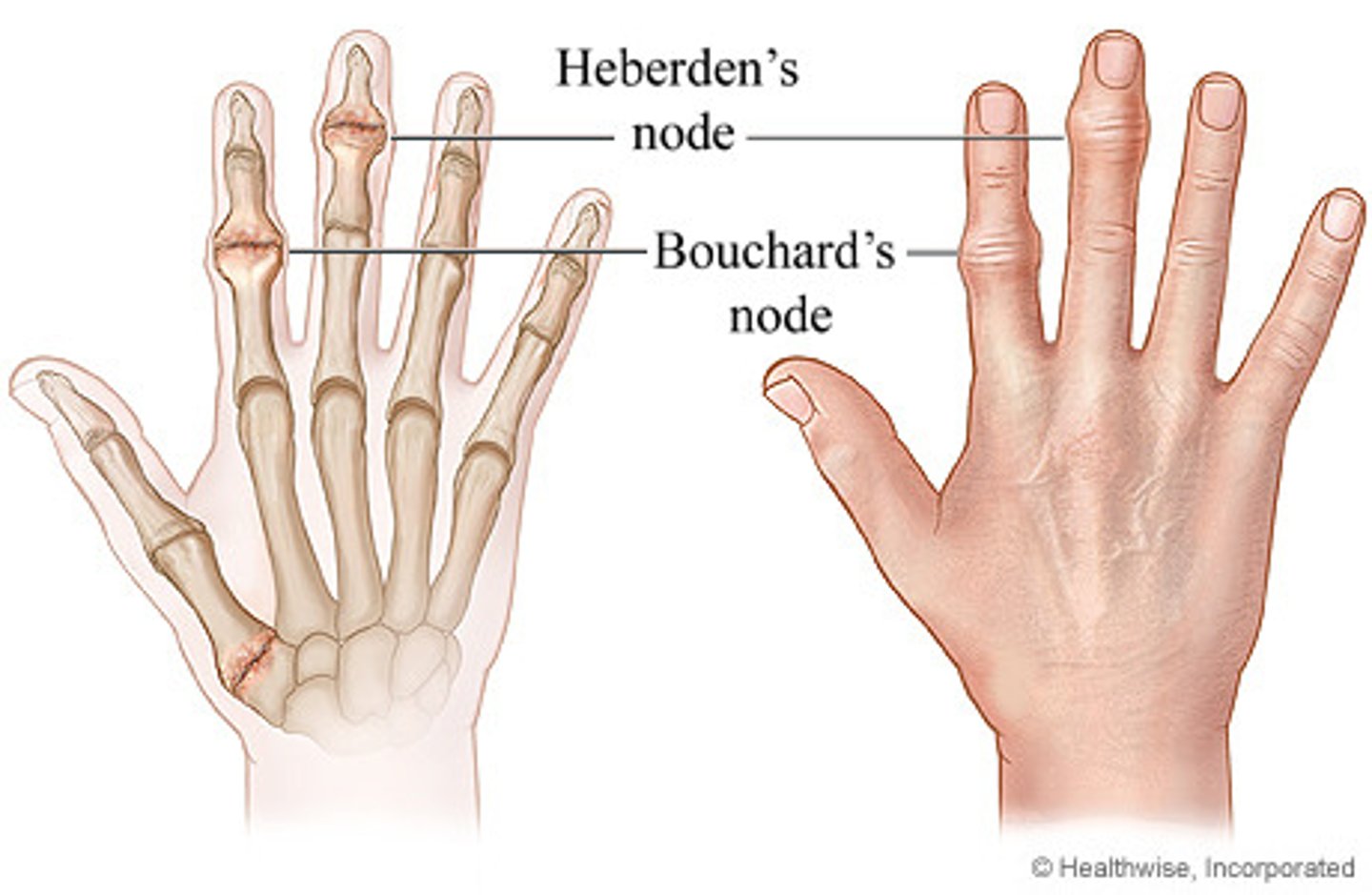
fusiform swelling of joints and heberden's nodes are most common in
a) OA
b) RA
OA
most common type of degenerative joint disease
a) OA
b) RA
OA
strongly correlated with age
a) OA
b) RA
OA
associated with heredity, obesity, anatomical joint abnormality, injury, overuse
a) OA
b) RA
OA
Before the age of 50, ... are more likely to have OA; past the age of 50, who predominates?
before 50: men
after 50: women predominate.
OA is classified as
primary or secondary
Primary OA: cause
has no known cause
may be localized (ie, involvement of one or two joints) or generalized (ie, diffuse involvement generally including three or more joints).
Secondary OA cause
can be related to an identifiable cause, such as trauma, anatomic abnormalities, infection, or aseptic necrosis.
hairdressers have a high risk of what disease?
OA - constant wear and tear of the hands and wrists
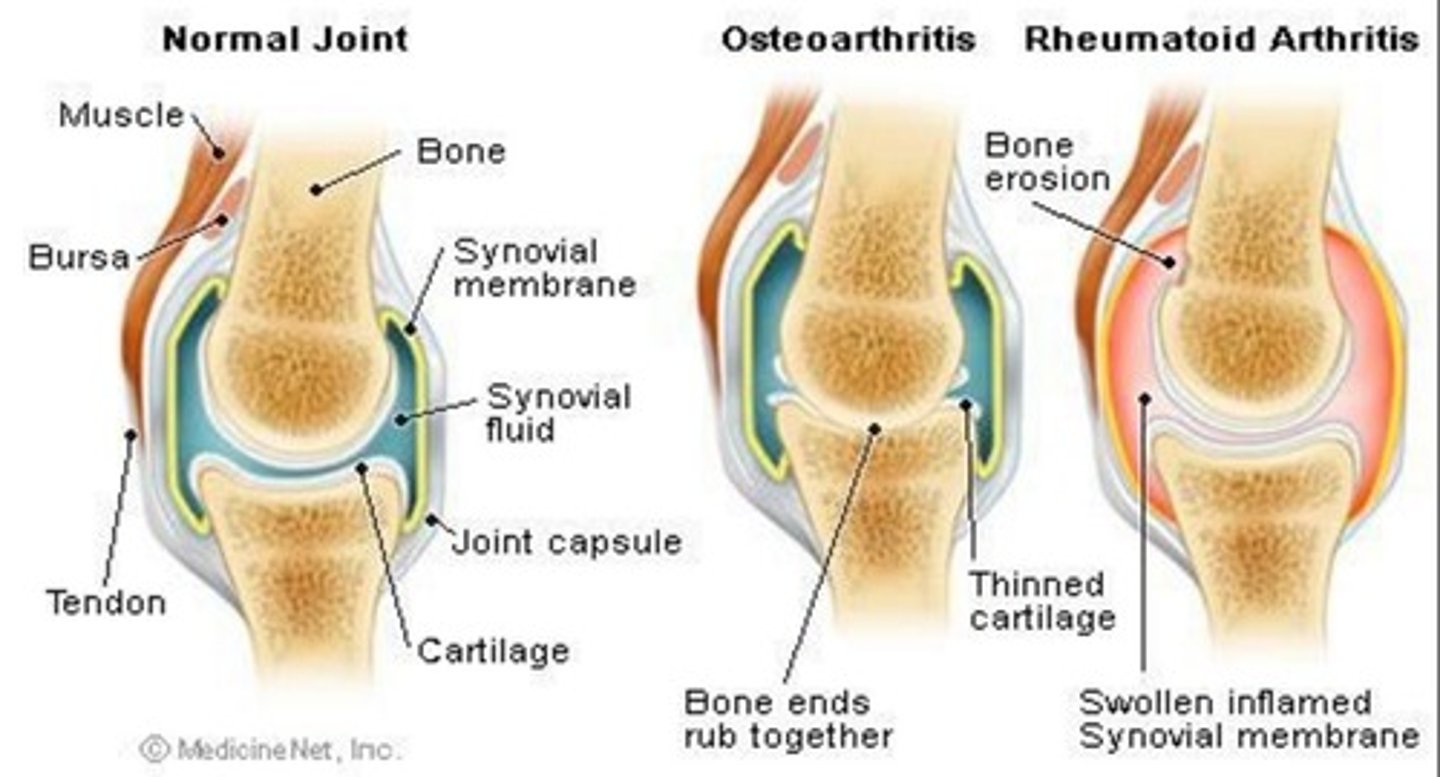
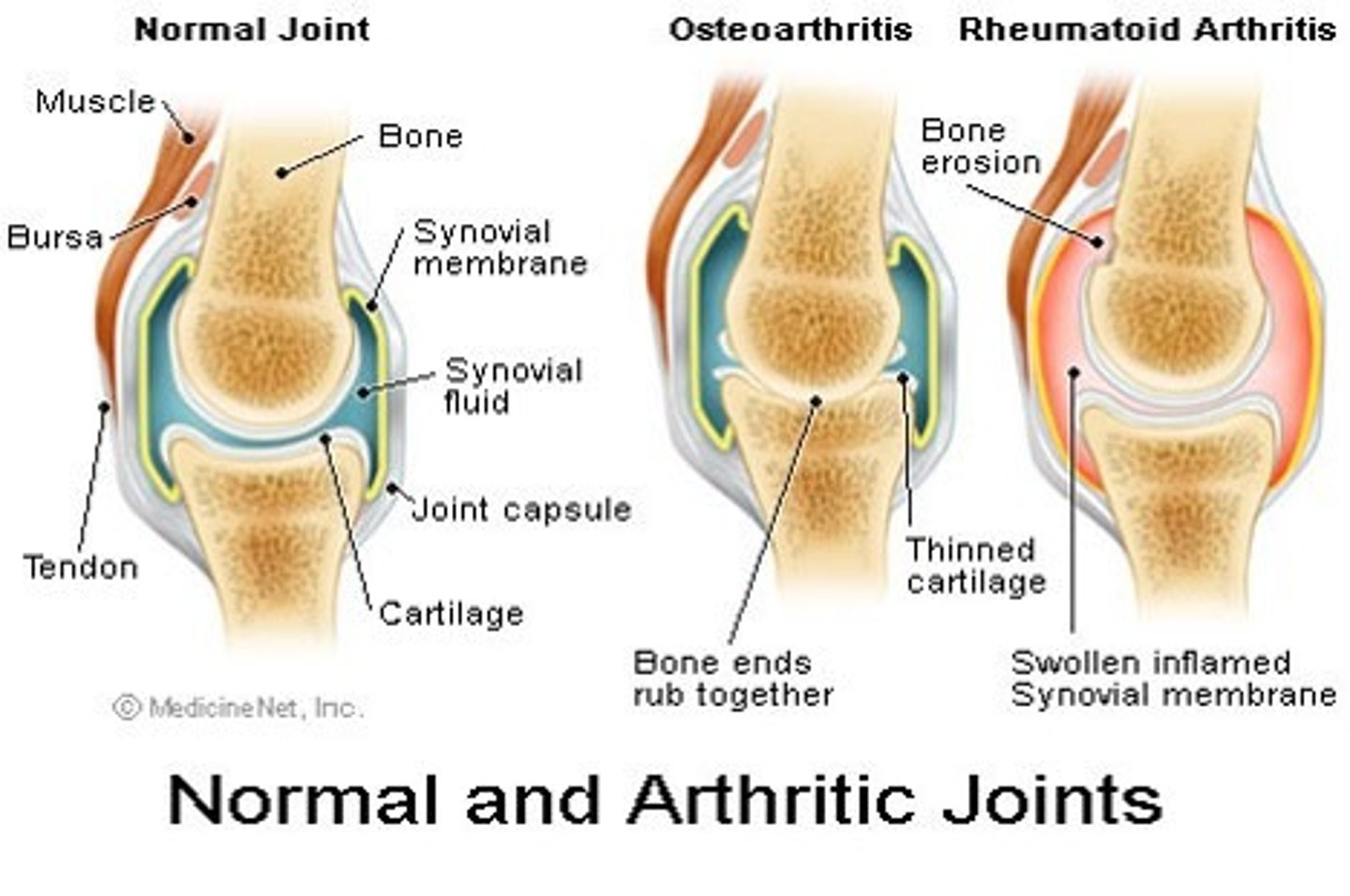
Cartilage wears down and interferes with joint movement
a) OA
b) RA
OA
bone erosion
a) OA
b) RA
RA
lines of the hands are normal and some swelling at the joints
a) OA
b) RA
OA
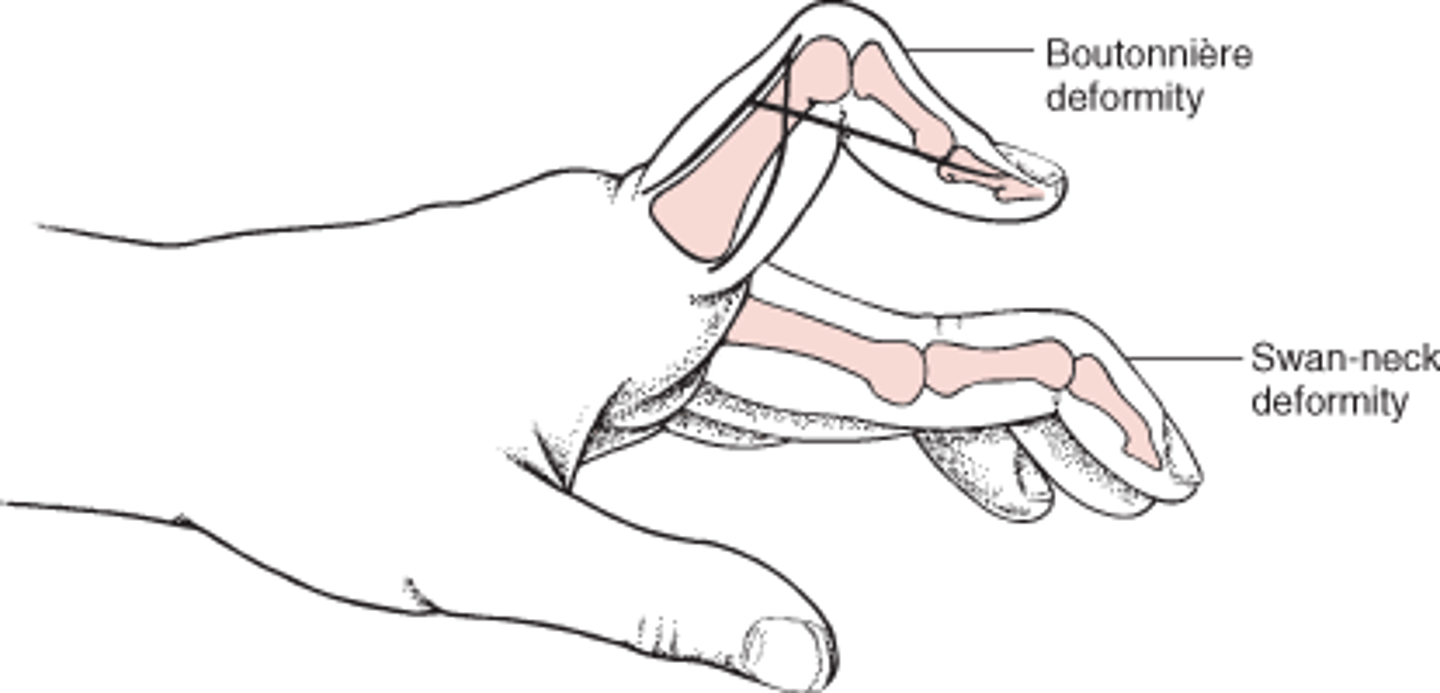
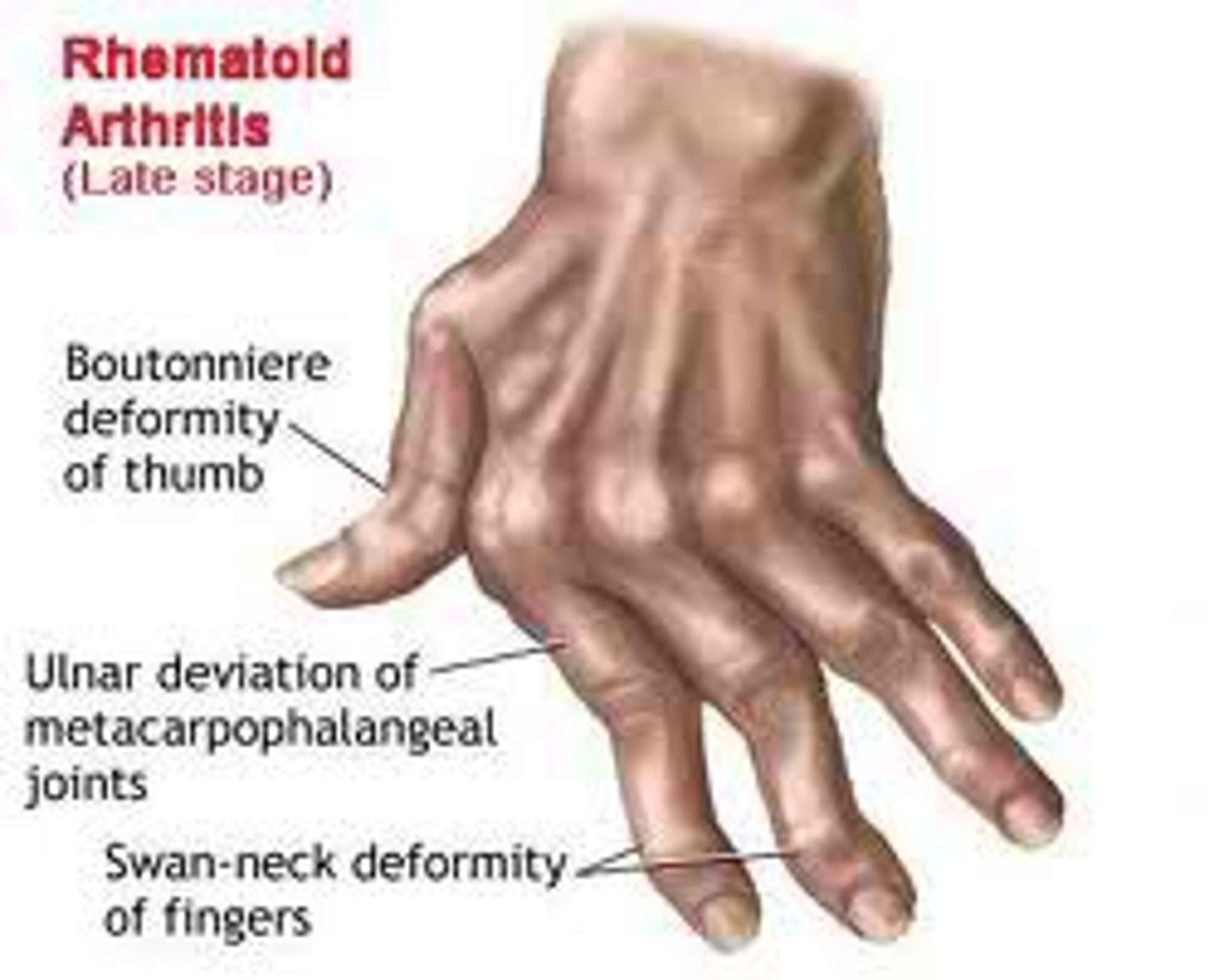
Boutonniere deformity
flexion of PIP joint and hyperextension of DIP joint
common in RA
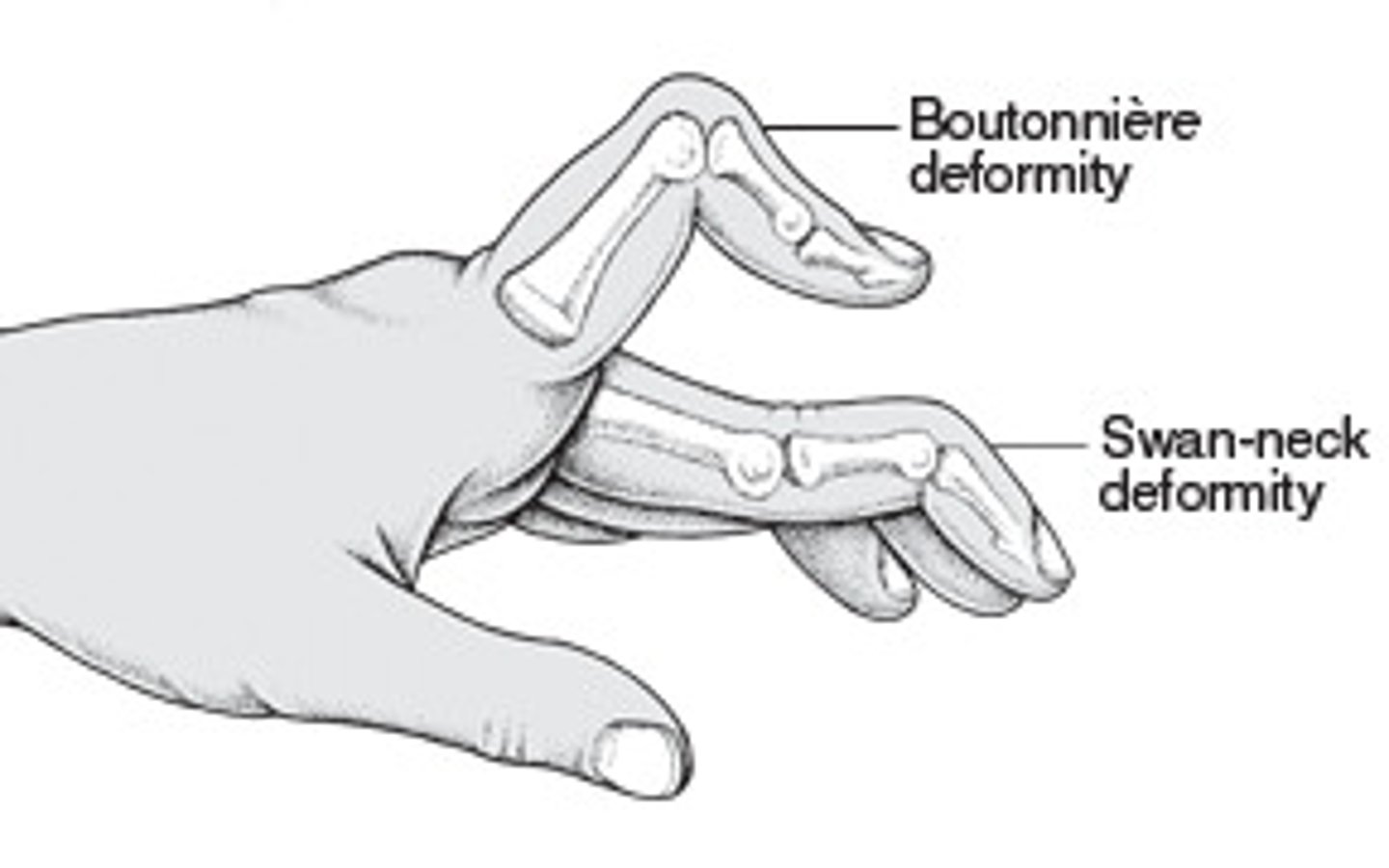
Swank neck deformity
PIP hyperextension
DIP flexion
common in RA
DJD
degenerative joint disease
ambulating with poor posture for a long time can lead to
a) OA
b) RA
OA
common joints that OA affects
- hands (DIP, PIP, thumb CMC)
- feet (MTP)
- hips
- knees
- spine (cervical and lumbar)
*may arise on both sides of the body
morning stiffness in OA
common but of short duration
usually less than 20 minutes
short morning stiffness
a) OA
b) RA
OA
swelling in OA
warm, swelling and joint redness are usually MINIMAL or NOT PRESENT
clinical features of OA
- pain
- stiffness
- tenderness
- limited movement
- variable degrees of local inflammation
- crepitus
- may see reduced ROM --> with crepitus and hard end field
crepitus
an audible or palpable crunching or popping in the joint caused by the irregularity of opposing cartilage surfaces
Pain and stiffness typically occur with activity and are relieved by rest, but eventually they become present at rest and at night.
a) OA
b) RA
OA
OA is a two part process:
1) deterioration of articular cartilage
2) new bone formation
type of OA related to an indetifiable cause
secondary
- trauma
- repetitive motions
- anatomical abnormalities
- infections
- necrosis
type of OA with no known cause and may be localized or generalized
primary OA
*most common
The diagnosis of OA is initially made on the basis of the patient's
history and physical examination, with a lack of systemic symptoms ruling out inflammatory disorders such as RA.
- X-rays
- MRI
does OA have a cure?
no
OA Hand Deformities
Heberden's nodes (DIP)
Bouchard's nodes (PIP)
Thumb Capometacarpal
Goals in the treatment of OA are
relieve symptoms
improve function
limit disability
avoid drug toxicity
OA medications may target ... or .... . What types of meds?
system or local joints
- pain relievers
- anti-inflammatory
- non pharmacological agents
*know symptoms and side effects and how they affect occupations (nausea, flush, sleep)
OA surgical management
- Arthroscopic joint debridement (small camera, clean out area)
- grafting (take part of the body and substitute)
- fusion (no movement = no pain)
- joint replacement
Tx for OA
positioning --> splints (why? help area rest, provides function, facilitates pinch)
pain management (meds, stretching)
joint protection techniques
increased function
OA and pain management techniques
1) positioning
2) splinting
3) thermal modalities
4) rest
5) medication management
6) energy conservation
7) relaxation techniques
8) TENS (e-stim for pain)
9) joint protection (consider internal and external forces)
10) exercise
when considering joint protection, what are some examples of external forces placed on the joints?
- odd shaped objects
- slippery surfaces
- tight fit objects (lids, covers)
- small handle
- cold object
most joints become stressed in what position?
flexion
- grasping objects tightly
- poor placement of hand and joints
what position must we avoid if RA is present? what activities?
ulnar deviation!
Avoid/find different ways to:
- holding knives
- lifting plates
- opening jars
- turning doorknob
- pushing in a drawer
- wringing out cloth
Adaptations for RA and OA
-use tools with large/rounded handles (avoid tight grasp)
- used spike board to stabilize veggies when cutting them
- grasp objects between the palms of both hands instead of using handles
The purpose of joint protection is to
reduce internal and external joint stress, pain, and inflammation in the involved joints and preserve the integrity of joint structures during the performance of daily activities
joint protection principles
1. Respect pain
2. Maintain strength and ROM
3. Use joint in most stable anatomical plane
4. Avoid positions of deformity
5. Use strongest joint available
6. Ensure correct patterns of movement
7. Avoid staying in one position for long periods
8. Avoid starting an activity that cannot be stopped
9. Balance rest and activity
10. Reduce force and effort
maintaining grasp or sustaining a position ...
fatigues muscles easily
STOP sustained activities .... muscle fatigues
before
... will decrease the torque
increasing the level arm will
circumference and joint protection
increasing the circumference decreases the force
big objects = easier
diameter and joint protection
increasing the diameter will decrease the amount of grip
preserves the smaller joins
reduces fatigue from static holding
ex: knifes, and spoons
what joints should we use whenever possible to reduce risk/pain from OA and/or RA?
use unaffected joints or larger joints whenever possible
joint protection: knives and scissors
make sure that they are sharp
stabilize using dycem
joint protection: stability
use pre-fabricated splints (sports braces)
non-intrusive and look "normal"
joint protection: adapt the environment
- arrangements of objects in environment
ex: place things hip to shoulder height
ex: an electric can opener may seem useful but if its in a cluttered environment it might be more stressful
joint protection: tooth brush
built up handle for bigger grasp which leads to less of an effort to hold
joint protection: correct way to hold a book
place both palms under the book
avoid using fingers
joint protection: key
avoid lateral pinch
use a key grip to hold using a power grip
joint protection: getting up from a chair
Use of palms to push off a chair helps protect finger joints.
For example, the client may use the dorsum of the fingers to push up from a seated position (knuckles). This movement places deforming forces toward MCP flexion. A more suitable pattern is to use the flat surface of the palm.
if unable, place forearms in a nearby table and push up
goals of assistive devices
1) maintain and/or increase independence/participation
2) simplify task
3) decrease pain
4) decrease unnecessary strain in the joints
Commonly used AD in arthritis interventions are
extended-handle devices (eg, reacher, bath sponge, shoe horn, dressing stick, comb) --> to compensate for loss of proximal ROM and strength
devices with built-up handles (eg, hairbrush, toothbrush, writing implement, eating utensil, knob turner) --> to compensate for limited hand function
patient education
• use self-management based on knowledge
• recognize need for assistance
• use members of team appropriately
• use community resources
• incorporate treatment into daily routine
• live as "normally" as possible
*confirm that the patient understood what you are educating them about
Repetition, reinforcement, and real-life application to the client's situation are other keys to education.
Rather than focusing exclusively on providing basic information and generic skills, encouraging ... has been suggested as a helpful part of rehabilitation.
client self-reflection and transformation of client perspectives
The purpose of joint protection is to
reduce internal and external joint stress, pain, and inflammation in the involved joints and preserve the integrity of joint structures during the performance of daily activities.
THR adaptive equipment
1) sock aid
2) reacher
3) easy shoe laces
*extended handled devices
AE for the bathroom after THR
1) elevated toilet seat
2) handrails or grab bars
3) adjustable tub or shower bench (must be higher to avoid flexion)
4) Handheld shower hose,
5) bath bench
6) long-handled sponge
THR Adaptations: environment
avoid scattered rugs
elevate the couch, chair or recliner
(seat height that is at least twenty inches above the floor)
THR adaptations: shelves
avoid excessive bending and lifting
arrange shelves and cupboards with frequently use items at waist to shoulder height
AE for dressing
Dressing stick, shoe horn, sock aid, button hook, zipper pull, elastic shoelaces
AE for toiletting
Raised toilet seat, grab bars, extended perineal hygiene aid
AE for hygiene and grooming
Built-up or extended-handle toothbrush, suction denture brush, extended-handle hairbrush or comb, suction nail brush, mounted nail clipper
AE for feeding
Built-up or extended-handle utensils, lightweight T-handled mug
AE for meal preparation
Electric can and jar openers, adapted cutting board, utensils with built-up handles, ergonomic right-angled knives, rolling utility cart, knob turner for stove, reacher
RA: classic external signs and symptoms of inflammation
- heat
- edema
- erythema
- pain
peak incidence of RA
The peak incidence occurs between 40 and 60 years of age, with the rate of disease two to three times higher in females
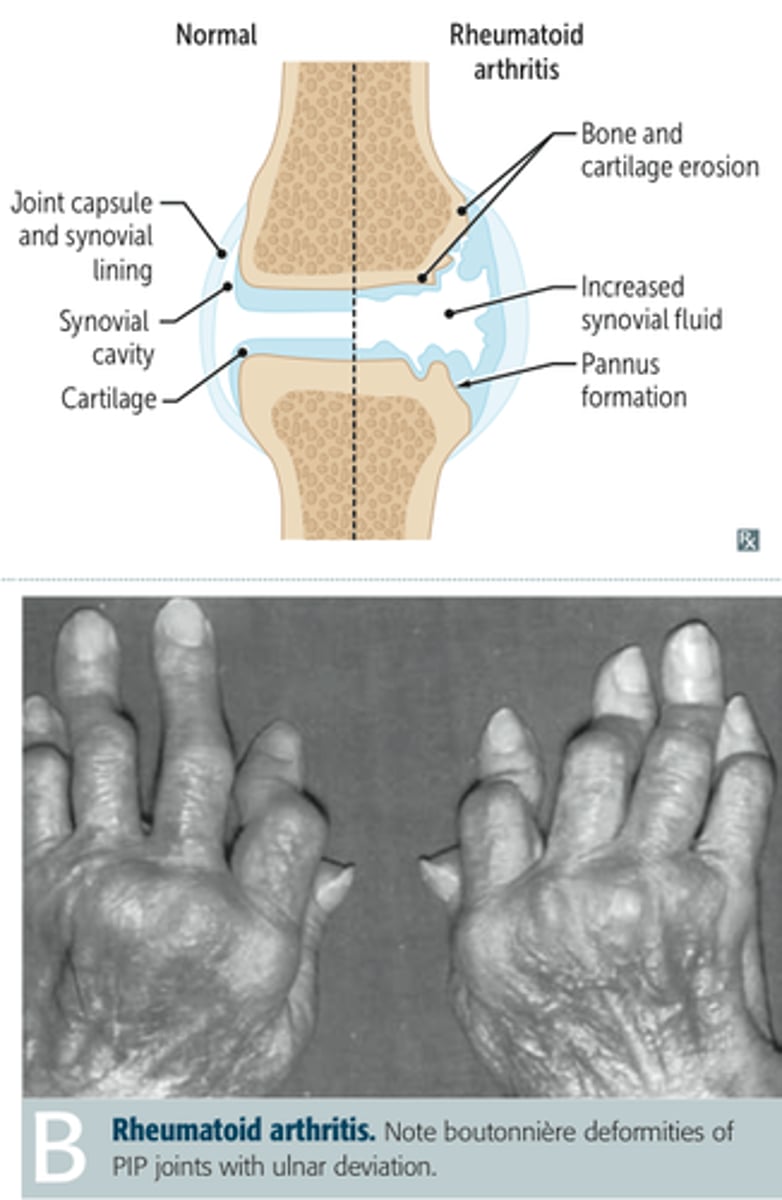
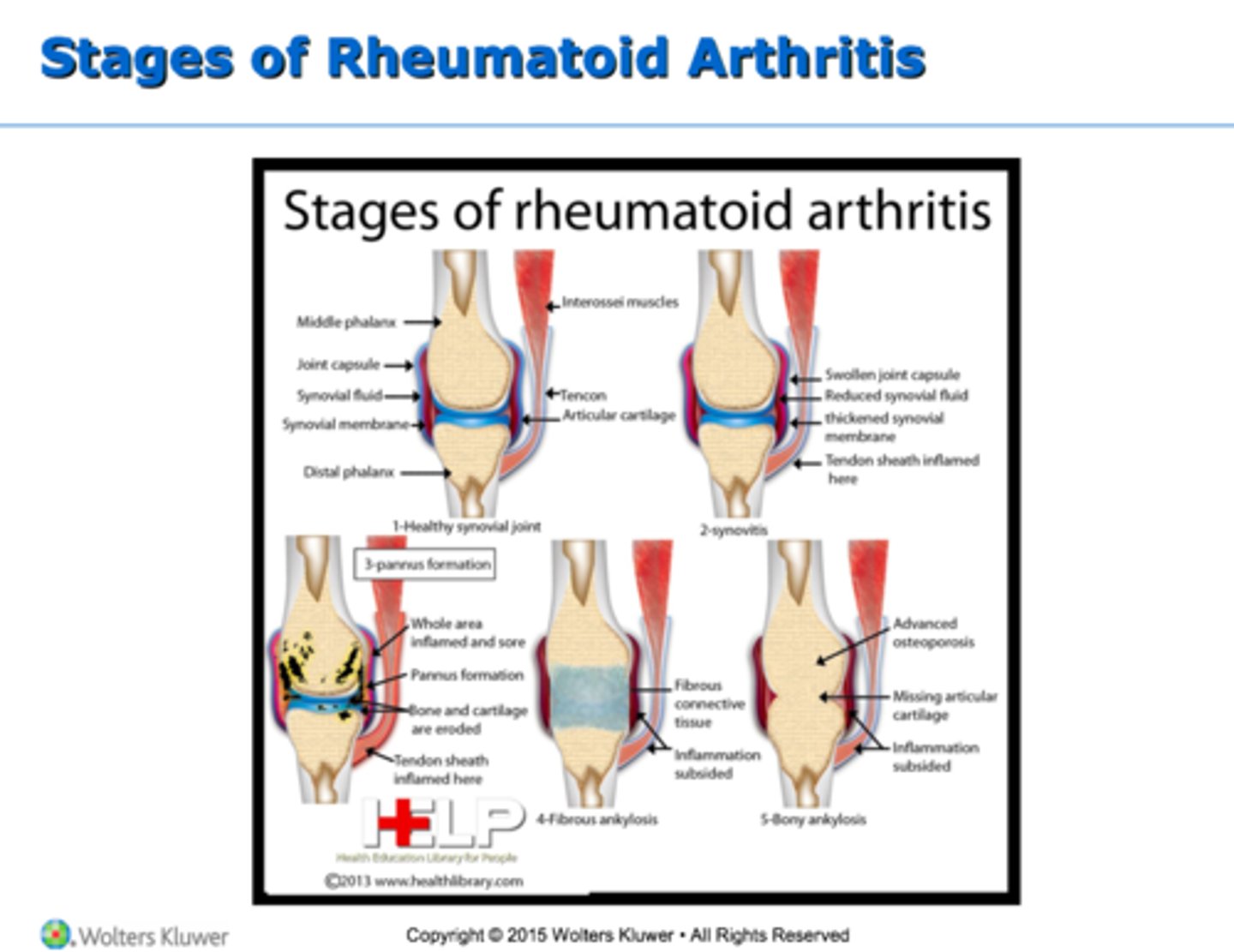
synovitis
inflammation of the synovial membrane that results in swelling and pain of the affected joint
present in RA
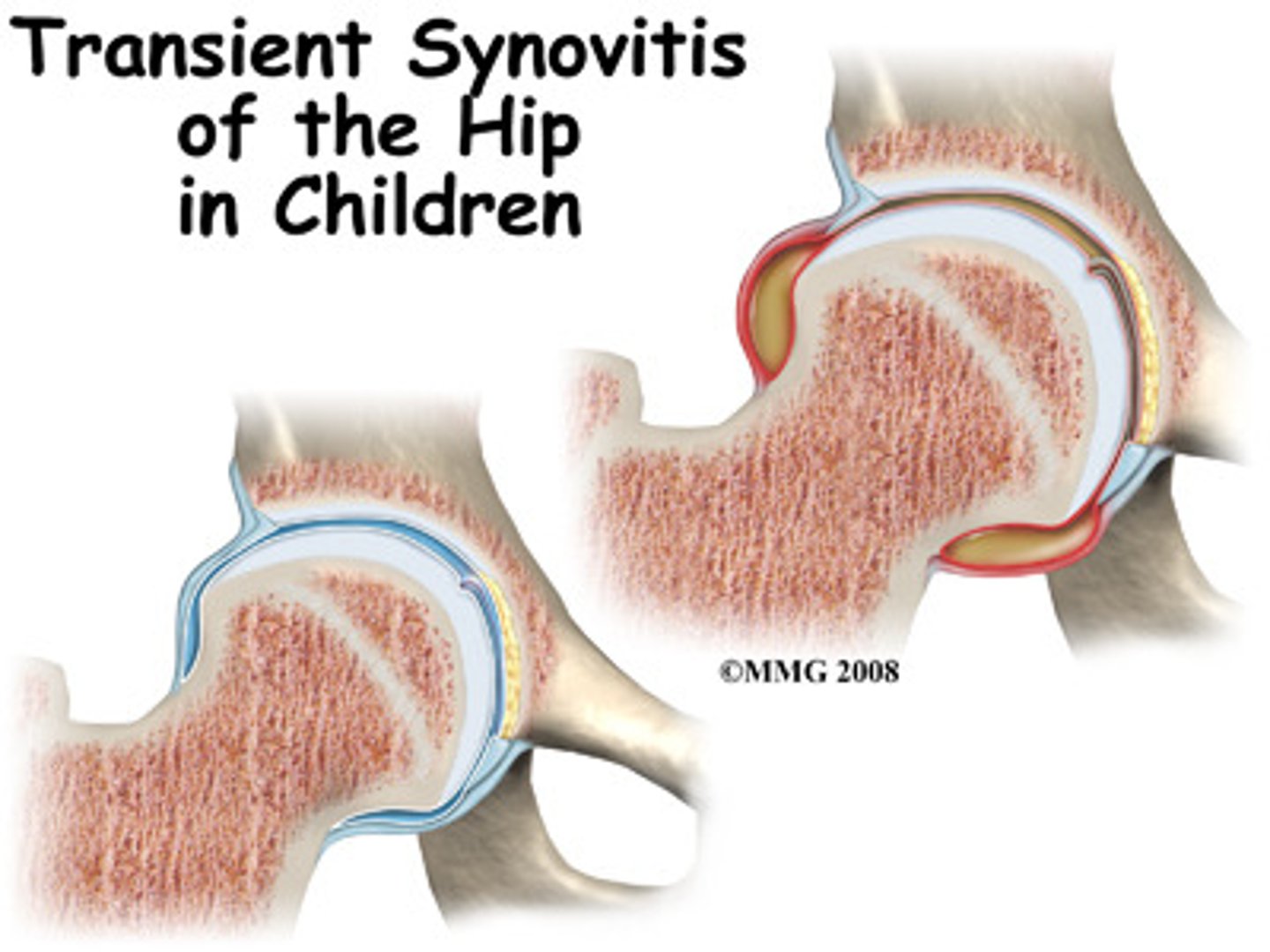
Joint swelling from RA results from
excessive production of synovial fluid, enlargement of the synovium, and thickening of the joint capsule
this weakens the joint capsule and distends tendons and ligaments.
As the inflammatory process continues, the diseased synovial membrane forms a pannus that actively invades and destroys cartilage, bone, tendon, and ligament.
Scar tissue can form between the bone ends and cause the joint to become permanently rigid and immovable.
Dx criteria for RA
▪Morning stiffness greater than 1 hour
▪Arthritis of 3 or more joint areas
▪Arthritis of hand joints
▪Symmetrical arthritis (involvement on both sides)
▪Rheumatoid nodules
▪RH factor (blood test)
▪X-ray changes
*need at least 4
signs of early stages of RA
edema
no deformity
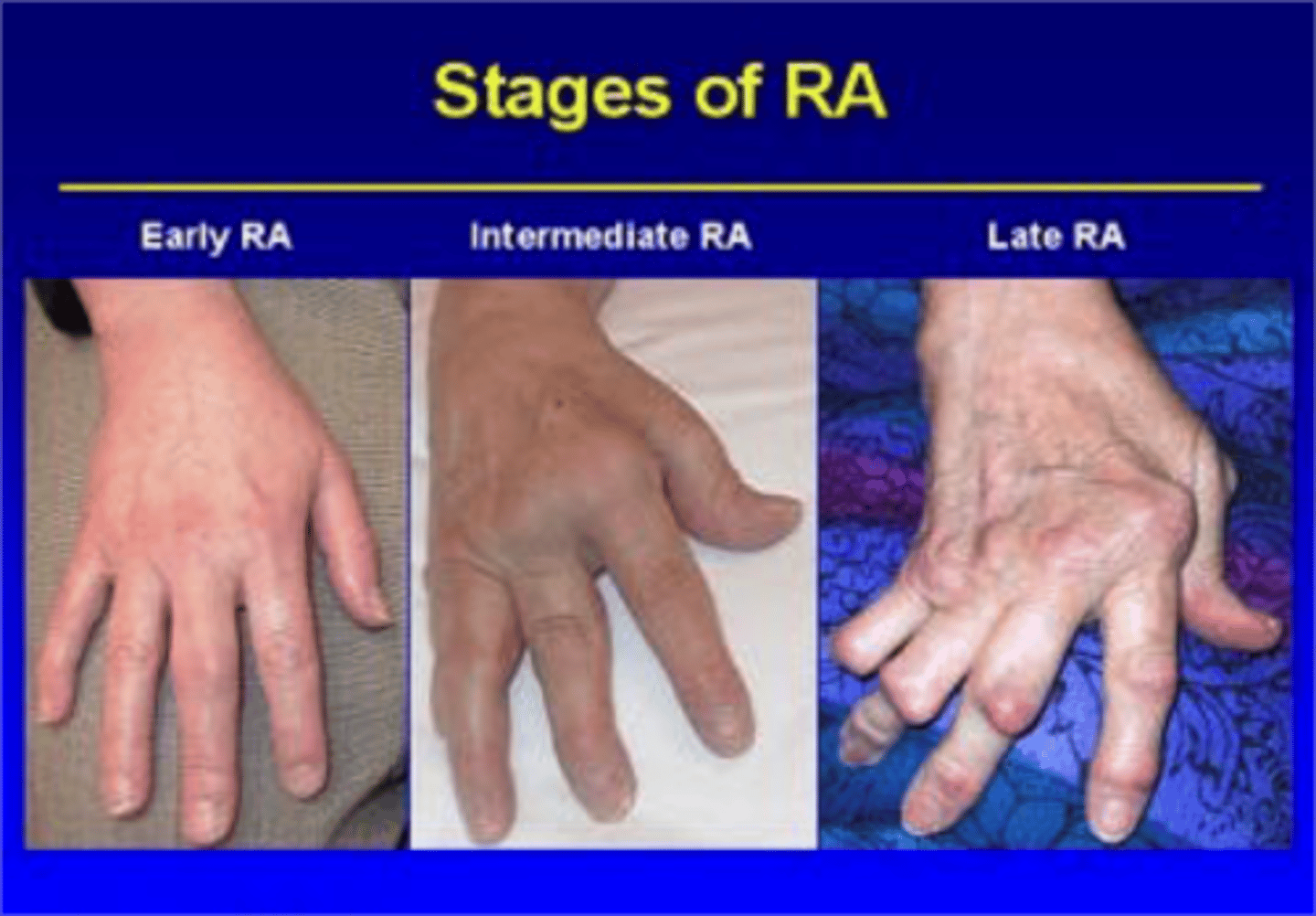
signs of late stages of RA
joint deformities
ulnar drift
The inflammatory process of RA has been described as having four stages:
1) acute (flares up)
2) subacute
3) chronic active,
4) chronic inactive.
acute stage of RA signs
typically a flare up
▪Pain
▪Inflammation
▪Hot, red joints
▪Tenderness
▪Overall stiffness
▪Limited motion
