Microscopic UA Part 3 - Crystals
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
Urinary Crystals Formation
Formed by precipitation of solutes (salts, meds, metabolites)
Influenced by:
Temperature: lower temps → ↑ precipitation
Solute concentration: ↑ [conc] → ↓ solubility
pH: affects both crystal formation and ID
Abnormal Urinary Crystals
May indicate:
Liver disease
Inborn errors of metabolism
Renal disease
Renal calculi (kidney stones)
Crystal Identification in Urinalysis
Morphology: Shape, color, size
pH: Determines crystal type
Polarized light: ability to polarize light
Solubility testing:
Insoluble = remains crystalline
Soluble = dissolves with pH or temperature
Example: Amorphous urates dissolve in alkaline (NaOH) or heat (Soluble)
"Normal" Crystals in Urine
Considered normal when their concentration is low and the patient is healthy
"Normal" is a relative term—context matters
Amorphous Crystals Overview
Non-crystalline: no defined shape (don't confuse with granular casts)
Amorphous. = No morphology
No clinical significance
Form in acidic or alkaline urine, depending on type
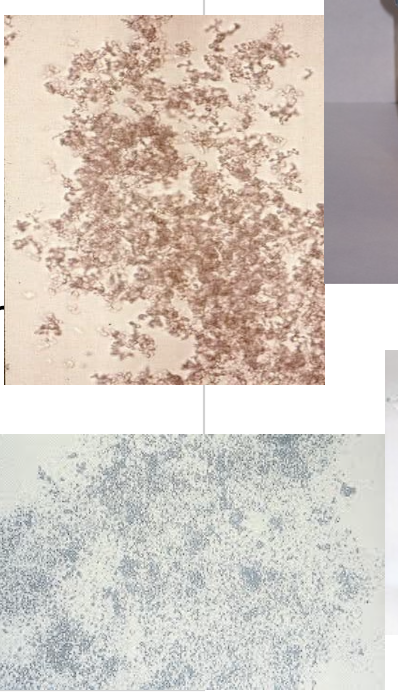
Amorphous Urates (Acidic Urine)
Common in refrigerated samples
Made of Ca²⁺, Mg²⁺, Na⁺, K⁺ urates
Pink sediment; brown-pink granules microscopically
Soluble in heat and alkaline conditions
Amorphous Phosphates (Alkaline Urine)
Composed of phosphates and calcium
Sediment is white
Soluble in acetic acid
Much more rare
Not clinically significant
Sodium Urate Crystals
Normal finding, often seen after refrigeration
Caused by protein-rich diet
Not clinically significant; typically not reported if observed in specimens
Uric Acid Crystals
Found in acidic urine
Normal in low concentrations
Increased levels associated with:
Gout
Acute febrile conditions
Chronic nephritis
Lesch-Nyhan syndrome (excess uric acid)
Soluble in alkali and heat
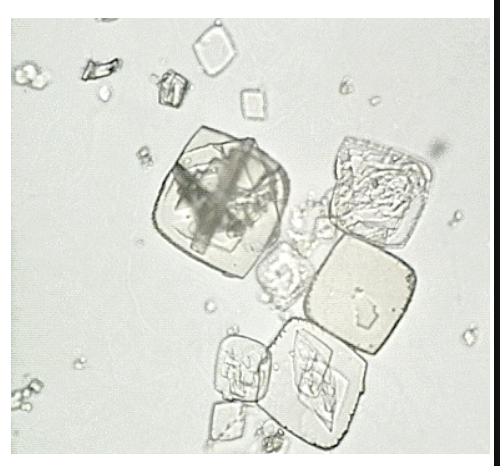
Uric Acid Crystal Morphology
Color: Typically yellow or brown; may also be colorless
Forms: Highly variable
Barrels
Rhombic plates
Rosettes
Morphology helps in identification but varies widely in shape
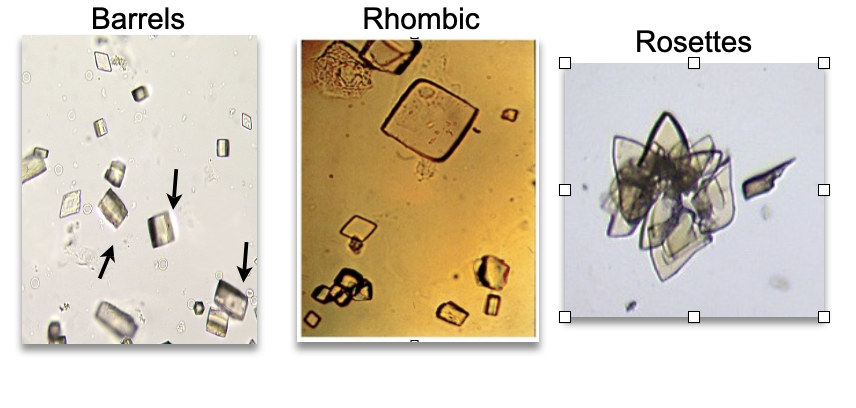
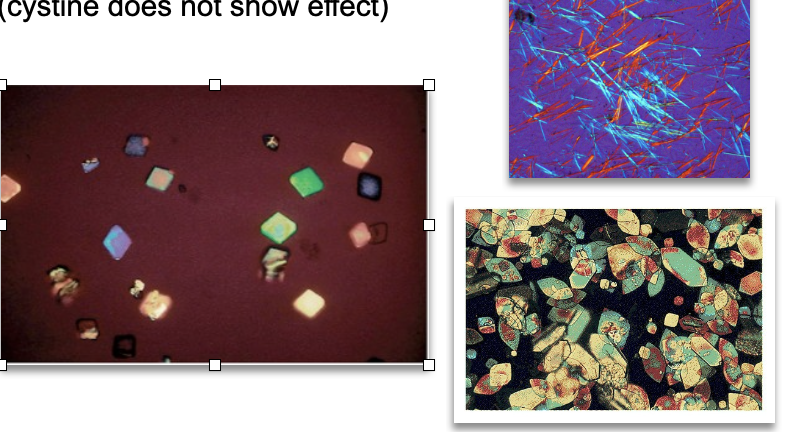
Uric Acid Crystal: Polarized Light Properties
Highly birefringent under polarized light
Exhibits colorful, refractive patterns
Helps differentiate from cystine crystals, which do not show birefringence
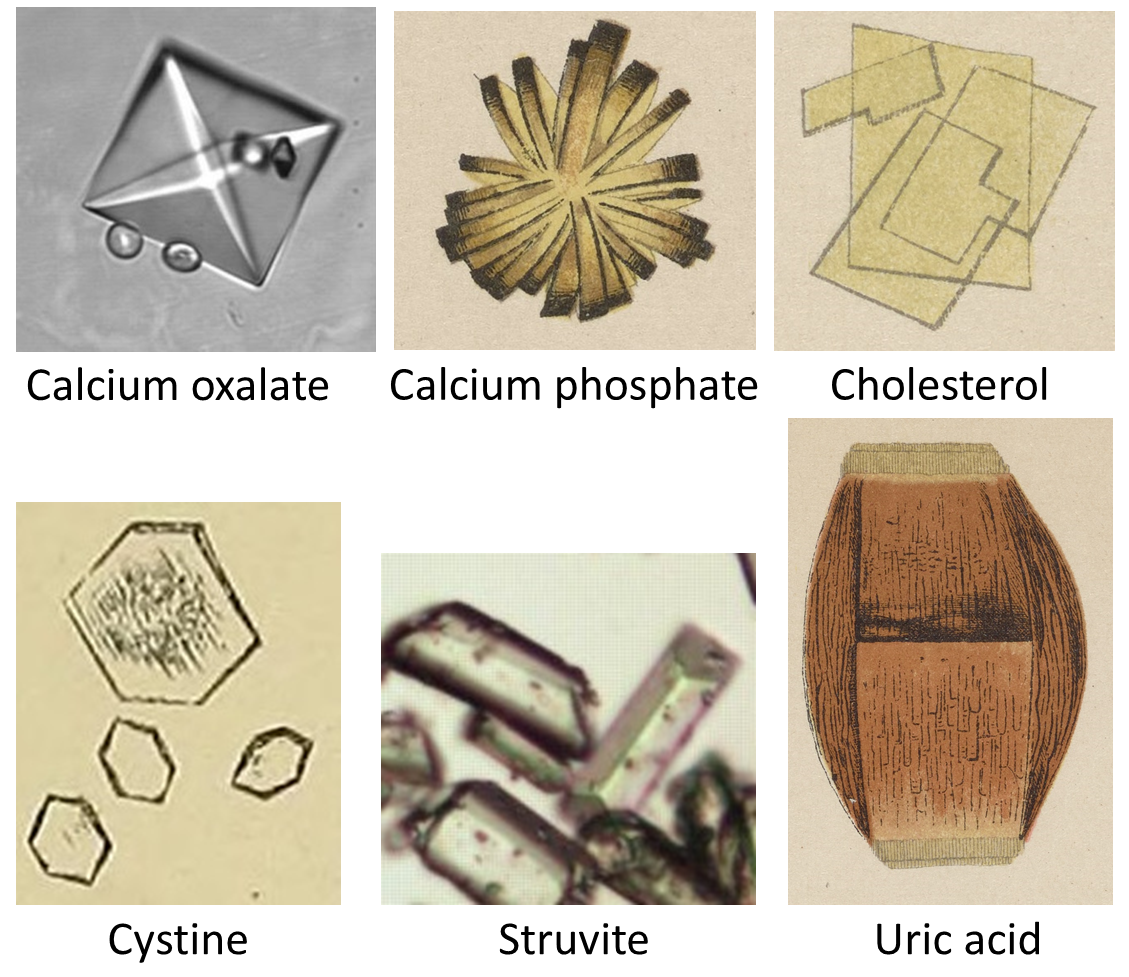
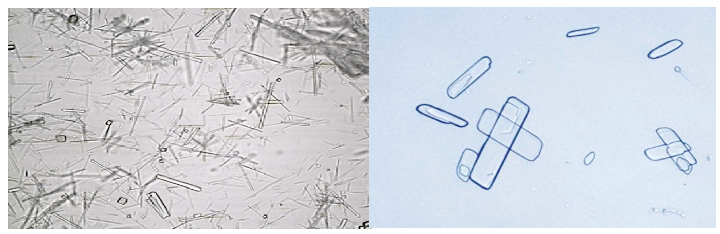
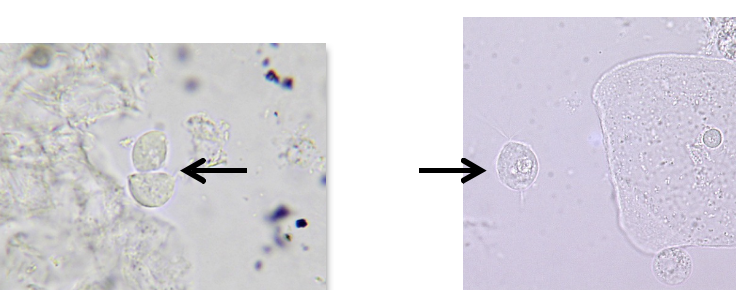
Calcium Oxalate Crystals
Found in acidic to slightly alkaline pH
Calcium oxalate crystals polarize light
Soluble in HCl
Insoluble in acetic acid
Morphologies: dumbbell, rectangular, octahedral ("envelope"), ovoid
Frequently encountered; common in kidney stones
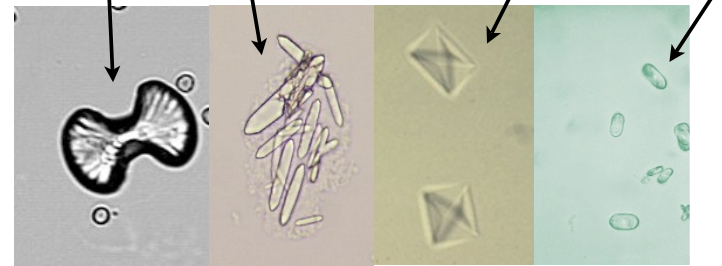
Calcium Oxalate Forms
Dihydrate: envelope-shaped (two pyramids base-to-base), most common
Monohydrate: dumbbell, oval, or rectangular (can resemble RBCs)
Long monohydrate form linked to ethylene glycol poisoning
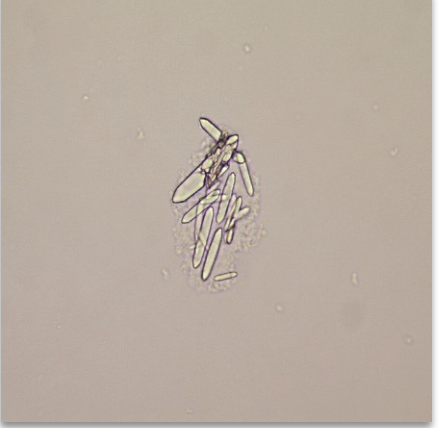
Clinical Relevance of Calcium Oxalate
Associated with:
Renal calculi (kidney stones)
Oxalic acid poisoning
Liver disease
Ethylene glycol poisoning (especially long monohydrate form)
May be confused with hippuric acid crystals—note shape differences
Hippuric Acid Crystals
Rare, colorless prisms/needles/plates in acid, neutral, or alkaline urine
Soluble in alkali, hot water
Associated with benzoic acid–rich diets, liver dysfunction, and toluene exposure
May resemble Ca oxalate monohydrate or triple phosphate—differentiate by solubility and weak polarization

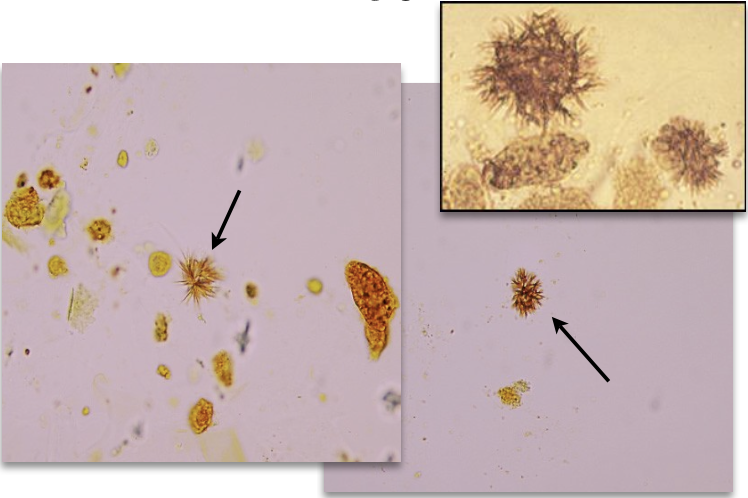
Ammonium Biurate Crystals
Appearance: “Thorny apples,” yellow-brown, seen in alkaline urine
Soluble in: Acetic acid, heat
Significance:
Only relevant in freshly voided urine
Typically an artifact from old/improperly stored specimens
Note: Converts to uric acid crystals with acetic acid addition

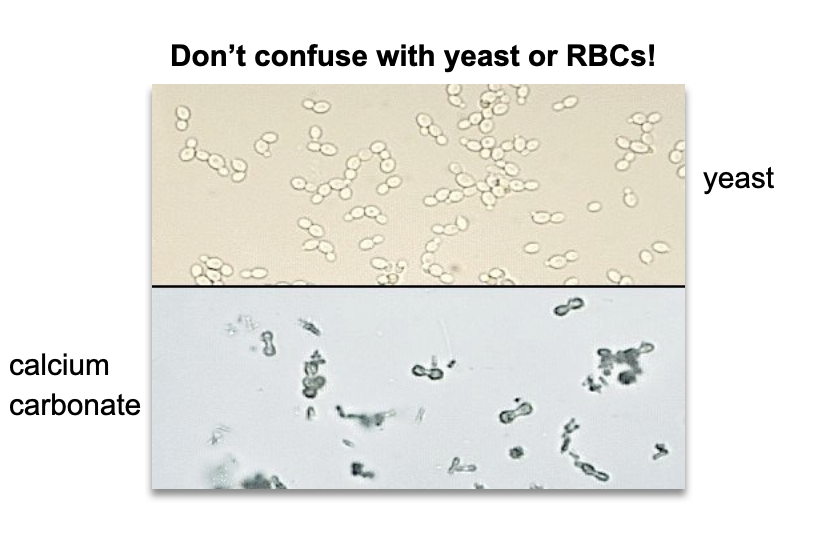
Calcium Carbonate Crystals
Found in alkaline urine
Morphology: Dumbbell or spherical shape; may resemble granules
Solubility: Effervesces with HCl and acetic acid
Differential ID: May be confused with yeast or RBCs—confirm with solubility and morphology
→ Watch for misidentification due to small, round appearance in clumps or singly
Calcium Phosphate Crystals
Appearance: Colorless; large flat plates, rosettes, or wedge-shaped prisms
Urine pH: Alkaline
Solubility: Dissolves in dilute acetic acid
Notes:
Rosette form may mimic sulfonamide crystals (distinguished by solubility: sulfonamides do not dissolve in acid)
Can appear in normal urine
May be associated with kidney stones
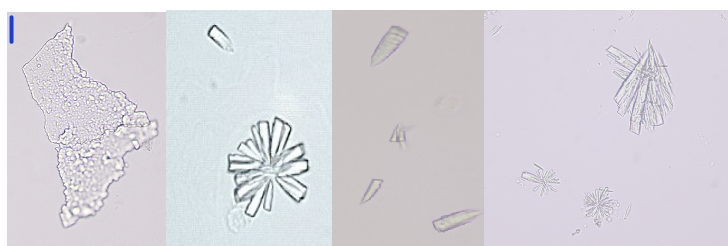
Triple Phosphate (Ammonium Magnesium Phosphate)
Appearance: Colorless, prism-shaped ("coffin lid"); may appear feathery as they dissolve
pH: Alkaline urine
Solubility: Soluble in acetic acid
Polarized Light: Birefringent
Formation: Common in alkaline urine due to bacteria that split urea into ammonia & CO₂
Contextual Note:
Often seen in urinary tract infections; appearance can vary—classic coffin-lid crystals may shift to feather-like shapes as they dissolve.

Abnormal Crystals – Key Features
pH: Typically found in acidic urine
Significance: Clinically significant; may indicate underlying pathology
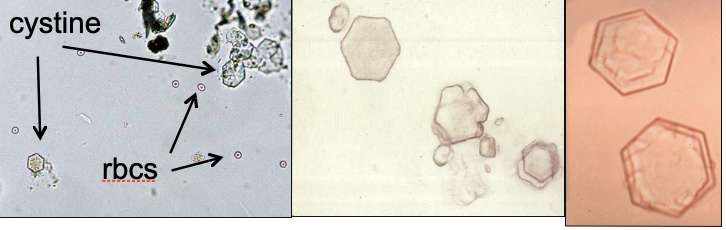
Cystine Crystals
Appearance: Colorless, thin, hexagonal plates
Found in: Acidic urine
Solubility: Soluble in HCl, NaOH, NH₄OH
Polarized light: No birefringence (differentiates from uric acid)
Associated condition: Cystinuria — an inherited metabolic disorder causing defective reabsorption of cystine by renal tubules
Clinical relevance: Most frequent cause of kidney stones in children
Differentiation tip: May resemble uric acid crystals; distinguish based on lack of birefringence and solubility profile
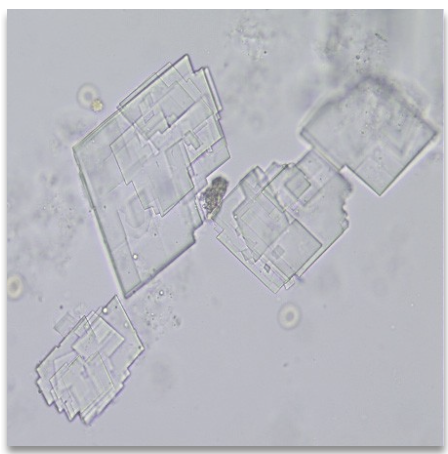
Cholesterol Crystals
Appearance: Clear, flat, rectangular plates with a notched corner
Urine type: Acidic
Solubility: Soluble in chloroform, ether
Polarized light: Birefringent (brightly colored under polarization)
Associated conditions:
Nephritis, nephrotic syndrome (excess tissue breakdown)
Chyluria (obstructed lymph drainage from tumors, filariasis, lymph node enlargement)
Additional notes:
Rare in urine; lipids typically remain as droplets
Refrigeration may artifactually cause appearance
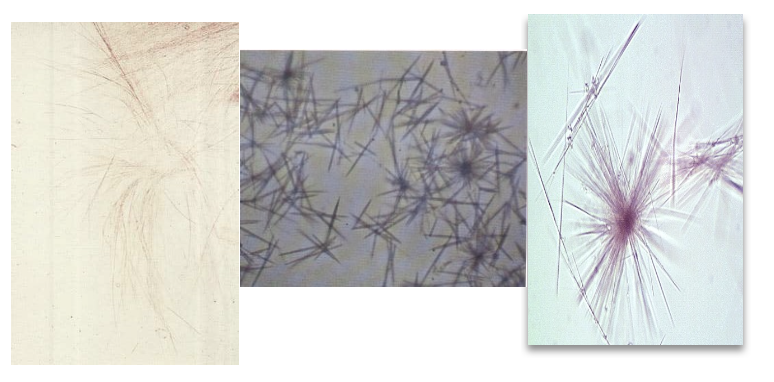
Tyrosine Crystals
Appearance: Very rare; colorless to yellow-brown. Fine, sharp needles—may appear singly, in sheaves, or rosettes.
Solubility: Soluble in HCl and NH₄OH
Urine pH: Acidic
Bilirubin test: Positive
Seen in:
Severe liver disease
Inherited amino acid metabolism disorders (e.g., tyrosinemia)
Often appears with leucine crystals
Contextual clue: Presence suggests hepatic dysfunction—especially if both tyrosine and leucine are observed.
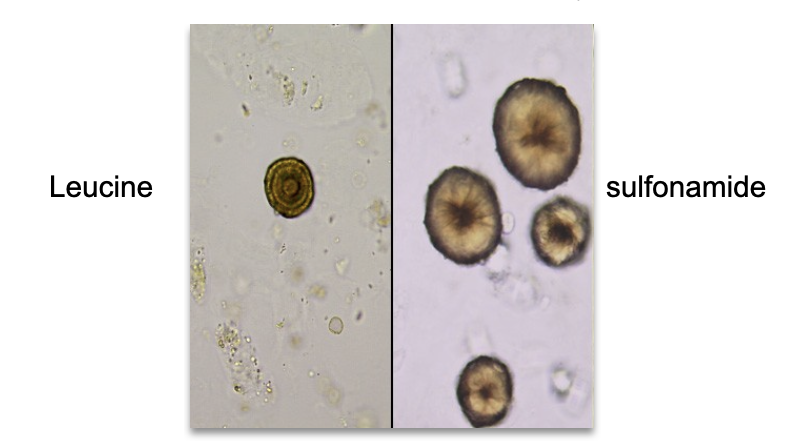
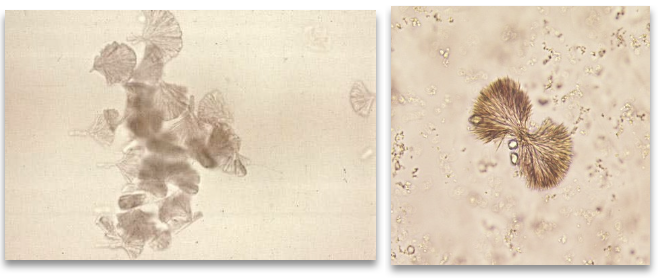
Leucine Crystals
Morphology: Yellow-brown spheroids with concentric rings (outer edge) and radial striations (center)
Found in: Acidic urine
Soluble in: NaOH, hot water
Associated Conditions:
Severe liver disorders (e.g. cirrhosis, severe viral hepatitis)
Maple syrup urine disease
Amino acid metabolism disorders
Often seen with: Tyrosine crystals
Bilirubin test: Positive
Pitfall: May be confused with sulfonamide crystals (distinguishable by structure). Many antibiotics have sulfonamides in them. Perform solubility test to distinguish between the two.
Bilirubin Crystals
Appearance: Yellow-brown (sometimes bright orange) needles or granules, often in clumps or attached to cells
Urine pH: Acidic
Solubility: Acetic acid, HCl, NaOH, acetone
Bilirubin test: Positive, won’t see this otherwise
Clinical context: Seen in severe liver disorders; correlate with patient history and jaundice
Additional notes: Can be mistaken for amorphous material; distinct spiky needle bundles
Radiographic Dye Crystals
Appearance: Flat needles or sheaves; highly variable
May mimic: Cholesterol, tyrosine, sulfonamides
Polarized light: Strong birefringence
Key ID clues:
Recent radiographic procedure (history essential)
Very high specific gravity (>1.035)
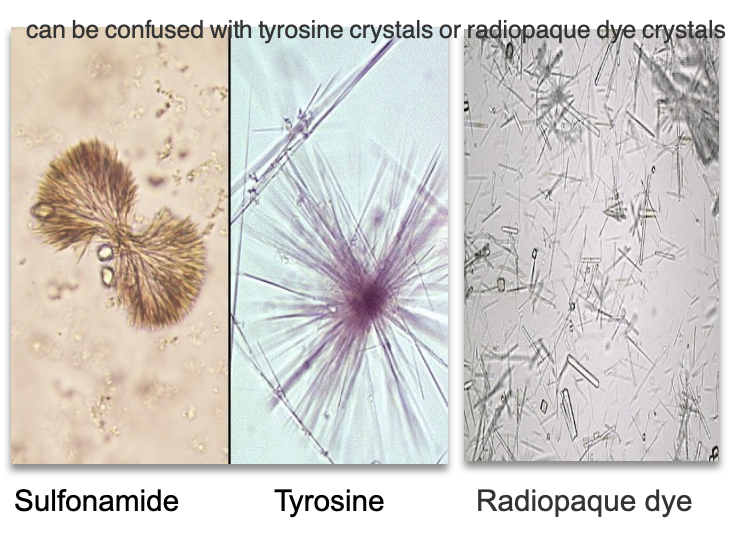
Sulfonamide Crystals – Morphology & Clinical Context
Appearance: Brown crystals seen as spheroids, flat needles, or sheaves of small needles
Urine pH: Acid
Solubility: Acetone & alkali
Cause: Seen in patients taking sulfonamide antibiotics
Associated: Risk of kidney stone formation, especially with dehydration
Clinical tip: Confirm via medical history
Sulfonamide Crystals – Differential Diagnosis
Can be mistaken for:
Leucine (spheroid, yellow concentric rings)
Tyrosine (fine needle sheaves/rosettes)
Radiographic dye (flat needles, high SG, birefringent)
Clue: Sulfa crystals typically brown; patient history + hydration status helps confirm diagnosis.
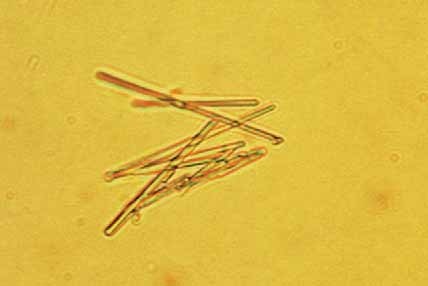
Acyclovir Crystals
Source: Anti-viral medication (e.g., herpes treatment)
Urine pH: Neutral to slightly alkaline
Morphology: Long, thin, needle-like crystals
May be confused with: Tyrosine crystals
Clinical tip: Confirm with patient medication history
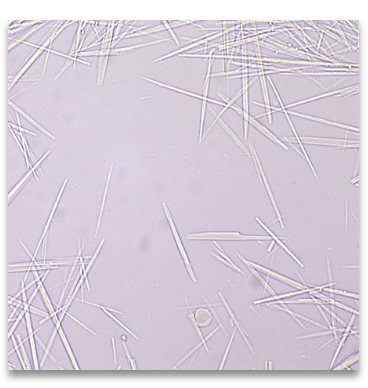
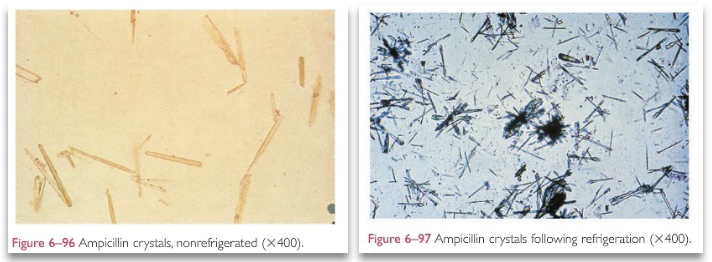
Ampicillin Crystals
Cause: High-dose ampicillin + poor hydration
Morphology: Colorless needles; may clump post-refrigeration
Key ID Clue: Appear bundled after refrigeration
Diagnostic Tip: Confirm via medication history
Artifacts (Contaminants in Urine)
Cause: Poor collection technique or dirty containers
Common Populations: Pediatric or nursing home patients
Lab Handling: Usually not reported unless contamination impedes analysis
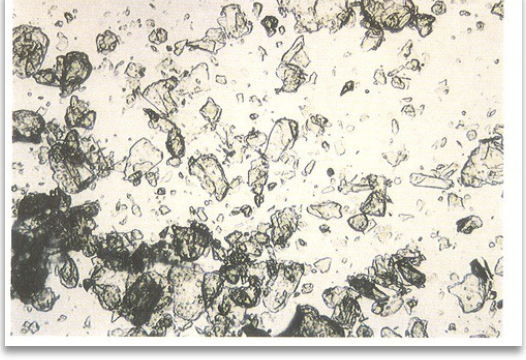
Talcum Powder (Artifact)
Appears as flat sheets
May be confused with cholesterol or other crystals
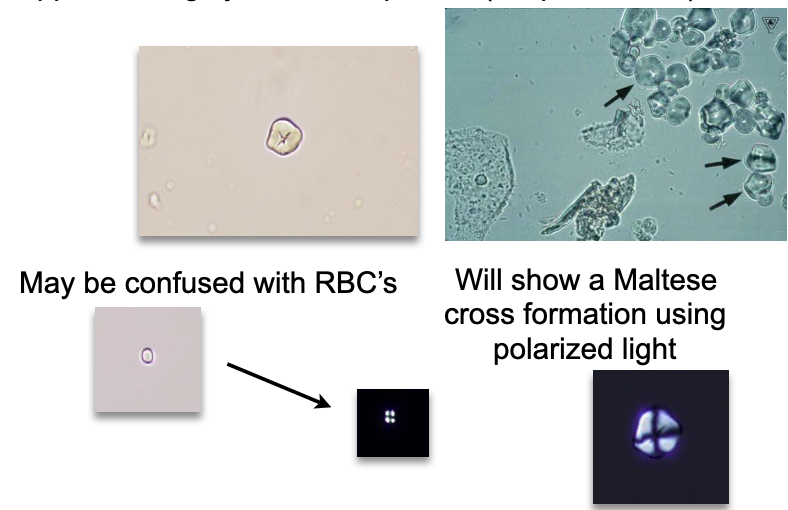
Starch (Artifact)
Highly refractile spheres with dimpled center
May be confused with RBCs
Shows a Maltese cross under polarized light
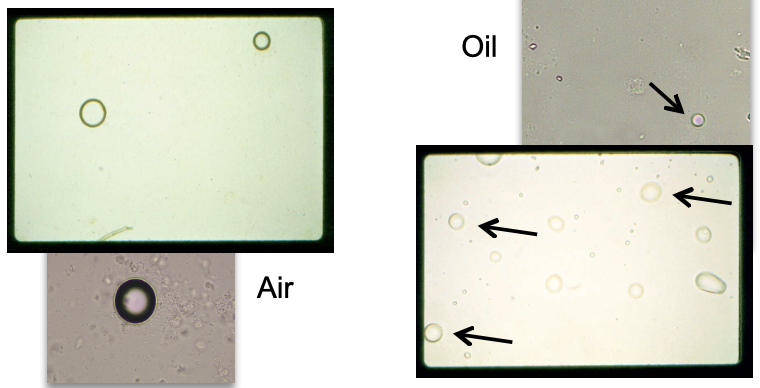
Oil Droplets / Air Bubbles (Artifact)
Highly refractile, spherical objects
May mimic RBCs under light microscopy
Oil tends to float; air bubbles may have a dark edge or central refractile ring
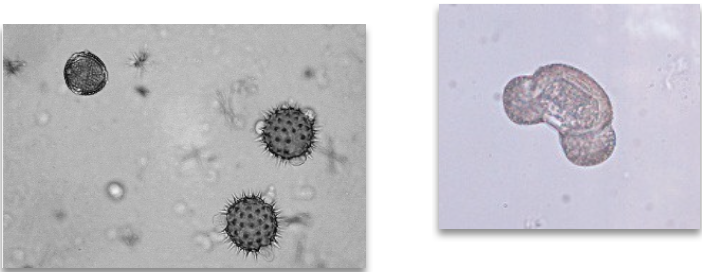
Pollen Grains (Artifact)
Large, spherical with distinct cell wall
Often contain concentric circles
Morphology may vary (can appear spiked or lobulated)
May be mistaken for parasitic ova or other large cells
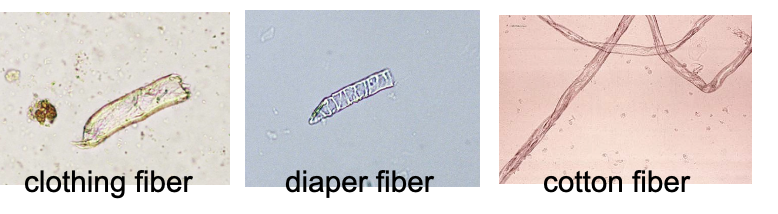
Hair and Cloth Fibers (Artifact)
May mimic casts or parasites
Types: clothing, diaper, cotton fibers
Key distinguishing traits:
• Highly refractile
• Lack cast outlineCareful observation under light microscopy essential
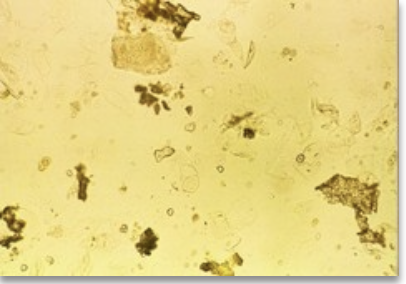
Fecal Contamination (Artifact)
Source:
• Improper collection (especially in infants)
• Entero-urinary fistulasMicroscopy:
• Irregular debris resembling plant material, meat fibers, or other gut contentsInterpretation tip:
• Consider patient age and clinical history
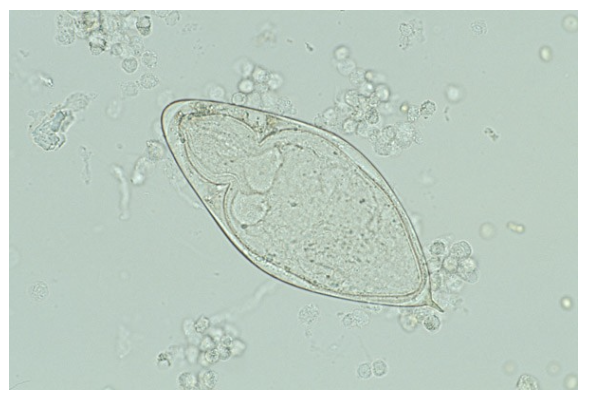
Schistosoma haematobium (Parasite)
Type: Trematode (fluke)
Habitat: Bladder venous plexus
Egg morphology: Oval with terminal spine
Clinical relevance:
• Associated with hematuria, bladder inflammation
• Risk factor for squamous cell carcinoma of the bladderDiagnosis: Microscopic ID of eggs in urine (not stool)
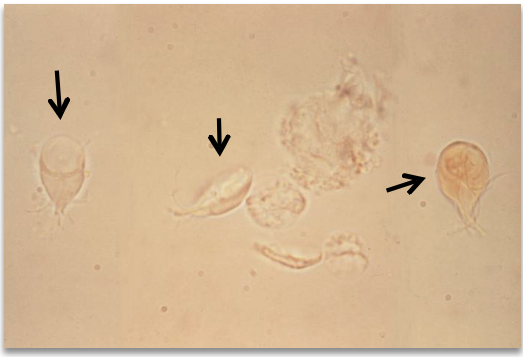
Trichomonas vaginalis
Most common urinary parasite
Pear-shaped flagellate with undulating membrane
Motile in fresh specimens
Non-motile forms mimic WBCs or epithelial cells
Confirm via patient history or video microscopy
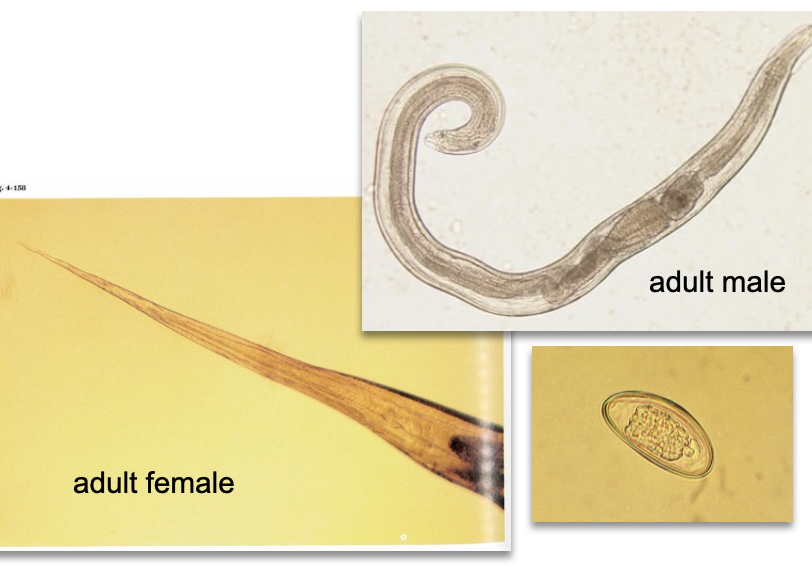
Enterobius vermicularis (Pinworm)
Intestinal nematode
Eggs or worms enter urine via fecal contamination
Most common in children
Oval, flattened eggs with a thick shell
Contextual Note: Not a true urinary parasite—presence indicates contamination or fistula.
Giardia lamblia
Intestinal protozoan
Pear-shaped with flagella and two nuclei ("face")
Rare in urine; enters via fecal contamination
Often mistaken for debris or epithelial cells
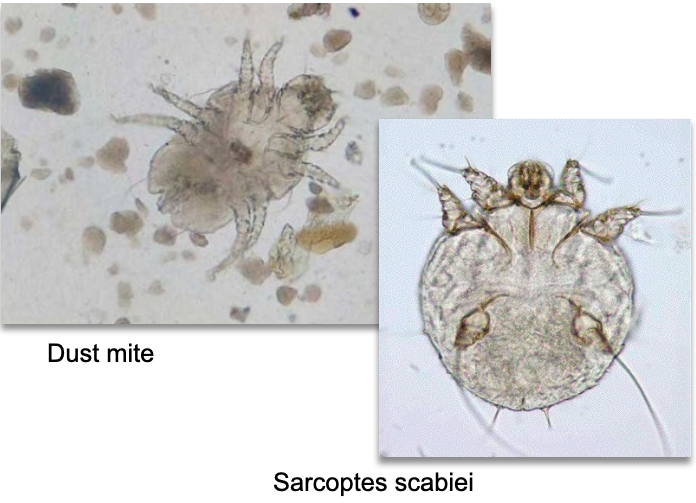
Mites (Urine Contaminants)
External skin parasites (e.g., Sarcoptes scabiei, dust mites)
Entry into Urine: Contamination
Note: Dust mites often environmental; scabies mites may indicate true infestation