Exam 2 (Everything but Renal)
1/181
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
182 Terms
What is shock?
A life-threatening medical condition that results from inadequate tissue perfusion.
It is not a disease itself, but rather the possible consequences of many diseases.
It is a systemic response to an illness/injury that leads to a cascade of events with a potentially fatal outcome.
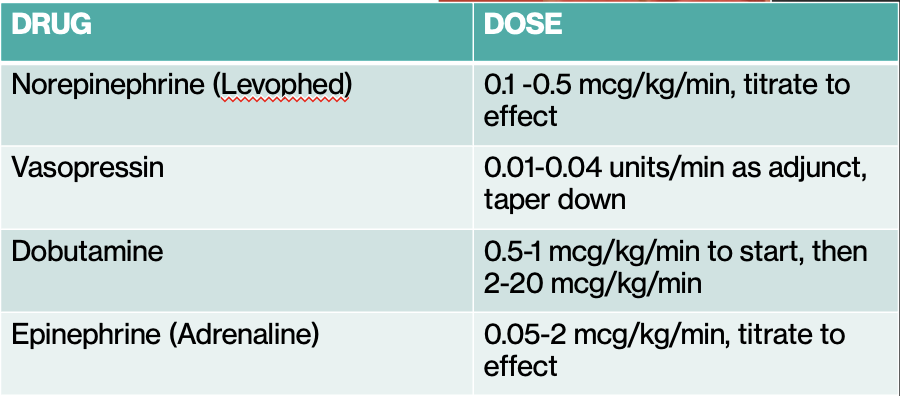
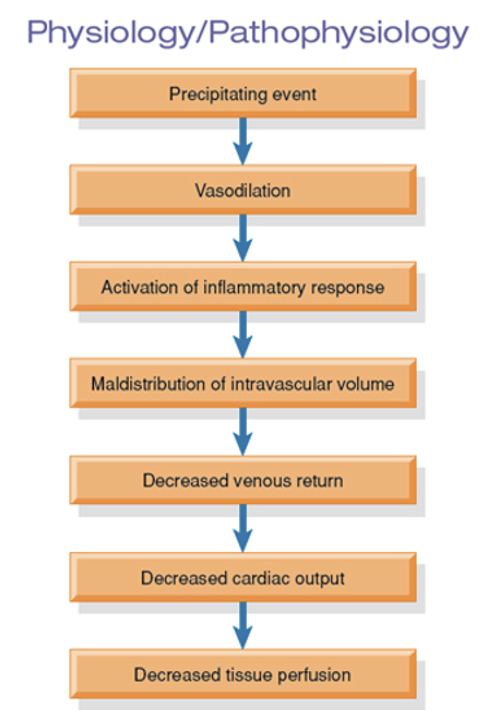
Regulatory Mechanisms in Shock (image)
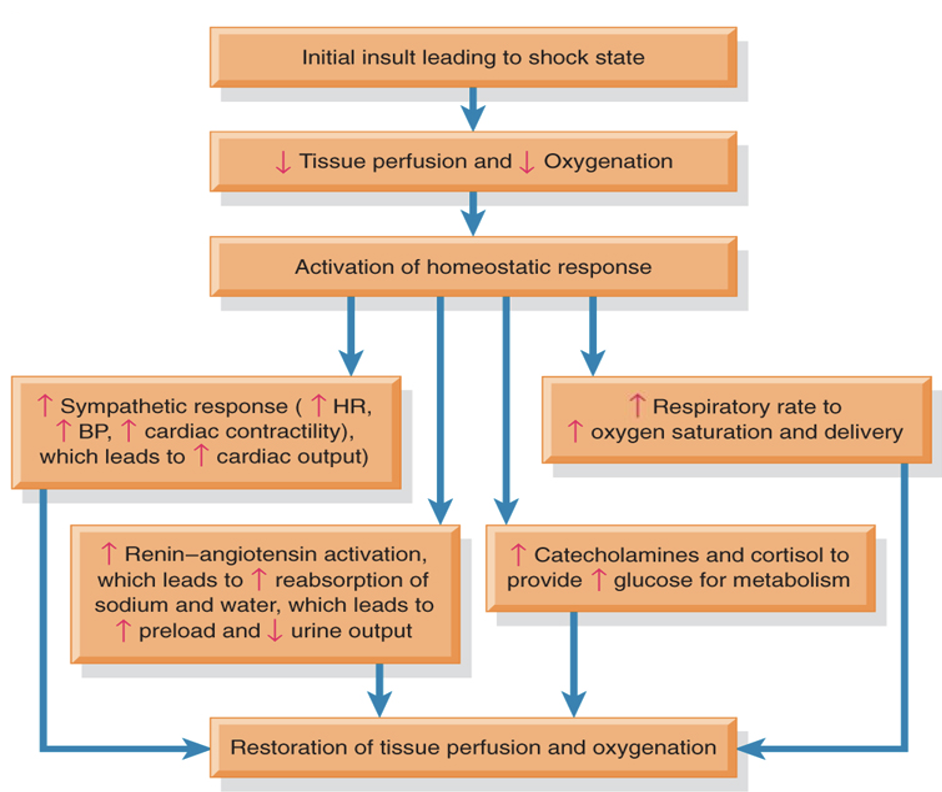
Pathophysiology of Shock (image)
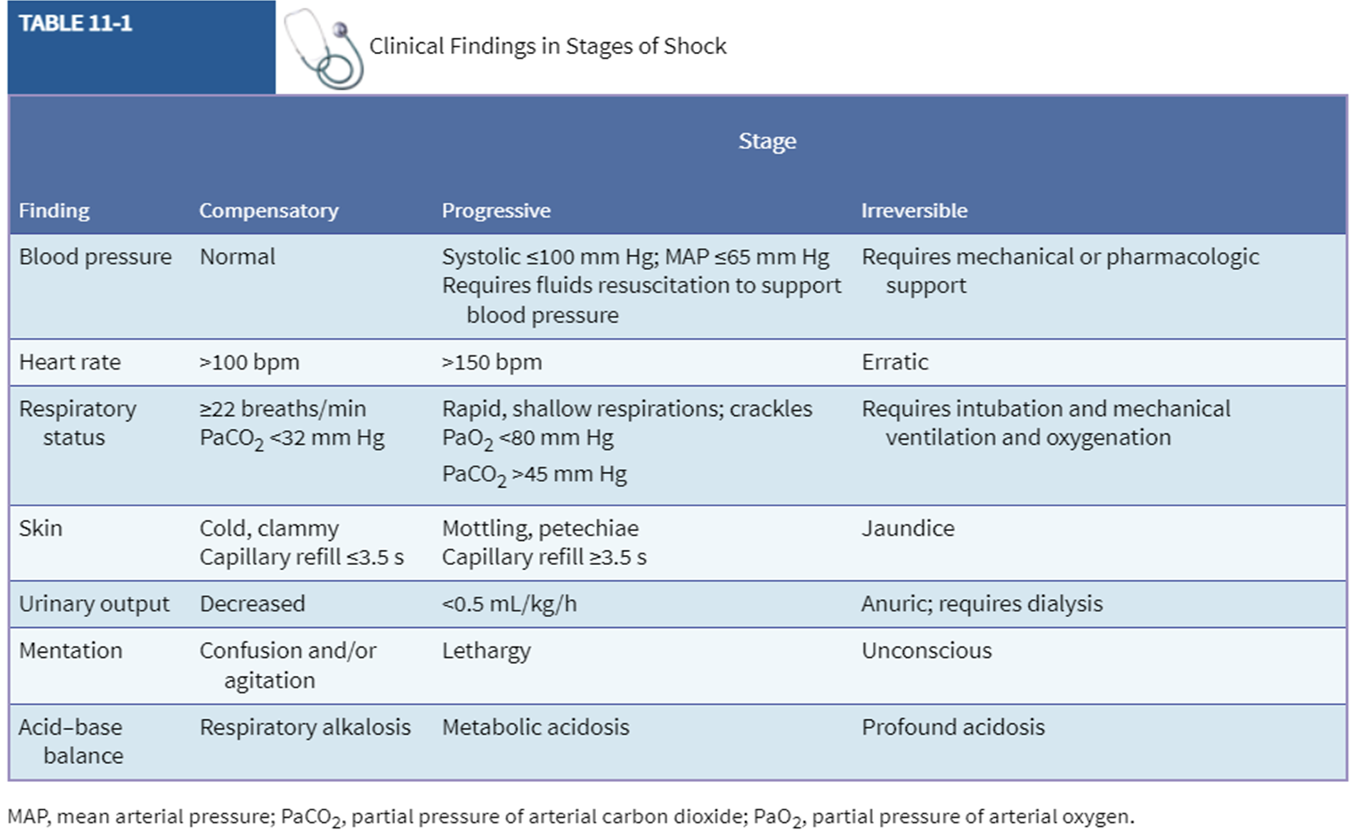
What are the Stages of Shock?
Initial Insult
Compensatory Stage—compensation
Progressive Stage—decompensation
Irreversible Stage—refractory (unresponsive to treatment)
Initial Insult: What are potential sources of shock?
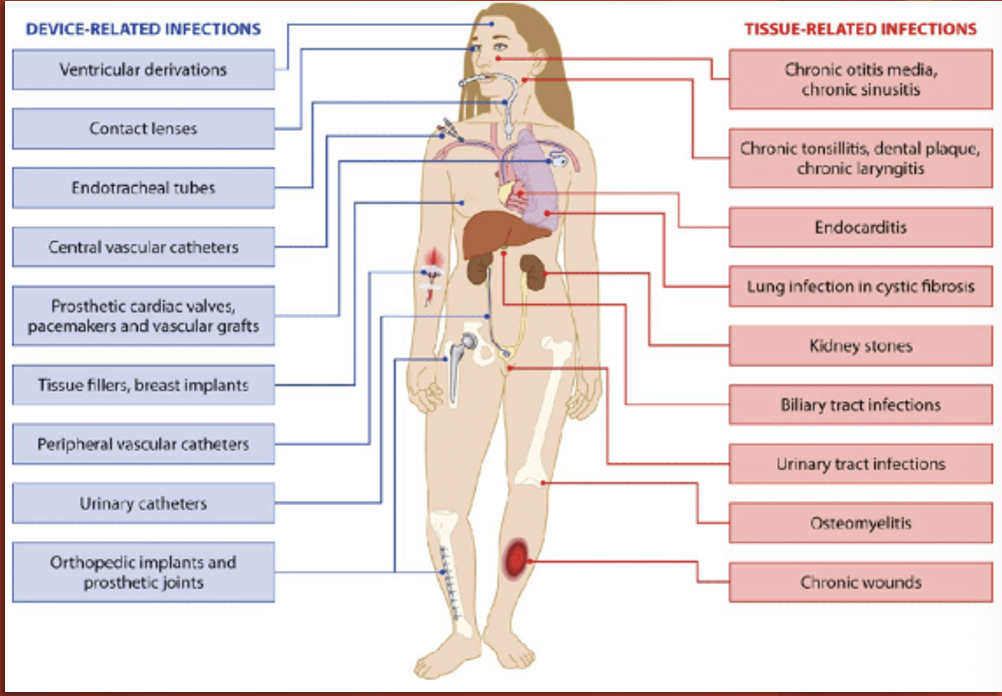
Infection
Trauma
Blood loss
Dehydration
Hyperthermia
Allergic reaction
Poisoning
SCI
MI
Burns
Each of these can lead to decreased cardiac output of blood circulation and begin the cascade toward a shock state.
Compensatory Stage—Systemic Actions: What does the body do?
Tries to increase supply to meet demand
Sympathetic nervous system activated
Renin-Angiotensin-Aldosterone (RAA) system activated
Glucocorticoids released
Blood flow decreases to non-vital organs
Compensatory Stage: Clinical Manifestations
Relatively normal BP
Tachycardia
Tachypnea
Decreased PaCO2
Diaphoresis
Cool or clammy skin (except in certain distributive shocks)
Decreased UOP
Hypoactive bowel sounds
Increased serum glucose
What are the 3 ways compensation is measured?
Mentation
Blood Pressure
Pulse Oxygenation
Progressive Stage—Systemic Actions: What does the body do?
Overworked heart can’t meet body’s requirements, becomes ischemic and fails.
Microcirculation regulation fails, leading to widespread capillary permeability.
Prolonged tissue hypoxia leads to acidosis and cellular dysfunction.
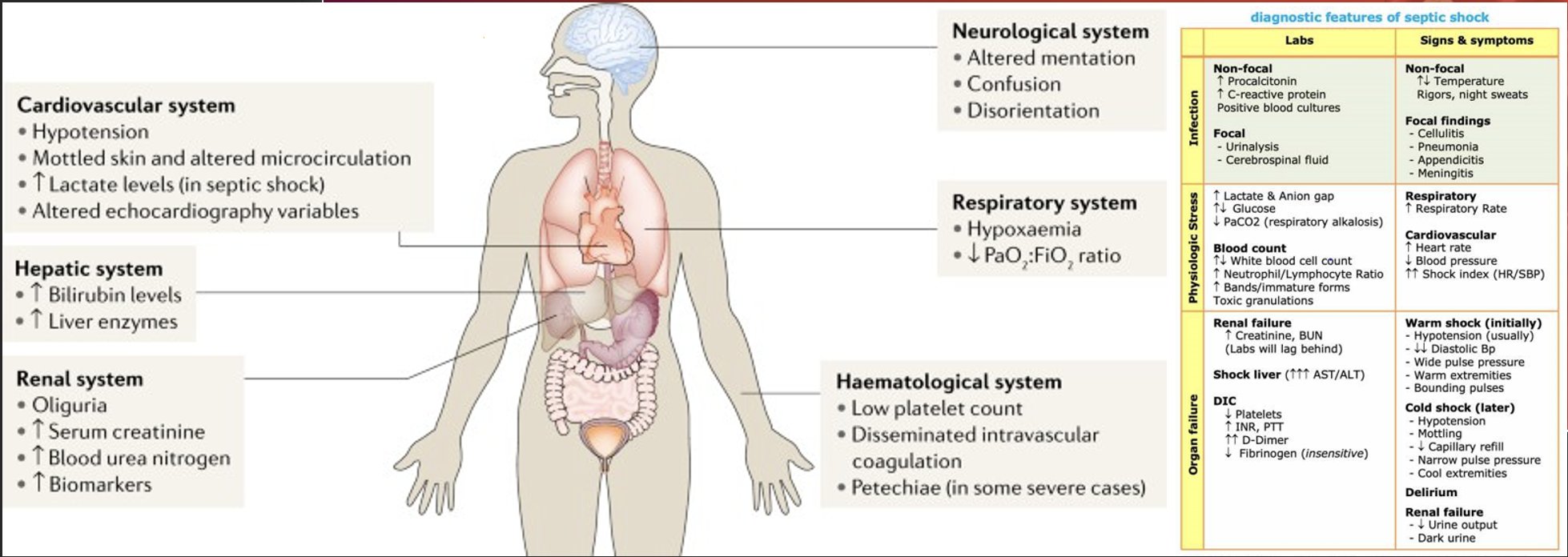
Progressive Stage: Clinical Manifestations
Hypotension (this is a late sign!)*
Tachycardia/tachypnea
Pulmonary edema/crackles
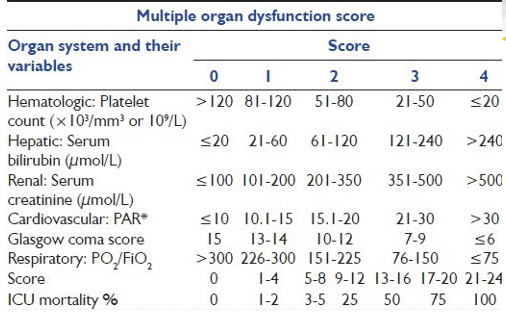
Multiple Organ Dysfunction Syndrome (MODS)**
Altered mental status
AKI (oliguria/anuria)
GI ischemia (ulcers/bloody diarrhea)
Abnormal hemostasis (increased clotting times, bruises/petechiae)
*Low B/P indicates prolonged tissue ischemia and poor prognosis. We must intervene before this develops.
Multiple Organ Dysfunction Syndrome (MODS)
Changes in other systems besides the initial area…
Respiratory P/F ratio < 250 w/o pneumonia, or < 200 w/ pneumonia
MAP < 65 mmHg, SBP < 90 mmHg, or SBP decrease > 40 from baseline
Creatinine > 2 mg/Dl
UOP < 0.5 mL/kg/hr in 6 hours or < 400 mL in 24 hours.
Bilirubin > 2 mg/dL
Platelets <100,000/mm3
INR > 1.5 or aPTT > 60 secs
Lactate > 2 mmol/L
Irreversible Stage—Systemic Actions: What does the body do?
MODS progresses to total organ failure
Liver and kidneys fail, leading to significant metabolic acidosis
BP stays low despite treatment
Survival is unlikely
Irreversible Stage: Clinical Manifestations
Significantly diminished cardiac output
Pale, cyanotic, or yellowish skin
Anuria
Disseminated Intravascular Coagulation (DIC)
Coma
Death
Disseminated Intravascular Coagulation (DIC)
Definition:
Inappropriate coagulation occurs within the blood vessels
Endothelial damage triggers clotting cascade and widespread clot formation
Systemic over-consumption of clotting factors
Clotting factors get used up and patient develops uncontrollable bleeding
Causes:
Not fully understood, but it’s most often associated with sepsis, severe infections, trauma, cancer, and obstetric complications.
Never the primary issue/disease; occurs in response to another disease process or injury.
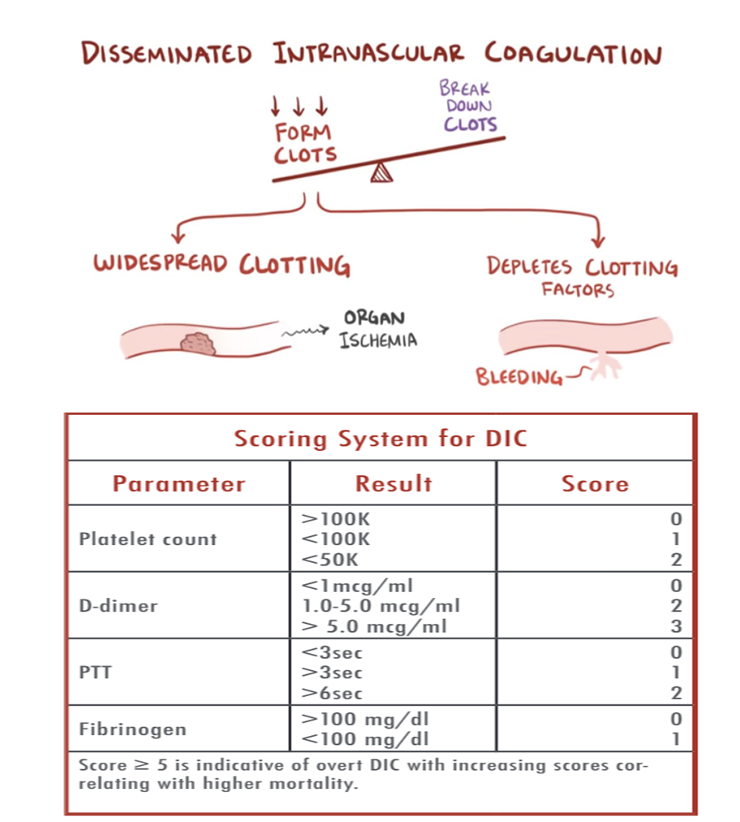
Some assessment findings on a patient with DIC
Blood leaking from around their IV sites
Bloody noses occurring often
Gums bleeding very easily
Pink tinges in their urine
Dark tarry stools
Petechiae, ecchymosis, bruising
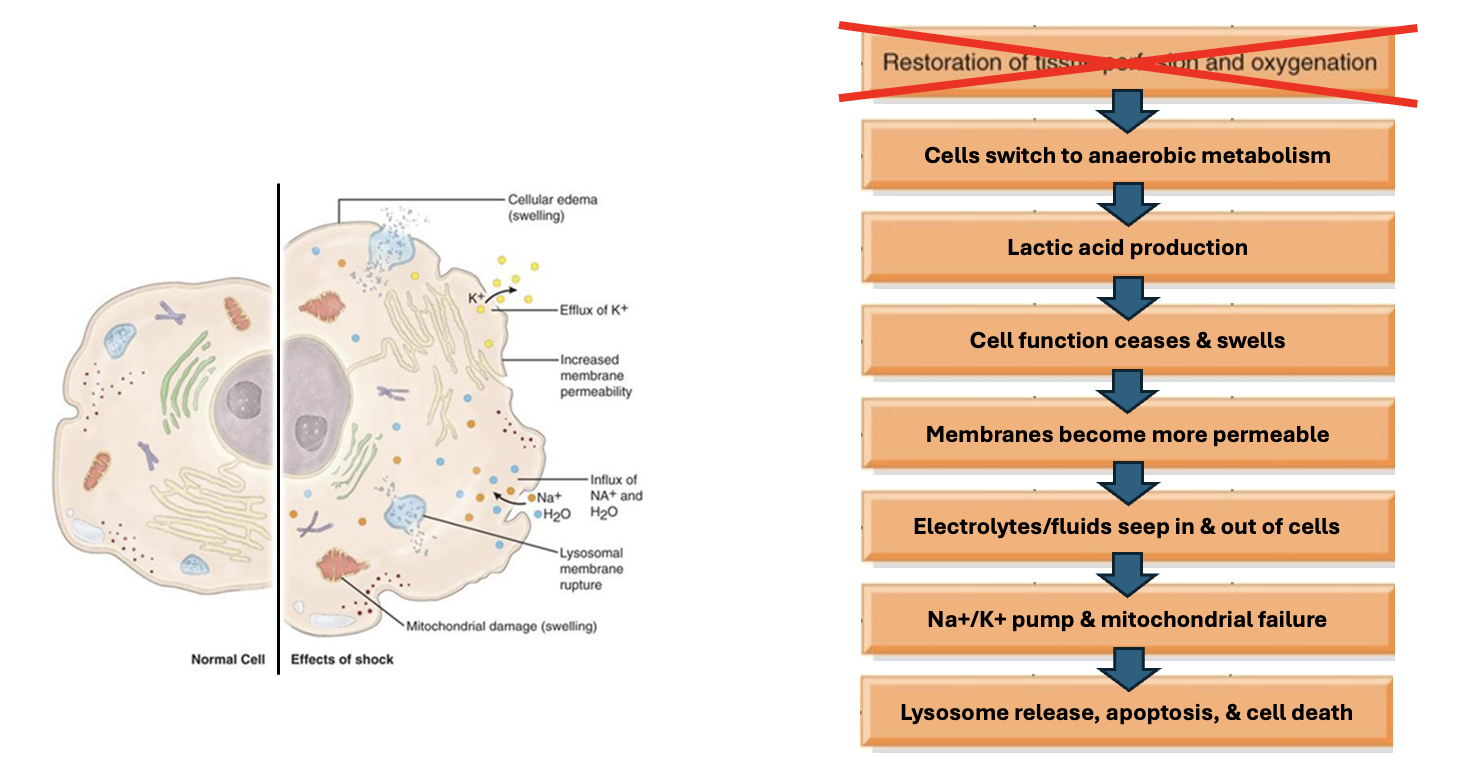
Clinical Findings in Shock (image)
Shock in General: Initial S/Sx
Tachycardia
Tachypnea/shortness of breath
Decreased blood pressure
Delayed capillary refill
Pale, cyanotic, cool, or clammy skin
Decreased urine output
Weakness/lethargy
Dizziness/lightheadedness
Altered level of consciousness
What are the 4 types of Shock?
Hypovolemic
Cardiogenic
Obstructive
Distributive
Hypovolemic Shock
Decreased intravascular volume due to fluid loss.
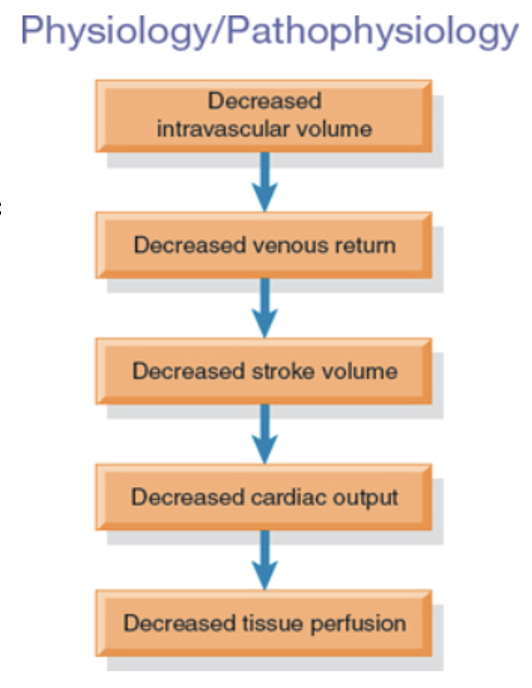
Hypovolemic Shock: Causes
External bleeding (trauma)
Internal bleeding (GI or bleeding disorders)
Burns
Diarrhea/vomiting
Dehydration
Diuresis (such as via hemodialysis)
Diabetes insipidus

poor skin turgor; thirst
In addition to the common signs and symptoms of shock, a patient in hypovolemic shock may exhibit ____ ____ ______ and ______.
Hypovolemic Shock: Primary Treatment Goals
Find the source and stop it! (#1)
Replace lost intravascular volume.
Redistribute fluid volume.
Cardiogenic Shock: Causes
Myocardial infarction (#1)
Heart failure
Dysrhythmias
Coronary artery disease
Cardiomegaly
Myocarditis
Cardiac valve disorders
Drug toxicity
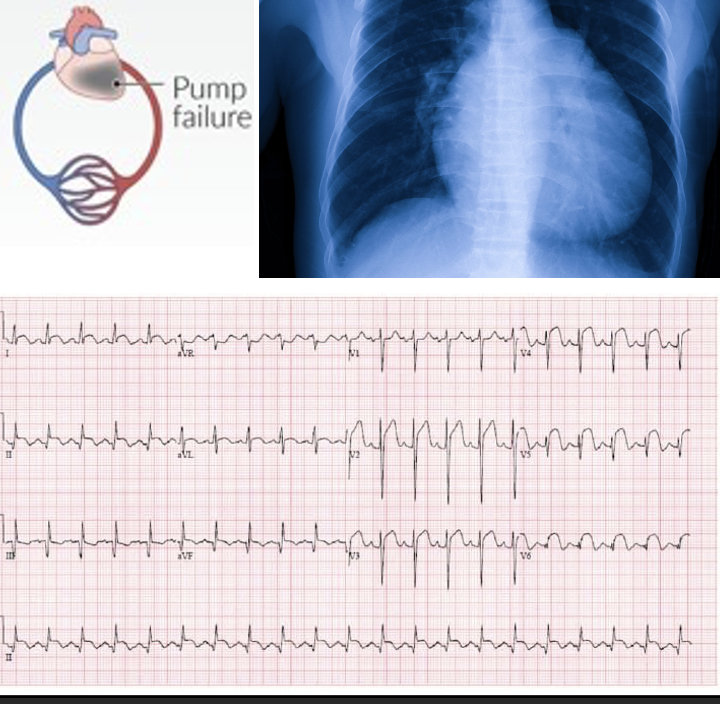
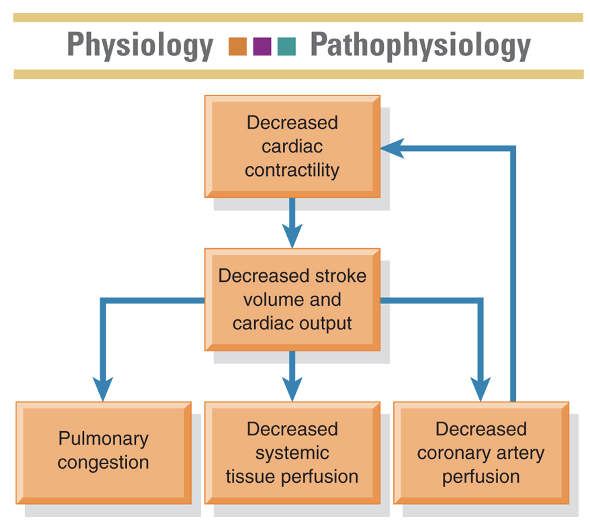
Cardiogenic Shock
Impairment or failure of the myocardium
crackles in lungs; chest pain
In addition to the common signs and symptoms of shock, a patient in cardiogenic shock may exhibit _______ __ _____ and _____ ____.
Cardiogenic Shock: Primary Treatment Goals
Restore tissue perfusion (including to the heart itself)
Improve cardiac contractility
Manage other organ dysfunction
Obstructive Shock
Inability of the heart to fill properly
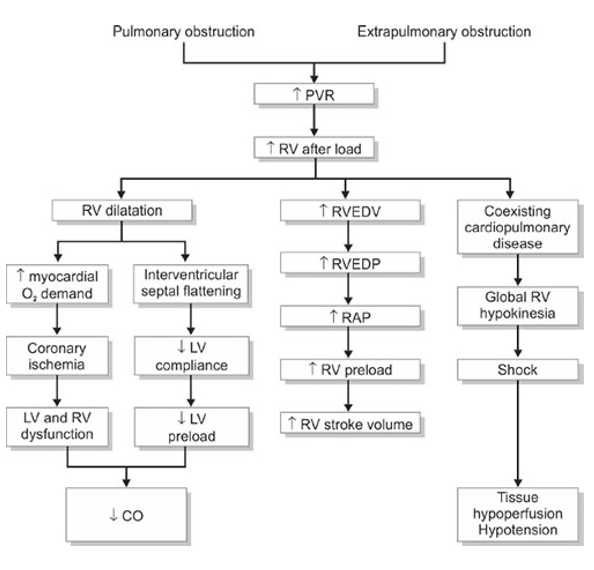
Obstructive Shock: Causes
Pneumothorax
Cardiac Tamponade
Pulmonary embolism
Pulmonary hypertension
Aortic dissection
Restrictive cardiomyopathy
Tumors
Sickle Cell Disease
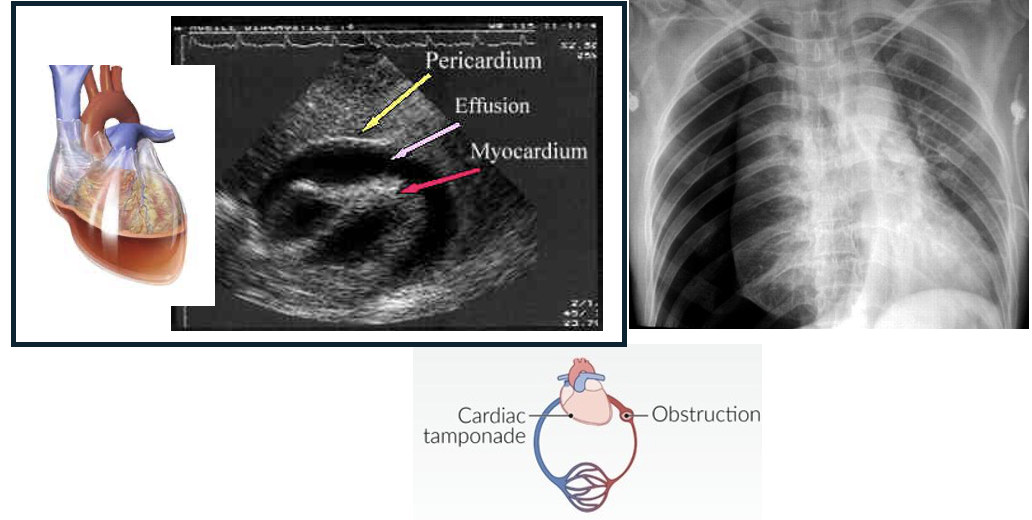
Chest or abdominal pain
Distended jugular veins
Muffled heat sounds (in cardiac tamponade)
Unequal peripheral pulses (in aortic dissection)
In addition to the common signs and symptoms of shock, a patient in obstructive shock may exhibit:
Obstructive Shock: Primary Treatment Goal
Remove the obstruction!
Distributive Shock
Loss of sympathetic vasomotor tone/ “maldistribution of blood flow”
is marked by systemic vasodilation that leads to increased capillary permeability and decreased blood flow to the brain, heart, and kidneys, causing damage to vital organs.
Distributive Shock: Causes
Sepsis (#1)
Neurological dysfunction
Spinal cord injury (SCI)
Anaphylaxis
Hypersensitivity reaction
Effects of medication
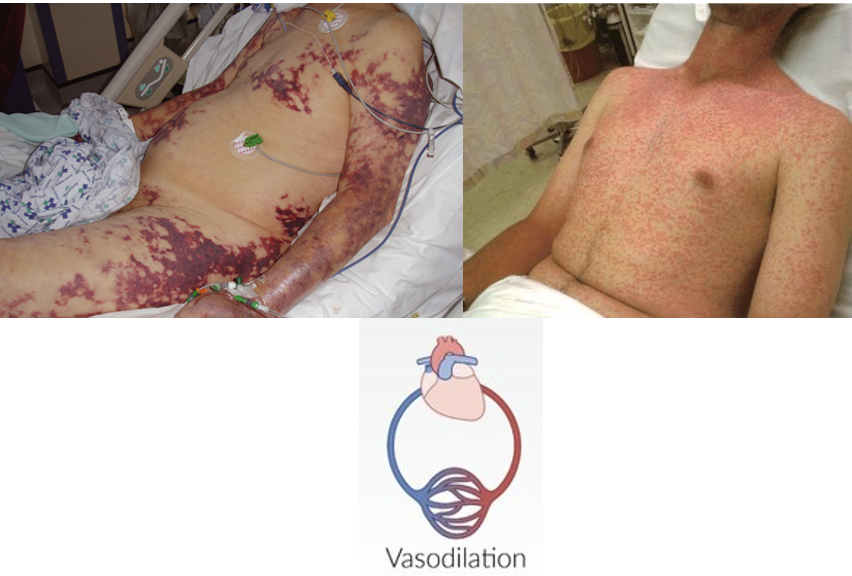
Warm or flushed skin
Blood sits/hangs out in vessels longer than normal due to the widespread vasodilation…
Other symptoms depend on the type of distributive shock the patient is experiencing
In addition to the common signs and symptoms of shock, a patient in distributive shock may exhibit:
Distributive Shock: Primary Treatment Goals
Restore sympathetic tone
Reverse the cause
Support BP, pulse, and respirations
Types of Distributive Shock
Neurogenic Shock
Anaphylactic Shock
Septic Shock
Neurogenic Shock
Is a life-threatening condition in which the central nervous system becomes damaged, leading to loss of vascular tone, widespread vasodilation, and dangerously low blood pressure.
Pathophysiology:
Damage to the sympathetic nervous system allows the parasympathetic system to take over unopposed, often leading to bradycardia and worsening cardiac output.
Intravascular volume remain the same, but vasodilation and bradycardia combine to create hypoxic state.
Causes:
Spinal cord injury (SCI) is the most common cause, but other causes can include:
Spinal anesthesia
Autoimmune disorders, such as Guillain-Barre Syndrome or Transverse Myelitis
Severe stroke
Meningitis
Anaphylactic Shock
Is a life-threatening condition in which the body’s immune system overreacts to an allergen, causing rashes, hives, itching, edema, and if left untreated, severe hypotension and airway obstruction.
Pathophysiology:
Allergens bind to IgE, which triggers a massive release of histamine from mast cells and basophils. Histamine then causes widespread vasodilation and capillary permeability, leading to hypotension and loss of intravascular fluid.
Histamines, along with prostaglandins and leukotrienes, cause smooth muscle contraction in the airways, limiting ventilation.
Causes:
Can be caused by any numbers of potential allergens, differing from person to person.
Medications (antibiotics, NSAIDs, contrast dye, ACE inhibitors)
Foods (nuts, fruits, shellfish, milk)
Insect stings (bees, wasps, hornets)
Latex
General Treatment of Shock: Early Identification
ABCs
Assess and report subtle changes:
LOC, UOP, skin tone, cap refill
Vital Signs:
HR, RR, BP, MAP, Temp, SpO2
Note and report concerning lab trends
Initiate timely treatment
Correct precipitating event
General Treatment of Shock: Establish Adequate Tissue Perfusion
Promote adequate cardiac output:
Restore intravascular volume (fluid replacement)
Restore vasomotor tone (vasoactive medications)
Ensure adequate oxygenation
General Treatment of Shock: Restore Normal Cell Function
Establish proper acid-base balance
Provide nutritional support
Use of antacids, PPIs, or H2 antagonists to prevent GI injury
Short-term, mild hyperglycemia may be acceptable (140-180)—Permissive hyperglycemia
We don’t want them in a hypoglycemic state because their body needs enough glucose to recover from this shock state.
General Treatment of Shock: Monitor Labs
Lactate levels
Complete metabolic panel (CMP)—for electrolyte balances
Complete blood count (CBC)—for blood cell counts, including WBCs and platelets
Blood cultures (if an infection is suspected)
Base deficit and anion gap
ABGs
Signs of MODs**
General Treatment of Shock: Monitor Hemodynamics
Blood pressure:
MAP is generally the guiding factor (desired > 65 mmHg)
Continuous monitoring (VS/ECG)
Other measurements as warranted (PP, CVP, etc.)
General Treatment of Shock: Provide Psychosocial Support
Provide emotional support and help reduce anxiety
Communication with the patient and family members, including education about condition
Care plan may include end-of-life issues and/or grief counseling
General Treatment of Shock: Provide Advanced Supportive Care as Needed
May include intubation, ventilation, dialysis, etc.
General: Fluid Replacement
Fluid Challenge: 500 to 1,000 mL bolus of isotonic crystalloid
One-time bolus to see how the patient does…
Aggressive Fluid Resuscitation: 30 mL/kg (using IDEAL body weight)
Long continuous bolus
Crystalloids for IV treatment of shock: (they’re more acidic!)
0.9% saline (Normal Saline Solution)—super cheap!
Lactated Ringer’s (closely mirrors regular blood plasma)—more $$
*Rule of Thumb: The best fluid is the fluid that’s readily available!
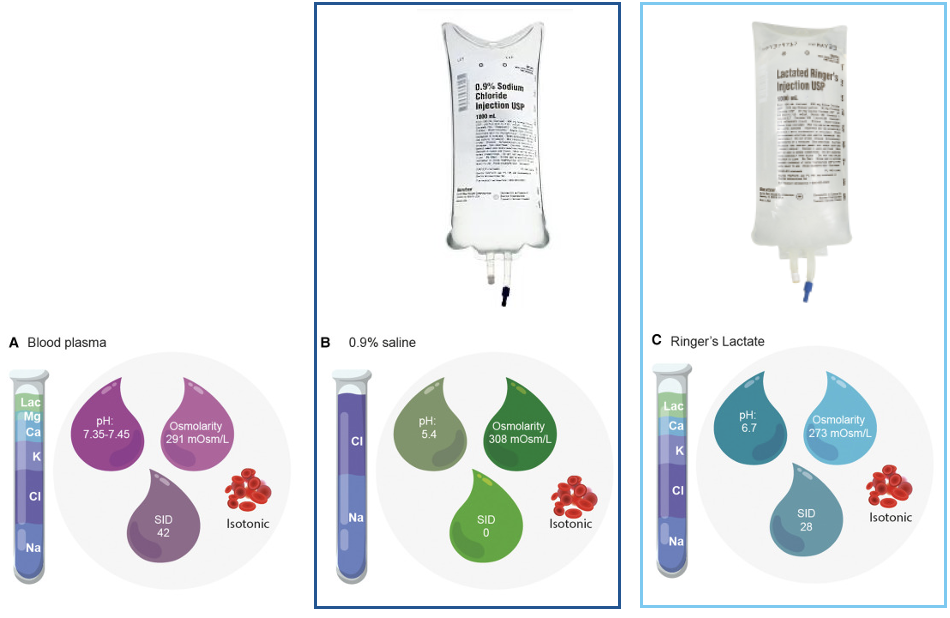
Why isn’t D5W included on the list for IV fluid treatment for shock?
D5W sitting in the bag is isotonic. The second it enters your body it’s not isotonic anymore because your body grabs onto the dextrose and uses it → converts it into sugar, and you’re just left with water, which is hypotonic.
General: Fluid Replacement (Alternative or Adjunctive)
The following solutions can be use in special cases of shock, especially when isotonic crystalloids are not available or sufficient. However, they are NOT first-line therapies.
Hypertonic solution for IV fluid treatment of shock:
3% Sodium Chloride (HSS)
Can only be administered once or else you’re going to give them hypernatremia.
Good for patients who have edema, increased ICP
Colloids for IV fluid treatment of shock:
Albumin—large protein molecule
Dextran—large sugar molecule
**essentially pulling more fluids back into the vasculature

Fluid Replacement in Shock (image)
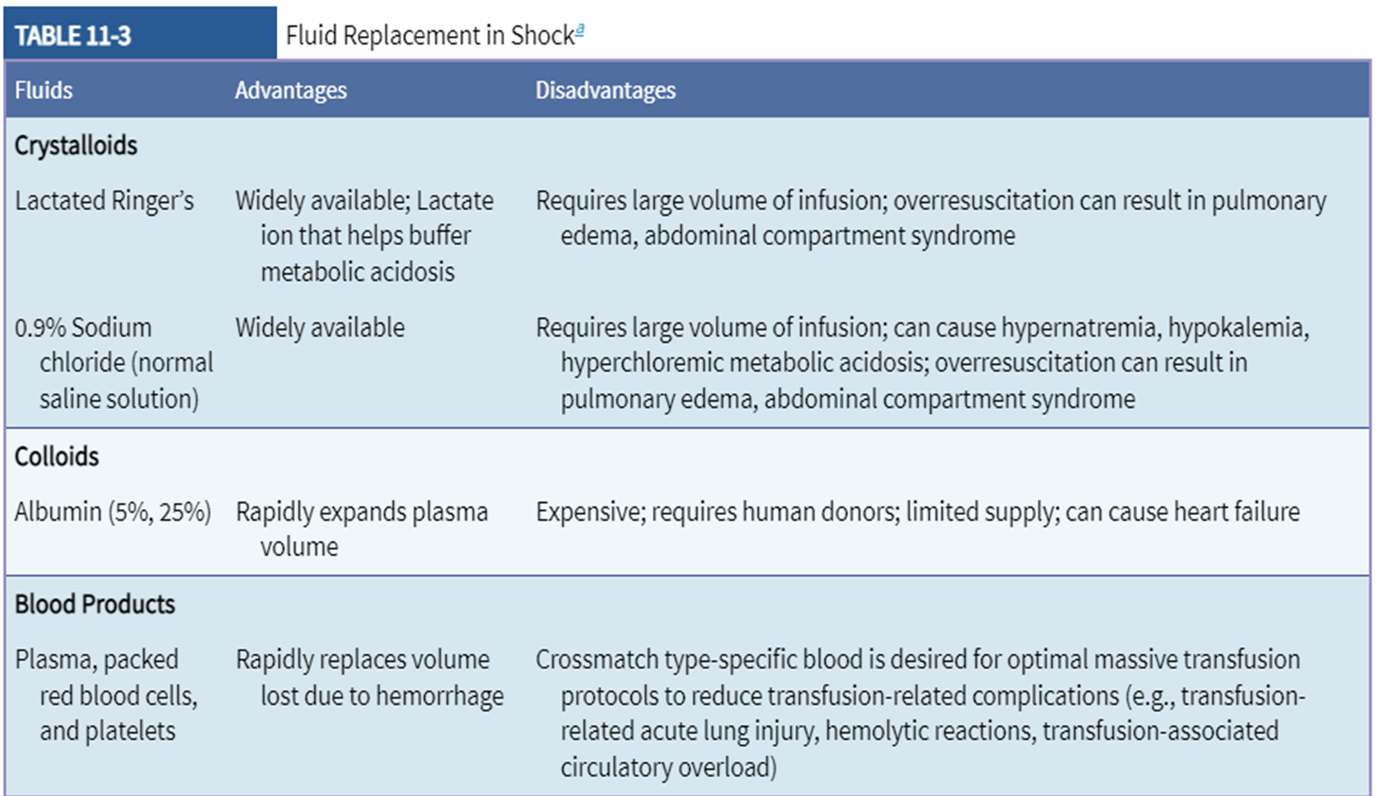
Complications of Fluid Replacement
Fluid administration can be a double-edged sword, both helpful and harmful. Close monitoring is essential to patient safety!
We need to avoid under resuscitating and over resuscitating.
Insufficient fluid replacement = higher incidence of morbidity and mortality due to lack of tissue perfusion.
Excessive fluid administration = higher incidence of morbidity and mortality due to multiple side effects:
Acute Lung Injury (ALI)
It’s basically pulmonary edema because a bunch of fluid is dumped into the patient and the fluid goes the wrong way (alveoli instead of blood vasculature)-this is why a fluid challenge is done!
Abdominal Compartment Syndrome (ACS) and/or Intra-abdominal hypertension (IAH)
similar to ascites
Multiple Organ Dysfunction Syndrome (MODS)
Hypothermia* (fluid = room temp 72F; patient = 98.6F)
Acidosis*
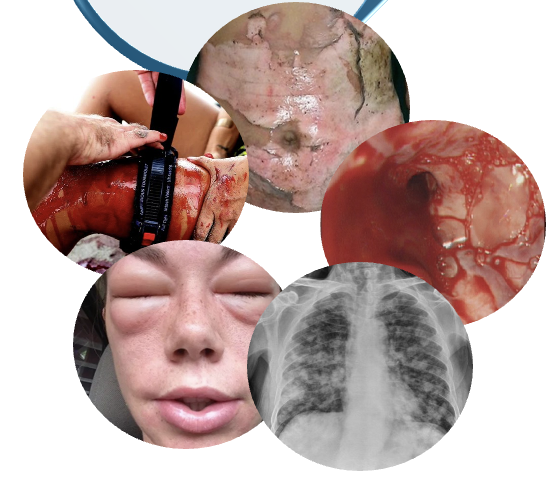
General: Vasoactive Medications
These medications are used when fluid therapy alone does not maintain MAP.
Dosages are often based on patient weight and titrated to patient response (mcg/min or mcg/kg/min)
Continuous monitoring is a must!
These medications should be administered in a central line to avoid extravasation and tissue necrosis.
The meds can be started in a peripheral, but eventually need to be moved to central asap.

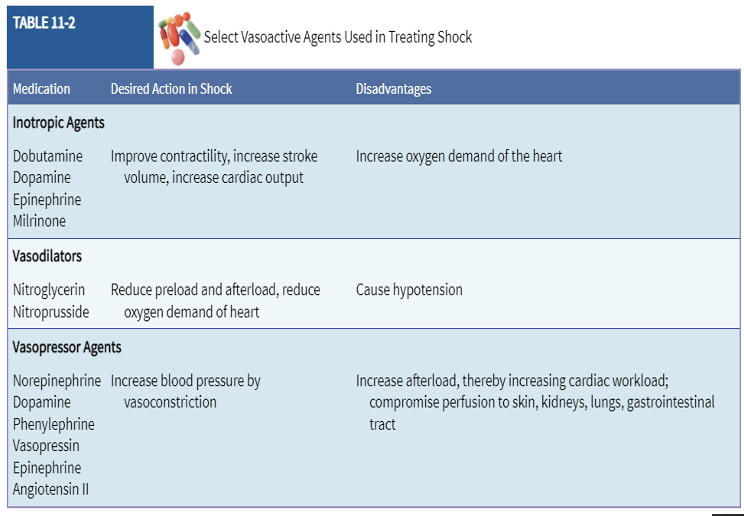
Select Vasoactive Agents Used in Treating Shock (image)
General: Nutritional Therapy
Catabolic process body breaks down lean muscle, so nutritional support is key.
Enteral nutrition (via the GI tract) is preferred, but parenteral nutrition (via central line) can be given if the patient has GI impairment.
Caloric intake may start off slowly due to fragile state of body (~12.5 kCal/kg), but as the body recovers, caloric intake is slowly increased to ~20-25 kCal/kg.
low → up
Protein intake is important—Shock patients should receive roughly 1.3 g/kg/day rather than the usual recommendation of 0.8 g/kg/day.
up → down
Nutrition includes carbohydrate (dextrose), amino acids, lipids, electrolytes, vitamins, trace elements (zinc, copper, manganese, selenium, etc.), and water. ← (TPN)
Administration of protective meds (antacids, H2 blockers, PPIs) are also important to prevent peptic ulcer formation.
Hypovolemic Shock: Potential Treatment Strategies
Surgical intervention to control bleeding (#1)
IV fluid resuscitation with isotonic crystalloids
Blood transfusion (generally if Hgb < 7 g/dL)*—varies by institution
Hypovolemic Shock Treatment: Blood Transfusions
Indicated in episodes of significant blood loss (Hgb < 7 g/dL).
Generally administered over 2 to 4 hours, unless its emergent, where it is given as rapidly as possible (use large gauge IV).
Time permitting, patient’s blood should be typed and crossmatched.
In an emergency, type O negative blood may be used.
Blood products may include whole blood, PRBCs, FFP, and platelets:
Rule of thumb: 1 unit of PRBCs should raise Hgb by 1 g/dL.
Severity of blood loss dictates how much the patient receives.
Massive transfusion protocol (MTPs) utilize varying ratios of PRBCs, FFP, and platelets (ex. 4:2:1, 2:1:1, or 1:1:1)
Monitor for transfusion reactions*:
Vital signs (including temperature)
SOB, increased WOB, adventitious lung sounds
Altered mental status
Hives/rash, flushing, back pain (wheezing)
**Should any undesirable symptoms occur, the first thing to do is stop the infusion!

Cardiogenic Shock: Potential Treatment Strategies
Thrombolytics, PCI, Stents, or CABG (for coronary artery occlusion)
Medications (for dysrhythmias or electrolyte imbalances)
Mechanical assistive devices (IABP, Impella, LVAD, or ECMO)
Use fluids with extreme caution.
Obstructive Shock: Potential Treatment Strategies
Fibrinolytics and DOACs (for PE)
Surgical intervention (for PE, tumors, aortic dissection, or splenic sequestration)
Needle decompression/chest tube (for pneumothorax)
Pericardiocentesis (for cardiac tamponade)
Medications (HTN meds for restricted cardiomyopathy or PH)
Use fluids with extreme caution
It’s not a volume problem. The fluids are being obstructed/backed up and adding more fluids can back it up even more, so be cautious!
Distributive Shock: Neurogenic Shock—Potential Treatment Strategies
Spinal stabilization and surgery
Atropine (for bradycardia)
DVT or VTE prophylaxis (LMWH)
Distributive Shock: Anaphylactic Shock—Potential Treatment Strategies
Remove causative agent
Medications (IM epinephrine 1:1000, B2 agonists, antihistamines, corticosteroids)
Hemodynamic Monitoring
The use of technology to provide quantitative information about a patient’s vascular capacity, fluid volume, pump effectiveness, and tissue perfusion.
Gives us insights into the patient’s preload, afterload, and/or SVR.
Used to guide their plan of care.

Volumes, Pressures, & Saturations: Cardiac Output
CO = Stroke volume (SV) x heart rate (HR)
Normal range = 4-8 L/min
Stroke volume is determined via echocardiography
Volumes, Pressures, & Saturations: Blood Pressure (BP)
Systolic blood pressure (SBP):
Normal range = 100-140 mmHg
Diastolic blood pressure (DBP):
Normal range = 60-90 mmHg
Usually measured via NIBP cuff readings, but arterial lines are most accurate.
Pulse Pressure (PP)
PP = SBP - DBP
Normal range = 40-60 mmHg
Wide pulse pressure (< 60 mmHg) usually indicates arteriosclerosis, atherosclerosis, or aortic regurgitation.
*Narrow pulse pressure (< 40 mmHg) can be an indicator of shock from decreased CO or increased SVR.*
Mean Arterial Pressure (MAP)
MAP = DBP + 1/3(SBP - DBP)***
Normal range = 70-100 mmHg
Most accurate estimate of organ perfusion
MAP below 65 mmHg in adults is associated with multi-organ failure
Volumes, Pressures, & Saturations: Saturation of Peripheral Oxygen (SpO2) and Saturation of Arterial Oxygen (SaO2)
Normal range = 95-100%
Volumes, Pressures, & Saturations: Central Venous Oxygen Saturation (ScvO2)
Normal range = 70-80%
Volumes, Pressures, & Saturations: End-Tidal Carbon Dioxide (EtCO2) and Arterial Pressure of Carbon Dioxide (PaCO2)
Normal range = 35-45 mmHg
Volumes, Pressures, & Saturations: Urine Output (UOP)
Normal range = > 0.5 mL/kg/hr
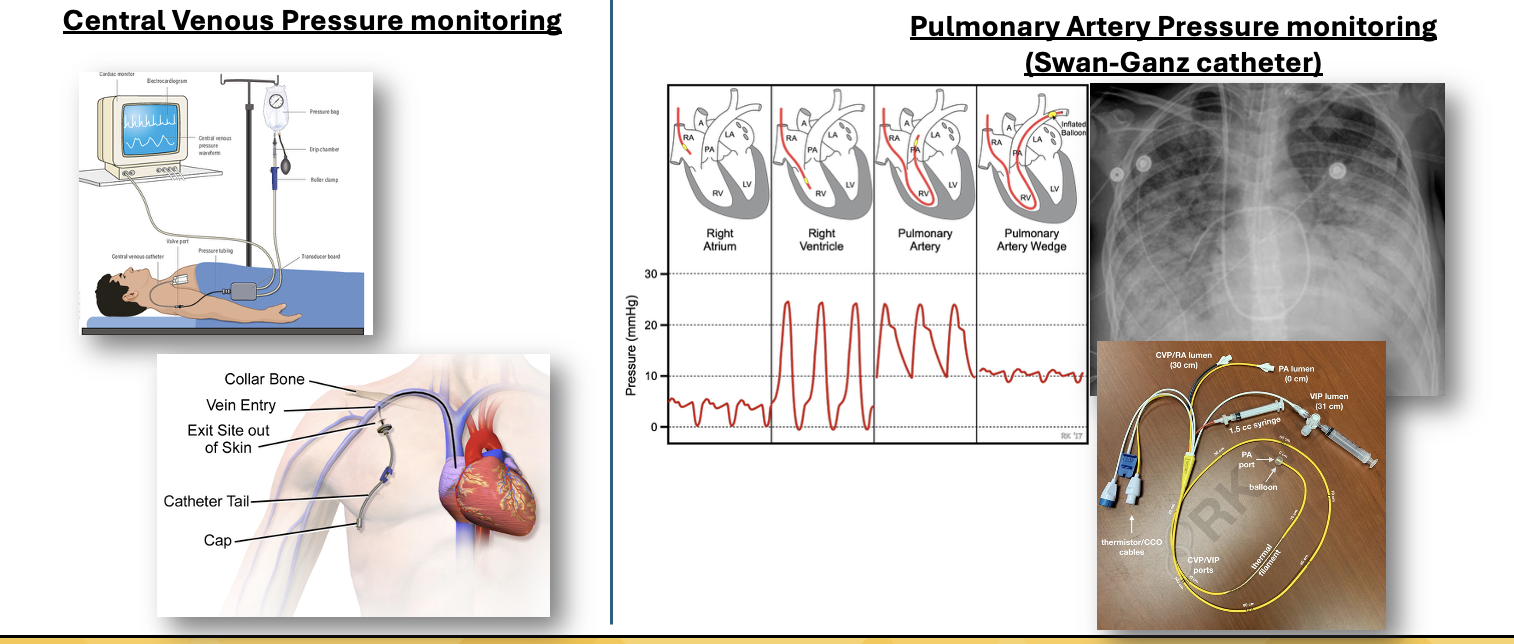
Volumes, Pressures, & Saturations: Central Venus Pressure (CVP)
Normal range = 8-12 mmHg
Used to estimate right arterial pressure and overall fluid status
Less than = dehydration or decreased fluid volume; Higher than = fluid overload
If used to evaluate fluid needs, also consider BP, UOP, and HR
Ex: if giving a lot of fluids and its at a 4, fluids might be elsewhere → should probably listen to the lungs! (ALI)
Volumes, Pressures, & Saturations: Pulmonary Artery Pressure (PAP)
Normal range = mPAP of 12-20 mmHg
Used to estimate right ventricular function and assess for pulmonary hypertension (PH)
right side of the heart → lungs
How well is the right side of the heart doing its job?
Volumes, Pressures, & Saturations: Pulmonary Artery Wedge Pressure (PAWP)
Normal range = mPAWP of 6-12 mmHg
Used to estimate left atrial pressure (left atrium)
Decreased in hypovolemic and distributive shock**
The left side of the heart has less blood in it
Elevated in cardiogenic shock***
The heart can’t pump it out (blood is pooling)
Increased or decreased in obstructive shock depending on the cause**
Examples of Invasive Hemodynamic Monitoring Equipment
Central Venous Pressure Monitoring
Pulmonary Artery Pressure Monitoring (Swan-Ganz catheter)
Sepsis: Prevalence and Vulnerable Populations
Each year in the U.S.:
1.7 million Americans develop sepsis
Roughly 350,000 die from sepsis
1 in 3 patients who die in the hospital has sepsis
The most vulnerable people are:
Older adults
Infants
Pregnant women
Those with chronic conditions
Immunocompromised patients

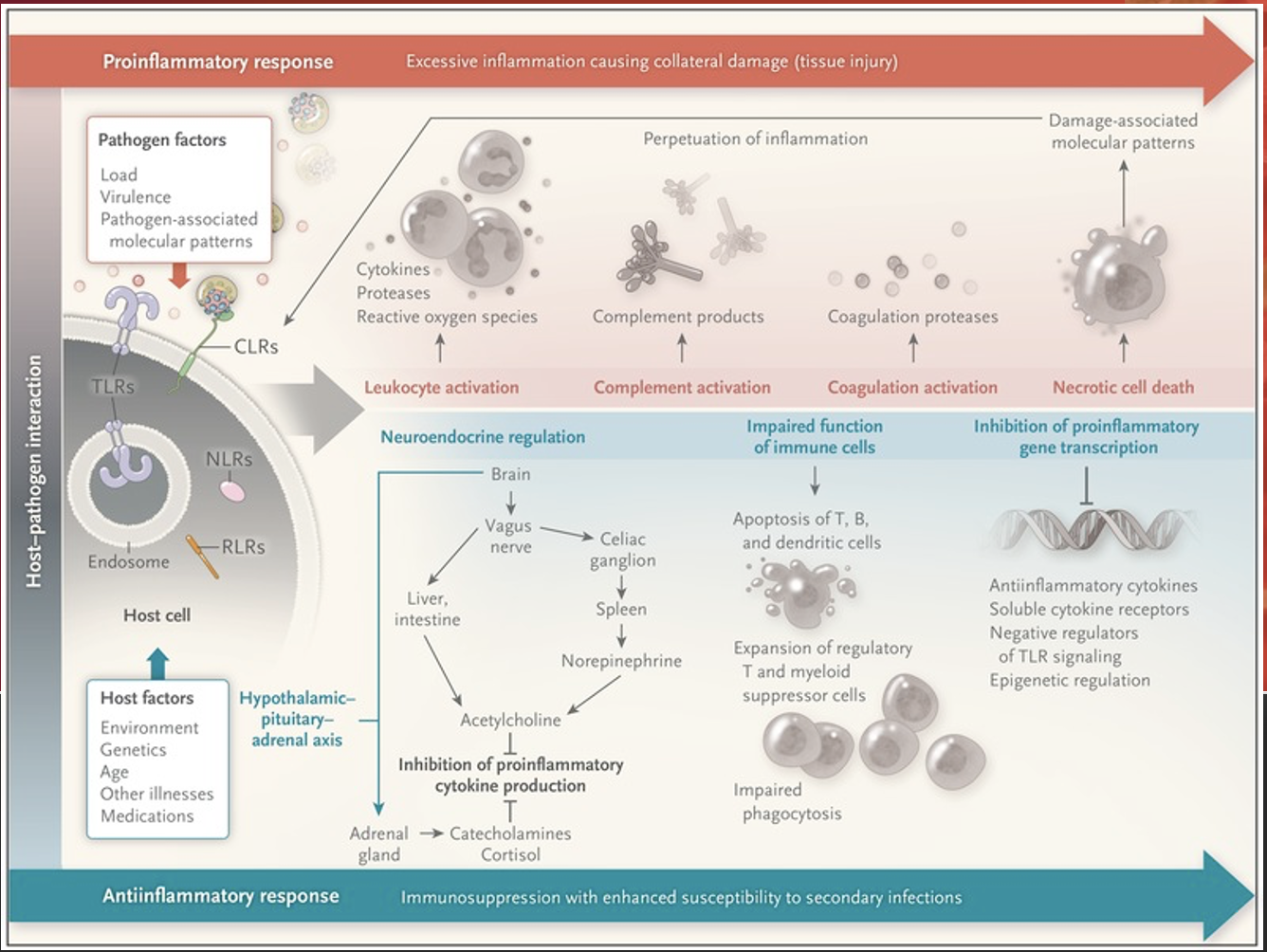
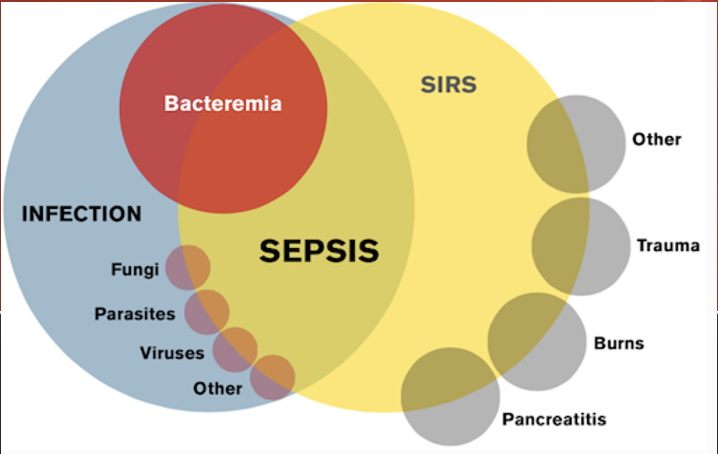
A form of distributive shock that is caused by a cascade of events:
Initiation of immune system
Inflammatory products activated
Vasodilation and blood vessel permeability (decreased SVR)
Impaired oxygen exchange
Trigged coagulation products
Developments of organ failure, ARDS, DIC
Sepsis is …
What are the most common HAIs?
Catheter Associated Urinary Tract Infection (CAUTI)
Central Line Associated Blood Stream Infection (CLABSI)
Ventilator Associated Pneumonia (VAP)
Surgical Site Infection (SSI)
Clostridium Difficile Infection (CDI)
Sepsis: Patient Assessment
Septic patients can present in different ways.
A thorough assessment is key.
Make sure to pay attention to labs!
Systemic Inflammatory Response Syndrome (SIRS)
SIRS criteria consists of:
Heart rate > 90 bpm
Respiratory rate > 20 rpm
Temperature > 38.8 C (100.9 F) or < 36.0 C (96.8 F)
WBC > 12,000/mm3 or < 4,000/mm3 or > 10% bands
Altered Mental Status
Glucose > 140 mg/dL in absence of diabetes
**2 or more and you’re positive for SIRS, but not everyone who is positive for SIRS is septic.
SIRS: What are bands?
They are immature WBCs.
Ex: someone’s WBCs went from 5,000 to 9,000—which is WNL, but if their bands are 17%, that means that their body had to ramp up production of WBCs because they have an acute infection.
source of infection; 2
A patient needs to already have a ______ __ _________ along with _ or more of the SIRS Criteria to be considered to have sepsis.
Not everyone who is positive for SIRS is septic. What are some examples?
A patient having an asthma exacerbation.
A patient experiencing a panic attack.
A patient suffering from heat exhaustion.
bacteremia
The biggest source of sepsis is __________.
Sepsis: Nursing Responsibilities
Recognize early
Treat promptly:
Follow the Sepsis Bundle**
Fluid Replacement
Pharmacologic
Astute ongoing assessment
The Surviving Sepsis Campaign (SSC)
Was launched in 2002 as a collaborative initiative of the European Society of Intensive Care Medium (ESICM), the International Sepsis Forum (ISF), and the Society of Critical Care Medicine (SCCM). It is updated every 4 years.
~Sepsis Bundle
Sepsis Nursing Responsibilities Soap Box
Monitor your patient for trends and report significant changes!
Do not just wait for a parameter to cross a predetermined threshold.
Nursing is about anticipation and preemptive action; addressing potential problems before they become actual problems.
If a patient’s SBP was 130, but now is 95, that’s concerning. If their potassium was 3.8, but now it’s 5.0, that’s concerning. If a patient’s WBC was 5.2, but now it’s 10.2, that’s concerning.
Sepsis Progression
Infection
Sepsis (Compensatory)
Severe Sepsis (Progressive)
Septic Shock (Irreversible)
Death or Recovery
Sepsis: Infection Stage
Initial Insult
Infectious Source
Pneumonia
UTI
Wounds
Gastrointestinal
Cellulitis
Sepsis: Sepsis Stage
Compensatory Stage
2 SIRS Criteria
Temperature
Heart rate
Respiratory rate
WBC
AMS
Hyperglycemia
Sepsis: Severe Sepsis Stage
Progressive Stage
Organ Dysfunction
Bilirubin
Platelets
Hypotension
AKI
Respiratory failure
INR/PTT
Lactic acidosis
Sepsis: Septic Shock Stage
Irreversible Stage
Presence of either:
Lactic acidosis
Persistent hypotension
*DIC most likely present
Severe Sepsis: Signs of Organ Dysfunction
Respiratory P/F ratio < 250 w/o pneumonia, or < 200 w/ pneumonia
MAP < 65 mmHg, SBP < 90 mmHg, or SBP decrease > 40 from baseline
Creatinine > 2 mg/Dl
UOP < 0.5 mL/kg/hr in 6 hours or < 400 mL in 24 hours.
Bilirubin > 2 mg/dL
Platelets <100,000/mm3
INR > 1.5 or aPTT > 60 secs
Lactate > 2 mmol/L
The Role of Lactate
Lactate is an indicator of global tissue hypoxia.
Increased lactate levels are associated with increased morbidity and mortality.
Lactate levels are used to guide resuscitation efforts.
persistent hypotension; lactic acidosis
Septic shock is classified by __________ ___________ and/or ______ ________ (lactate > 4 mmol/L)
Sepsis 1-Hour Bundle
Our Priorities:
Obtain lactate level
Obtain blood cultures x2 (from two different sites, aerobic + anaerobic—so technically 4)
Administer fluids
Administer broad spectrum antibiotics
Administer vasopressors if needed
Constantly reassess
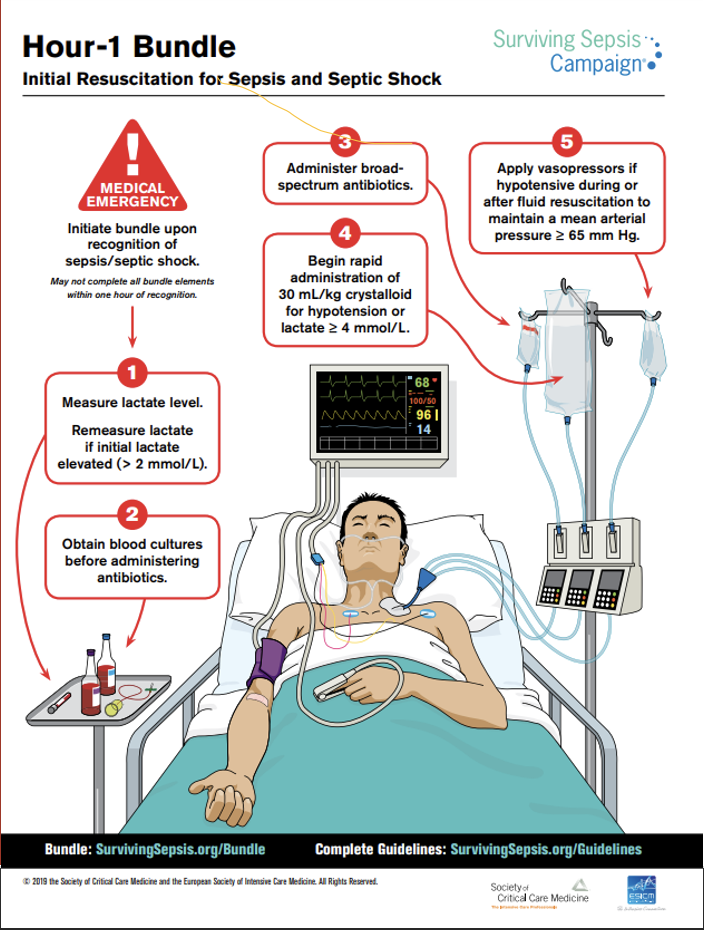
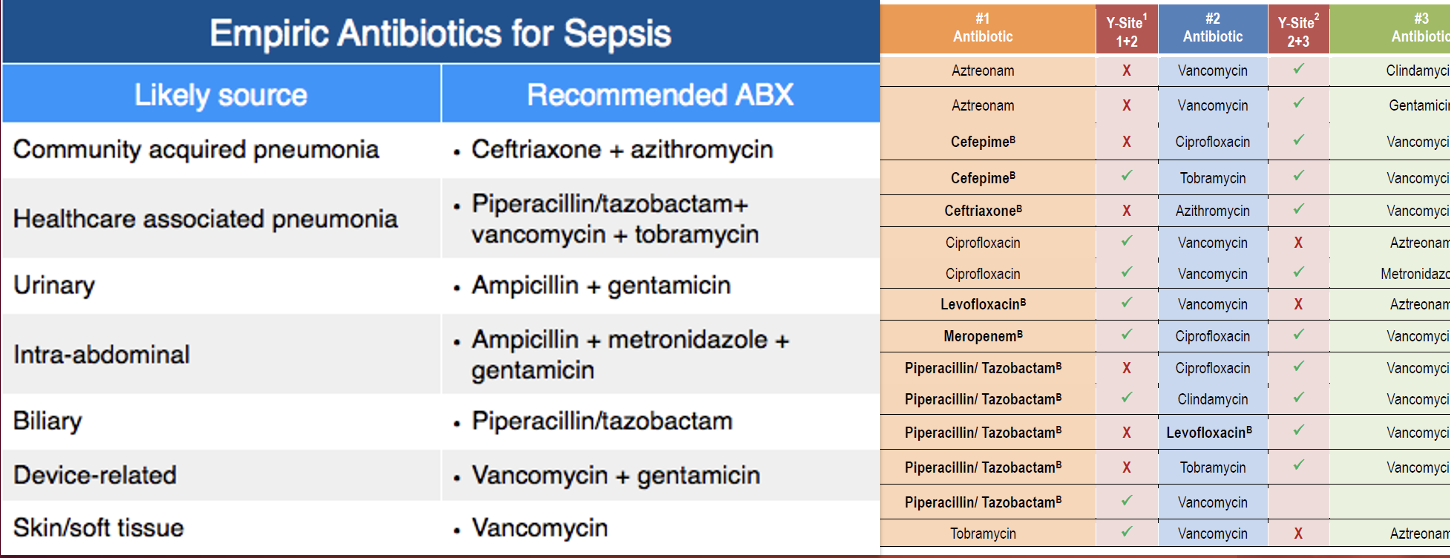
Sepsis: Broad Spectrum Antibiotics
Multiple antibiotics can be used; check for compatibility.
Delay in antibiotic administration is linked to increased mortality.
Administer IM, PO, or IO
If you can’t get IV access on your patient for broad spectrum antibiotics…
Broad Spectrum Antibiotics Compatibility
Incompatible medications can do many things when mixed:
Antagonizing (nullifying) effects
Precipitation (crystallization)
Consistency changes
Gas production, all of which are harmful to our patients!
Always check for compatibility within your documentation software. When in doubt, call the pharmacist!
Sepsis: Fluid Resuscitation
30 cc/kg of isotonic crystalloid solution
Normal Saline
Lactated Ringers
Calculation should be made using Ideal Body Weight (IBW)
FALSE! A history of heart failure does not exempt a patient from receiving a fluid bolus! Careful monitoring is required!
T/F: A history of heart failure exempts a patient from receiving a fluid bolus because it’s too dangerous.
Sepsis: Persistent Hypotension and Vasopressors
IF:
BP is measured every 15 minutes post-fluids, so…
Two consecutive low BP readings indicates persistent hypotension…
THEN:
Vasopressors should be started without delay!
Norepinephrine (Levophed)
What is our first-line vasopressor in septic shock?
Persistent Hypotension and Vasopressors: Norepinephrine Dose + Receptor
Dose: 0.1-0.5 mcg/kg/min, titrate to effect
Receptor: a1 & b1