2. Urinary System Disorders
1/148
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
149 Terms
ANSWER: B
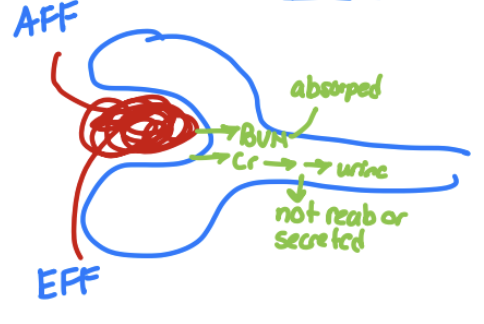
-> albumin a protein in blood, and stays in blood
In a healthy glomerulus, where would you find albumin?
a. In the filtrate
b. In the capillary lumen
ANSWER: D
glucose is smaller
glucose is freely filtered @ the glomerulus, starts there and filtered thru lumen, cross Basement Membrane go thru tubule
hence D is the answer
Same with Na, any electrolyte, a.a’s, water
IN a healthy glomerulus, where would you find glucose?
a. Filtrate
b. Basement membrane
c. Capillary lumen
d. Everywhere
Glomerular Disorders
Generally referred to as glomerulopathies
Alterations to glomerular structure and function – endothelium, basement membrane, and/or podocytes
Course of the disease
Proportion and parts of glomeruli effected
Histological
Glomerular disorders Can be classified according to:
________________:
Acute, rapidly progressive, chronic, insidious
_______________________________:
Diffuse vs. focal; global vs. segmental
__________ characteristics:
Minimal change, proliferative, membranous, sclerotic
Etiologies
Primary vs. secondary vs. hereditary
These terms are sometimes combined to describe the glomerular abnormality
Diffuse: All or nearly all glomeruli are involved
Focal: Only some glomeruli are involved → concentrated in an area
Diffuse vs. focal glomerulopathies
global: The entire glomerular tuft is involved
segmental: Only a portion (segment) of the glomerular tuft is affected
global vs. segmental glomerulopathies
Glomerulopathies
Commonly result in:
Proteinuria
Hematuria
RBC casts
Decreased GFR
Hypertension
Nephrotic syndrome
Excessive (>3-3.5g/24 hr) loss of proteins in urine
Due to damage to podocyte slit pore proteins and increased glomerular permeability → proteins escape from capillaries into tubule
Nephritic syndrome
Hematuria and RBC casts
will also have proteinuria but isnt a massive characteristic
Due to glomerular inflammation and leakiness
Proteinuria
Glomerular filtration membrane is made of three layers
Endothelial cells, basement membrane, filtration slits (podocytes)
Podocytes ultimately control what can pass through
Small proteins (e.g. cytokines, insulin) can cross slit diaphragm, but anything larger is prevented from crossing
podocyte damage
Proteinuria usually indicates _______________
Changes in slit diaphragm; increased permeability
Hallmark: presence of large proteins like albumin in urine
Hematuria
Blood can come from anywhere in urinary tract
May indicate urological OR renal disorders
________________ usually indicates physical disruption to filtration membrane
RBC fragments isolated from urinary casts often have abnormal shape
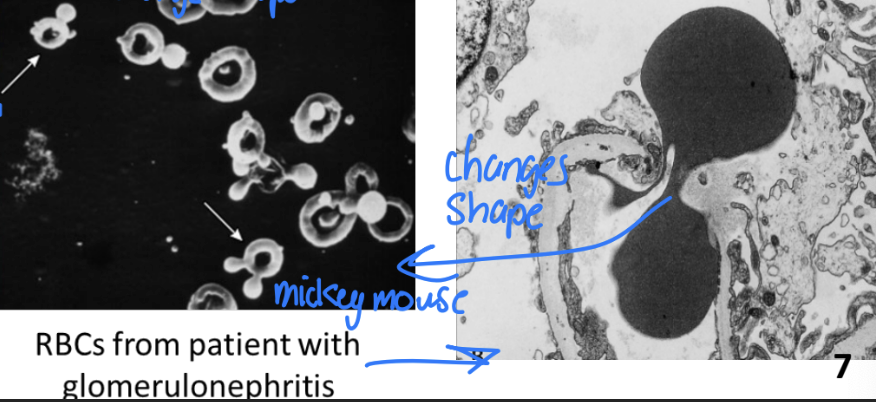
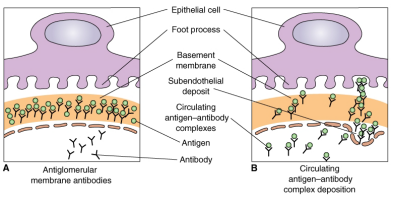
Glomerulonephritis
Variety of immune -mediated conditions that cause glomerular inflammation
Primary
Secondary
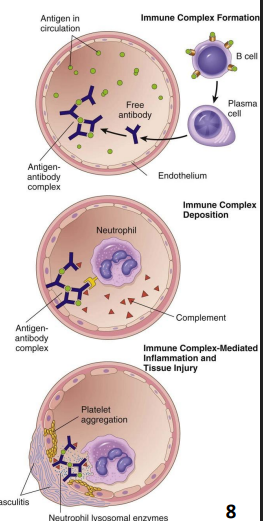
Etiology of Glomerulonephritis
_______:
Autoantibodies against glomerular antigens
_________:
Infectious or Autoimmune → from somewhere else in the body
Circulating antibody complexes get trapped in glomerular membrane
Metabolic (e.g. diabetes)
Hemodynamic (e.g. hypertension)
Toxic (e.g. drugs, chemicals, radiation)
glomerular
Pathogenesis of Glomerulonephritis:
Immune complex deposition or other causes of glomerular damage
Recruitment of immune cells
Damage to _________ BM → BM thickening → scarring → decreased GFR
Proteinuria and/or hematuria
Hematuria
Proteinuria and hypoproteinemia = edema
Vulnerability to infections (loss of immunoglobulins)
Vitamin D insufficiency (loss of vitamin D-binding protein)
Edema → decrease plasma proteins
Hyperlipidemia and lipiduria (fatty casts) → excessive compensation
Thrombotic complications (increased hepatic synthesis of clotting factors) → leans towards pro coag
Hypertension → decreased excretion = decreased GFR => positive feedback loop with damage to kidney further decline in GFR
Renal impairment – uremia → mild toxicity, oliguria
Signs and symptoms of Glomerulonephritis
Urinalysis (proteinuria, hematuria, WBCs, RBCs, casts)
Serology (antibodies, creatinine, BUN, GFR measurements)
Renal biopsy → find out type
Diagnosis of Glomerulonephritis
Treat underlying disease
Blood pressure control – ACE inhibitors
Diet – salt restriction, protein and vitamin D supplements
Diuretics
Anti-hyperlipidemic drugs – e.g. niacin, statins
Anti-coagulants
Immunosuppressive agents – e.g. corticosteroids
Dialysis
Kidney transplant
treatment of Glomerulonephritis
Some forms spontaneously recover
Some forms are treatable
Causes ~25% of end-stage renal failure
Prognosis of Glomerulonephritis
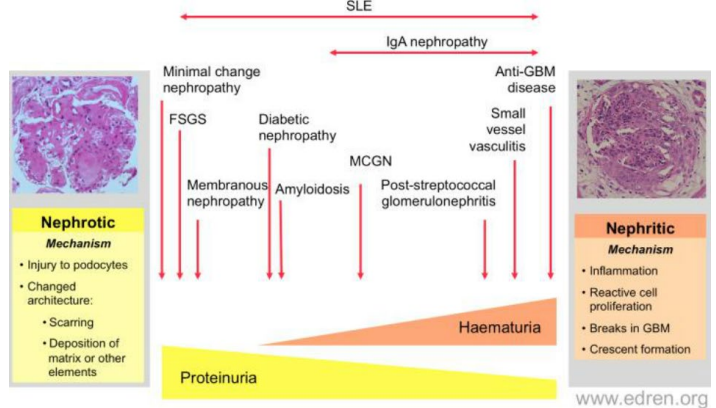
Nephrotic syndromes
Two Main Clinical Patterns - ______________:
Characterized by proteinuria
Minimal change disease
Membranous nephropathy
Focal segmental glomerulosclerosis
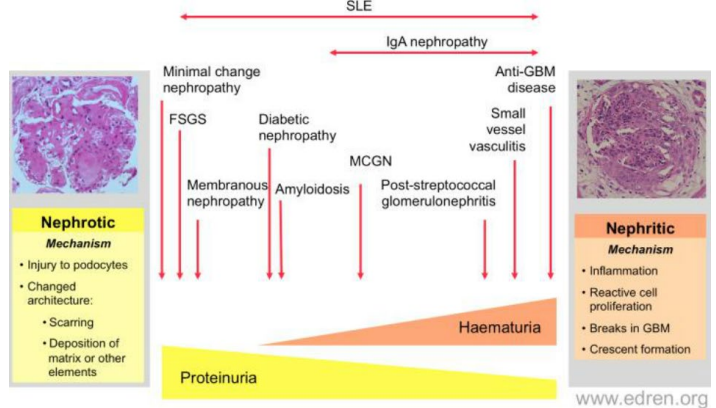
Nephritic syndromes
Two Main Clinical Patterns -_______________:
Characterized by hematuria
Acute proliferative glomerulonephritis
IgA nephropathy
Crescentic glomerulonephritis
ANSWER: C
if it said characterized then its nephrotic
in this case both have proteinuria, as if we have enough hole for RBC to go thru = also proteins go thru inapprop filtration membrane and enter kidney tubule
Proteinuria is associated with..
a. Nephritic syndromes
b. Nephrotic syndromes
c. Both
d. Neither
ANSWER: A
Hematuria is associated w/…
a. Nephritic syndromes
b. Nephrotic syndromes
c. Both
d. Neither
Answer: D
Glucose starts in blood, goes into tubule, and gets reabsorbed, in the tubules
If its in urine (glycosuria)
If we have a problem with podocytes, does this effect flow of this, no
If we have problem w/ inflam here in glomerulus and RBC here, does this effx glucose = no
What would need to be defective to get glucose in urine = the tubular cells = tubulointerstitial disorders = glucose in urine
But nephrotic and nephritic = no impact on tubules - hence nothing to do w/ glycosuria or not
Glycosuria is associated with..
a. Nephritic syndromes
b. Nephrotic syndromes
c. Both
d. Neither
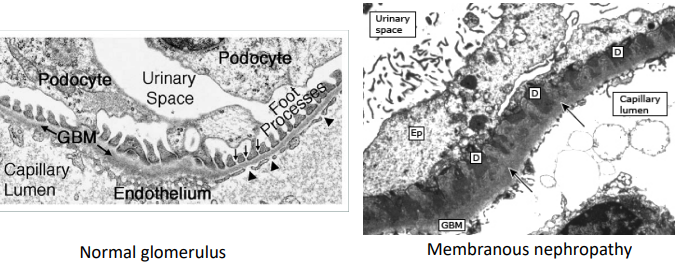
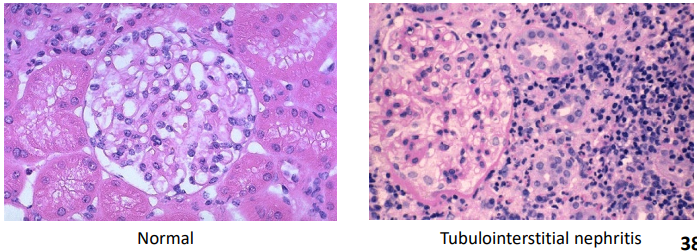
The Normal Glomerulus
Open capillary loops
Sharp glomerular basement membrane
Nephrotic Glomerular Disease
Damage to podocytes and loss of the negatively charged glycoprotein barrier lead to increased filtration of proteins into urine
Changes to slit membrane; increase in podocyte/glomerular permeability
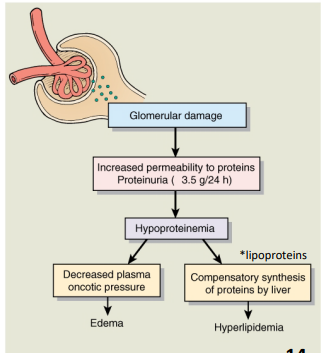
Massive proteinuria (>3.5 g/24hr)
Hypoalbuminemia (<30 g/L)
Edema
Hyperlipidemia
Increased clotting factor synthesis
key features of Nephrotic Glomerular Disease
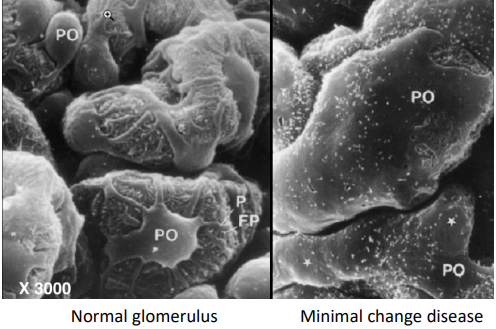
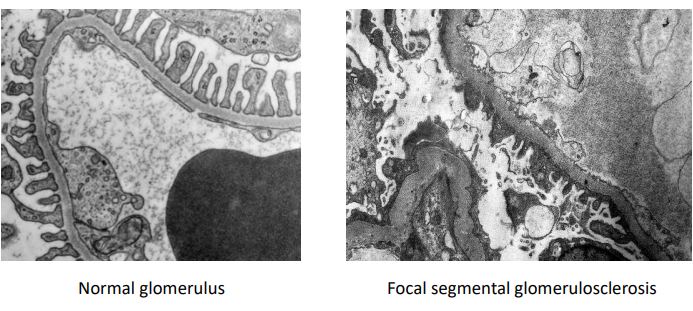
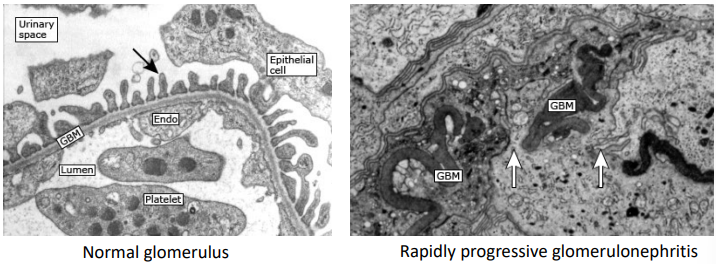
Minimal Change Disease
Compare the glomeruli in these light microscopy images:
Open capillaries
Sharp glomerular basement membrane
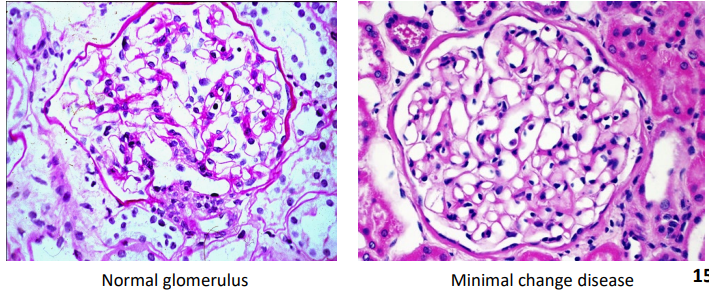
Loss of digitating processes
Minimal Change Disease
Compare the podocytes in these scanning electron microscopy images:
_______________ and podocytes become more permeable
Minimal Change Disease (previously Lipoid Nephrosis)
Most common cause of childhood nephrotic syndrome
Accounts for ~10% of nephrotic syndrome in adults
Allergic or immune disorder → systemic T or B cell dysfunction → release of glomerular permeability factor → fusion of podocyte processes and loss of negatively charged proteoglycans
Pathogenesis of Minimal Change Disease
Biopsy showing normal-appearing glomeruli on light microscopy
Absence of complement or immunoglobulin deposits on immunofluorescence microscopy
Diagnosis of Minimal Change Disease
Most patients are responsive to glucocorticoid treatment
Remission of proteinuria in ~90% of cases
Prognosis of Minimal Change Disease
Membranous Nephropathy
Compare the glomeruli in these light microscopy images:
Thickening of glomerular basement membrane
Number of cells unchanged
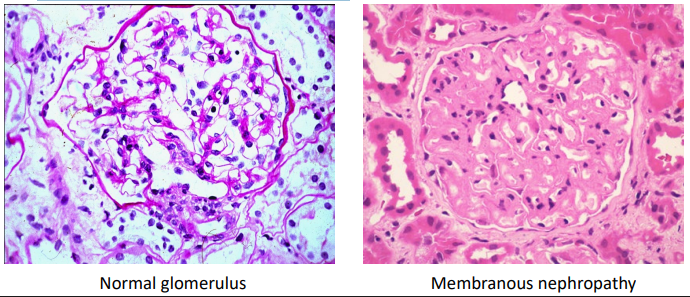
Membranous Nephropathy
Compare the podocyte processes in these electron microscopy images:
Dark patches (D) scattered within a thickened glomerular basement membrane (GBM)
primary glomer?
Antibodies against antigens on podocyte foot processes → complement activation and MAC formation → loss of slit membrane integrity
Injured podocytes secrete ECM proteins → GBM thickening
Pathogenesis of Membranous Nephropathy
Complete or partial remission in some patients
Others have persistent nephrotic syndrome that may proceed to end-stage renal disease
Prognosis of Membranous Nephropathy
ANSWER: B
need to be able to dx based on images for tests & underlying etiology/patho
Membranous nenprhaty is caused by…
a. Prior step infection
b. Autoimmune attack of podocyte processes
c. Immune cell release of soluble factors
d. Accumulation of immune complexes
Focal Segmental Glomerulosclerosis
Compare the glomeruli in these light microscopy images:
Deposition of excess matrix (pink material)
Rest of glomerulus looks normal
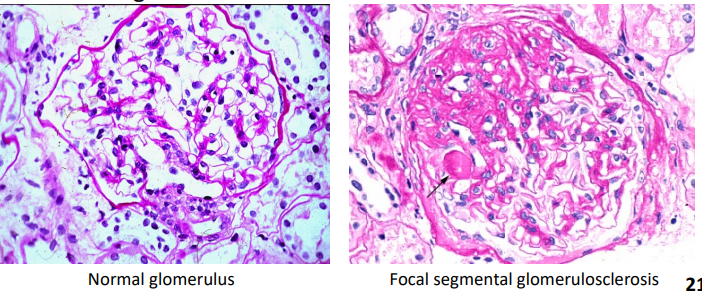
Focal Segmental Glomerulosclerosis
Compare the podocyte processes in these electron microscopy images:
Loss of normal podocyte architecture
Focal Segmental Glomerulosclerosis
Found in ~35-50% of adult patients with idiopathic nephrotic syndrome
Putative circulating permeability factors
Some patients develop recurrent FSGS after kidney transplant
Plasmapheresis reduces proteinuria in these patients
Nephron injury or loss → decreased podocyte density in focal areas
Nephron damage → cytokine release → accumulation of ECM components → scar formation
pathogensis of Focal Segmental Glomerulosclerosis
Some patients are responsive to glucocorticoids
Some patients develop rapidly progressive renal failure
prognosis of Focal Segmental Glomerulosclerosis
Nephritic Glomerular Diseases
Destruction of glomerular filtration membrane (due to inflammation) leads to presence of red blood cells in urine
Hematuria
Proteinuria (may reach nephrotic range)
Edema from sodium and fluid retention
Hypertension
Key features of Nephritic Glomerular Diseases
Acute Proliferative Glomerulonephritis
Compare the glomeruli in these light microscopy images:
Poorly defined capillary loops
Increased number of cells
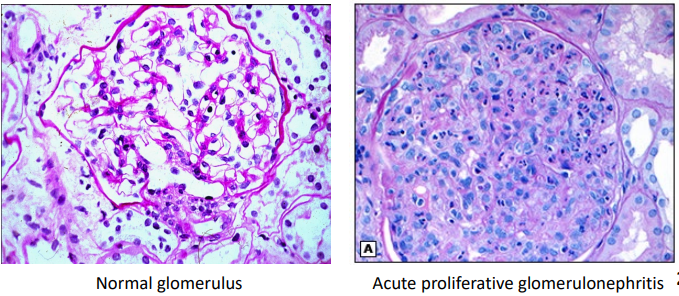
Acute Proliferative Glomerulonephritis
Compare these electron microscopy images:
Dark patches (D) showing subepithelial immune deposits
Neutrophil attached to GBM
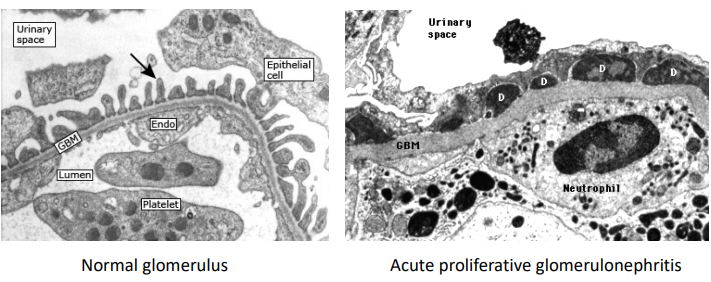
Acute Proliferative Glomerulonephritis
Most commonly caused by prior infection with group A β- hemolytic streptococcus (GAS)
Most common cause of acute nephritis in children
GAS infection → deposition of streptococcal antigens in the GBM → antibody binding and inflammatory response
pathogensis of Acute Proliferative Glomerulonephritis
Clinical findings of acute nephritis + evidence of recent GAS infection (throat or skin culture, or serum antibodies)
impetigo, cellulitis, necrotizing fasciitis
diagnosis of Acute Proliferative Glomerulonephritis
Generally favourable (self-resolving), especially in children
<1% of cases proceed to rapidly progressive GN
prognosis of Acute Proliferative Glomerulonephritis
IgA Nephropathy
Compare the glomeruli in these light microscopy images:
Segmental areas of increased mesangial cell matrix
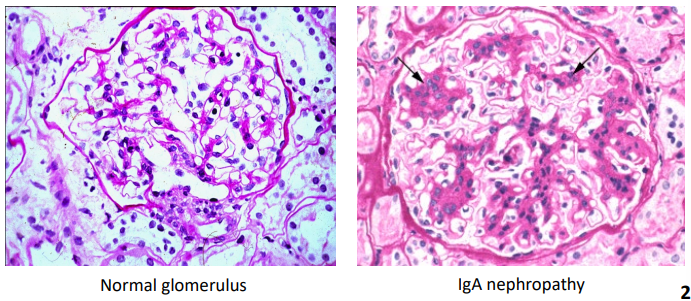
IgA Nephropathy
Compare these electron microscopy images:
Immune deposits (D) limited to mesangial regions
GBM appears normal
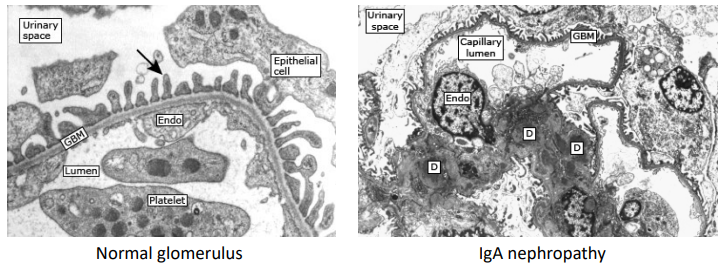
IgA Nephropathy
Most common cause of GN worldwide
Peak incidence during age 10 – 30, predominantly in Asian and Caucasian populations
Often triggered by upper respiratory tract / GI infections → mucosa
Mesangial deposition of circulating IgA immune complexes
Impaired clearance of the complexes
Injury, inflammation and scarring
pathogensis of IgA Nephropathy
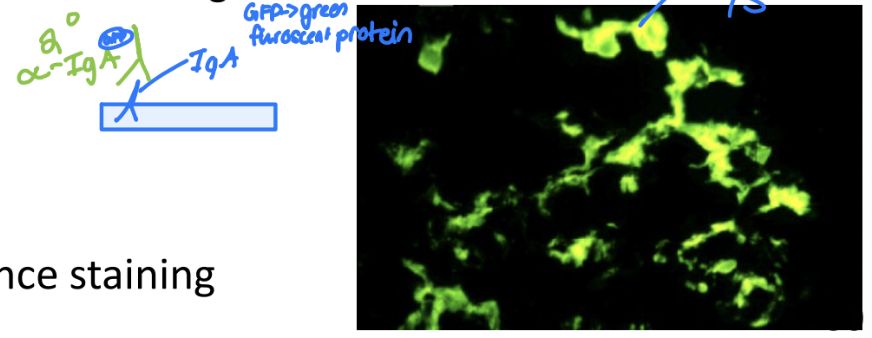
Biopsy and IgA immunofluorescence staining
diagnosis of IgA Nephropathy
Supportive measures (e.g. BP control, ACE inhibitors)
Glucocorticoids to treat underlying inflammation
treatment of IgA Nephropathy
Some patients are asymptomatic
Some patients have one episode of hematuria
Some patients have recurrent, slowly progressive GN
Some patients rapidly develop end-stage renal failure
prognosis of IgA Nephropathy
Crescentic Glomerulonephritis
Compare the glomeruli in these light microscopy images:
Crescent made of proliferating epithelial cells
Compression of glomerular capillaries
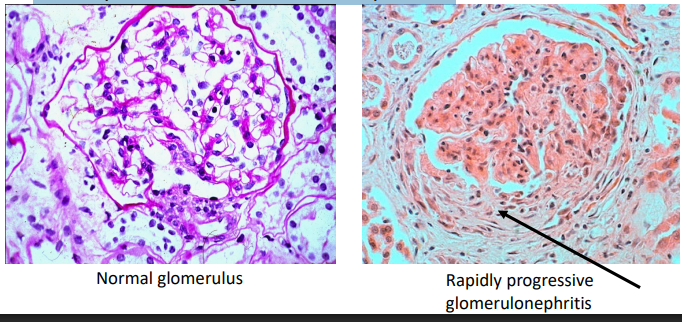
Crescentic Glomerulonephritis
Compare these electron microscopy images:
Breaks in the GBM
Fibrin leaks into glomerular capsule → crescent formation
Crescentic Glomerulonephritis
Characterized by progressive loss of renal function over a short period of time (days to months)
secondary autoimmune?
Primary: Anti-GBM antibodies (e.g. Goodpasture’s disease)
Secondary: Immune complexes (e.g. SLE)
Etiology of Crescentic Glomerulonephritis
Severe injury to glomerulus → movement of fibrinogen and inflammatory cells into glomerular capsule
pathogenesis of Crescentic Glomerulonephritis
Biopsy and immunofluorescence staining (e.g. anti-GBM antibodies, antinuclear antibodies)
Decreased GFR
diagnosis of Crescentic Glomerulonephritis
Supportive measures (e.g. BP control, ACE inhibitors)
Glucocorticoids and other immunosuppressive therapies to treat underlying inflammation
Plasmapheresis
treatment of Crescentic Glomerulonephritis
Severity of disease depends on underlying cause
Poor prognosis if patient has anuria
prognosis of Crescentic Glomerulonephritis
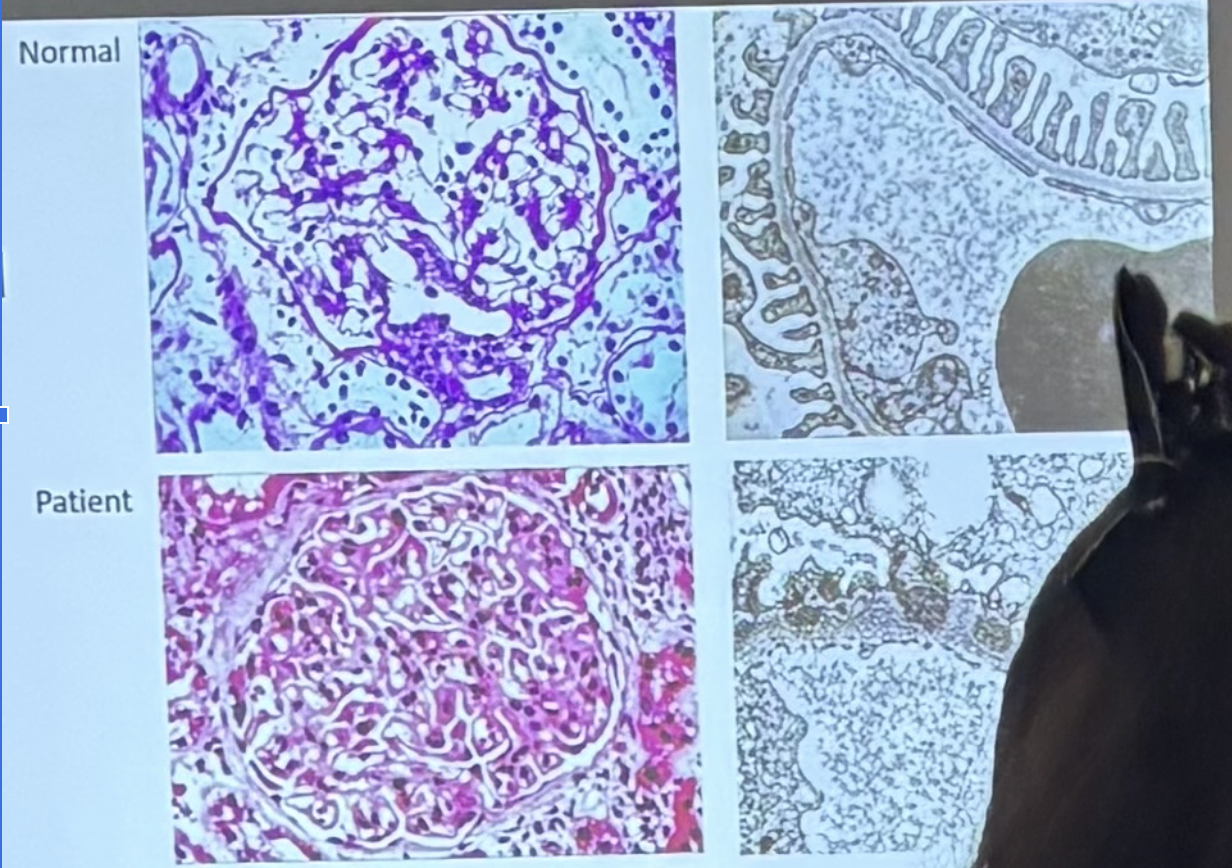
ANSWER: B
D) on light graph we would see crescent of prolif epithelial cells & fluids + compression of capillaries = not seen here
C) not minimal change = look very sim
B and A) expect to see thickening of ECM = and we see that
What do we look to see to differentiate between the two = # of cells
→ not that many extra cells seen
Lets use the high tech microscope to see and confirm this
Podocytes are changed
Deposition of material between podocytes but rest looks okay
Consistent w/ dx of membranous nephropathy = caused by what?
What type of GN is this? How do you know?
a. Acute proliferative GN
b. Membranous nephropathy
c. Minimal change disease
d. Rapidly progressive GN
Tubulointerstitial Disorders
Disorders that affect renal tubular structures and the surrounding tissues
Altered tubular function → loss of sodium and water, retention of H+
Pyelonephritis
Tubulointerstitial nephritis
Two principle forms of Tubulointerstitial Disorders:
_______________
Infectious causes (covered in UTIs)
_________________________
Non-infectious causes
Analgesics (e.g. aspirin, NSAIDs)
Antibiotics (e.g. penicillin, tetracycline, streptomycin)
Diuretics
Heavy metals
Toxins (e.g. mushroom poisons)
etiology of Tubulointerstitial Nephritis
Damage to nephron tubules → inflammation of kidney interstitum → scarring → decline in renal function
More common in older patients
pathogensis of Tubulointerstitial Nephritis
Renal tubular acidosis
Glycosuria and aminoaciduria
Electrolyte wasting
Oliguria → hypertension
Azotemia (increased nitrogen substances in blood)
Renal failure
manifestations of Tubulointerstitial Nephritis (depends on toxin, dose, and exposure)
Elevated serum creatinine
Urinalysis showing WBCs and WBC casts
Biopsy
diagnosis of Tubulointerstitial Nephritis
Remove underlying cause
Glucocorticoids
Supportive treatment for hypertension, electrolytes
treatment of Tubulointerstitial Nephritis
Acute cases: (partial) recovery usually occurs if offending substance removed
Chronic cases: inflammation and scarring cause irreversible loss of function
prognosis of Tubulointerstitial Nephritis
Renal Failure
Condition in which the kidneys:
Fail to remove metabolic waste products from the blood
Fail to regulate fluid → fluid overload = HTN, electrolyte → Increased K+ → lack secretion, and pH balance of the extracellular fluids
ALL LEAD TO DECREASED GFR
Acute
Chronic
Two forms of Renal Failure:
______ – rapid onset, potentially reversible
__________– develops slowly, irreparable damage
Acute Kidney Injury (AKI)
Occurs in ~10% of hospitalized patients and 50% of patients in the ICU, with mortality rate ~40 – 75%
Abrupt decrease in renal function characterized by decreased GFR
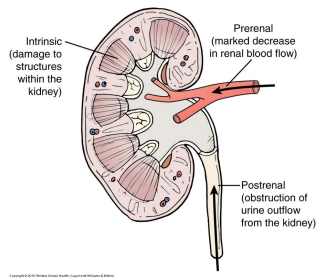
Pre-renal
Intra-renal
Post-renal
etiology of Acute Kidney Injury (AKI)
Pre-Renal Kidney Injury
AKI that results from diminished renal blood flow
Hypovolemia
Dehydration
Hemorrhage
Diuretics
Vomiting or diarrhea
Burn injuries
Decrease in circulating volume → still have fluid BUT NOT IN VESSELS
Shock – anaphylaxis, sepsis → mass vasodilation → decrease BP → decrease GFR
Third-spacing and edema → Alcholic liver disease → busy metaboliziing ethanol = decreased production of albumin
Decreased cardiac output (e.g. heart failure, myocardial infarct)
Renal hemodynamic abnormalities
Renal artery occlusion
Drugs that interfere with renal autoregulation (e.g. NSAIDs, ACE inhibitors) → NSAIDS block COX-1 → produces prostaglandins → vasodilation of Afferent arteriole → remain too constricted
etiology of Pre-Renal Kidney Injury
Oliguria
Elevation of BUN:creatinine ratio
decreased GFR → travel through tubule slowly → increased BUN/Cr ratio
increased GFR → fast through tubule → decreased BUN/Cr ratio
Activation of RAA system → renal vasoconstriction → increased vol by production of renin = fluid reab
Renal hypoxia and tubular cell death if blood flow <25% of normal
manifestations of Pre-Renal Kidney Injury
Restore adequate perfusion
Can be reversed if cause is identified and corrected before damage occurs
treatment of Pre-Renal Kidney Injury
Post-Renal Kidney Injury
Rare
AKI that occurs due to bilateral obstruction of urine outflow from kidneys
Ureters – e.g. calculi and strictures → space occupying lesion
Bladder – e.g. tumours, neurogenic bladder
Urethra – e.g. prostate hyperplasia
Increased capsular hydrostatic pressure = decreased GFR
Remove obstruction as reestablish urine flow before permanent nephron damage occurs
treatment of Post-Renal Kidney Injury
Intra-Renal Kidney Injury
AKI that results from damage to kidney structures
Glomerular, tubular, interstitial, vascular
Note: All cases AKI will eventually involve intra-renal kidney injury if not treated promptly
Tubular cell injury → acute tubular necrosis
Most common cause of intra-renal kidney injury
Glomerular: Acute GN
Interstitial: Acute pyelonephritis, interstitial nephritis
Vascular: Vasculitis, emboli, damage from hypertension
Tubular: Ischemia, toxins, obstruction
Tubular cell injury → acute tubular necrosis
Most common cause of intra-renal kidney injury
etiology of Intra-Renal Kidney Injury
Acute Tubular Necrosis
Accounts for ~50% of AKI cases in hospitalized patients
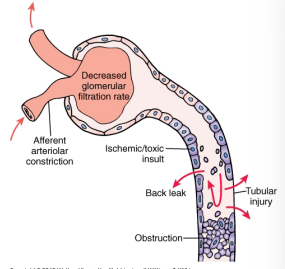
Tubular epithelial cells are very sensitive to ischemia and toxins
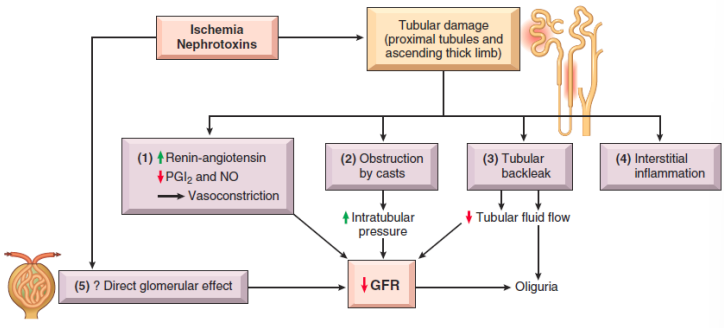
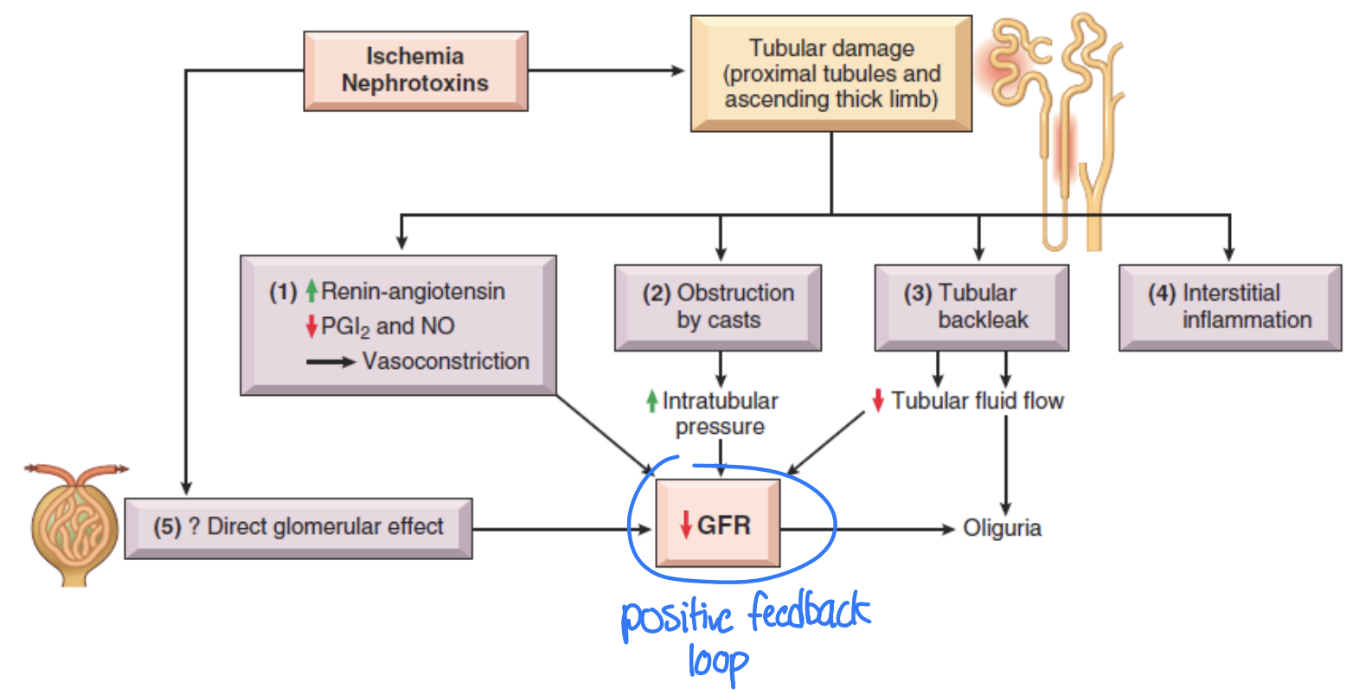
Ischemia → RAA activation → vasoconstriction of afferent arteriole
Damaged tubular epithelial cells are shed from BM and obstruct tubular flow
Increasing tubular pressure forces filtrate through tubular BM into interstitial space → tubular back leak
3. Interstitial inflammation
Positive damaging feedback loop
mechanism of injury of Acute Tubular Necrosis
ANSWER: D
(most common cause of intra-renal AKI) all of the following except for what?
2 most common causes = A & B
If have damage = need immune resp = WBC come in clean up and cause inflamm
If we get inflamm we often get casts in CD = casts get dislodged = in urine and see it = indicative fo renal inflam specific in tubule
What we dont see is polyuria bc we get reduced GFR = leads to oliguria
Acute tubular necrosis is NOT associated with:
a. Ischemia
b. Nephrotoxins
c. Interstitial inflammation
d. Polyuria
e. Urinary Casts
Prodromal phase
Stages of Acute Tubular Necrosis:
Decreased perfusion and/or increased toxicity → injury
Oliguric phase
Stages of Acute Tubular Necrosis:
Decrease in GFR → oliguria
Increased BUN and serum creatinine
Retention of metabolites
Fluid retention → hypertension
Post-oliguric phase
Stages of Acute Tubular Necrosis:
Repair of renal tissue – normal function reestablished when damaged is stopped = sable to reverse effects
Removal of necrotic cells and casts, and regeneration of renal cells (depends on intact BM)
however does not happen with everyone → can lead to acute kidney failure
ANSWER: D
problem is blood flow to kidneys , cause v/c of afferent arteriole = even more lack of blood flow
A is incorrect b/c an example of INTRA renal
B is incorrect b/c post renal
C is incorrect b/c prob w/ intra (part of kidney)
Which of the following is a pre-renal cause of AKI?
a. Acute tubular necrosis
b. Bilateral kidney stones
c. Glomerulonephritis
d. Severe hypotension
ANSWER: C
all forms of AKI, result in decr GFR, hence why they lead to kidney dysfunction
Which of the following statements is TRUE?
a. Reduced GFR is only peasant in pre-renal AKI
b. Reduced GFR is only present in post-renal AKI
c. Both pre- and post- renal AKI are assoc with reduced GFR
d. Neither is associated with reduced GFR
ANSWER: E
Uremia = urine in blood ;stuff that should come out, stays in
When we have uremia = do we have accum of nitrogenous wastes in the blood
Anemia d/t EPO, and vit d = calcitriol
General weakness = effx all body systems
Which of the following is NOT a symptom of uremia?
a. Accumulation of nitrogenous wastes in the blood
b. Anemia and impaired vitamin D synthesis
c. General weakness, fatigue, and nausea
d. HTN
e. All of the above are symptoms of uremia
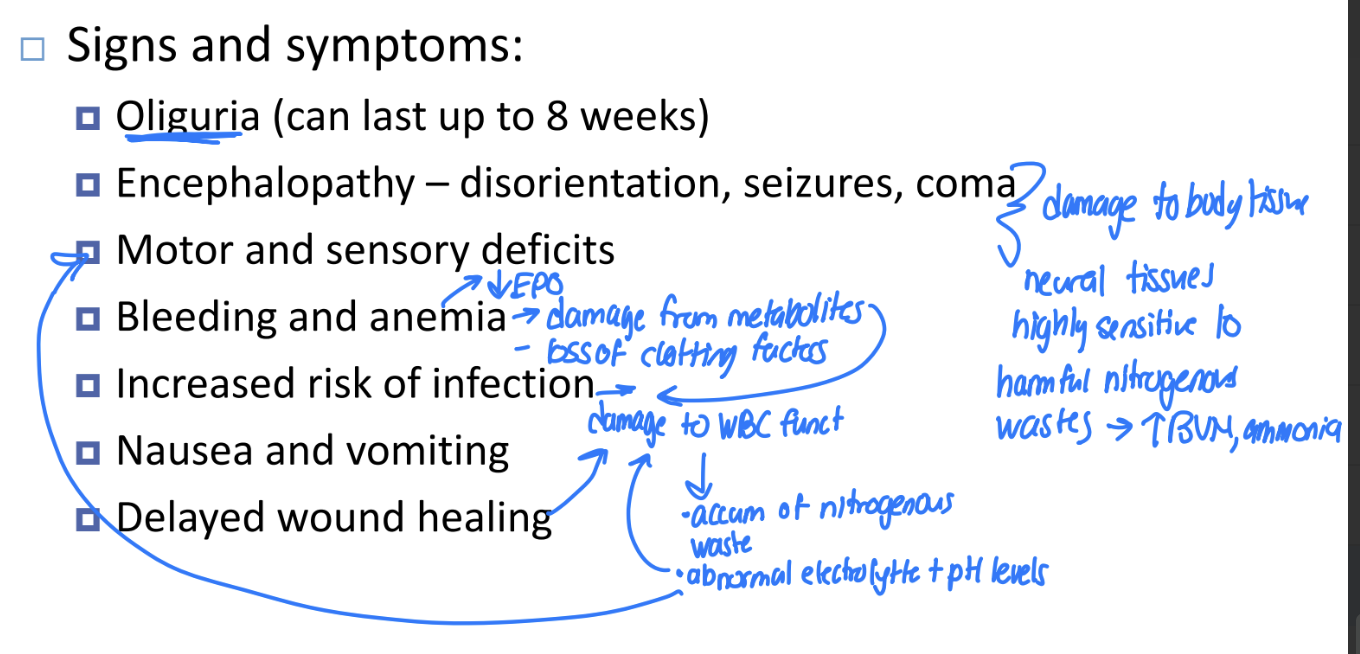
Oliguria (can last up to 8 weeks)
Encephalopathy – disorientation, seizures, coma
Motor and sensory deficits
Bleeding and anemia → decreased EPO
Increased risk of infection
Nausea and vomiting
Delayed wound healing
Signs and symptoms of Acute Kidney Injury
Patient history and physical exam
Urine output
GFR measurement
Urinalysis
Proteinuria
Hematuria
Casts or crystals
Urine osmolarity, pH, and electrolytes
Blood tests
BUN
Creatinine
Response to volume repletion
diagnosis of Acute Kidney Injury
Treatment – goal is to keep the patient alive until renal function has recovered:
Acute dialysis
Discontinuing nephrotoxic drugs
Early treatment of obstruction
Fluid and electrolyte management
Monitoring and adjustment of blood parameters and pressure
Antibiotics prn
Diet to maintain nutrition
treatment of Acute Kidney Injury
Incomplete recovery in 30% of patients
60% mortality rate
prognosis of Acute Kidney Injury