Week 13 - Human Hereditary Disease and Genetic Screening
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
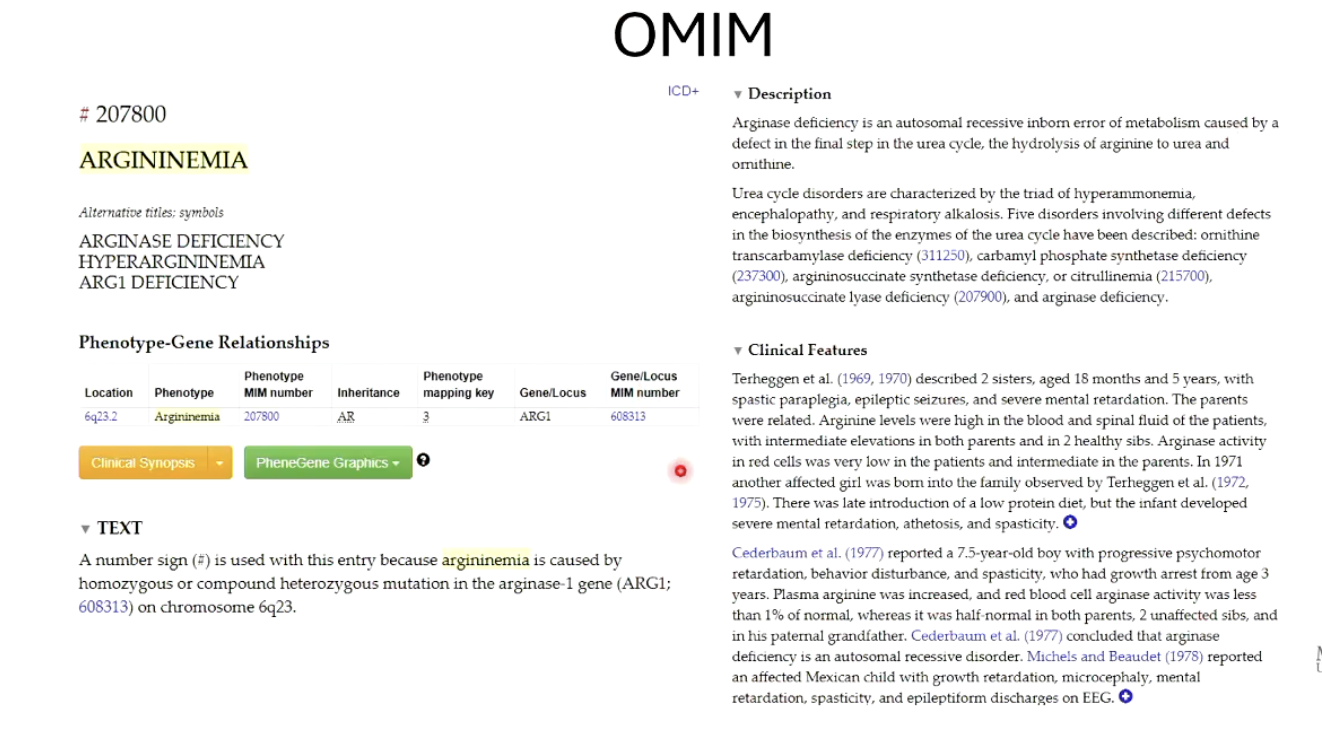
Who is B.K., and why is his story important in learning about genetic screening?
B.K. was born healthy in 2015 but tested positive for argininemia (ARG) during newborn screening.
ARG is a rare autosomal recessive disease caused by a deficiency in arginase, an enzyme that breaks down arginine.
If untreated, it can lead to ammonia buildup, poor growth, muscle control issues, and cognitive delays.
His story highlights how early genetic screening can detect and prevent severe outcomes.
How was B.K.’s condition managed after diagnosis?
Treated with a low protein diet, medication to remove ammonia, and regular blood tests.
Parents received genetic counselling, confirming they were both heterozygous carriers.
Early intervention allowed B.K. to meet developmental milestones and live a relatively normal life.
What is the field of medical genetics and its main goals?
Aims on diagnosing and managing the medical, psychological, and social aspects of inherited diseases.
Main goals include:
Diagnosing hereditary conditions in infants.
Providing treatment and care for rare inherited diseases.
Assessing genetic risk for future children through family history and genetic testing.
Who works in the field of medical genetics?
Medical genetics is a collaborative field involving:
Physicians
Diagnostic technicians
Laboratory researchers
Genetic counsellors
All work together to support patients and families affected by hereditary diseases.
What are the three main categories of hereditary disease?
Mendelian conditions
Autosomal dominant (Huntington’s Disease)
Autosomal recessive (ARG)
X-linked recessive (hemophilia)
X-linked dominant (hypertrichosis)
Chromosomal conditions
Non-disjunctions
Chromosomal translocations (Robertsonian translocation)
Chromosomal Inversions
Multifactorial conditions
Caused by multiple genes and environmental factors
Examples: Diabetes, heart disease, cancer
What is the goal of medical geneticists?
To diagnose which category a “disease phenotype” falls into
What is OMIM and how is it used by medical geneticists?
OMIM stands for Online Mendelian Inheritance in Man.
It's a free online database at https://www.omim.org.
Contains detailed information about human genes and genetic disorders.
Useful for finding:
Chromosomal locations
Gene functions
Known mutations
Associated phenotypes
Links to primary literature for further research
Can OMIM be used for non-disease traits?
Yes! OMIM also catalogs information on non-disease phenotypes, such as traits that vary in the general population.
It includes:
Gene functions
Chromosomal location
Mutations and their effects
Associated traits or phenotypes
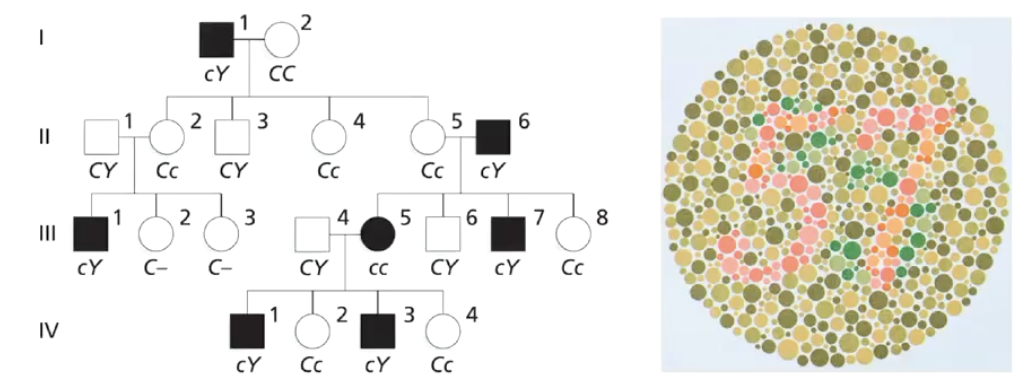
What is the purpose of pedigree analysis in genetics?
Pedigree analysis helps identify patterns of inheritance within families.
Genetic counsellors use pedigrees to assess risk of inherited diseases.
It is often used w hen physicians suspect a genetic condition and refer patients for genetic counselling.
Especially useful for couples considering starting a family.
What are the main types of genetic screening?
Newborn genetic screening
Prenatal genetic screening
Non-invasive protocols
Invasive protocols
What is newborn genetic screening, and how is it performed?
A standard protocol in many countries.
Involves a heel-prick to collect a blood sample shortly after birth.
The blood is analyzed for genetic and physiological abnormalities.
Helps identify treatable conditions early.
What condition led to the development of newborn genetic screening?
Phenylketonuria (PKU) was the first condition screened in newborns.
Children with PKU appear normal at birth, symptoms appear after a few months.
It’s an autosomal recessive disorder caused by absence of the enzyme phenylalanine hydroxylase which converts phenylalanine (Phe) to tyrosine
Leads to buildup of phenylalanine which is toxic to nervous system, causing severe mental and developmental impairment if untreated.
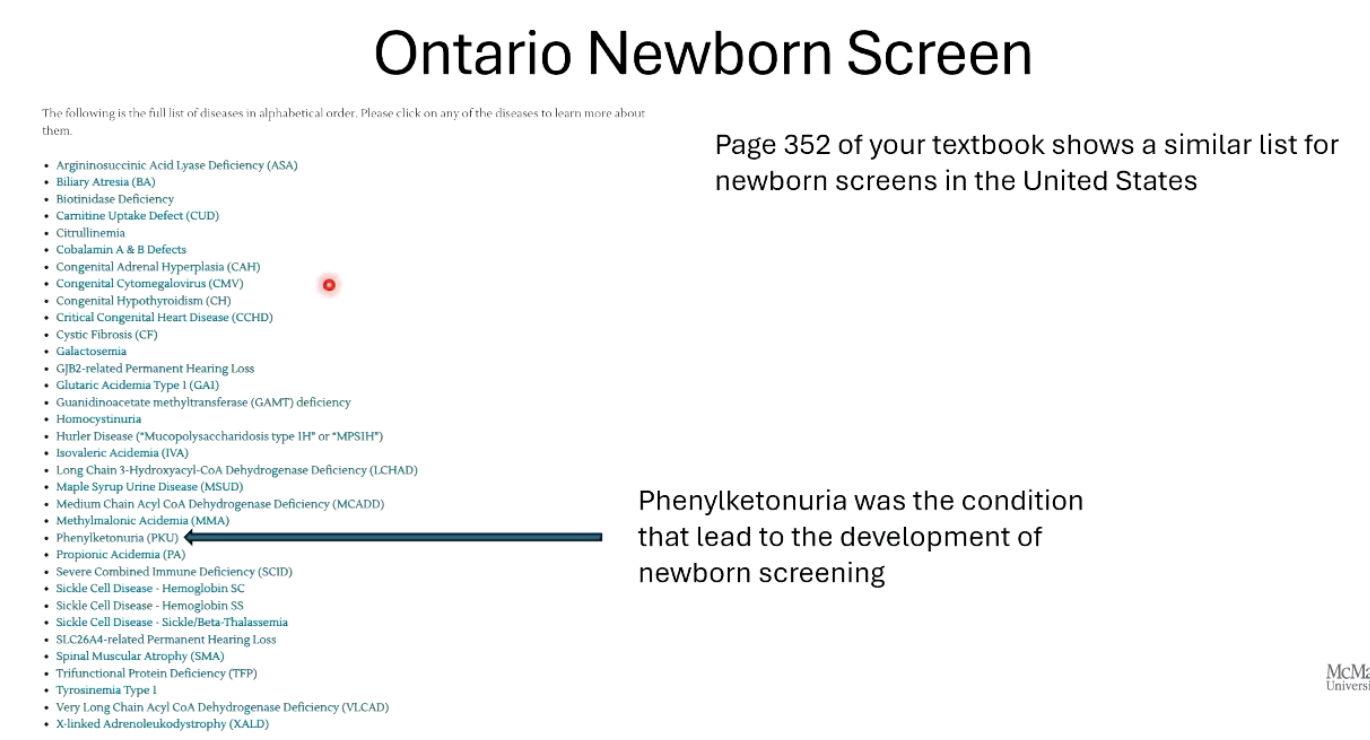
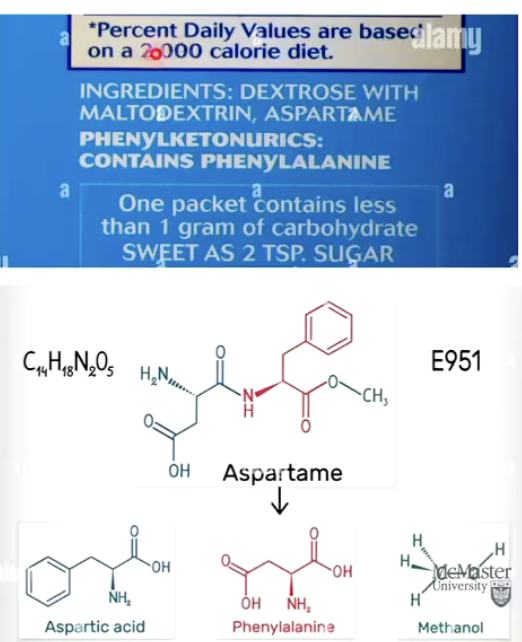
How is PKU managed?
Managed with a low-protein diet.
Avoiding aspartame (an artificial sweetener containing phenylalanine).
Early detection and treatment allow children with PKU to lead normal lives.
Estimated that since 1960s more than 50000 PKU babies lead to normal lives.
What is prenatal genetic screening?
Genotyping a child before birth to detect inherited conditions.
Includes both non-invasive and invasive methods w/ small risk of harming fetus.
Invasive encouraged if non-invasive methods are inconclusive and if there are concerns about child inheriting condition that runs in family.
Used especially when there's a family history of genetic conditions.
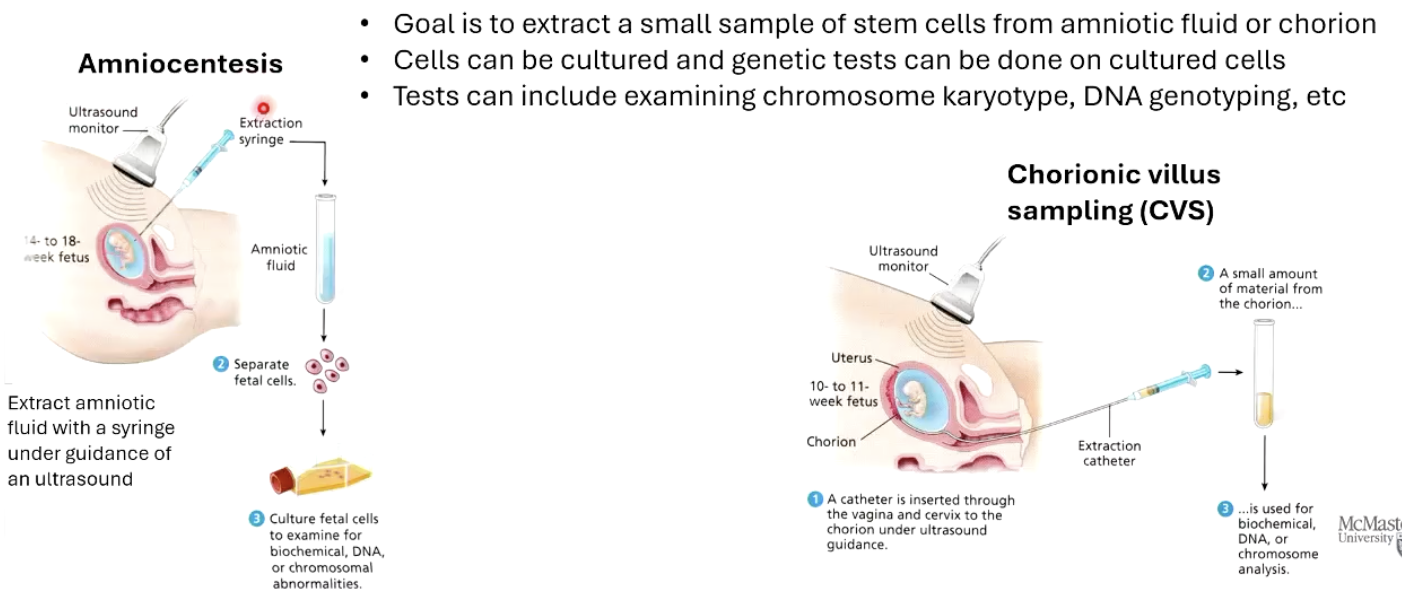
What are two examples of invasive prenatal tests?
Amniocentesis – extracts small sample of stem cells from amniotic fluid using a syringe guided by ultrasound.
Chorionic Villus Sampling (CVS) – extracts stem cells from the placenta (chorion).
Cells can be cultured and genetics tests can be done:
Tests include examining chromosome karyotype, DNA genotyping, etc.
What are examples of non-invasive prenatal tests?
Ultrasound imaging – detects physical abnormalities like Down syndrome or neural tube defects (by examining head and spine).
Fetal cell sorting – isolates fetal cells from the mother's blood for genetic testing. Requires further development.
Non-invasive methods are safer, but may be less conclusive.
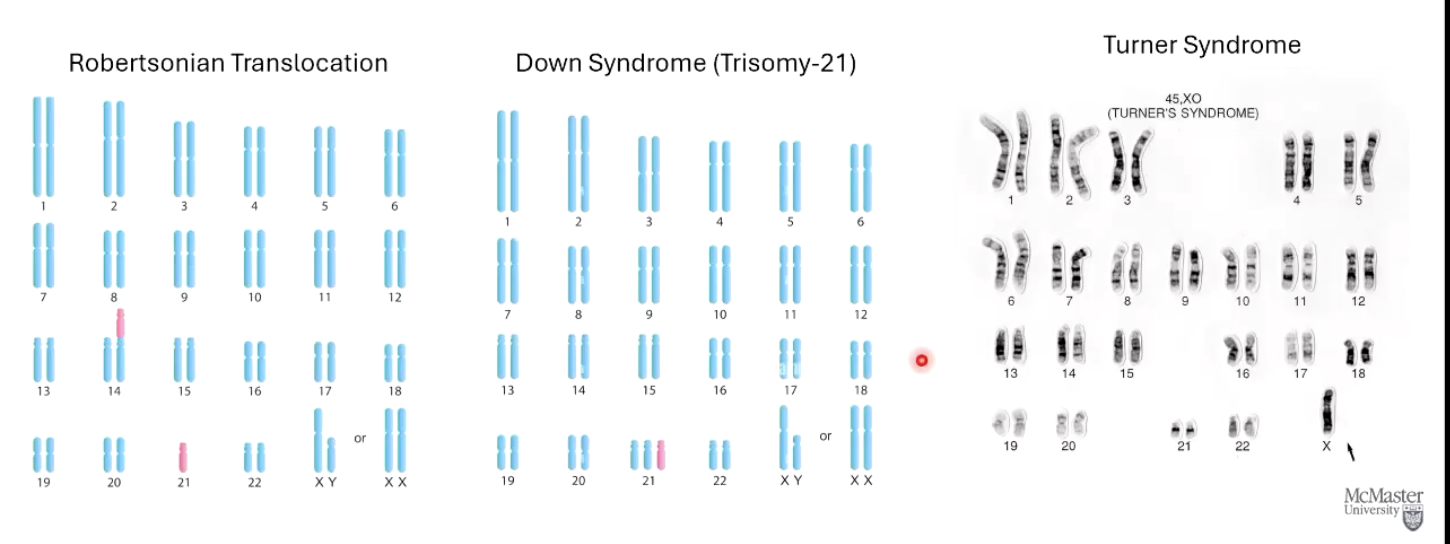
What can the karyotype detect?
Robertsonian Translocation
Chromosome 21 translocates to chromosome 14
Down syndrome (Trisonomy-21)
3 chromosome 21s
Turner Syndrome
Female missing X chromosome
No Y chromosome
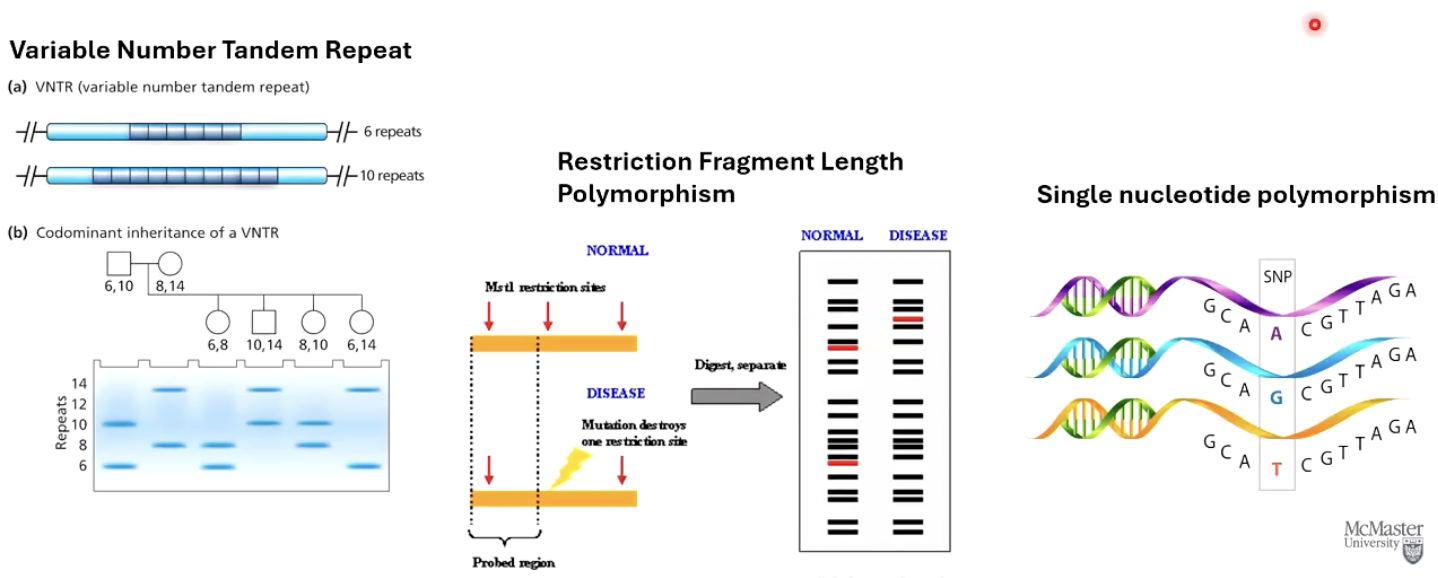
What kinds of genetic markers are used in DNA tests?
Variable Number Tandem Repeats (VNTR)
Restriction Fragment Length Polymorphism (RFLP)
Single Nucleotide Polymorphisms (SNPs)
These markers are linked to disease-causing genes and used for diagnostic purposes.
What is Huntington’s Disease (HD)?
A neurodegenerative, autosomal dominant condition.
Symptoms appear between ages 30–50 and start off with mood changes and mental abilities, and rapidly advance and lead to inability to talk, dementia, depression, and immobility.
Caused by too many CAG repeats in a gene. More than 34 repeats leads to disease.
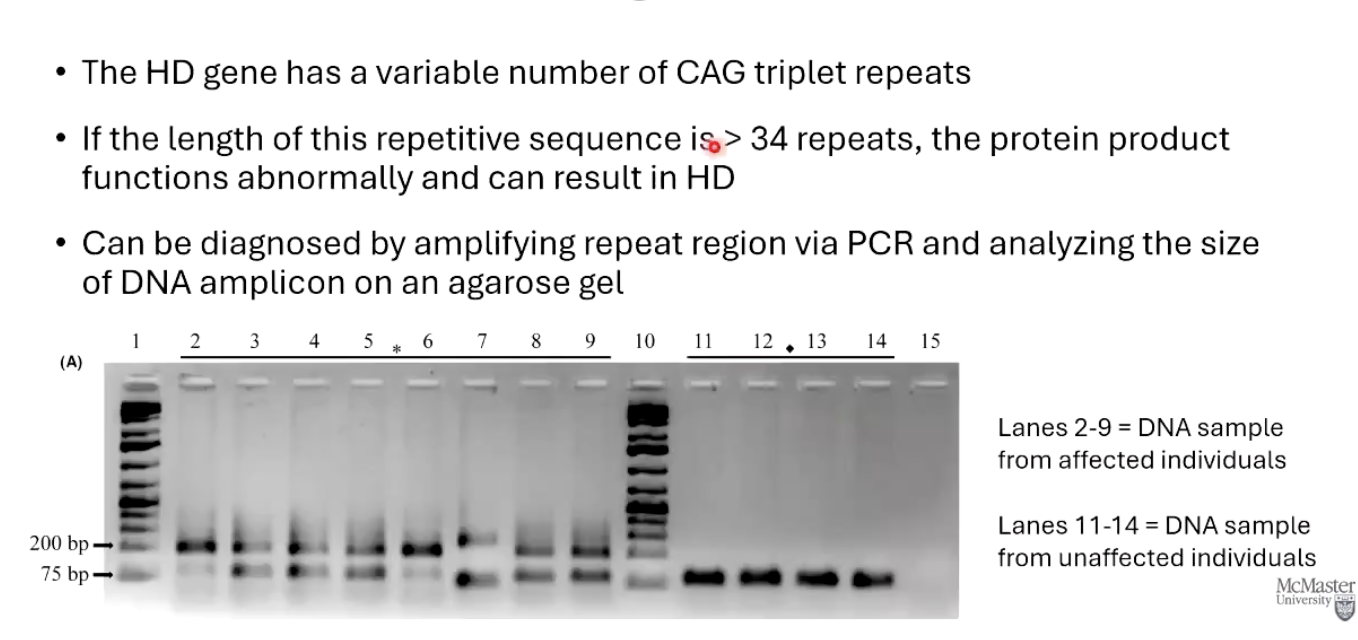
How is Huntington’s Disease tested for genetically?
Uses PCR to amplify the CAG repeat region.
The number of repeats is analyzed by running the DNA on an agarose gel.
More than 34 CAG repeats indicates presence of the disease allele.
What are the ethical concerns related to genetic testing, especially for diseases like HD?
Knowing your genetic status can be psychologically stressful.
Raises questions like:
Would you want to know your status if your parent had HD?
Would you test your unborn child?
Would being a carrier change how you treat your child?
Not everyone may want to know their genetic fate.
What is eugenics, and how is it related to genetic screening?
Eugenics is the idea of improving humanity by encouraging or discouraging certain people to have children.
Widespread genetic screening and editing may unintentionally support eugenic ideas.
Raises concerns about discrimination, denial of healthcare or insurance, and employment bias based on genetic data.

What are the benefits of genetic screening?
Identifies treatable rare diseases in newborns.
Empowers individuals to make lifestyle changes for better health.
Can reconnect families through shared genetics.
Fuels research for advanced therapies, such as personalized cancer treatment.
Overall, it improves health outcomes and knowledge.