Module 2 FINAL - Central Lines, NG/OG Tubes, Chest Tubes, Pacemakers and Respiratory Tubes
1/99
Earn XP
Description and Tags
Flashcards about Central Lines, NG/OG Tubes, Chest Tubes, Pacemakers and Respiratory Tubes based on lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What are central venous catheters (CVCs)?
Long, flexible catheters with the tip in the SVC, cavo-atrial junction, or right atrium for long-term infusion of multiple medications.
Why are CVCs used?
For long-term infusions, frequent blood draws, avoiding peripheral irritation, and critical care situations requiring multiple access points.
What are the three main categories of central lines?
Non-Tunneled Catheters, Tunneled Catheters, and Peripherally Inserted Central Catheters (PICCs)
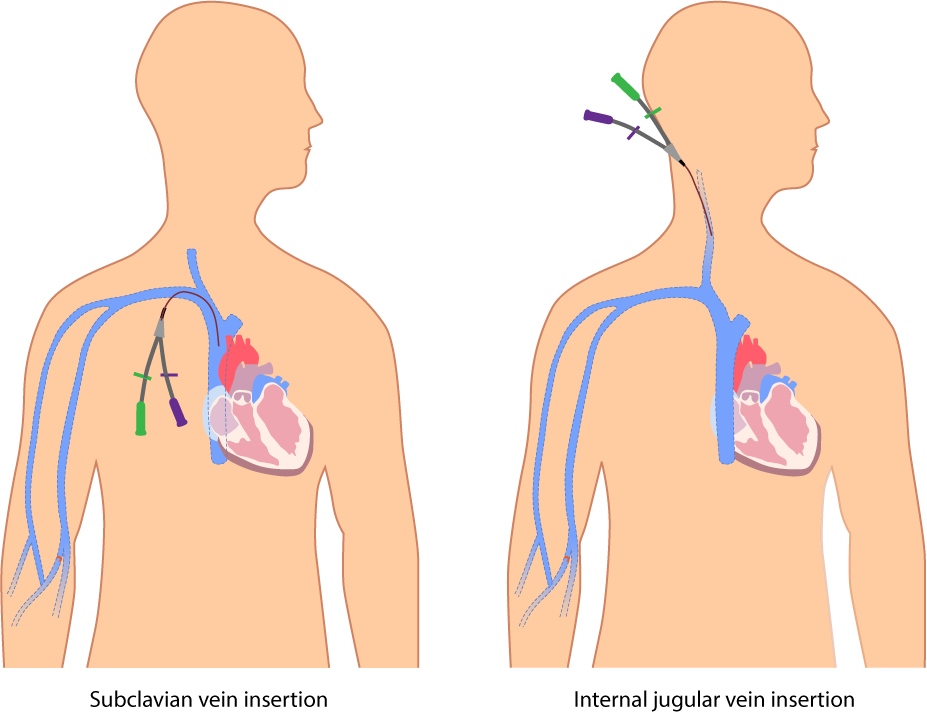
Where are non-tunneled catheters typically inserted?
Subclavian or jugular veins—preferably the right side.
What is the purpose of NTCs (Non Tunneled Catheter)?
Fast, reliable venous access in acute care settings for medications and blood draws.
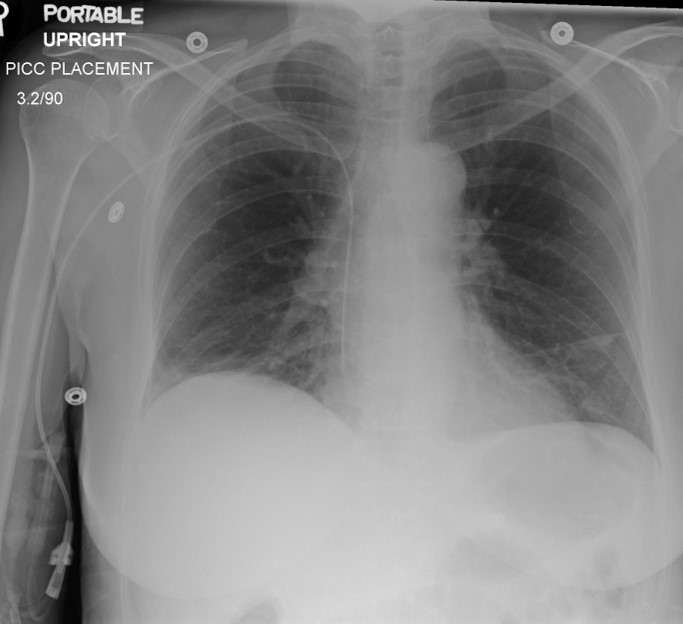
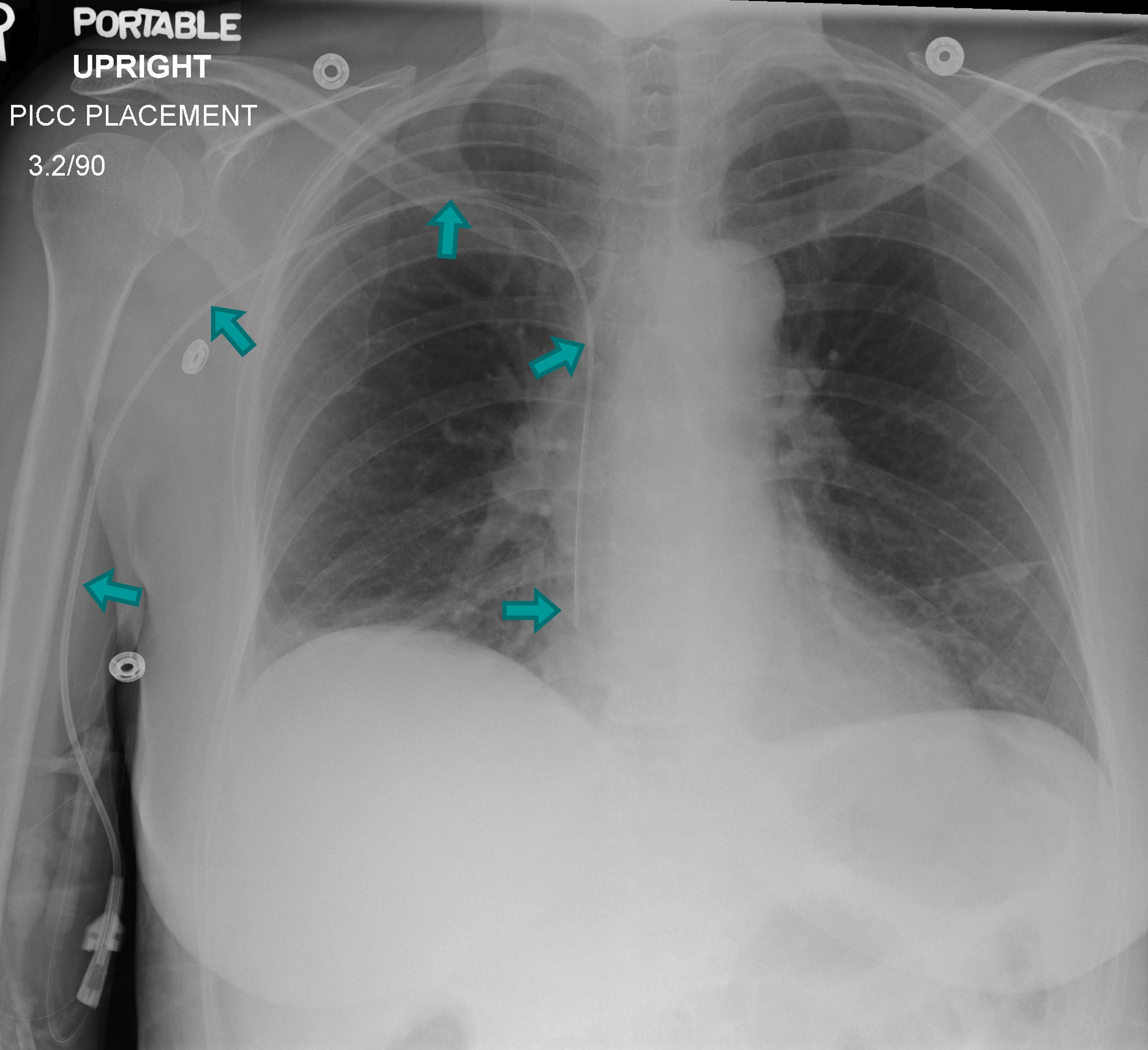
What must occur before using an NTC (Non Tunneled Catheter)?
Radiographic confirmation of correct placement.
What distinguishes tunneled catheters from NTCs?
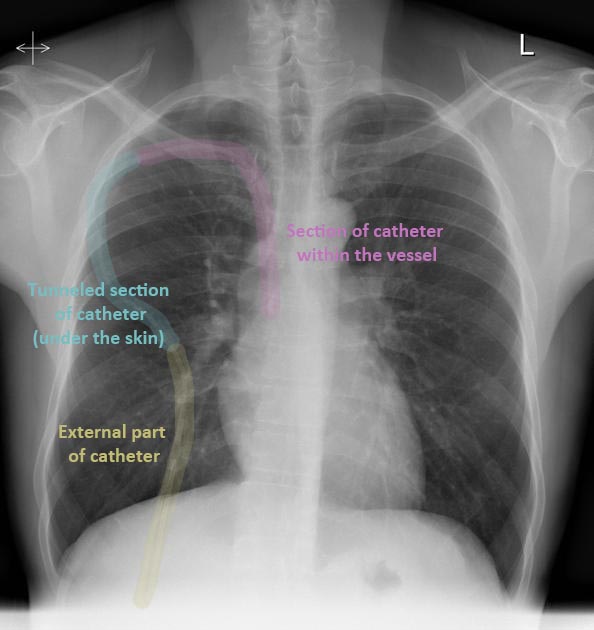
They are tunneled under the chest skin, reducing infection risk and dislodgement.
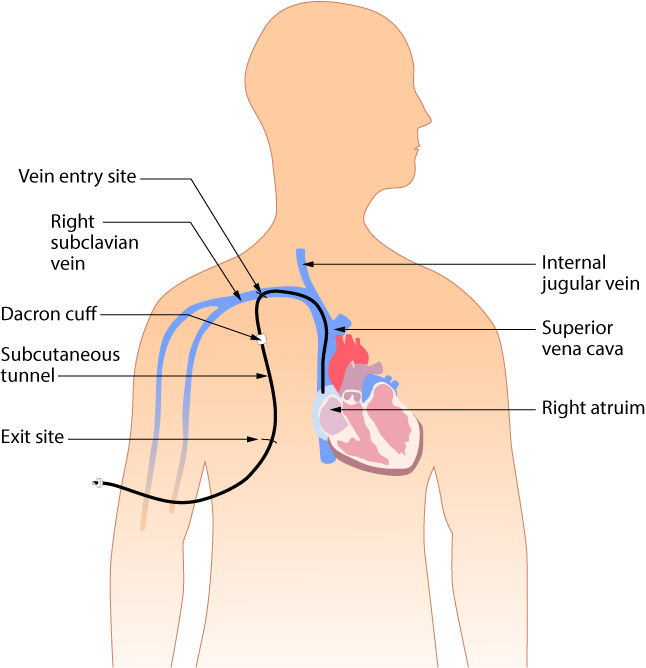
Who typically uses tunneled catheters?
Patients undergoing long-term outpatient therapy (e.g., chemotherapy, dialysis).
Name common tunneled catheter types.
Hickman, Broviac, and Permacath.
How is a tunneled catheter placed?
Two incisions made; forceps create a tunnel; catheter is threaded subcutaneously between vein and exit site.
What is a Port-a-Cath?
A fully implantable tunneled catheter with a self-sealing internal port and no external tubing.
How is a Port-a-Cath accessed?
With special needles and tubing; the needle is removed after medication delivery.
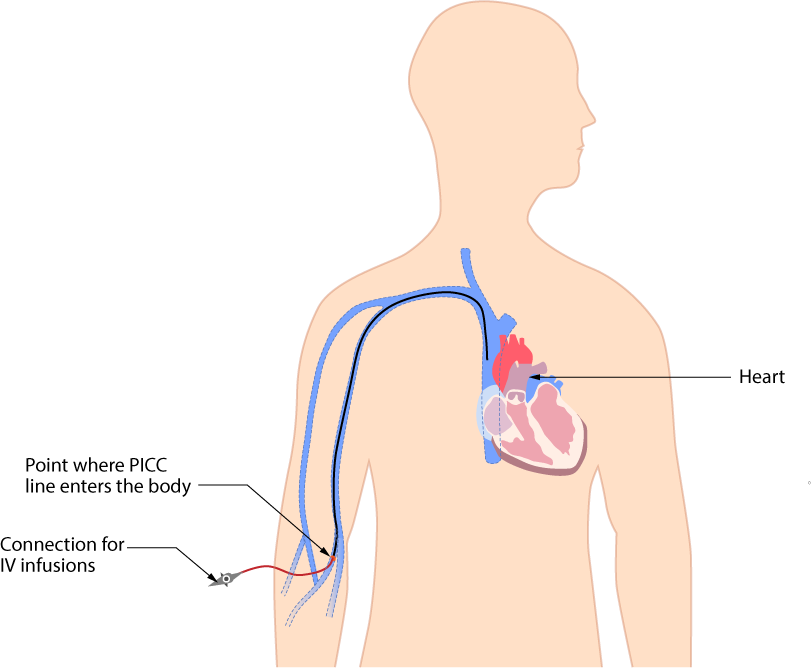
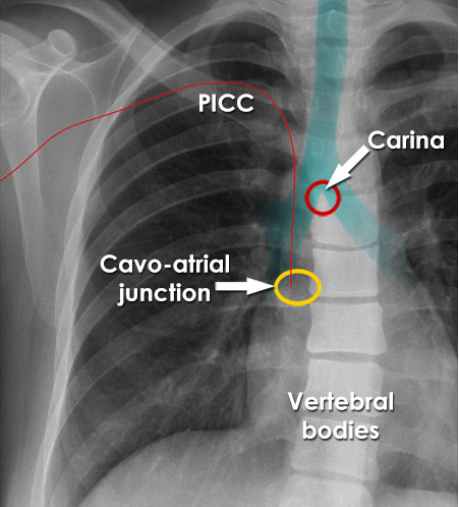
What does PICC stand for?
Peripherally Inserted Central Catheter.
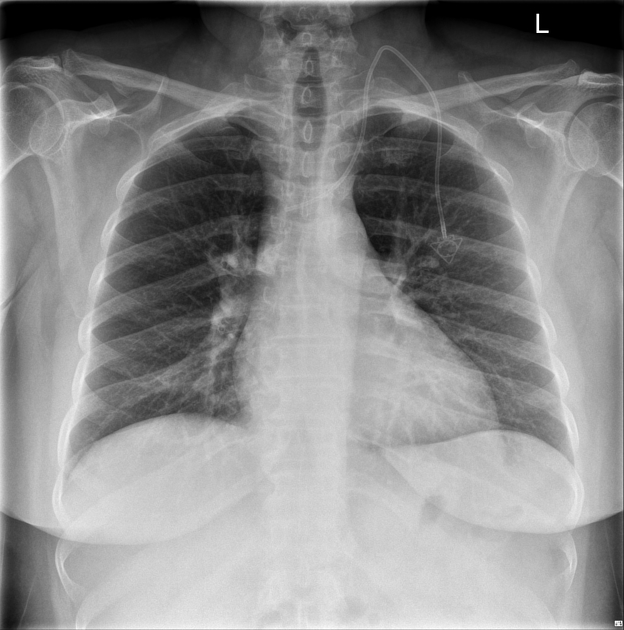
Where is a PICC line inserted?
In the upper arm, usually the basilic vein.
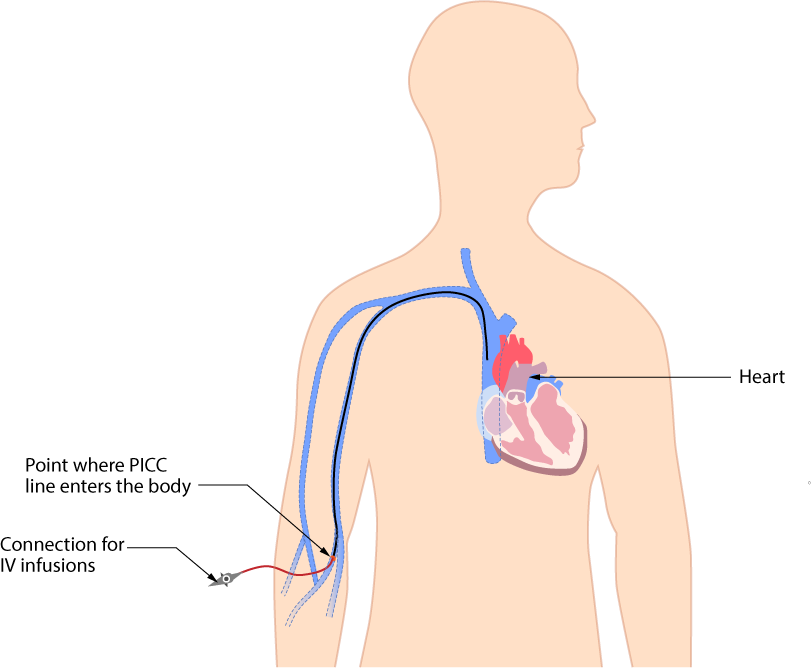
What are the advantages of PICCs?
Lower infection risk, ease of insertion, and long or short-term use.
What should MRTs ensure during imaging of CVCs?
Adequate mediastinal visualization, correct positioning, and no line dislodgement.
What must MRTs do after imaging?
Inform staff of image availability and possible malpositioning.
Can MRTs access central lines?
No, they are not qualified to access or manipulate any central line.
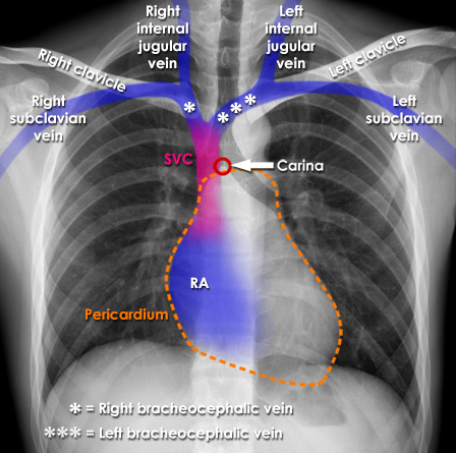
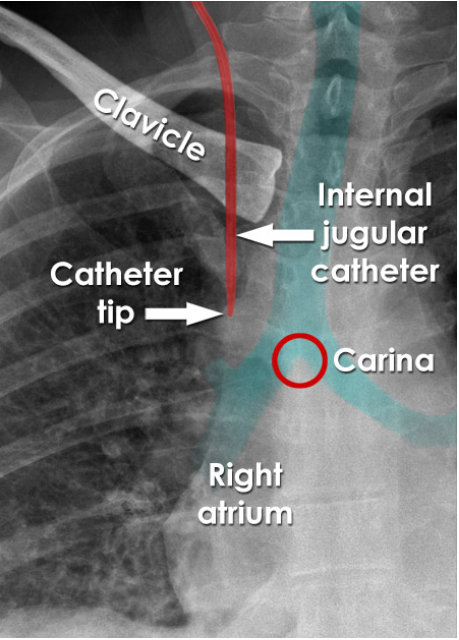
What is the ideal placement for most CVCs?
Between the SVC and right atrium.
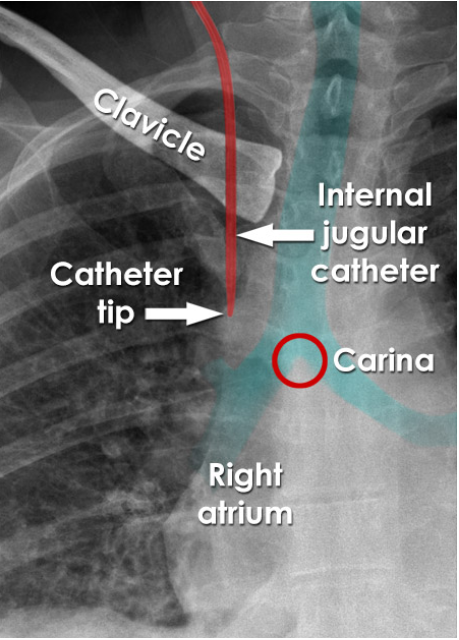
What anatomical landmark helps confirm CVC placement?
The carina at T4–T5.
Why avoid placing catheters before the SVC?
Increased risk of infection and thrombosis.
When is SVC placement appropriate?
For maintenance medications and fluids.
Where is the cavo-atrial junction radiographically?
~2 vertebral bodies below the carina.
What are the risks of atrial placement?
Cardiac tamponade, tissue erosion, and perforation.
Where do malpositioned CVCs often end up?
Jugular vein (wrong direction), internal mammary, azygos/hemiazygos veins, or extravascular.
What are complications of malpositioning?
Perforation, thrombosis, catheter dysfunction, and cranial injection.
What is the purpose of PACs (Pulmonary Artery Catheter)?
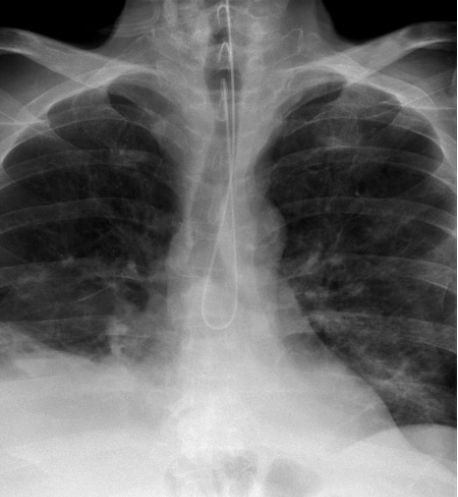
Measure cardiac output, heart pressures, and monitor oxygen saturation post-surgery or in heart failure.
Where are PACs inserted and advanced to?
Inserted via subclavian/jugular/femoral vein and floated into the pulmonary artery.
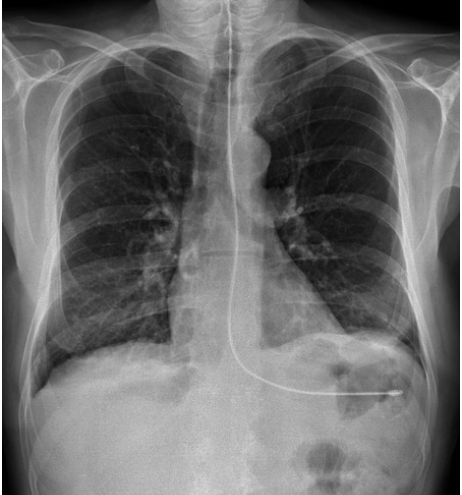
How do PACs (Swan Ganz) appear on radiographs?
Make a U-turn in the heart shadow, with the tip in the pulmonary trunk, just below the carina.
What is the MRT’s role during Swan-Ganz placement?
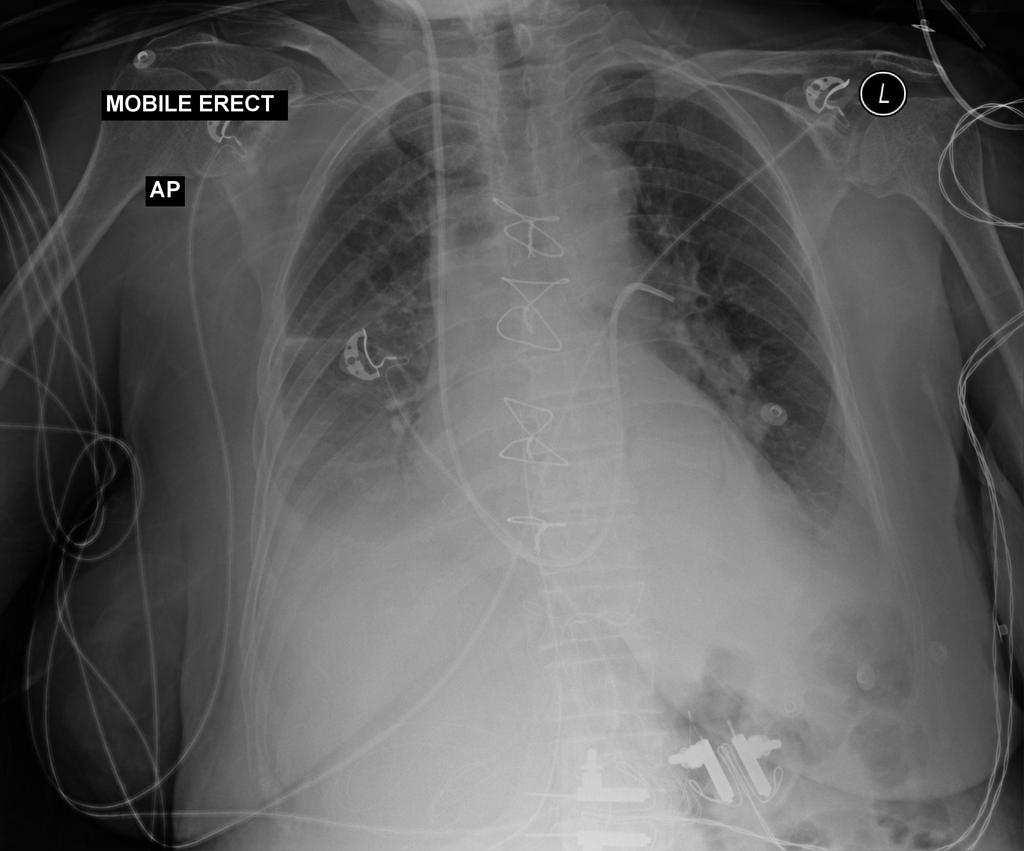
Assist with mobile imaging for placement and ensure careful positioning without dislodging the catheter. (Image - Swan-Ganz in Left Pulmonary Artery)
What must MRTs communicate post-insertion?
Image availability and any concerns about misplacement.
Why are CVCs manufactured with radiopaque strips?
To allow radiographic visualization for placement confirmation and ongoing monitoring.
What must MRTs evaluate in a CVC radiograph?
Tip location, patient rotation, beam alignment, and mediastinal visualization.
How can MRTs detect catheter migration?
By comparing the current radiograph with previous imaging.
Can CVCs be used for contrast injections in imaging?
Yes, if they are pressure-rated and color-coded for that use.
Who is responsible for accessing and disconnecting CVCs during imaging procedures?
A radiology nurse or the patient’s primary nurse—not the MRT.
What should MRTs do if the patient has a power-injectable port?
Confirm with the patient or care team and ensure it's clearly documented or labeled.
Why is the right side preferred for CVC insertion?
It offers a more direct route to the SVC, reducing complications.
Why must CVC use be delayed until placement is confirmed?
To avoid complications like infusion into incorrect vessels or extravascular spaces.
How does the tunneling of a catheter reduce infection risk?
The subcutaneous path creates a barrier that reduces bacteria migration.
What are the risks of an improperly placed catheter tip?
Infection, thrombosis, cardiac tamponade, tissue erosion, or vascular perforation.
What are signs of catheter migration or misplacement on a radiograph?
Tip above carina, into wrong vessel (e.g., jugular), or coiled.
What is the consequence of a CVC tip in the right atrium?
Increased risk of cardiac perforation and tamponade.
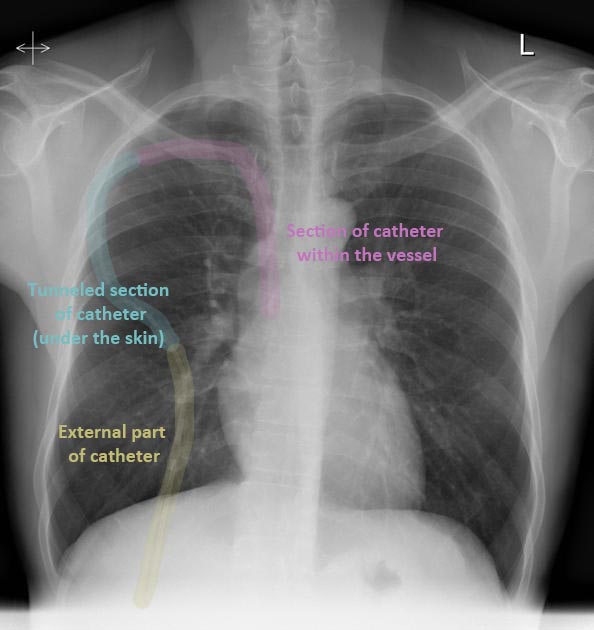
What is a Hickman or Broviac line used for?
Long-term therapies like chemotherapy or parenteral nutrition. (image shows hickman line)
What makes a Port-a-Cath unique?
It is fully implanted under the skin, with no external tubing.
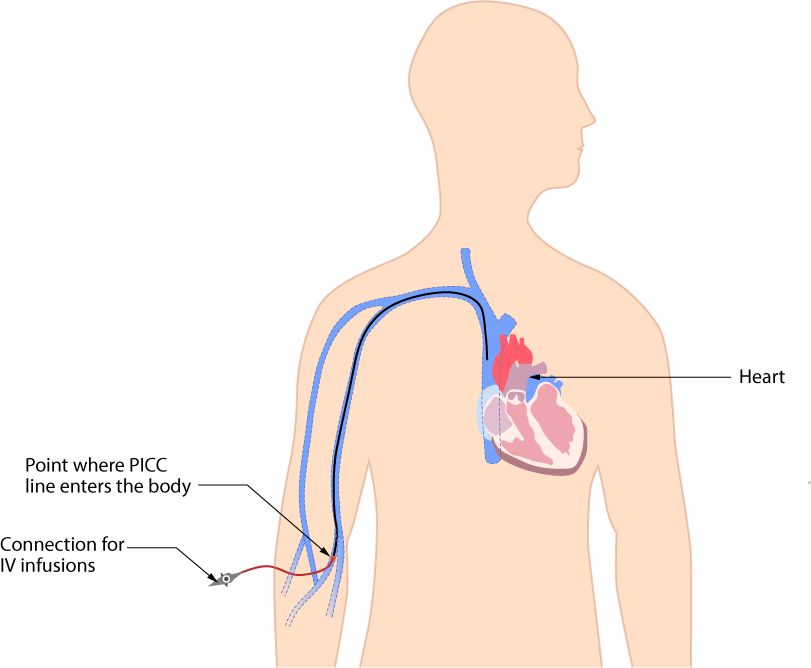
What makes PICC lines advantageous for outpatient care?
They're easier to maintain, have fewer complications, and don’t require surgical insertion.
What does the balloon tip on a Swan-Ganz catheter do?
It helps float the catheter through the heart chambers into the pulmonary artery.
What vital functions does a PAC (Swan Ganz) monitor?
Cardiac output, pulmonary artery pressures, left heart diastolic pressure, and blood oxygenation.
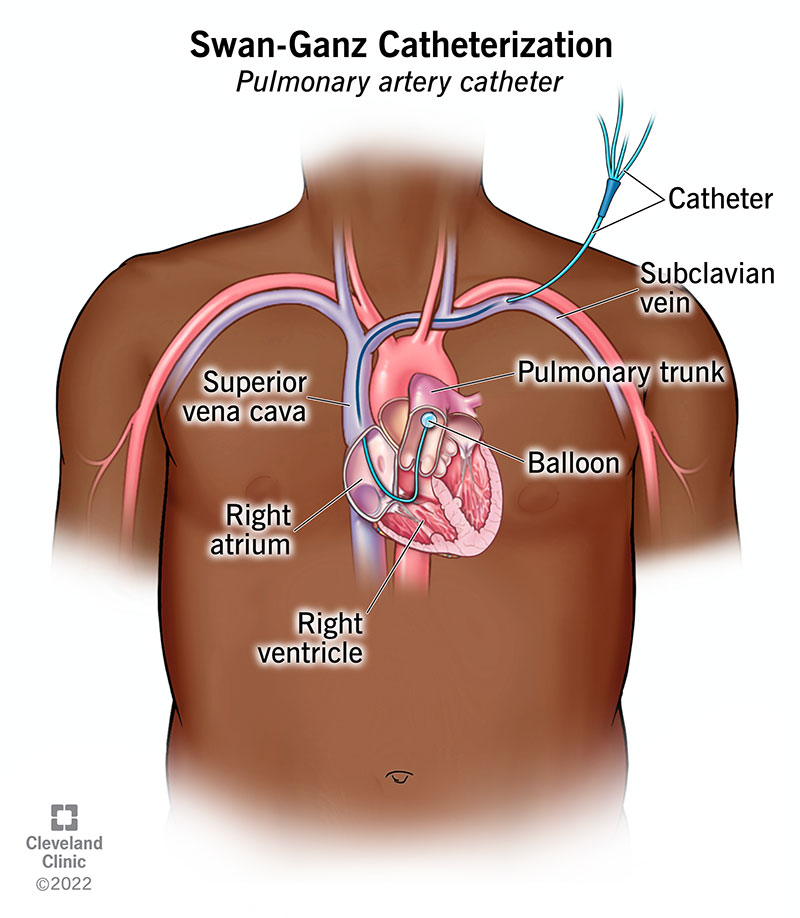
Where should the tip of a PAC (Swan Ganz) be located radiographically?
Within the pulmonary trunk, just below the carina, visible as a looped line in the cardiac silhouette.
Why is it important for MRTs to notify the care team after imaging?
To prevent use of a malpositioned catheter and ensure rapid intervention if needed.
Why must MRTs avoid repositioning patients aggressively post-insertion?
Sudden movement could displace or damage the catheter.
What is the MRT’s responsibility if the catheter appears malpositioned?
Do not use the line; notify the appropriate care team immediately.
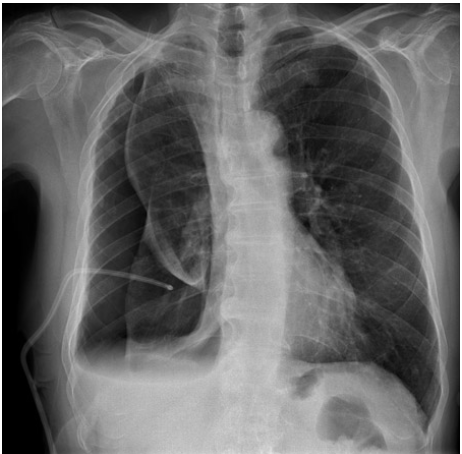
What are NG and OG tubes used for?
NG (nasogastric) and OG (orogastric) tubes are used when a patient cannot swallow safely, often for feeding or gastric decompression.
How are NG and OG tubes inserted?
NG through the nose, OG through the mouth.
What are clinical indications for NG/OG tubes?
Stroke with aphasia, decreased consciousness, cognitive decline, esophageal or oral tumors.
How are NG/OG tubes used in overdoses?
To deliver neutralizing agents like activated charcoal.
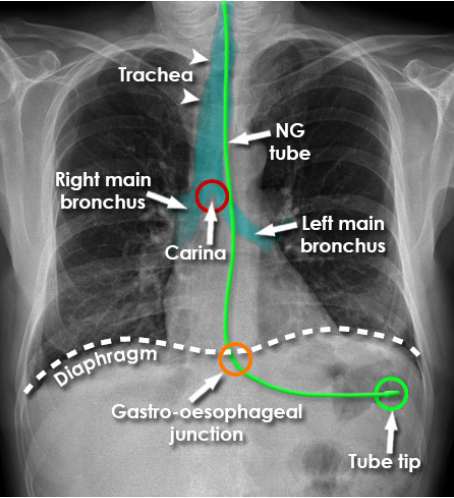
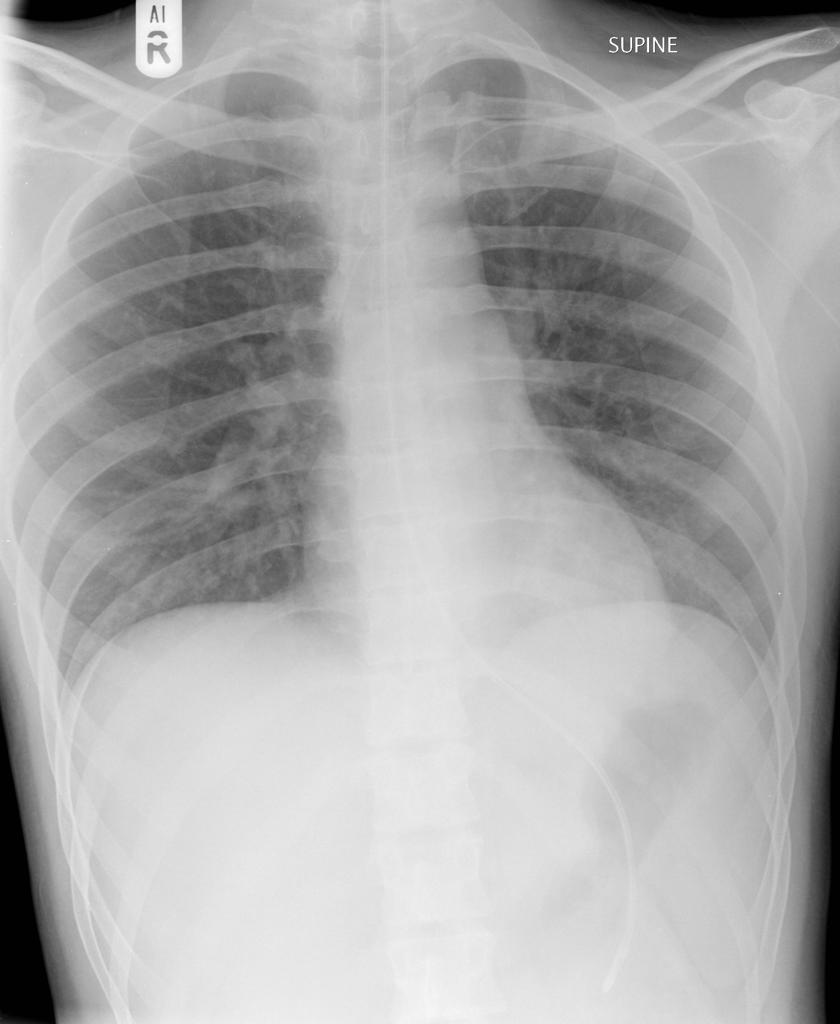
How is NG/OG tube placement confirmed?
Via mobile chest radiograph that includes the stomach.
What should the MRT do if feeding is ongoing during radiography?
Pause the feeding to avoid aspiration or disconnection.
What is the ideal location of the NG/OG tube tip?
At least 10 cm below the diaphragm, within the stomach, over the gastric bubble.
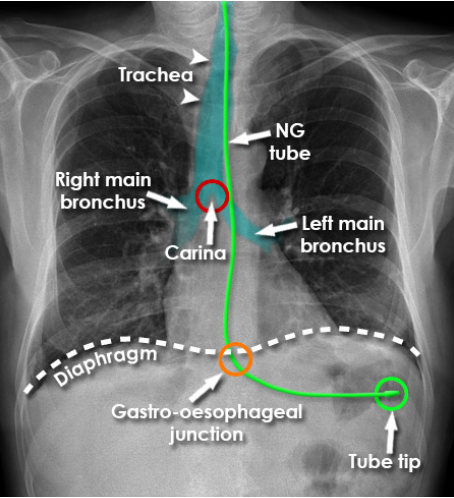
How does the tube appear radiographically?
It should be parallel to the spine, curve into the stomach, and end with the weighted tip angled downward.
What complications may result from misplacement?
Aspiration, pneumothorax, esophageal perforation, hemorrhage, or death (rare).
What might cause mispositioned NG/OG tubes?
Uncooperative patients, unusual anatomy, incorrect tube length insertion.
Where do NG/OG tubes commonly misplace?
Right bronchus, lung, or coiled in the esophagus.
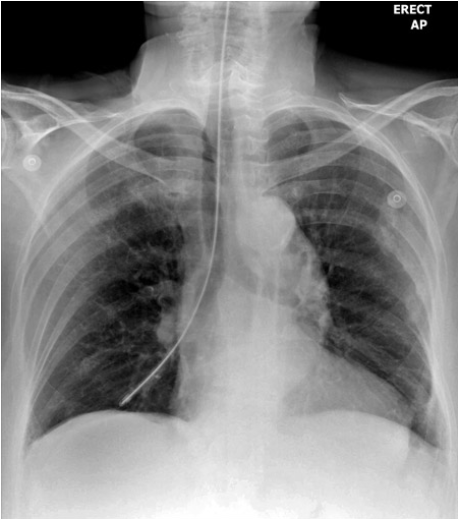
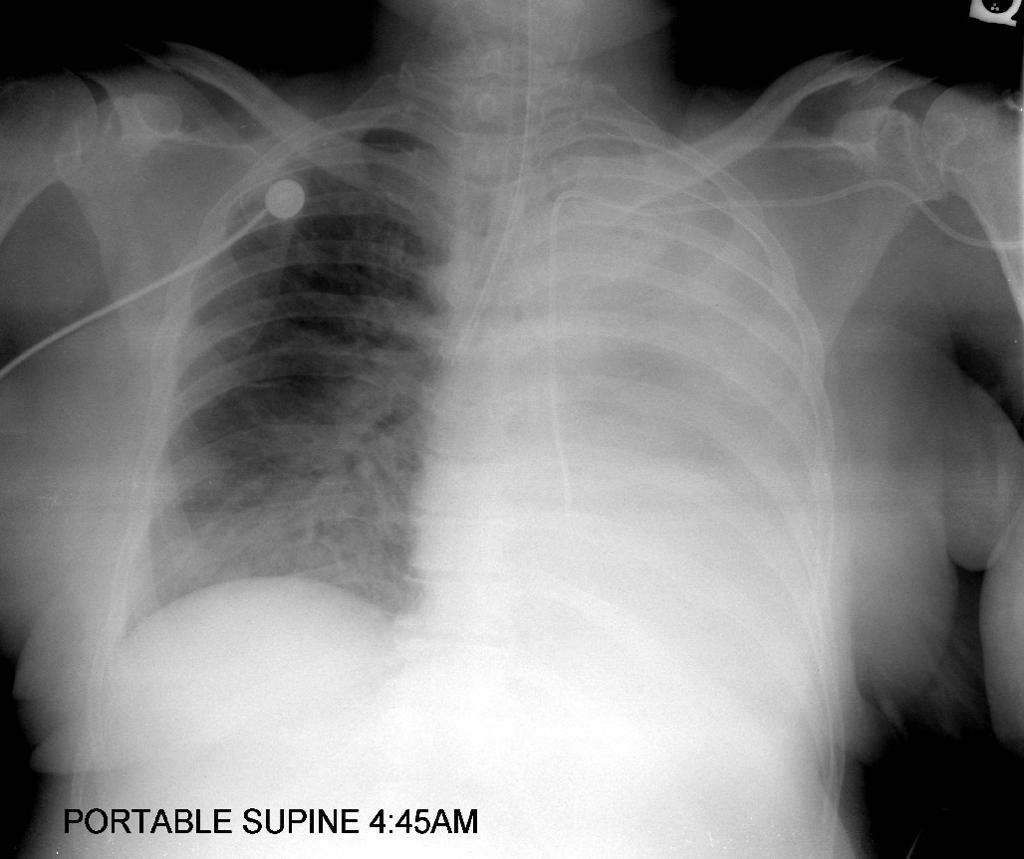
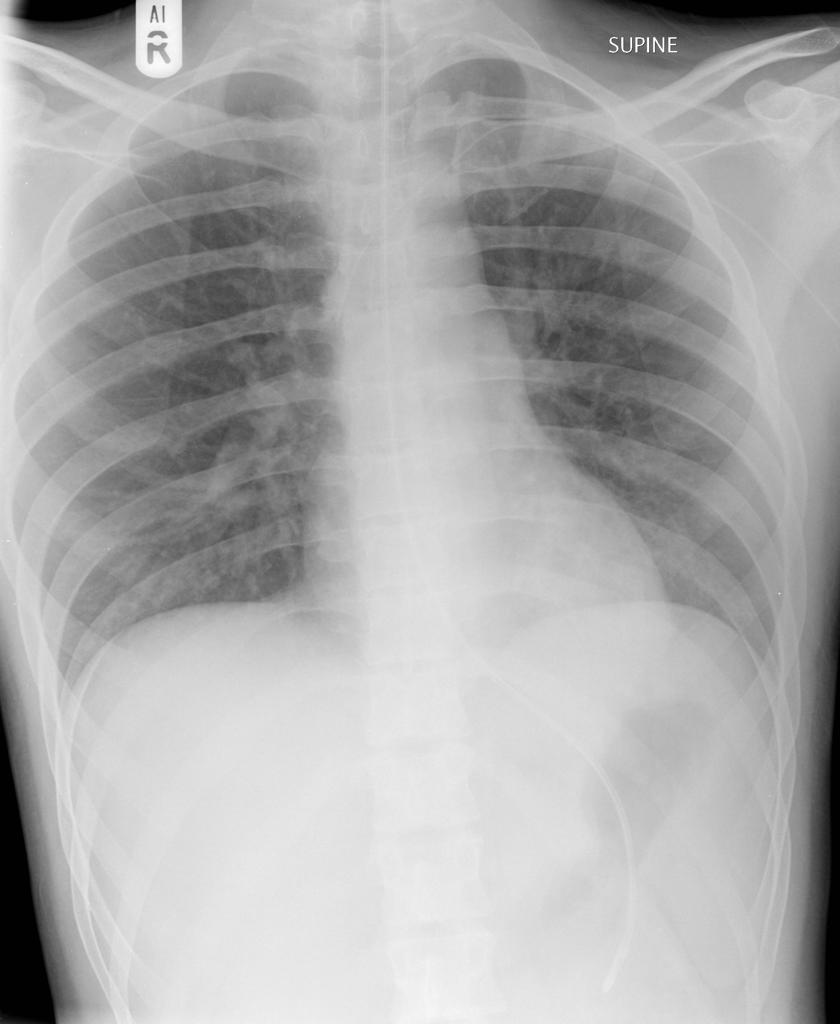
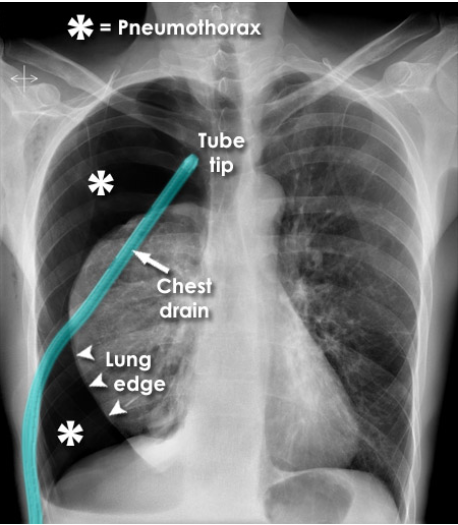
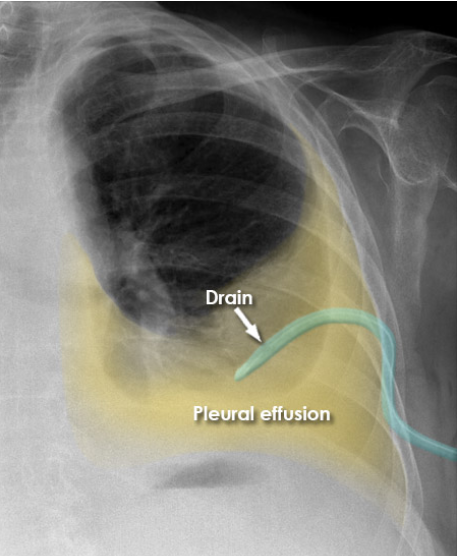
What is the primary purpose of chest tubes?
To remove air (pneumothorax) or fluid (pleural effusion) from the pleural cavity.
Where is the safe zone for chest tube insertion?
5th intercostal space, slightly anterior to the mid-axillary line.
What’s the difference between large-bore and small-bore chest tubes?
Large-bore removes air (pneumothorax); small-bore drains fluid (effusion).
Where should large-bore chest tubes be directed?
Anteriorly and superiorly into the pleural apices.
Where should small-bore chest tubes be directed?
Posteriorly and inferiorly to the dependent fluid collections.
What radiographic precaution should MRTs take with chest tubes?
Avoid pulling the tube; be cautious when placing the IR; release Kelly clamps carefully.
Where must the chest tube drain apparatus be positioned?
Below the insertion site to avoid reverse flow.
What is the purpose of the one-way valve in a chest tube drain?
To prevent air from re-entering the pleural space during exhalation.
What are potential complications of chest tubes?
Pneumothorax, tension pneumothorax, hemorrhage, and surgical emphysema.
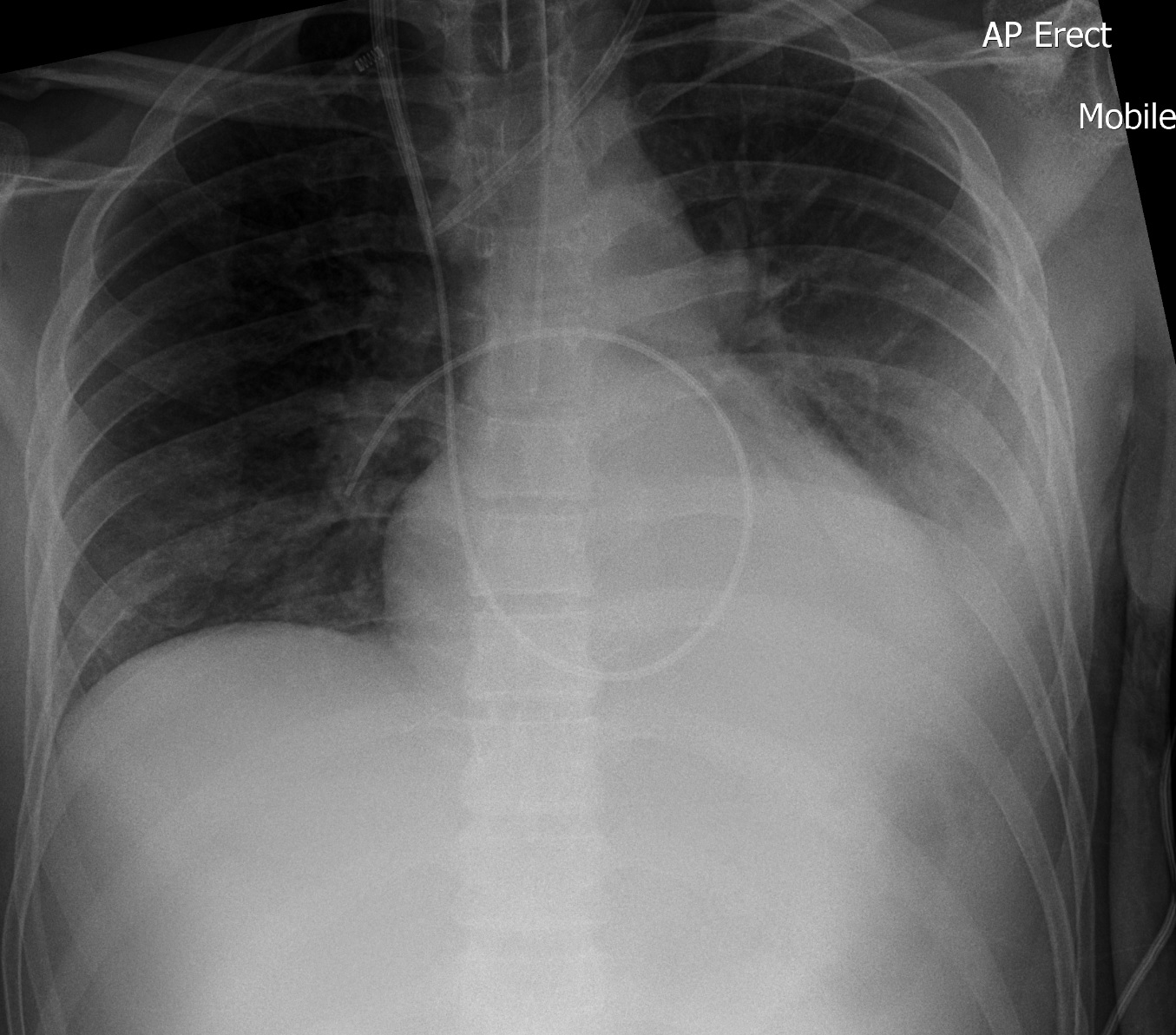
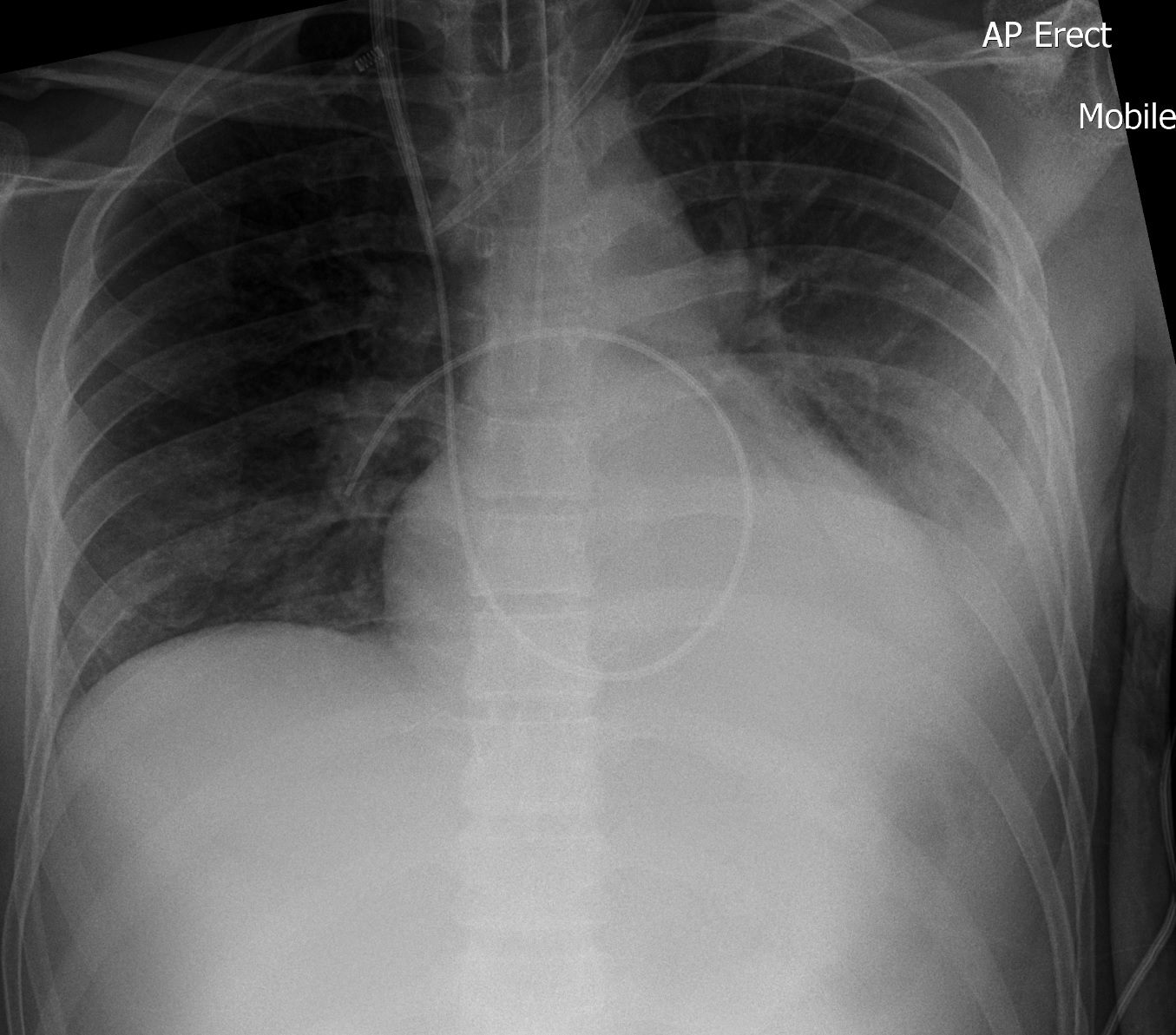
What is the function of a pacemaker?
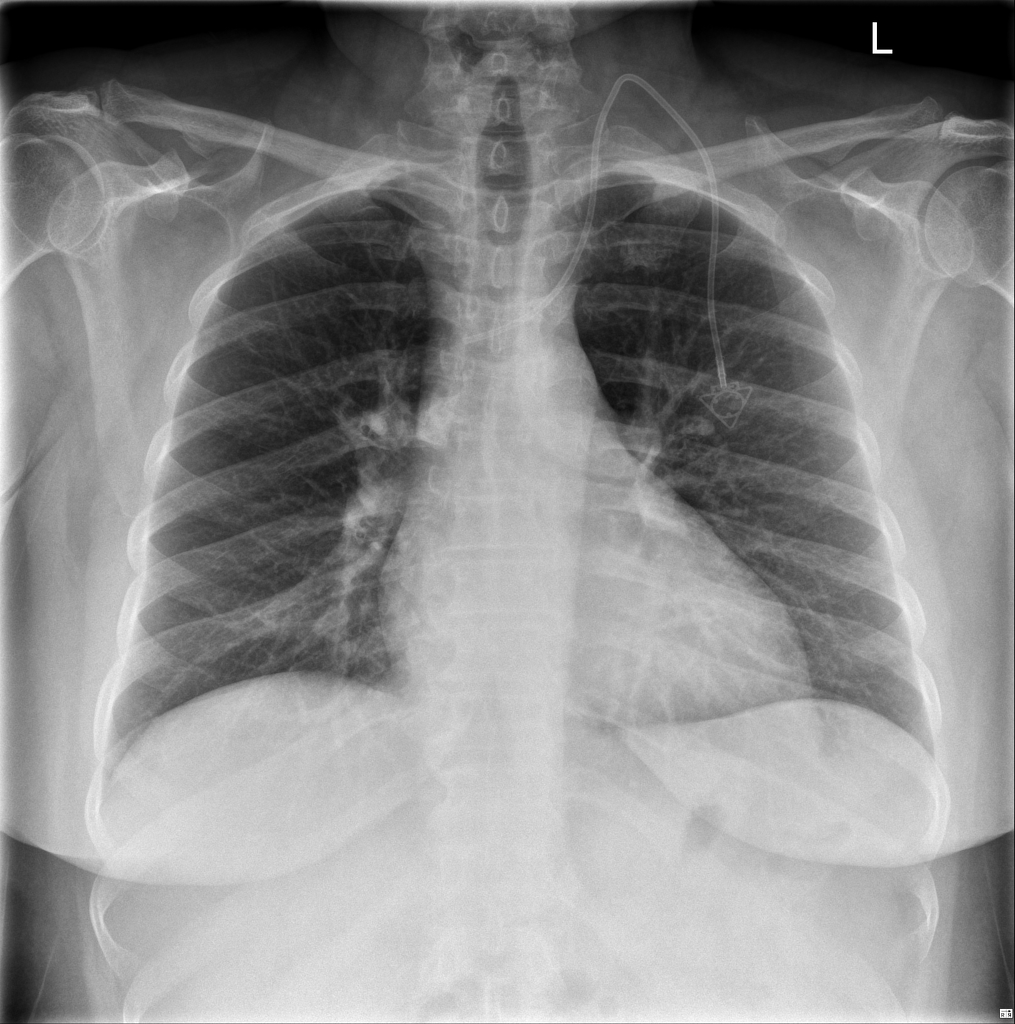
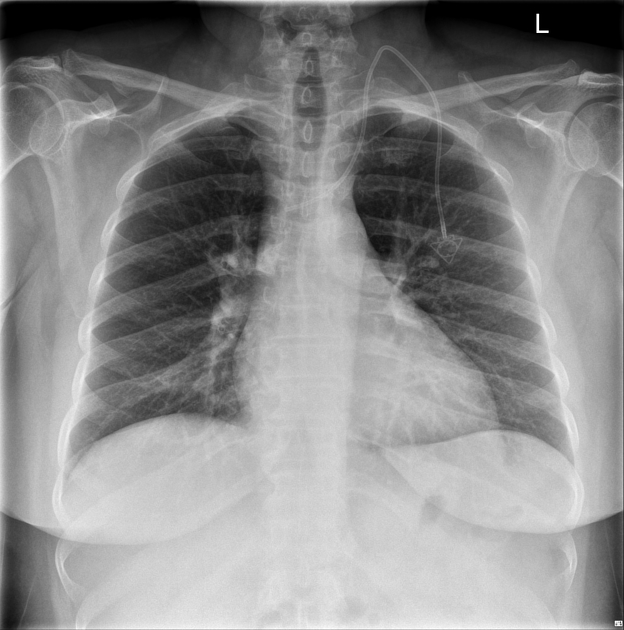
It maintains adequate heart rate and rhythm by delivering electrical impulses. (IMAGE Pneumothorax induced during insertion of pleural drainage catheter)
What symptoms do pacemakers help relieve?
Fatigue, fainting, and symptoms of arrhythmias.
What’s the difference between internal and external pacemakers?
Internal: surgically implanted; External: temporary, placed post-surgery or for testing.
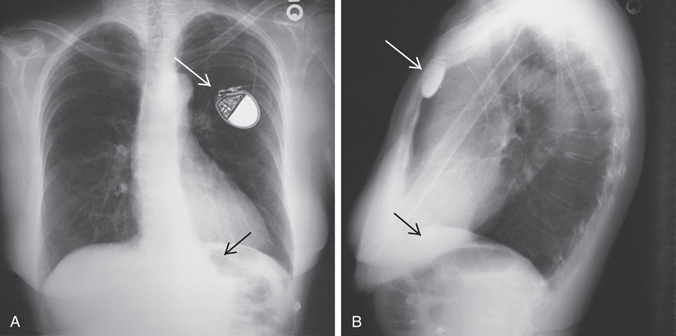
Where are pacemaker leads typically placed?
In the myocardium near electrical nodes, often via the subclavian vein.
What radiographic rule applies after pacemaker insertion?
The patient’s left arm should not be abducted or elevated for 24 hours.
What projections confirm pacemaker and lead positioning?
PA and lateral chest radiographs.
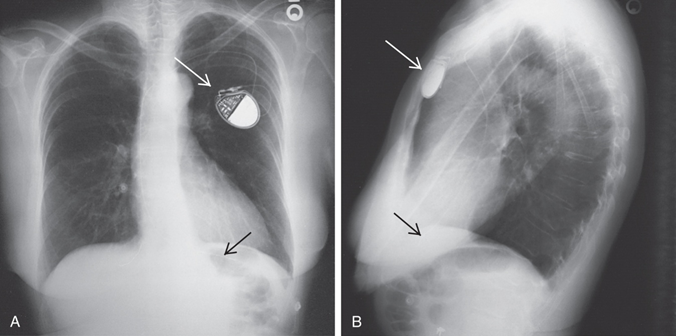
What are potential complications of pacemaker placement?
Lead dislodgement, pneumothorax, lead/generator failure, or migration.
What is the typical lifespan of a pacemaker generator?
Approximately 10 years.
What is the purpose of a tracheostomy?
To bypass upper airway obstructions such as cancer or burns, and establish a direct airway.
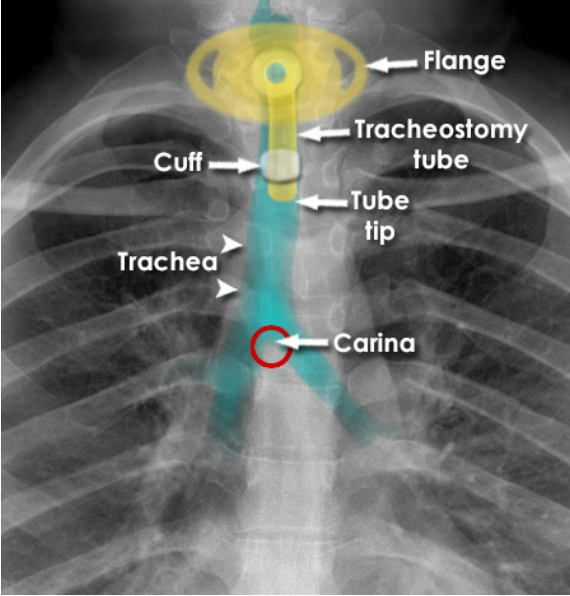
How is a tracheostomy performed?
Surgically, by creating an opening into the trachea.
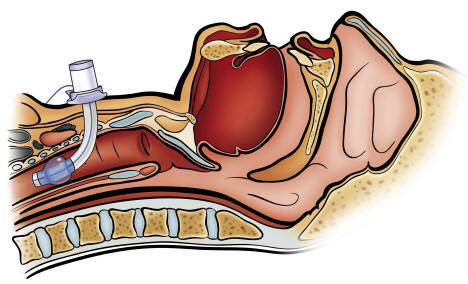
What is an endotracheal tube (ETT) used for?
Airway control during general anesthesia or respiratory collapse (e.g. ARDS, pulmonary edema).
How are ETTs inserted?
Through the mouth or nose, into the trachea.
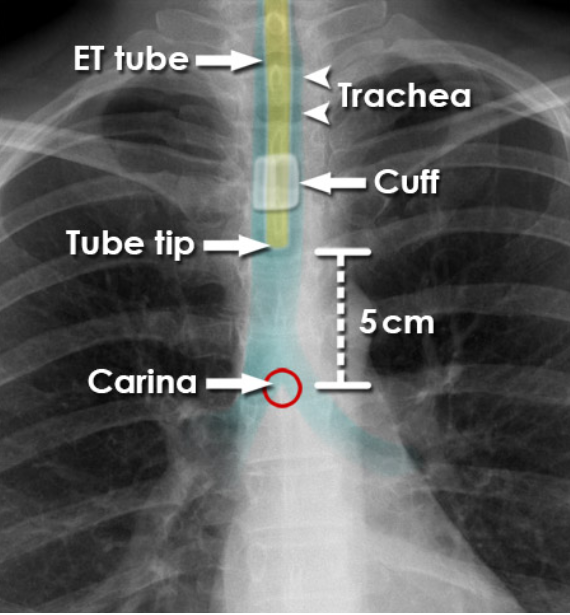
Where should the distal tip of an ET tube be located?
In the trachea, 5–7 cm above the carina in neutral neck position.
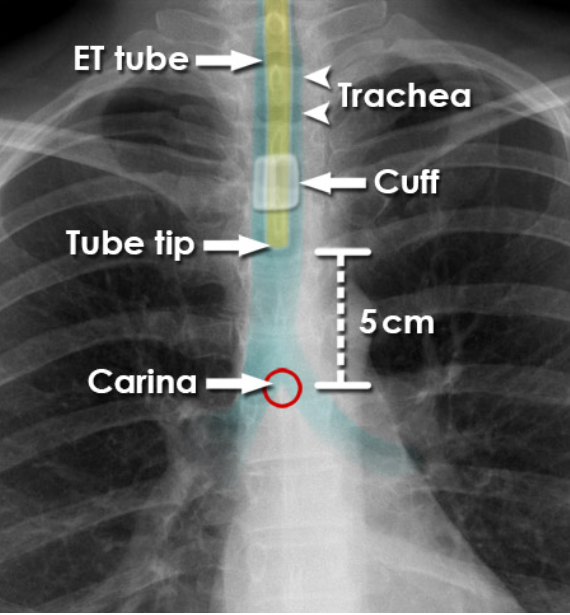
How does neck position affect ET tube tip placement?
Neck flexion or extension can cause the tube tip to move significantly.
What imaging considerations are important for ventilated patients?
Capture the image between breaths to avoid motion blur.
What are signs of ET tube misplacement?
Tip in right bronchus, high in trachea, or dislodged—potentially leading to collapse or aspiration.
Why must the MRT mark the approximate tube length before NG/OG tube insertion?
To ensure proper tube length and reduce risk of over- or under-insertion.
How should MRTs handle patients trying to remove NG/OG tubes?
Maintain a hold on the loose restraint ties when positioning to prevent accidental tube removal.
What does the radiopaque strip in NG/OG tubes help with?
It allows clear visualization of the tube path and tip on X-rays.
What should MRTs communicate if gross misplacement of an NG/OG tube is seen on the radiograph?
Inform the care team immediately to prevent potential harm.
Why is sterile technique critical when inserting chest tubes?
To prevent infection of the pleural space and surrounding tissues.
What are Kelly clamps used for in chest tube management?
To secure the chest tube to the mattress or patient’s sheet.
How do MRTs protect themselves when imaging patients with chest tubes?
By wearing gloves due to blood or fluid seepage from the insertion site.
What precaution is taken regarding arm movement after pacemaker placement?
Avoid abducting or elevating the left arm for 24 hours to prevent lead dislodgement.
Why might external pacemakers be used temporarily after cardiac surgery?
To stabilize heart rhythm until a permanent internal pacemaker is placed.
What is the difference between oral/nasal tracheal tubes and tracheostomy tubes?
Oral/nasal tubes enter through the mouth or nose; tracheostomy tubes enter directly into the trachea via a surgical opening.
When imaging an intubated patient on a ventilator, why is timing important?
To minimize respiratory motion and obtain a clear image.
What causes the need for a tracheostomy instead of oral/nasal intubation?
Long-term airway management, upper airway obstruction, or injury to the mouth/throat.