1-8 Circulatory System
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
Cardiovascular System. General Microscopic, Ultramicroscopic and Functional Characteristics of its Organs
The cardiovascular system is responsible for transporting blood, oxygen, nutrients, hormones, and waste products throughout the body. It maintains homeostasis by regulating body temperature, and fluid balance, and delivering immune responses
Microscopic Characteristics:
Heart: Composed of cardiac muscle tissue (striated, branched, with central nuclei and intercalated discs).
Arteries: Thick tunica media (smooth muscle and elastic fibers); smaller lumen.
Veins: Thinner walls, larger lumen, often with valves.
Capillaries: Single layer of endothelial cells resting on a basement membrane.
Ultramicroscopic Characteristics:
Cardiomyocytes: Contain numerous mitochondria, T-tubules, sarcoplasmic reticulum; intercalated discs have desmosomes and gap junctions for synchronized contraction.
Endothelial cells: Have pinocytotic vesicles and tight junctions; involved in transport and barrier functions.
Basement membrane: Supports endothelium; selectively permeable.
Functional Characteristics:
Heart: Pumps blood via rhythmic contractions; generates pressure to drive circulation.
Arteries/Arterioles: Transport blood under high pressure; regulate blood flow and pressure.
Capillaries: Site of gas, nutrient, and waste exchange.
Veins/Venules: Return blood to the heart; act as blood reservoirs.
Major (Systemic) Circulation and Lesser (Pulmonary) Circulation
Major (Systemic) Circulation
This refers to the part of the circulatory system that carries oxygenated blood from the heart’s left ventricle through the arteries to the body and returns deoxygenated blood to the heart’s right atrium via the veins.
It provides tissues with nutrients and oxygen while removing waste.
Lesser (Pulmonary) Circulation
Pulmonary circulation is the loop through the lungs where blood is oxygenated.
Deoxygenated blood is pumped from the right ventricle to the lungs via the pulmonary arteries and returns to the left atrium oxygenated through the pulmonary veins.
Embryonic Development of Major Blood Vessels
Embryonic Development of Major Blood Vessels:
Blood vessels begin forming in the 3rd week of embryogenesis via vasculogenesis (formation from mesodermal blood islands).
Angiogenesis follows: new vessels sprout from existing ones.
Aortic Arches (Pharyngeal Arch Arteries):
Derived from the aortic sac and form six paired arches (not all persist).
Contribute to major arteries:
3rd arch → Common carotid arteries and proximal internal carotids
4th arch:
Left → Aortic arch
Right → Right subclavian artery
6th arch → Pulmonary arteries and ductus arteriosus (left side)
Dorsal Aortae:
Paired initially; fuse to form descending thoracic and abdominal aorta.
Vitelline Arteries:
Supply the yolk sac; contribute to celiac, superior, and inferior mesenteric arteries
Umbilical Arteries:
Carry deoxygenated blood from fetus to placenta.
After birth, become medial umbilical ligaments
Cardinal Veins:
Main venous system; gives rise to:
Superior and inferior vena cava
Brachiocephalic veins
Renal and iliac veins
Fetal Circulation
Fetal circulation refers to the circulatory system of a fetus, which differs from postnatal circulation
Since the fetus's lungs are not yet functional, oxygen and nutrients are supplied through the placenta
Blood bypasses the lungs via structures like the foramen ovale and ductus arteriosus, which close after birth, transitioning the newborn to regular pulmonary and systemic circulation
Foramen Ovale: Allows blood to flow directly from the right atrium to the left atrium
Ductus Arteriosus: Connects the pulmonary artery to the aorta, bypassing the lungs
Ductus Venosus: Allows oxygenated blood from the umbilical vein to bypass the liver and enter the inferior vena cava
Heart. Embryonic development.
Begins in week 3 from splanchnic mesoderm.
Starts as a paired endothelial heart tube, which fuses into a single tube.
Undergoes looping (day 23–28) → establishes left-right asymmetry.
Differentiates into five regions (from inflow to outflow): Sinus venosus → Atrium → Ventricle → Bulbus cordis → Truncus arteriosus.
Septation forms:
Atria and ventricles (interatrial and interventricular septa)
Outflow tracts (aorticopulmonary septum → separates aorta and pulmonary trunk)
Fully partitioned heart by end of week 8.
Heart. Macroscopic characteristics.
Hollow muscular organ, located in the mediastinum.
Surrounded by pericardium (fibrous and serous layers).
Has four chambers: Two atria (receive blood), two ventricles (pump blood).
Valves: Atrioventricular (tricuspid, mitral) and semilunar (aortic, pulmonary) ensure unidirectional blood flow.
Wall layers: Endocardium (inner), myocardium (middle muscle), epicardium (outer).
Supplied by coronary arteries; drained by cardiac veins.
Heart. Atria and Ventricles
Right Atrium
Receives deoxygenated blood from the superior vena cava, inferior vena cava, and coronary sinus.
Contains the fossa ovalis, a remnant of the fetal foramen ovale.
The right auricle is a muscular pouch on the RA.
Pectinate muscles: Ridged muscles in the atrial walls.
Right Ventricle
Pumps deoxygenated blood into the pulmonary trunk via the pulmonary valve.
Trabeculae carneae: Irregular ridges of muscle on the inner walls.
Papillary muscles: Anchor the chordae tendineae, which are attached to the tricuspid valve.
The moderator band helps conduct electrical signals within the ventricle.
Left Atrium
Receives oxygenated blood from the pulmonary veins.
Has a smooth inner wall, except for the left auricle, which contains pectinate muscles.
Thinner wall than the ventricles due to lower pressure requirements.
Left Ventricle
Pumps oxygenated blood into the aorta via the aortic valve.
The strongest and thickest-walled chamber due to the high pressure needed to pump blood through the systemic circulation.
Contains trabeculae carneae and papillary muscles like the RV (right ventricle), but they are more pronounced.
Heart. Valves of the Heart.
Heart valves ensure one-way blood flow through the heart, preventing backflow.
Atrioventricular Valves
Tricuspid Valve: Between the right atrium and right ventricle. It has three cusps (flaps).
Mitral (Bicuspid) Valve: Between the left atrium and left ventricle. It has two cusps.
Both AV valves are supported by chordae tendineae, which prevent them from inverting when the ventricles contract.
Semilunar Valves
Pulmonary Valve: Located between the right ventricle and pulmonary trunk. It has three crescent-shaped cusps.
Aortic Valve: Located between the left ventricle and aorta, also with three cusps.
These valves open when the ventricles contract, allowing blood to flow into the pulmonary and systemic circuits, and close when the ventricles relax to prevent backflow.
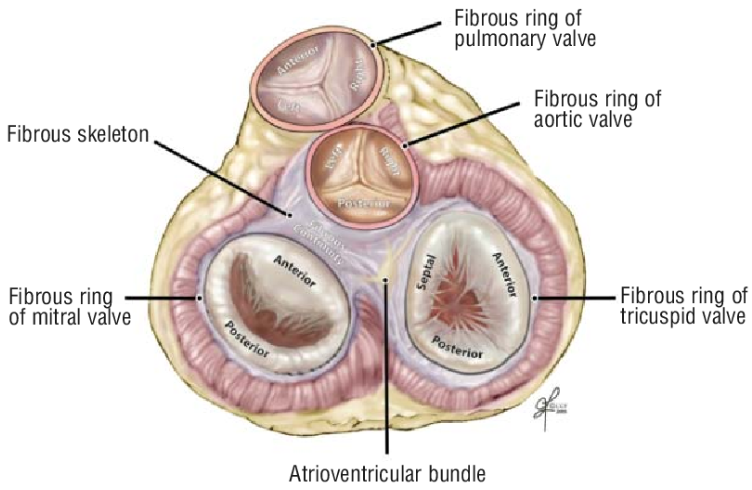
Fibrous Skeleton of the Heart
Dense connective tissue framework within the heart.
Located mainly at the level of the atrioventricular (AV) junction.
Consists of:
Four fibrous rings (annuli fibrosi) around the heart valves.
Right and left fibrous trigones (connect rings).
Membranous part of the interventricular septum.
Functions:
Anchors heart valves and maintains their shape.
Provides electrical insulation between atria and ventricles (ensures orderly contraction).
Serves as an attachment point for myocardium.
Conducting System of the Heart
Specialized cardiac muscle cells that generate and conduct impulses.
Coordinates rhythmic contraction of atria and ventricles.
Sinoatrial (SA) Node:
Located in right atrium near the superior vena cava.
Natural pacemaker; initiates heartbeat (~60–100 bpm).
Atrioventricular (AV) Node:
Located in interatrial septum near coronary sinus opening.
Delays impulse to allow atrial contraction before ventricular contraction.
AV Bundle (Bundle of His):
Passes through fibrous skeleton into interventricular septum.
Only electrical connection between atria and ventricles.
Right and Left Bundle Branches:
Run down either side of the septum toward the apex.
Purkinje Fibers:
Spread through ventricular myocardium.
Ensure rapid, coordinated ventricular contraction.
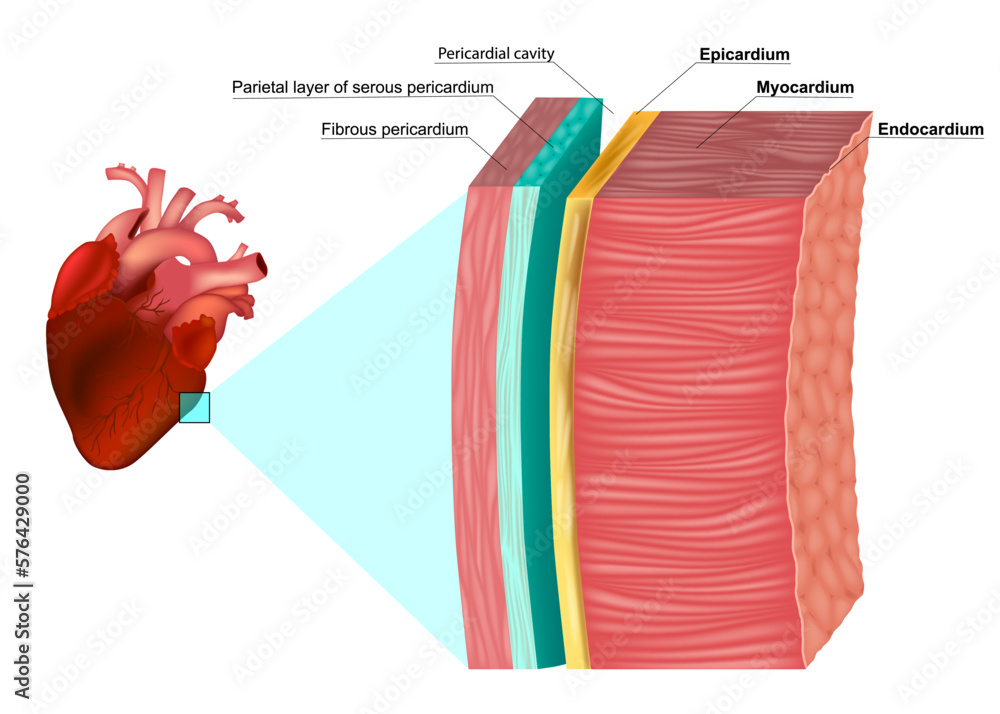
Heart – Microscopic, Ultramicroscopic and Functional Characteristics of the Heart Wall.
Microscopic Characteristics of the Heart Wall - Three layers:
Endocardium: simple squamous epithelium + connective tissue.
Myocardium: cardiac muscle cells with intercalated discs; thickest layer.
Epicardium: mesothelium + connective tissue with fat, vessels, nerves.
Ultramicroscopic Characteristics:
Cardiomyocytes:
Striated, branched, single central nucleus.
Contain T-tubules, sarcoplasmic reticulum, and many mitochondria.
Intercalated discs:
Contain desmosomes (mechanical link) and gap junctions (electrical link).
Endothelium of endocardium:
Has tight junctions, pinocytotic vesicles; regulates exchange and prevents clotting.
Functional Characteristics of the Heart Wall:
Endocardium: Smooth inner lining to reduce friction and prevent clotting.
Myocardium: Main contractile layer; responsible for pumping blood.
Epicardium: Protective outer layer; contains coronary vessels and fat.
Heart. Nerve and Blood Supply
Cardiac Plexus
Sympathetic fibers (from T1–T5):
Increase heart rate and contractility.
Parasympathetic fibers (via vagus nerve):
Decrease heart rate.
Sensory (afferent) fibers:
Relay information like pain (e.g. in angina) to CNS.
Blood Supply:
Arterial supply:
Right and left coronary arteries (from ascending aorta).
Supply different regions of the heart (e.g. LAD artery = anterior wall).
Venous drainage:
Mainly via the coronary sinus → into right atrium.
Also includes anterior cardiac veins and Thebesian veins (small direct drains into chambers).
Arteries. Microscopic, Ultramicroscopic, and Functional Characteristics of the Arterial Wall.
Microscopic Characteristics of the Arterial Wall:
Tunica intima: Inner layer with endothelium, subendothelial connective tissue, and internal elastic lamina (in larger arteries).
Tunica media: Thickest layer in arteries: smooth muscle cells, elastic fibers, collagen, and external elastic lamina (in large arteries).
Tunica adventitia (externa): Outer connective tissue layer with collagen and elastic fibers, vasa vasorum (in large arteries), and nerves.
Ultramicroscopic Characteristics:
Endothelial cells: Simple squamous, connected by tight junctions; contain pinocytotic vesicles and basal lamina.
Smooth muscle cells (in tunica media):
Spindle-shaped, with gap junctions for coordination.
Capable of vasoconstriction and vasodilation.
Elastic laminae: Rich in elastin; allow stretch and recoil during the cardiac cycle.
Functional Characteristics of Arterial Wall:
Tunica intima: Provides a non-thrombogenic surface; regulates permeability and vascular tone.
Tunica media: Controls vessel diameter and blood pressure; more developed in arteries than in veins.
Tunica adventitia: Provides structural support, elasticity, and houses vessels and nerves for the artery wall.
Arteries. Classification.
1. Elastic Arteries (Conducting Arteries):
Large arteries (e.g. aorta, pulmonary trunk).
Thick tunica media with many elastic fibers.
Function: Dampen pulsatile pressure and maintain continuous blood flow.
2. Muscular Arteries (Distributing Arteries):
Medium-sized (e.g. radial, femoral arteries).
Tunica media rich in smooth muscle, less elastic tissue.
Function: Distribute blood to organs; control blood flow and pressure via vasoconstriction/dilation.
3. Arterioles (Resistance Vessels):
Smallest arteries; 1–2 layers of smooth muscle.
Major regulators of systemic vascular resistance and blood pressure.
Lead directly into capillary beds.
Aorta. Microscopic, Ultramicroscopic and Functional Characteristics of its Wall.
Microscopic Characteristics of the Aortic Wall:
Classified as an elastic artery.
Wall has three tunics (layers):
1. Tunica intima:
Endothelium (simple squamous epithelium) on a basement membrane.
Subendothelial connective tissue with occasional smooth muscle cells.
Prominent internal elastic lamina (though less distinct due to surrounding elastic layers).
2. Tunica media:
Thickest layer.
Contains 40–70 concentric elastic lamellae.
Smooth muscle cells interspersed between elastic layers.
Also contains collagen fibers for structural support.
3. Tunica adventitia:
Composed of collagen and elastic fibers.
Contains vasa vasorum (small vessels supplying the outer wall).
Also has autonomic nerves and connective tissue cells.
Ultramicroscopic Characteristics:
Endothelial cells (tunica intima): Joined by tight junctions; contain pinocytotic vesicles for transport.
Smooth muscle cells (tunica media):
Synthesize elastin, collagen, and ground substance.
Connected by gap junctions for functional coordination.
Elastic lamellae: Composed of elastin, allow the wall to stretch and recoil.
Vasa vasorum: Provide nutrient exchange to outer layers (media and adventitia).
Functional Characteristics of the Aortic Wall:
Acts as a pressure reservoir:
During systole: stretches to accommodate blood volume.
During diastole: recoils to maintain continuous blood flow.
Tunica media’s elasticity: Buffers blood pressure fluctuations from the heartbeat.
Tunica intima: Maintains smooth, non-thrombogenic surface for blood flow.
Tunica adventitia: Provides tensile strength and protects against overdistension.
Veins. Microscopic, Ultramicroscopic and Functional Characteristics of the Venous Wall.
Microscopic Characteristics of the Venous Wall:
Veins have three layers like arteries, but thinner walls and larger lumens.
Less smooth muscle and elastic tissue compared to arteries.
1. Tunica intima:
Endothelium (simple squamous epithelium) with thin subendothelial connective tissue.
May have valves (folds of intima) in medium and large veins, especially in limbs.
2. Tunica media:
Thin layer with few smooth muscle cells and scattered elastic fibers.
Much less prominent than in arteries.
3. Tunica adventitia:
Thickest layer in veins.
Made of collagen, elastic fibers, and vasa vasorum in large veins.
Contains autonomic nerves and connective tissue cells.
Ultramicroscopic Characteristics:
Endothelial cells:
Have tight junctions and pinocytotic vesicles.
Sit on a basement membrane; regulate permeability.
Valves:
Composed of folds of tunica intima with a connective tissue core.
Prevent backflow of blood, especially in limbs.
Smooth muscle cells (in media):
Fewer in number; loosely arranged with collagen.
Adventitia may have nerve endings and vasa vasorum for nourishment.
Functional Characteristics of the Venous Wall:
Low-pressure system: walls are thin and compliant.
Large lumen: holds most of the body’s blood (veins act as capacitance vessels).
Valves:
Ensure unidirectional flow toward the heart.
Assist venous return with the help of skeletal muscle contraction.
Adventitia provides mechanical support and protects the vein.
Veins. Classification.
1. Large veins:
Examples: Superior and inferior vena cava.
Thin media, well-developed adventitia with vasa vasorum.
2. Medium-sized veins:
Examples: Radial, tibial, femoral veins.
May contain valves.
Most common type in limbs.
3. Venules:
Smallest veins; drain blood from capillaries.
Postcapillary venules: endothelium with pericytes; site of inflammation and exchange.
Muscular venules: have a thin media of smooth muscle.
Microcirculatory blood system. Arterioles. Classification. Microscopic, Ultramicroscopic and Functional Characteristics.
Classification:
Terminal branches of arteries; lead into capillary beds.
Precapillary arterioles control flow into individual capillaries.
Microscopic Characteristics:
Tunica intima: Endothelium with a thin subendothelial layer.
Tunica media: 1–2 layers of smooth muscle cells.
No distinct internal or external elastic lamina.
Ultramicroscopic Features:
Endothelial cells with tight junctions and pinocytotic vesicles.
Smooth muscle cells linked via gap junctions.
Functional Role:
Major resistance vessels; regulate blood pressure and flow.
Vasoconstriction/vasodilation adjusts perfusion of capillary beds.
Microcirculatory blood system. Venules. Classification. Microscopic, Ultramicroscopic and Functional Characteristics.
Classification:
Postcapillary venules: directly after capillaries; major site of leukocyte migration.
Muscular venules: have a few layers of smooth muscle.
Microscopic Characteristics:
Postcapillary venules: endothelium + basal lamina.
Muscular venules: add 1–2 layers of smooth muscle.
Ultramicroscopic Features:
Endothelial cells may express adhesion molecules during inflammation.
May have pericytes and gaps facilitating immune cell movement.
Functional Role:
Collect blood from capillaries.
Involved in inflammation and immune cell transport.
Microcirculatory blood system. Capillaries. Classification. Microscopic, Ultramicroscopic and Functional Characteristics.
Classification:
Continuous capillaries (most common; muscle, brain, lungs).
Fenestrated capillaries (endocrine glands, kidneys, intestines).
Sinusoidal capillaries (liver, spleen, bone marrow).
Microscopic Characteristics:
Composed of:
Endothelium (single cell layer).
Basement membrane.
Occasional pericytes on outer surface.
Ultramicroscopic Features:
Endothelial cells with tight junctions, pinocytotic vesicles, and fenestrations (in fenestrated types).
Pericytes regulate capillary stability and permeability.
Functional Role:
Main site of exchange of O₂, CO₂, nutrients, and waste.
Thin walls ensure efficient diffusion.
Microcirculatory blood system. Arteriovenous anastomoses.
Definition: Direct connections between arterioles and venules, bypassing capillaries.
Location: Found in skin, fingertips, ears, nose, lips (areas needing temperature regulation).
Structure: Lined by endothelium; surrounded by smooth muscle to regulate opening/closing.
Function:
Thermoregulation: shunt blood away from capillaries to conserve heat.
Regulate blood flow based on tissue demand.