1.2 Wound repair
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
the three parts of tissue repair:
cell and tissue regen
scar formation
factors influencing repair
restoration of tissue architecture and function after injury
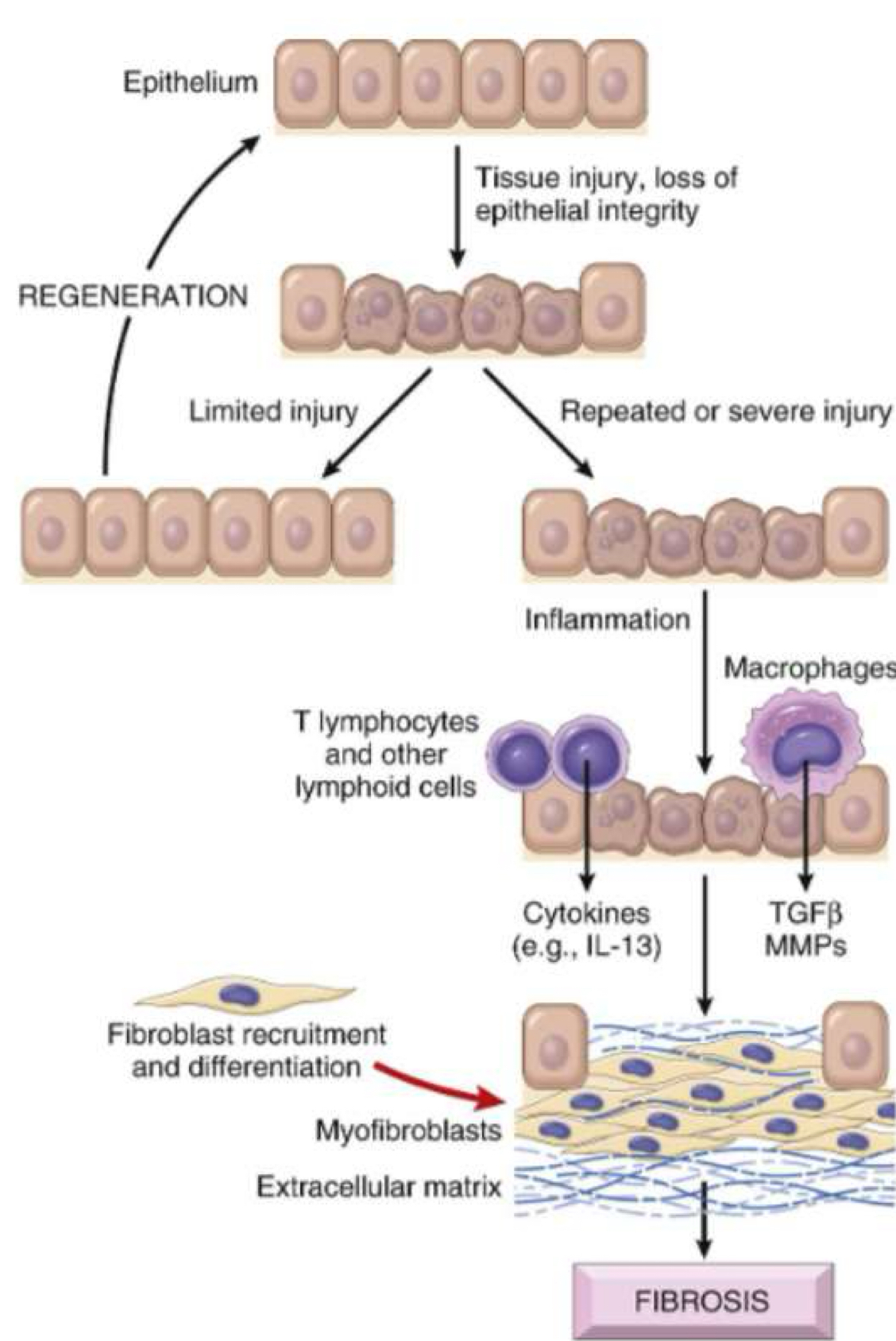
occurs by regen (midl or superficial injury) or scar formation (severe injury)
what is tissue repair?
proliferation of residual cells that retain capacity to divide and by replacement from stem cells
typical response in organs w rapidly dividing cells i.e skin, mucosa, liver
what is regeneration?
repair occurs by laying down CT
fibrous tissue cannot perform function of previous tissue but provides stability
fibrosis= deposition of collagen in organs after chronic inflam (excess)
infection or injury leads to injury site the inflammation and then formation of granulation tissue then scar
what is scarring?
tissue that is replaced by scar tissue
granulation tissue
what does granulation tissue replace?
inflammation cells
what does regenerative capacity depend on?
ability of tissue to regenerate
what was the significance of varicose veins?
vein that has lost elasticity so it is expanded
re-canalization: reopen
three types of proliferative tissues?
labile tissue: continuous division
stable tissue: quiescent cells w minimal replicative activity
permanent tissue: terminally differentiated
high turnover rate
high regenerative capacity
ex: squamous, glandular, and GI epithelium; bone marrow
skin, oral mucosa, genitals
labile cells
low turnover rate
can proliferate rapidly when called upon
ex: fibroblasts, osteoblasts, liver, kidney, endothelial cells
“solid organs”
stable cells
cannot divide
cannot regen
heal with scar tissue
ex: neurons and cardiac cells; tooth enamel
why damage to these can be so detrimental; necrosis here is final
permanent cells
best but uncommon possible outcome of acute inflam
regeneration: acute inflam resolves and damaged epithelial cells regen
five factors that favor regen:
tissue w regen capacity
minimal cell death fast elimination of agent
fast removal of debris
adequate drainage
T or F: regen restores normal structure and function without scarring (regen)
T
T or F: acute inflam exudate is removed by liquefaction and phagocytosis (regen)
T
T or F: support stroma does not have to be in tact for regen
F: stroma must be in tact
T or F: damaged cells must be able to regen for regen to happen
T (duh)
how does repair by CT deposition occur?
angiogenesis
granulation tissue development: pink granular appearance
remodel of CT
granulation tissue
proliferation of capillaries, endothelial cels, inflammatory cells, fibroblasts, CT
granulomas
epithelioid histiocytes
multi-nucleated giant cells and lymphocytes
chronic inflammation
what conditions have granuloma in their name but are not granulomas? they have granular tissue?
growth/swelling = granuloma but granulation tissue
periapical granuloma
pyogenic granuloma
peripheral giant cell granuloma
central giant cell granuloma
traumatic ulcerative granuloma
what helps with blood vessel formation and lines walls?
pericyte
mechanism of repair by CT deposition
deposition of CT
fibroblast migrate, proliferate, and deposit ECM: TGF beta (cytokine for Ct synthesis and deposition of CT proteins)
remodel CT: depends on synthesis and degradation of proteins
infection
diabetes: abnormal wound healing (abs can help)
nutrition: vit C deficiency
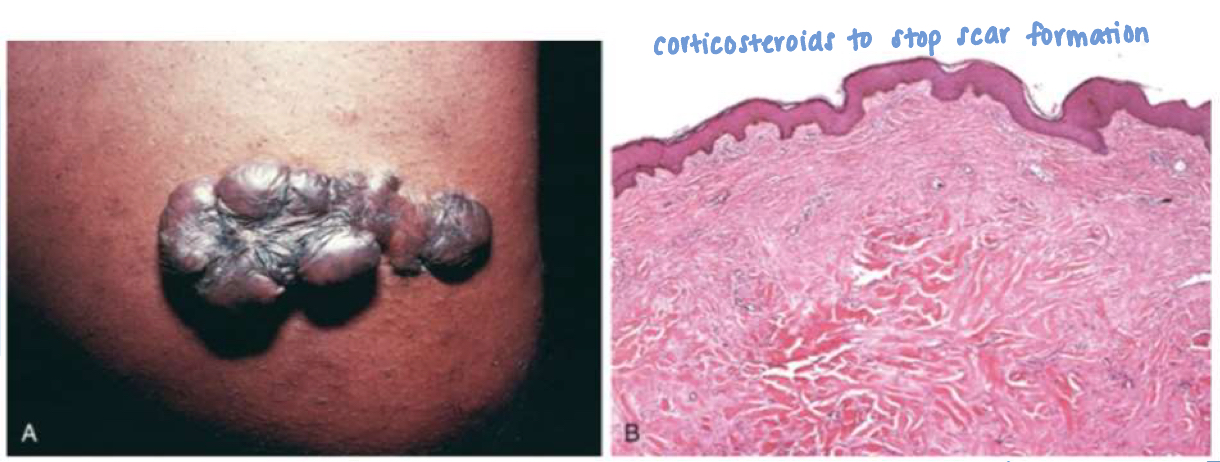
glucocorticoids: steroids weaken scar formation by inhibiting TGFβ (use for keloids)
mechanical variables: no undo strain or stress
place suture along normal lines of tension, medial to lateral rather than anterior to posterior
poor perfusion: poor vascular flow i.e arterial sclerosis
foreign bodies: suture can cause foreign body rnx
type and extent of injury
location of injury
factors that influence repair
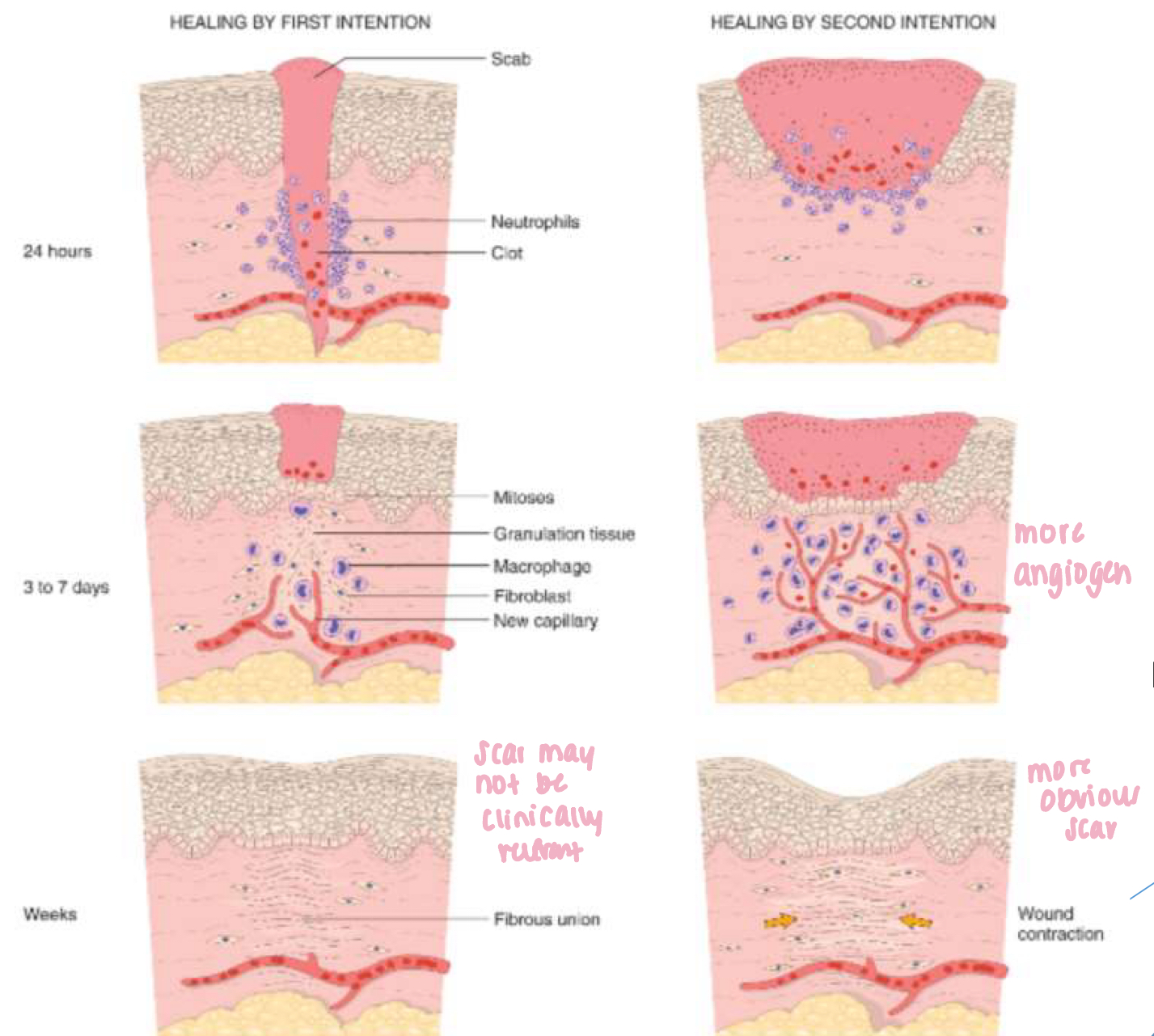
primary vs secondary healing
Primary healing occurs when a wound heals without infection and the edges are close together (suture)
Secondary healing occurs when a wound is left open to heal naturally
primary intention is
healing of closely opposed surfaces
epithelial regen is principal mechanism of repair
small scar with minimal wound contraction
days of healing by primary intention
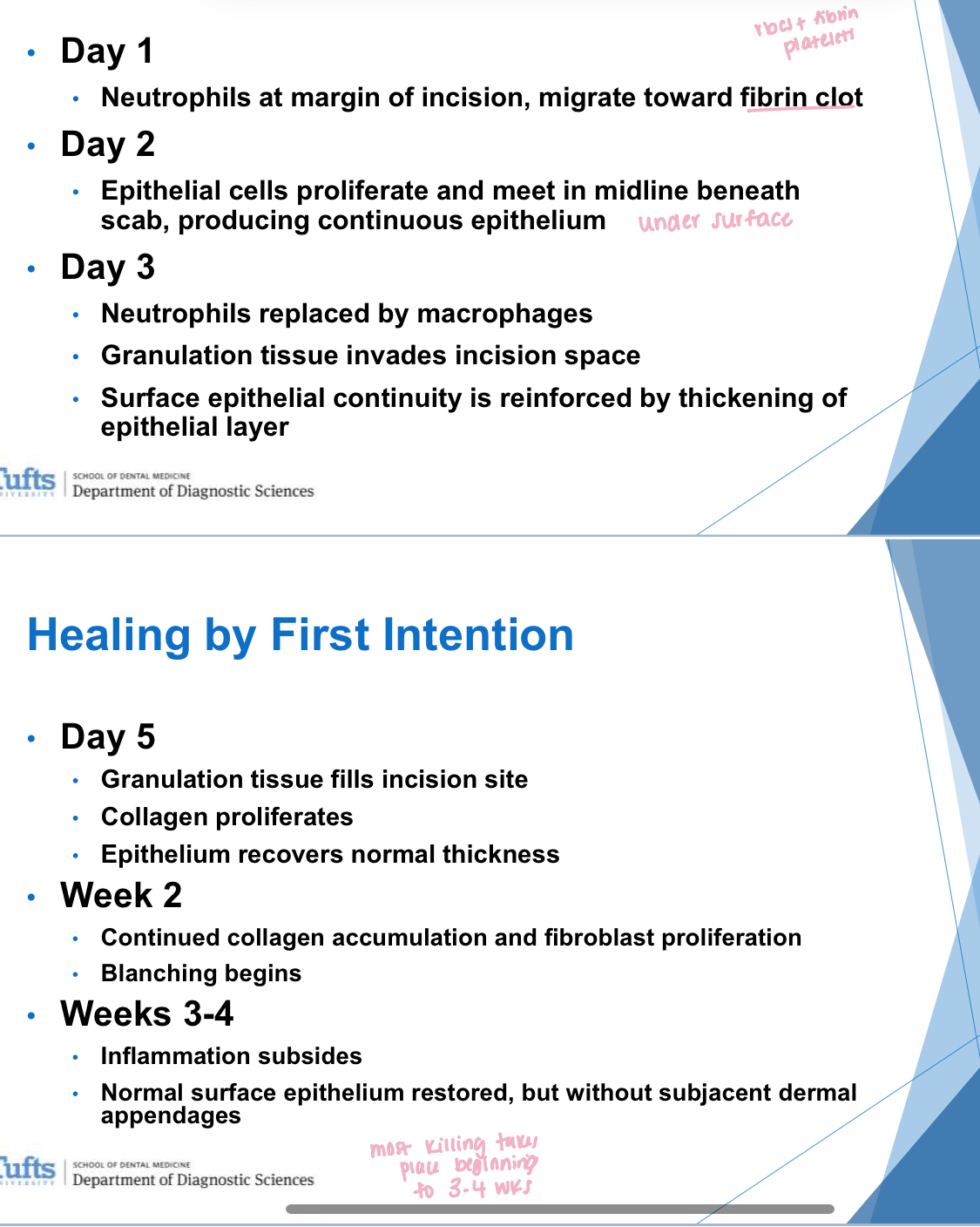
differences in healing from second intention compared to first
larger clot
more intense inflam
more granulation tissue
wound contraction: w/in 6 weeks large wounds reduced 5-10% their original size
do sutured wounds regain strength of normal skin?
NO
regain 10% when suture removed at 1 week
reach max of 70-80% in 3 months
parenchymal organs:
liver, lungs, kidney, spleen, adrenal glands
tissue repair for parenchymal organs:
collagen deposition normal in wound healing
excessive deposition of collagen or ECM = fibrosis
amalgam tattoo
benign, flat, discolored area in the mouth caused by amalgam particles from a dental filling
during procedure or removal
gingiva, bucal mucosa, tongue
tissue repair for brain damage
repaired through proliferation of astrocytes (brain support cells) not fibroblasts
necrotic tissue replaced by fluid
glial scar/astrocyte gliosis: cystic lesion surrounded by compacted glial fibers produced by astrocytes
tissue repair for bone damage
collagenous scarring insufficient to repair bone
fractures repair through organization, granulation tissue formation, and fibroblasts in-growth with osteoblast proliferation
define callus
mixture of fibrous granulation tissue and developing new bone
what is wound dehiscence?
surgical complication that occurs when a surgical incision opens or separates; often after abdominal surgery due to increased pressure
wound abnormality
what are hypertrophic scars and keloids?
prominent raised scars resulting from excess production of ECM
steps to fibrosis