The kidneys - chapter 19
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
122 Terms
What is the most important function of the kidney?
the homeostatic regulation of water and ion content of the blood
How do the kidneys maintain normal blood concentration of ions and water?
By balancing intake of water and ions with their excretion in the urine.
they obey the principle of mass balance
In which 6 function can the kidneys be subdivided?
redulation of the extracellular fluid volume and blood pressure. — When extracellular volume decreases, blood pressure also decreases
regulation of osmolarity — the body integrates kidney function with behavioral drives to maintain blood osmolarity
maintainance of ion balance — the kidneys keep concentrations of key ions within a normal range, by balancing dietary intake with urinary loss
homeostatic regulation of pH — the pH of plasma is kept within a narrow range. If extracellular fluid becomes too acidic, the kidneys remove H+ and conserve bicarbonate ions (HCO3 -) which act as a buffer.
excretion of wastes — the kidneys remove metabolic waste products and xenobiotics, or foreign substances
production of hormones
Whcih hormones do the kineys produce?
the kidney cells synthesize erythropoietin(epo) — regulates red blood cell synthesis
they release renin — an enzyme that regulates the production of hormones involved in Na+ balance and blood pressure homeostasis
renal enzymes — help convert vitamin D3 into a hormone that regulates Ca2+ balance
What happens during micturition/ urinination?
the bladder contracts and expels urine through the urethra
Which structures does water and solute go through during urine production?
Urine production begins when;
water and solute move from plasma into the hollow tubes that make up the bulk of the kidneys.
The tubules modify the composition of the fluid as it passes into a smooth muscular tube – ureter.
There are 2 ureters leading from each kidney to the urinary bladder.
What does it mean when the kidneys are described as "retroperitoneal"?
It means the kidneys are located behind the peritoneal cavity.
What structures emerge from the concave surface of the kidney?
blood vessles
nerves
lymphatics
ureters
Which arteries supply blood to the kidneys, and where do they originate?
The renal arteries supply blood to the kidneys, and they branch off the abdominal aorta.
Where do the renal veins carry blood from the kidneys?
The renal veins carry blood from the kidneys to the inferior cava.
What are the 2 layers the interior of the kidneys are arranged in? and how are these 2 layers formed?
the outer cortex
the inner medulla
the layers are formed by the organized arrangement of the nephrons
How does blood flow in the renal portal system?
blood flows:
from renal arteries into an afferent arteriole
from the afferent arteriole it goes into the glomerulus(1st capillary bed).
blood leaving the glomerulus flows into an efferent arteriole.
then into the peritubular capillaries(2nd capillary bed) that surrounds the tubule.
peritubular capillaries converge to form venules and small veins, sending blood out of the kidney through the renal vein.
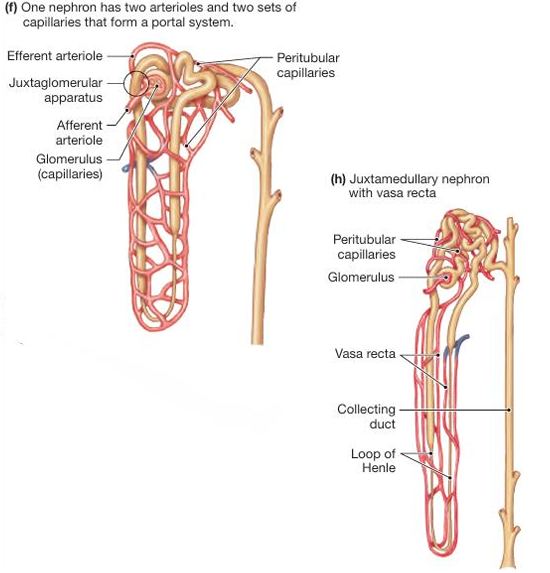
What is the vasa recta?
specialized, hairpin-shaped blood vessels in the kidney that run parallel to the loops of Henle.
in juxtamedullary nephrons, the long peritubular capillaries that dip into the medulla.
What is the function of the renal portal system?
the function of the renal portal system is to filter fluid out of the blood and into the lumen of the nephron at the glomular capillaries, then to reabsorb fluid from the tubulu lumen back into the blood at the peritubular capillaries
What type of cells make up the kidney tubule?
A single layer of epithelial cells connected near their apical surface.
What can be found on the apical and basal side of the epithelium?
The apical surfaces are folded into microvilli, and the basal side of the polarized epithelium rests on a basement membrane. The cell-cell junctions are mostly tight but some have selective permeability for ions.
What is the name of the structure at the beginning the nephron?
the Bowman’s capsule
What does Bowman’s capsule surround?
the glomerulus
How is fluid filtered from the blood into the nephron?
The endothelium of the glomerulus is fused with the epithelium of Bowman’s capsule, allowing fluid to pass directly into the lumen of the proximal tube.
What is a renal corpsule?
the combination of the glomerulus and the Bowman’s capsule
What is the loop of Henle?
a hairpin-shaped segment that dips down toward the medulla and then back up.
What are the 2 limbs of the loop of Henle?
A thin descending limb
an ascending limb with thin and thick segments
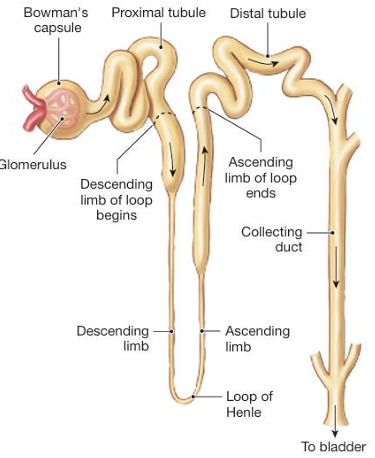
What is the route fluid takes in the kidneys
Glomerulus
– Blood is filtered here.
Bowman’s Capsule
– Surrounds the glomerulus and collects the filtrate.Proximal Tubule
– First segment of the tubule where reabsorption begins.Loop of Henle
Thin descending limb
Thin ascending limb
Thick ascending limb
– Regulates concentration of urine via water and salt movement.
Distal Tubule
– Performs further ion exchange and pH balance.Collecting Duct
– Collects fluid from multiple nephrons; further concentrates urine.Renal Pelvis
– Collects fluid from collecting ducts.Ureter
– Transports urine from the kidney to the bladder for excretion.
Which region is known as the juxtaglomerular apparatus?
the nephron twists and folds back on itself so that the final art of the ascending limb of the loop of Henle passes between the afferent and the efferent arterioles
What does the proximity of the acending limb and the arterioles allow?
paracrine communication between the 2 structures
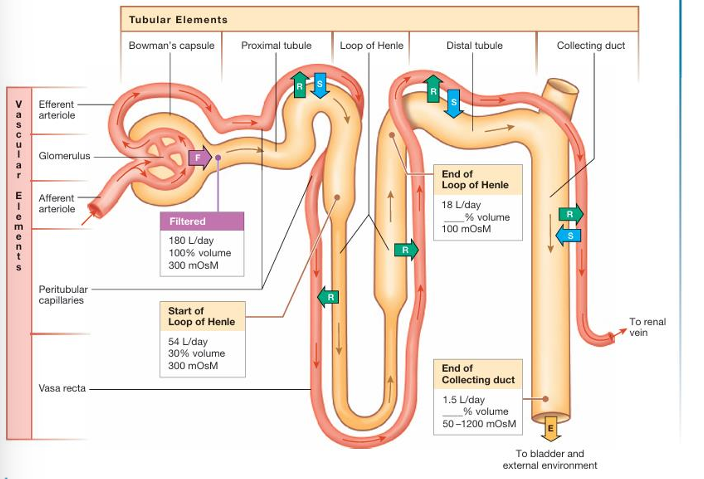
Which are the 3 basic processes that take place in the nerphron?
filtration
reabsorption
secretion
What is filtration?
the movement of fluid from blood into the lumen of the nephron.
Once the filtrate passes into the lumen of the nephron, it becomes part of the external environment. For this reason, anything that filters into the nephron is destined for excretion.
What is reabsorption?
the process of moving substances in the filtrate from the lumen of the tubule back into the blood flowing through the peritubular capillaries
What is secretion?
selectively remoes molecules from the blood and adds them to the filtrate in the lumen.
When does reabsorption occur?
it occurs when the proximal tubule transports solutes out of the lumen, and water flows by osmosis.
The filtrate leaving the proximal tube has. … osmolarity as filtrate that entered.
The filtrate leaving the proximal tube has the same osmolarity as filtrate that entered.
What is the primary function of the proximal tube?
the isosmotic reabsorption of the solutes and water
What is the primary site for creating dilute urine? and what happens at this site?
the loop of Henle
here more solute is reabsorbed than water, and the filtrate becomes hypoosmotic relative to the plasma.
What takes place at the distal tubule and the collecting duct?
the fine redulation of salt and water balance under the control of hormones
What determines the final composition of the filtrate?
reabsorption
secretion
On what does the final volume and osmolarity of the urine depend?
on the body’s needto conserve or excrete water and solute
What is the composition of the filtrate?
plasma minus most of the plasma proteins.
Under normal conditions, blood cells remain in the capillary, so that the f iltrate is composed of water and dissolved solutes.
What is filtration fraction?
the percentage of renal plasma flow that filteres into the tubule.
Only 1/5 of the plasma that flows through the kidneys filters into the nephrons.
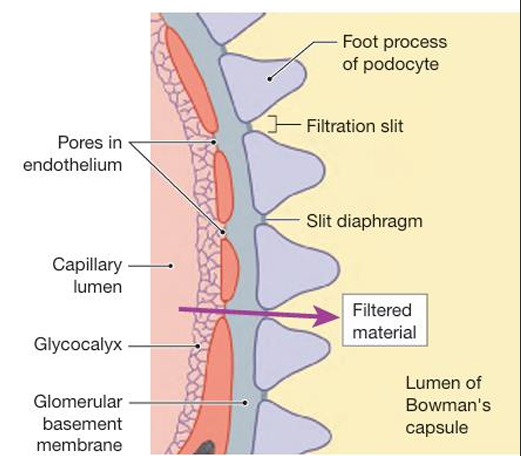
Through which 3 filtration barriers must plasma pass before entering the lumen?
the glomular capillary epithelium
are fenestrated — allow most of the components of the plasma to filter through
The luminal surface of the capillary and the pores are lined with a layer of glycoproteins with a negative charge — repel the negatively charged plasma proteins
a basement membrane
extracellular matrix that seperates the capillary endothelium from the epithelium of the Bowmans capsule.
this membrane consists of negatively charged glycoproteins, collagen and other proteins
it excludes most plasma proteins from the fluid that filters through it
the epithelium of the Bowman’s capsule
consists of podocytes — which have long cytoplasmic extensions.
foot processes wrap around the glomerular capillaries and interlace with one another, leaving narrow filtration slits closed by a slit diaphram.
What is the function of glomerular mesanglial cells?
Glomerular mesangial cells lie between and around the glomerular capillaries, creating a support structure for the tuft of capillaries.
mesanglial cells influence filtration by altering the surface area of the filtration slits.
mesanglial cells secrete cytokines associated with immune and inflammatory processes
Which 3 pressures influence the glomerular filtration rate?
capillary blood pressure
capillary collod osmotic pressure
capsule fluid pressure
What is capillary blood pressure?
The hydrostatic pressure of blood flowing through the glomerular capillaries forces fluid through the leaky endothelium.
Capillary blood pressure favors filtration into Bowman’s capsule. Although pressure decreases as blood moves through the capillaries, it remains higher than the opposing pressures. So, filtration takes place along nearly the entire length of the glomerular capillaries.
What is capillary calloid osmotic pressure?
the pressure gradient due to the presence of proteins in the plasma
The colloid osmotic pressure inside glomerular capillaries is higher than that of the fluid in Bowman’s capsule. so the pressure gradient favors fluid movement back into the capillaries
What is capsule fluid pressure?
the presence of fluid in the capsule creates a hydrostatic fluid pressure that opposes fluid movement into the capsule.
Fluid filtering out of the capillaries must displace the fluid already in the capsule lumen.
What is the driving net force of filtration?
The net driving force is 10 mm Hg in the direction favoring filtration.
When combined with the very leaky nature of the fenestrated glomerular capillaries, it results in rapid fluid filtration into the tubules.
What is the glomular filtration rate(GFR)?
the volume of fluid that filters into Bowman’s capsule per unit time
What is the average GFR per minute? and per day?
The average GFR is 125 mL/min, or 180 L/day.
By which 2 factors is the GFR influenced?
the net filtration pressure
the filtration coefficient
What primarily determines the filtration pressure>
renal blood flow
blood pressure
What are the 2 components of the filtration coefficient?
the surface area of the glomerular capillaries available for filtration
the permeability of the filtration slits
Blood pressure provides the … that drives glomerular filtration.
Blood pressure provides the hydrostatic pressure that drives glomerular filtration.
By what is the GFR primarily controlled?
by the regulation of blood flow through the renal arteries
If the overall resistance of the renal arterioles increases, renal blood flow decreases, and blood is diverted to other organs.
When doe the GFR decrease?
If the resistance increases in the afferent arteriole, hydrostatic pressure decreases on the glomerular side of the constriction.
When does the GFR increase?
If the increases in efferent arterioles, blood “damps up” in front of the constriction and hydrostatic pressure in the glomerular capillaries increases
What is the function of autoregulation of the GFR?
It protects the filtration barrier from high blood pressures that might damage them.
Autoregulation of glomerular filtration rate is a local control process in which the kidneys maintains a relatively constant GFR in the face of normal fluctuations in blood pressure.
Which mechanisms are at work during autoregulation of GFR?
myogenic response
tubuloglomerular feedback
What is the myogenic response?
the intrinsic ability of the vascular smooth muscle to respond to pressure changes
How does the myogenic response, react to increased blood pressure?
increased blood pressure, stretches the smooth muscle in the arteriole wall
stretch sensitive ion channels open, and the muscle cells depolarize
depolarization opens voltage-gated Ca2+ channels
the vascular smooth muscle contracts
vasoconstriction increases the resistance to flow
blood flow in the arteriole diminishes
blood pressure decreases
Why is vasodialation, at decreased blood pressures not as effective?
because normally the afferent arteriole is fairly relaxed
What is tubuloglomerular feedback?
a paracrine signalling mechanism through which changes in fluid flow through the loop of Henle influences GFR
What is the juxtaglomerular apparatus?
a specialized structure in the kidney, crucial for regulating blood pressure and glomerular filtration rate.
What is the mechanism of tubuloglomerular feedback when their is a high blood pressure?
the GFR increases
flow through the tubules increases
flow past the macula densa increases
paracrine signal from the macula densa to afferent arteriole
afferent arteriole constricts
resistance in afferen arteriole increases
hydrostatic pressure in glomerulus decreases
GFR decreases
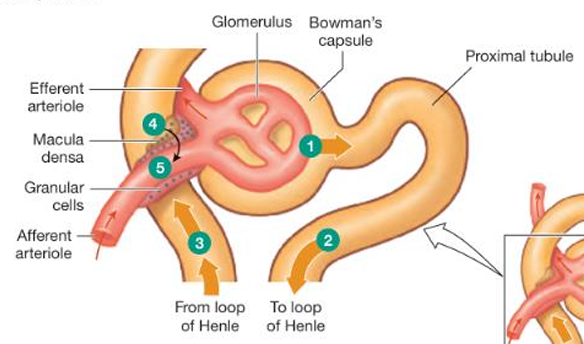
What is the function of the macula densa cells? and what is their role in tubuloglomerular feedback?
act as sensors for sodium chloride concentration in the tubular fluid. The macula densa cells transport NaCl, and that increases in salt transport initiate tubuloglomerular feedback. —They play a crucial role in regulating blood pressure and glomerular filtration rate by initiating tubuloglomerular feedback.
When these cells detect changes in sodium chloride levels, they signal to the juxtaglomerular apparatus, which then adjusts the constriction of the afferent arteriole and renin release.
What is the function of granular cells? and what is their role in tubuloglomerular feedback?
The granular cells secrete renin, an enzyme involved in salt and water balance as well as paracrine signal molecules.
When NaCl delivery past the macula densa increases as a result of increased GFR, the macula densa cells send a paracrine message to the neighboring afferent arteriole. The afferent arteriole constricts, increasing resistance and decreasing GFR.
How can flow be sensed in the renal tubule cells?
by the primary cilia, which are located on the apical surface facing the lumen.
Hormones and the autonomic nervous system alter glomerular filtration rate, in which 2 ways?
changing resistance in the arterioles
altering the filtration coefficient
What part of the nervous system controls GFR through neural pathways?
the sympathetic nervous system
Which blood vessels in the kidney are innervated by sympathetic neurons?
Both the afferent and efferent arterioles
how does the sympathetic system cause vasoconstriction
By sympathetic innervation of alpha-receptors on vascular smooth muscle causes vasoconstriction.
What happens to GFR if systemic blood pressure drops sharply and sympathetic activity increases?
sympathetically induced vasoconstriction of the arterioles decreases GFR and renal blood flow. This is an adaptive response that helps conserve f luid volume.
What is Angiotensin II?
a potent vasoconstrictor
These same hormones may also affect the filtration coefficient by acting on podocytes or mesangial cells. Podocytes change the size of the glomerular filtration slits. If the slits widen, more surface area is available for filtration, and GFR increases.
What is the function of regulated reabsorbtion in the distal nephron?
The regulated reabsorption in the distal nephron allows the kidneys to return ions and water to the plasma selectively, to maintain homeostasis.
What are the 2 reasons for reabsorption?
foreign substances are filtered into the tubule, but not reabsorbed into the blood. this helps clear unwanted molecules from the plasma rapidly
the high glomerular filtration rate, filters ions and water into the tubule. if water and ions reach the distal nephron and are not needed to maintain homeostasis they pass into the urine. with a high GFR this can occur quite rapidly
On what does reabsorption of water and solutes depent? and why?
active transport.
The filtrate flowing out of Bowman’s capsule into the proximal tubule has the same solute concentrations as extracellular f luid. The tubule cells must therefore use active transport to create concentration/electrochemical gradients.
What is the mechanism of renal reabsorption?
active transport of Na+ from the tubule lumen to the extracellular fluid
an electrical gradient is created in which the lumen is more negative than the ECF
anions follow the positively charged Na+ out of the lumen
luminal fluid becomes diluted and increases the concentrations of the ECF
water leaves the tubule by osmosis
loss of volume from the lumen increases the concentration of solutes left behind in the filtrate
solutes diffuse out of the lumen if the epithelium is permeable to them
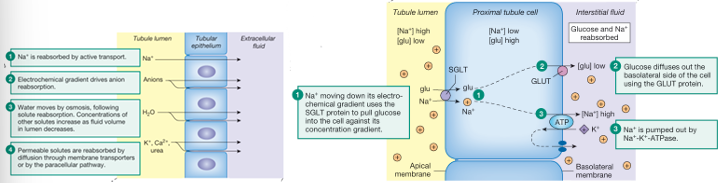
reabsorption involves?
transepithelial transport
paracellular transport
What is transepithelial transport?
Substances cross apical and basolateral membranes of the tubule epithelial cell to reach the interstitial fluid
What is paracellular transport?
Substances pass through the cell-cell junctions between 2 adjecent cells
What is the primary driving force of most renal reabsorption?
the active transport of Na+
What transport proteins is used for apical movement of Na+ ?
In the proximal tubule:
the Na+-H+ exchanger (NHE).
What antiport transport protein is used for basal movement of Na+ ?
once inside the cel Na+ is actively transported out across the basolateral membrane in exchange for K+ by the Na+-K+-ATPase.
A basolateral K+ leak channel prevents K+ from accumulating in the cell. The end result is Na+ reabsorption across the tubule epithelium.
What is responsible for the reabsorbtion of many substances?
Secondary active transport: symport with Na+
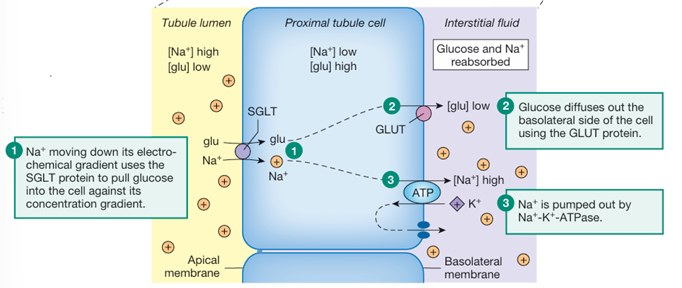
How is glucose transported across the epithelium?
Na+ moving doen its electrochemical gradient uses the SGLT proetin to pull glucose into the cell against its concentration gradient
glucose diffuses out of the basolateral side of the cell using the GLUT protein
Na+ is pumped out by Na+-K+-ATPase
How is urea reabsorbed?
urea can move through the epithelial junctions by diffusion if there is a urea concentration gradient
When Na+ and other solutes are reabsorbed from the proximal tubule, the transfer of osmotically active particles makes the extracellular fluid more concentrated than the filtrate remaining in the lumen.
In response to the osmotic gradient, water moves by osmosis across the epithelium.
When water is reabsorbed, the concentration of urea in the lumen increases.
Once a concentration gradient for urea exists, urea moves out of the lumen into the extracellular fluid by transport through the cells or by the paracellular pathway..
How are plasma proteins reabsorbed?
Filtered proteins are too large to be reabsorbed by carriers or through channels. Most enter the proximal tubule cells by receptor-mediated endocytosis at the apical membrane.
Once in the cells, the proteins are digested in lysosomes. The resulting amino acids are transported across the basolateral membrane and absorbed into the blood.
Most transport in nephrons uses membrane proteins and exhibit 3 characteristics of mediated transport.
these are?
saturation
specificity
competition
What is saturation?
the maximum rate of transport that occurs when all available carriers are occupied by a substrate.
The transport rate at saturation is transport maximum.
At substrate concentrations below the saturation point, transport rate is directly related to …?
substrate concentration
What is the renal threshold for glucose?
The plasma concentration at which glucose first appears in the urine
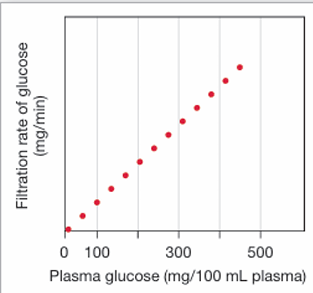
explain the following figure.
the filtration rate of glucose from plasma into Bowman’s capsule is proportional to the plasma concentration of glucose. Because filtration does not exhibit saturation, the graph continues infinitely in a straight line.
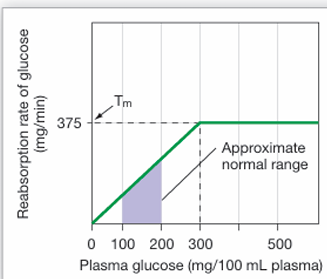
explain the following figure.
The reabsorption rate of glucose in the proximal tubule against the plasma concentration of glucose. Reabsorption exhibits a maximum transport rate (Tm) when the carriers reach saturation.
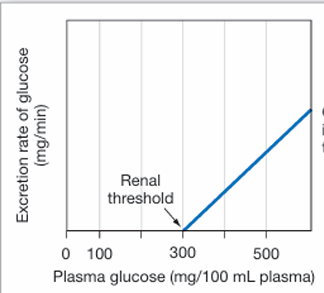
explain the following figure.
The excretion rate of glucose in relation to the plasma concentration of glucose. Excretion = filtration - reabsorption. When plasma glucose concentrations are low enough that 100% of the filtered glucose is reabsorbed, no glucose is excreted. Once the carriers reach saturation, glucose excretion begins.
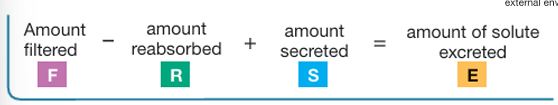
how do you determine the amount excreted?
amount exreted = amount filteres - amount reabsorbed + amount secreted
how do you determine the amount of glucose excreted?
glucose excreted = glucose filtered - glucose reabsorbed
this is because glucose is not secreted
What is glucosuria/glycosuria?
excretion of glucose in the urine. this is indicated an elevated blood-glucose concentration
The hydrostatic pressure that exists along the entire length of the peritubular capillaries is … than the colloid osmotic pressure, so the net pressure gradients favor … .
The hydrostatic pressure that exists along the entire length of the peritubular capillaries is less than the colloid osmotic pressure, so the net pressure gradients favor reabsorption.
What is secretion?
the transfer of molecules from extracellular fluid into the lumen of the nephron. it depends mostly on the membrane transport systems.
Secretion enable the nephron …?
to enhance the excretion of the substance
What type of process is secretion? why?
Secretion is an active process because it requires moving substances against their concentration gradient.
What does the organic anion transporter(OAT) transport? via which process?
the organic anion transporter(OAT) transports a wide variety if endogenous and exogenous anions.
secretion of organic anions on the OAT is tertiary active transport, where the use of energy from ATP is 2 steps removed.