Glomerular Disease Discussion
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
what is nephrotic syndrome characterized by?
1) damage at the glomerulus (either the capillary tuft, the podocytes, and/or the basement membrane
2) loss of large amounts of protein (albumin) in the urine
3) many causes and specific diseases lead to nephrotic syndrome
what is nephritic syndrome characterized by?
1) inflammation at the glomerulus
2) loss of blood in the urine (hematuria)
3) may have protein loss, but blood in urine is more prominent feature
4) many causes and specific diseases lead to nephritic syndrome
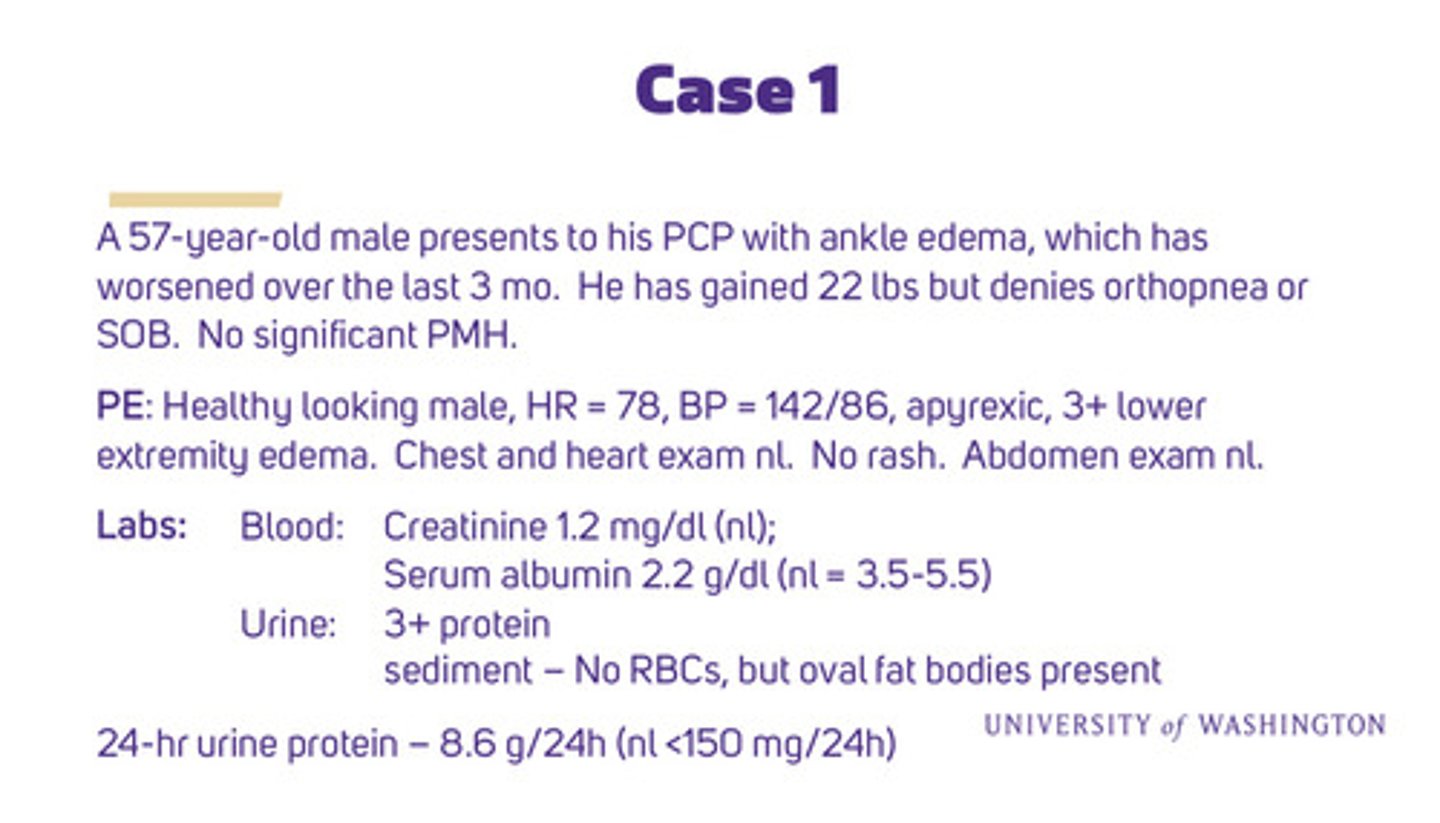
use this case for the following questions
what are the 5 clinical features of nephrotic syndrome
1) proteinuria >3.5 g/24 hours
2) hypoalbuminemia
3) interstitial edema (decreased plasma oncotic pressure + Na+ retention from ENaC activation)
4) hyperlipidemia - partially caused by body trying to quickly make up for low protein
5) lipiduria (oval fat bodies from spilling fat in the urine)
does our case 1 pt have nephritic or nephrotic syndrome?
nephritic syndrome results from inflammation of glomerulus and the characteristic feature is hematuria usually as "casts". pts with nephritic may have HTN and mild proteinuria. our pt has severe proteinuria, hypoalbuminemia, and no hematuria therefore: our pt has nephrotic syndrome
what complications of nephrotic syndrome might the pt develop?
1) low serum oncotic pressure from loss of albumin (plus increased Na+ reabsorption in CCD) —> fluid accumulation in interstitial tissues —> edema
2) renal loss of albumin (necessary for many vital processes), and edema in GI tract leading to poor GI function (impaired nutrient absorption) —> protein malnutrition (deficiency)
3) hypoalbuminemia stimulates liver to synthesize lipoproteins (cholesterols and related fats) to make up for lost albumin —> hyperlipidemia (presents as accelerated atherosclerosis) —> CVD
4) increased hepatic synthesis of pro-coagulation factors (eg fibrinogen) and urinary loss of regulatory factors (eg anti thrombin III, protein C, and protein S) —> hypercoagulability —> thrombosis (often exacerbated by diuretics - volume loss)
5) urinary losses of IgG and complement and impaired cellular immunity —> increased susceptibility to infection (esp by gram positive bacteria)
what are the 3 causes of primary nephrotic syndrome
renal diseases:
1) minimal change disease
2) focal segmental glomerulosclerosis
3) membranous nephropathy
what are the characteristics of minimal change disease
1) most common nephropathy in children under 10 years old
2) good prognosis w steroid tx
what are the characteristics of FSGS
1) most common primary glomerular disease resulting in ESRD (irreversible, scarring)
2) can happen on its own or as a result of another disease or toxin (as can all nephrotic diseases)
what are the characteristics of membranous nephropathy
most common cause of nephrotic syndrome in adults > 60 y/o
what are the 3 causes of secondary nephrotic syndrome
systemic diseases:
1) diabetic kidney disease (30-40% T1DM; 10-20% T2DM)
2) systemic lupus erythematosus
3) amyloidosis
what are the characteristics of diabetic kidney disease
1) most common secondary glomerular disease resulting in ESRD
2) proteinuria indicates kidney damage (glucosuria is an indicator of poor glucose control, not kidney damage)
what are the characteristics of SLE
lupus can have nephrotic and nephritic manifestations
what are the characteristics of amyloidosis
1) abnormal beta pleated sheets of protein deposit in many organs
2) second most common cause of nephrotic syndrome in elderly
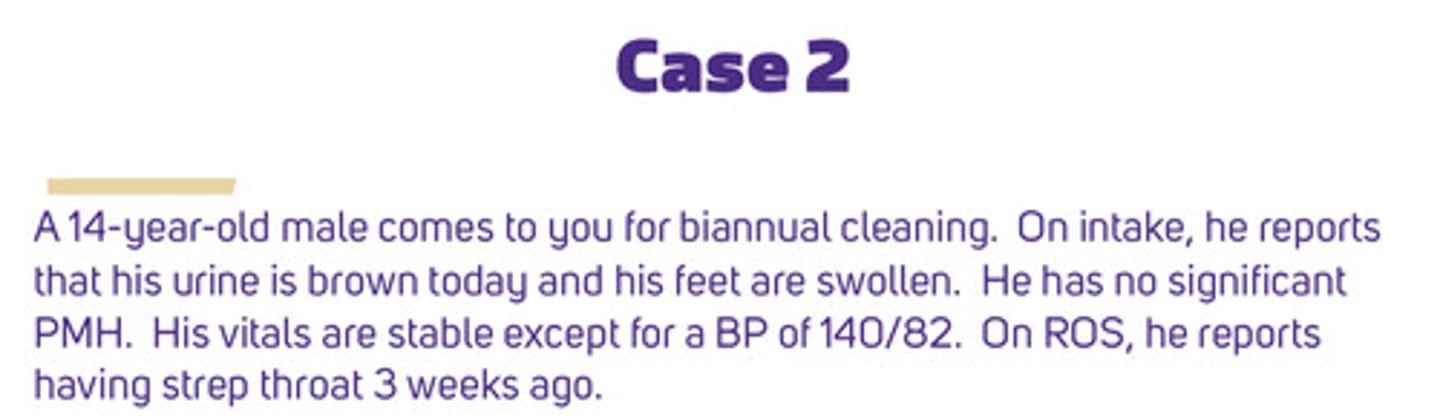
use this case for the following questions
why is case 2 pt's urine brown?
hematuria can appear as pink, red, or brown colored urine. "frank blood" usually describes urine or another excretion with obvious red blood in it. hematuria, esp from nephritis, can be cola or iced tea colored as the heme products are breaking down
what does the case 2 pt have
a child w dark urine a few weeks after strep throat likely has a post streptococcal glomerulonephritis (PSGN), an unpredictable non-infectious consequence of group A streptococcus pharyngitis (immune complexes deposited at the basement membrane of the glomerulus).
pts presents w red or brown urine, HTN, sometimes edema; course is mild to severe —> nephritis (nephritis usually resolves without much consequence, but some pts have prolonged renal dysfunction, with severe episodes requiring dialysis)
what are the 3 causes of primary nephritic syndrome
these are all immune complex glomerulonephritis diseases:
1) post infectious GN (males 5-14 y/o, rarely >65): post streptococcal - PSGN
2) IgA nephropathy: the most common cause of GN in the world (unknown why mesangial IgA deposits cause damage)
3) rapidly progressive GN (RPGN can reach ESRD in few weeks if untreated): can result from severe PSGN or IgA GN or from a long list of other diseases like anti-GBM (glomerular basement membrane)
what are the 2 causes of secondary nephritic syndrome
1) immune complex GN; autoimmune (lupus nephritis), females 10-40 y/o: SLE, RA
2) ANCA/vasculitis (anti-neutrophil cytoplasmic antibodies): multiple systemic small vessel vasculitis syndromes (will usually involve kidneys): wegener's, churg-strauss, microscopic polyangiitis (these can also affect lungs and other parts of the body)
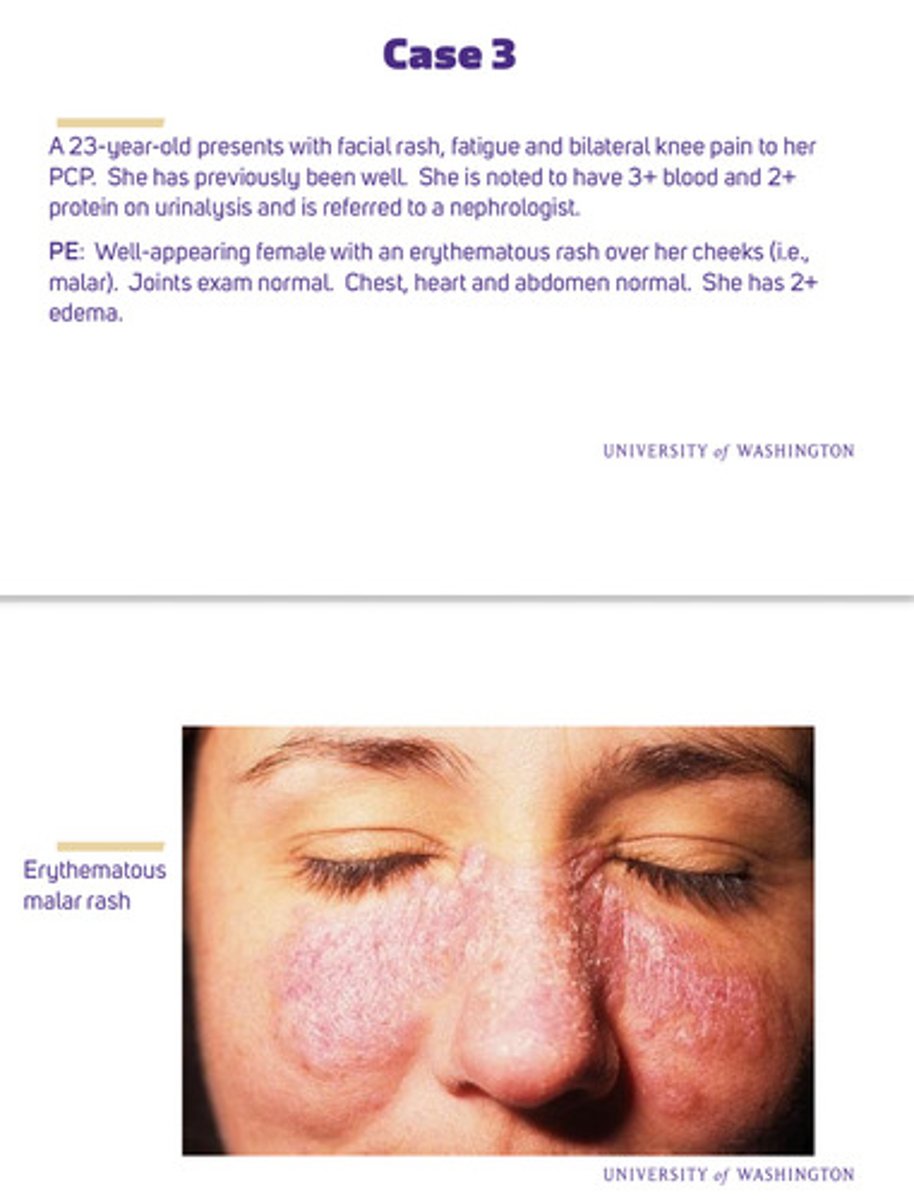
use this case for the following questions
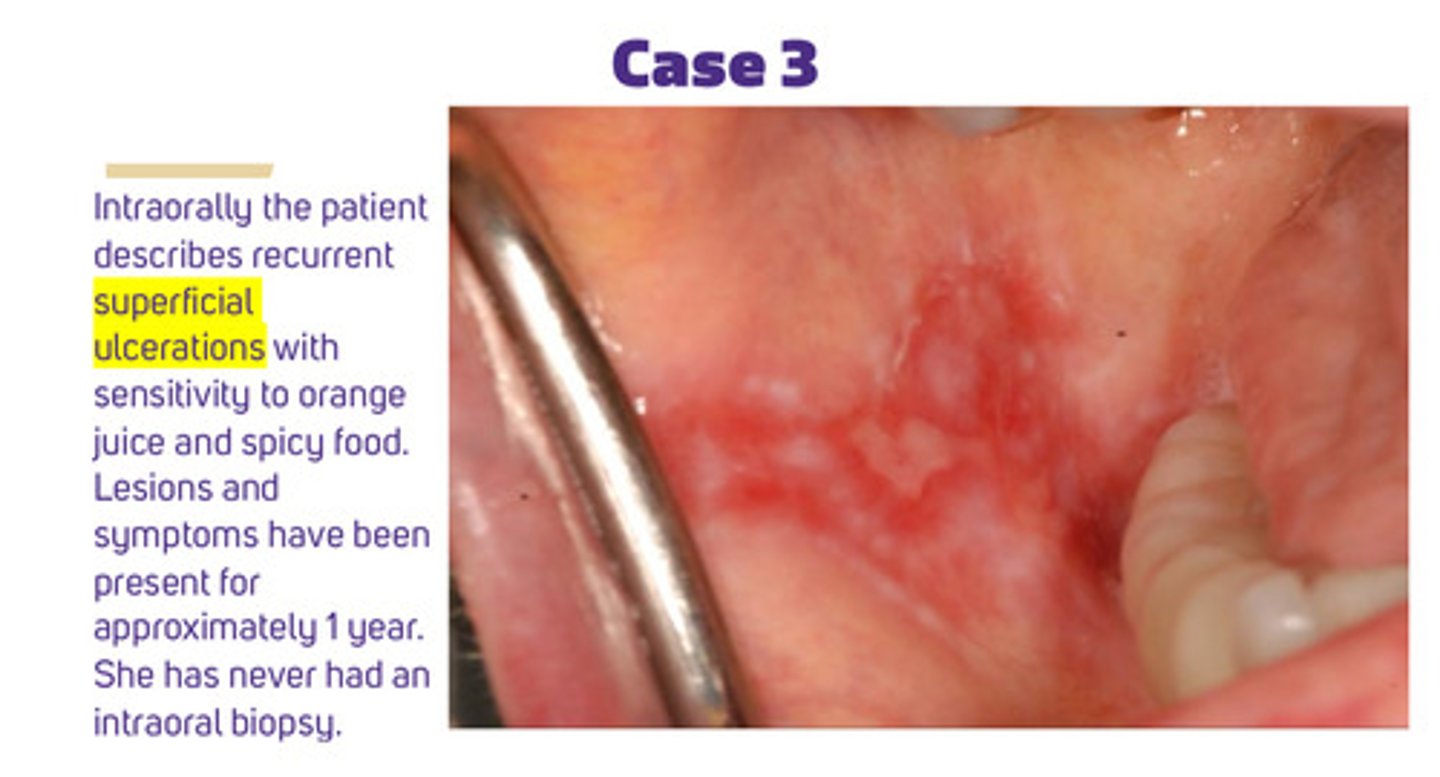
intraorally, case 3 pt describes recurrent superficial ulcerations with sensitivity to orange juice and spicy food. the lesions and symptoms have been present for approximately 1 year. she has never had an intraoral biopsy.
what systemic disorder might this case 3 pt have?
the combination of fatigue, arthralgia, malar rash, cytopenias, and renal involvement in a young woman is highly suggestive of systemic lupus erythematosus
what are typical features of SLE or lupus
1) often a combination of fatigue, fever, myalgia, arthralgia, malar rash, and renal involvement
2) more common in young adult females
3) alopecia, mouth ulcers, serositis, photosensitivity, thrombotic disease, cardiac disease, ophthalmologic disease, neurologic changes
4) mild to extremely debilitating and life-threatening, often w flare ups
why is SLE very complicated to diagnose? what tests might help w diagnosis?
anti nuclear antibody (ANA) is found in most pts with SLE (sensitive), but also in other diseases too (not specific). additional testing might include complement C3 and C4 level and anti-phospholipid antibody panel
describe the extent of kidney involvement in SLE
1) very common and ranges widely from mild, asymptomatic hematuria to nephrotic syndrome (lupus membranous) to AKD from a severe proliferative glomerulonephritis
2) enhanced risk of ESRD (transplant, dialysis)
how is SLE usually treated
1) a variety of meds, but most of them are immunosuppressive
2) when kidney is involved, stronger immunosuppression is required w steroids
3) from dental perspective: immunosuppression increases her risk of infection, including yeast and caries (also for squamous cell dysplasias)
how would you first definitively confirm the case 3 pt's diagnosis
biopsy is indicated to confirm the dx! clinical lesions in lupus can minis other autoimmune conditions (esp oral lichen planus). biopsy is necessary as the cause cant be presumed simply from lupus in her PMH. the lesion may represent a different process or a dysplastic/pre-malignant area
how would you treat the case 3 pt's oral lesion
1) topical steroids are first line tx for oral lesions confirmed to be caused by lupus
2) dexamethasone rinse would be appropriate initial therapy
3) for pts with active lupus, coordinate care w their PCP
pts with SLE are at risk for secondary autoimmune diseases like myasthenia gravis and sjögren's syndrome. what is sjögren's syndrome?
an inflammatory autoimmune disease that targets exocrine glands (primarily the salivary and lacrimal glands - but any moisture producing gland)
what does sjögren's syndrome lead to?
decreased salivary output and the risk for xerostomia —> dental caries, candidiasis, halitosis, etc
individuals with sjogrens are at a very increased risk of what?
44x increased risk for mucosal associated lymphoid tissue (MALT) lymphoma, primarily in the parotid glands. oral physicians need to know this association because they observe parotid and mucosal tissue daily and are important safety nets to catch this disease early
in the diagnostic criteria for sjogrens (including dry eyes), the oral symptoms include at least one of the following:
1) symptoms of dry mouth for at least 3 months
2) recurrent or persistently swollen salivary glands
3) needs for liquids to swallow dry foods
summary of nephrotic syndrome in terms of: disorder of, predominant cell injury, proteinuria, edema, BP, urine sediment, GFR
1) disorder of: glomerular filtration barrier
2) predominant cell of injury: podocyte
3) proteinuria: >3.5 g /24 hours
4) edema: 3-4+
5) BP: variable
6) urine sediment: lipiduria
7) GFR: normal/slow decrease
summary of nephritic syndrome in terms of: disorder of, predominant cell injury, proteinuria, edema, BP, urine sediment, GFR
1) disorder of: glomerular inflammation
2) predominant cell of injury: mesangial/endothelial
3) proteinuria: variable
4) edema: mild
5) BP: elevated
6) urine sediment: dysmorphic RBC and casts
7) GFR: faster decrease/RPGN