Week 11: Kidneys
1/364
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
365 Terms
Renal means
pertaining the to kidneys
Functions of the kidneys
Regulate the water and ionic composiiton of the body
Excrete waste products in the urine
Excrete foreign chemicals
Produce glucose during prolonged fasting (Gluconeogenesis)
As an endocrine gland - Release factors and hormones into the blood (Renin, 1,25-dihydroxyvitamin D, and
Erythropoietin)
Examples of metabolic waste products the kidneys excrete
Urea (from protein)
Uric acid (from nuclei acid)
Creatinine (from muscle creatine)
Erythropoietin produced by the kidney does what
controls erythrocyte production
Renin produced by the kidney does what
is an enzyme that controls the formation of anghiotensin, which influences blood pressure and sodium balance
1,25-dihydroxyvitamin D produced by the kidney does what
influences calcium balance
Kidneys location
Back of the abdominal wall in the retroperitoneal space - behind the peritoneum (lining of the abdominal cavity)
Urine flow sequence
Kidneys → Ureters → Bladder → Urethra → Environment
Ureters function
transport urine from kidneys to bladder
Bladder function
stores urine until voided from body
Urethra function
carries urine from bladder to the outside of the body
Blood flow through kidneys sequence
Aorta → Renal arteries → Renal circulation → Renal veins
Structural and Functional unit of the kidneys
Nephrons
Nephron consists of
Renal corpuscle and a Renal tubule
Juxtamedullary nephrons
Renal corpuscle located in cortex just next to the medulla and have long loops of Henle that penetrate deep into the medulla
Two types of nephrons
Juxtamedullary
Cortical
% of nephrons that are Juxtamedullary
15%
% of nephrons that are Cortical
85%
Cortical nephrons
have short or no loops of Henle
Efferent arterioles of juxtamedullary nephrons give rise to
Vasta recta - long looping capillaries
Efferent arterioles of cortical nephrons give rise to
peritubular capillaries
About how many nephrons are in 1 kidney
1 million
Renal corpuscle consists of
Glomerulus (capillary tuft) and a Bowman’s Capsule (which the tuft protrudes into)
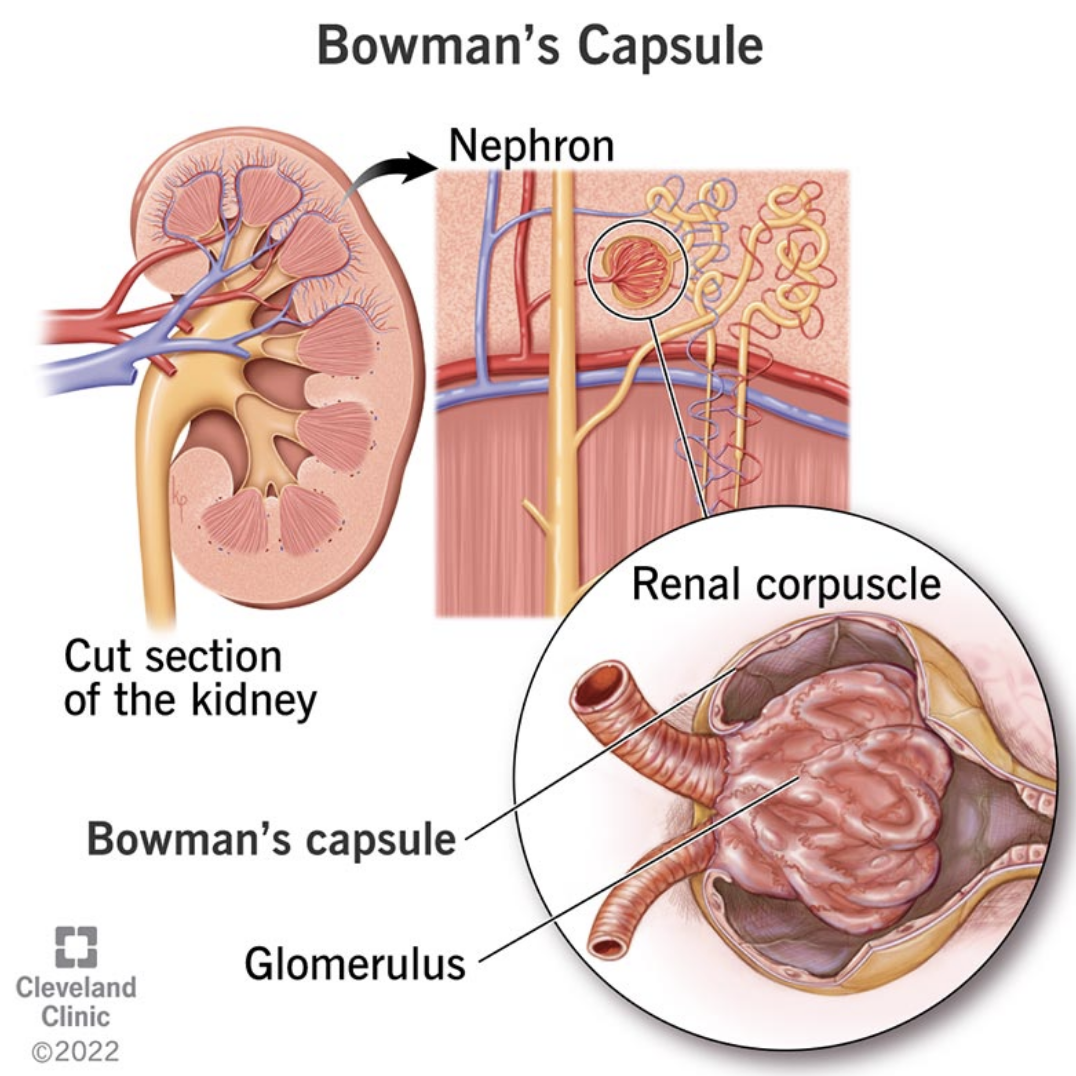
Bowman’s Space
within the Bowman’s capsule from which fluid flows into the start of the nephron tubule
Fluid flow sequence in Nephron
Glomerulus → Bowman’s Capsule → Proximal Convoluted Tubules→ Loop of Henle (descending and ascending limbs) → Distal Convoluted Tubules → Collecting ducts (cortical and medullary)
Substance filtration sequence in the renal corpuscle
Capillary pores b/w endothelial cells → basement membrane → filtration slits b/w the foot processes (pedicles) → enters capsular space → lumen of proximal convolutes tubule
Multiple collecting ducts in the kidneys join and empty into
the renal pelvis, from which urine flows through the ureters → bladder
The capillaries of the glomerulus are
fenestrated, which allows large amounts of solute-rich fluid to pass between the epithelial cells
Glomerulus is supplied with blood by
an Afferent arteriole
As blood flows through the Glomerulus, how much plasma is filtered into the Bowman’s capsule
20%
Glomerulus blood is drained by
an Efferent arteriole
Efferent arteriole leaving the Glomerulus
branch into peritubular capillaries, which supply the tubule
Only capillaries in the body that are fed and drained by an arteriole
glomerular capillaires
Vasa recta
long capillary loop that runs next to the loop of Henle
How many layers of filtration barrier is in the renal corpuscle
3
Filtration barriers in the renal corpuscle
Capillary endothelium
Glomerulus basement membrane
Bowman’s capsule epithelium (podocytes); mesangial cells
Podocytes
cells making up the epithelial lining of Bowman’s capsule - inner layer of the glomerular filtration barrier
Podocytes posses a large number of
extensions/foot processes, which surround the basement membrane
Filtration slits
clefts between the podocytes; as the filtrate passes through them, it enters the capsular space
Mesangial cells
modified smooth muscle cells in the glomerulus that helps regulate the blood flow in the glomerulus by contraction, which reduces the surface area available for filtration
Fluids free of proteins from the glomerulus filter into the
Bowman’s space
Juxtaglomerular Apparatus
composed of the macula densa (patch of tubular wall cells at end of ascending limb of the loop of Henle) and juxtaglomerular (JG) cells (afferent arteriole wall cells that secrete renin)
Macula Densa
Apart of Juxtaglomerular apparatus - patch of tubular wall cells at end of ascending limb of the loop of Henle
Macula Densa cells function
senses changes in the NaCl content of the filtrate
Helps to regulate sodium balance and blood pressure
Juxtaglomerular (JG) cells
Apart of Juxtaglomerular apparatus - afferent arteriole wall cells that secrete renin in response to decrease in stretch)
3 basic renal processes
Glomerular filtration
Tubular reabsorption
Tubular secretion
Tubular secretion
Movement of a substance from Peritubular capillary to Tubular Lumen
Most important substances that enter the forming urine by tubular secretion
Hydrogen ions and Potassium ions, some creatinine (organic anions) as well
Tubular secretion is important mechanism for
Disposing of drugs and drug metabolites
Eliminating undesired substances or end-products that have been reabsorbed by a passive process
Removing excess K+ from the blood
Controlling blood pH
Tubular Reabsorption
Movement of a substance from Tubular Lumen to Peritubular Capillary
Can occur through transcellular or paracellular transport
transport can be active or passive
Amount excreted =
Amount filtered + Amount secreted - Amount reabsorbed
Urine formation begins with
glomerular filtration - essentially protein-free plasma into Bowman’s space
Glomerular Filtration
a bulk-flow passive process in which hydrostatic pressure forces water and all low-molecular weight substances through a filtration barrier
The glomeruli in the kidney are a much more efficient filter compared to other capillary beds in the body b/c:
the glomerular filtration barrier has a large surface area and is very permeable to water and solutes
the glomerular capillary blood pressure is higher (60 mmHg) than in typical systemic capillary
Main reabsorptive force keeping water in the glomerular capillaries
the osmotic force due to the presence of protein in the plasma
Hematuria
Blood cells in the urine
Proteinuria
Protein in the urine
Hematuria or proteinuria indicates
potential problems with the glomerular filtration barrier
Glomerular filtration rate per day
180 L/day of essentially protein-free plasma
Glomerular filtrate contains
all plasma substances other than proteins (and substances bound to proteins) in virtually the same concentrations as in plasma
Glomerular filtrate concentration is the same as
plasma
Glomerular filtration pressure is driven by
Starling forces - hydrostatic pressure in the glomerular capillaries and is opposed by both the hydrostatic pressure in Bowman’s space and the osmotic force due to the proteins in the glomerular capillary plasma
Forces involved in glomerular filtration
Glomerular capillary blood pressure
Fluid pressure in Bowman’s space
Osmotic force due to protein in plasma
Force involved in glomerular filtration FAVORING filtration
Glomerular capillary blood pressure
Force involved in glomerular filtration OPPOSING filtration
Fluid pressure in Bowman’s space
Osmotic force due to protein in plasma
GFR
Glomerular Filtration Rate
Glomerular Filtration Rate (GFR)
the volume of plasma filtered from glomerular capillaries into Bowman’s space per unit time
Glomerular Filtration Rate (GFR) is determined by
net filtration pressure
the permeability of the corpuscular membranes
the filtration surface area
Glomerular filtered load =
GFR × plasma concentration of filtered substance
Constriction of afferent arteriole =
decreased GFR
Dilation of efferent arteriole =
decreased GFR
Constriction of efferent arteriole =
increased GFR
Dilation of afferent arteriole
increased GFR
Renal tubule
a long cylinder, extending from Bowman’s capsule to the collecting ducts of the nephrons; consists of several parts
Parts of the renal tubule
Proximal convolutes tubule
Loop of Henle
Distal convoluted tubule
Collecting duct
Metabolism by the tubules
Renal tubule cells can synthesize glucose during fasting and add it to the blood
Can catabolize certain organic substances such as peptides, taken up from either the tubular lumen or peritubular capillaries. Catabolism eliminates these substances from the body as if excreted into the urine
By the time the filtrate reaches the medullary collecting ducts
modification has been finished and the finished product is urine
The most abundant cation in the filtrate
Na+
Substances to which the tubular epithelium is permeable are reabsorbed by diffusion
because water reabsorption creates tubule-interstitial-fluid-concentration gradients
Active reabsorption of a substance requires the participation of transporters in the
apical membrane (between tubular lumen and cell) or basolateral membrane (between interstitial space next to capillaries and cell)
Tubular reabsorption rate is high for
nutrients, ions, and water
Tubular reabsorption rate is low for
waste products
Transport maximum is exhibited by
substances moved by mediated transporters
Regulation of membrane channels and transporters
achieved by hormones and paracrine or autocrine factors
If the filtered load of a substance exceeds the reabsorptive transport maximum
the substance will be excreted in the urine
Role of proximal tubule
reabsorbs most filtered water and solutes, and is the major site of tubular secretion, with the exception of K+ ions
Role of Loop of Henle
reabsorbs large amounts of major ions and to a lesser extent, water
Diabetic nephropathy
when diabetes mellitus (hyperglycemia) is poorly controlled. Filtered load of
glucose exceeds reabsorptive transport maximum so glucose “spills” into the urine, which can lead to decrease in renal function
Familial Renal Glucosuria
defect in the glucose transporter
Renal Clearance of any substance
is the volume of plasma from which that substance is completely removed (“cleared”) by the kidneys per unit time (e.g., units are in mL/min)
Clearance formula
Cs = UsV / Ps
= (urine concentration of S x Urine volume per unit time) / plasma concentration of the substance
Importance of Glucose clearance
it is important not to lose glucose in the urine, it is completely reabsorbed so its renal clearance rate is zero in healthy people
Renal clearance of substance > GFR means
the substance must undergo tubular secretion
Renal clearance of substance < GFR means
the substance must undergo some reabsorption
GFR of Inulin
= clearance rate
small carbohydrate that is filtered but not reabsorbed or secreted; infused experimentally
How to estimate GFR clinically
with Creatinine clearnace b/c it is filtered, not reabsorbed, and secreted only a little
Renal plasma flow is estimated by
the clearance of a substance that is filtered, not reabsorbed, and 100% secreted. All that enters the kidneys from the blood is cleared.
Micturition
Urination
Spinal micturition reflex is
involuntary
Spinal micturition reflex
Bladder distension stimulates stretch receptors that trigger spinal reflexes
These reflexes lead to contraction of the detrusor muscle (bladder smooth muscle).
mediated by parasympathetic and sympathetic neurons
mediated by relaxation of both the internal and the external urethral sphincters (inhibition of neural input)