renal disorders
1/50
Earn XP
Description and Tags
Pathophysiology exam 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
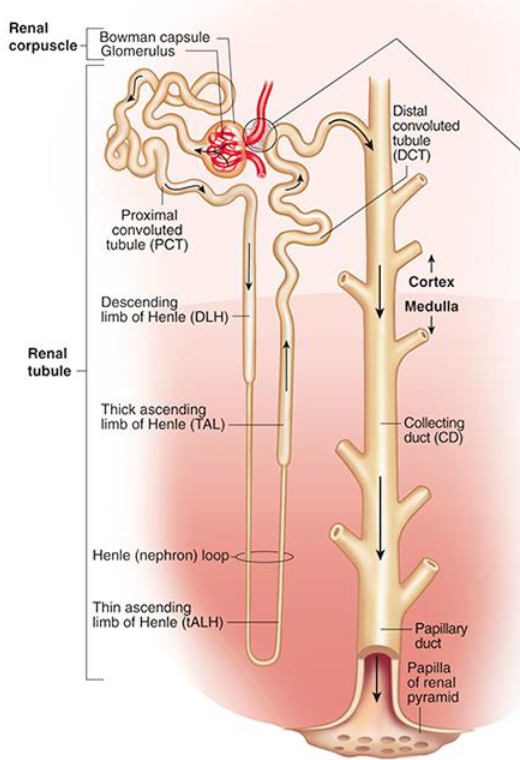
nephron
functional unit of kidney and contains the glomerulus.
– urine flows from bowman’s capsule →proximal convoluted tubule →loop of Henle →distal convoluted tubule →collecting duct
– surrounding blood vessels=reabsorb water & solutes
renal(urinary) system
__/__ system functions:
– maintaining fluid electrolyte balance, maintain acid-base balance, regulate BP, release erythropoietin to stimulate RBC production, and activate vitamin D
glomerulus
bundle of capillaries that sit within Bowman’s capsule—site of filtration
juxtaglomerular cells
regulation of urine/fluid balance + BP: release renin in response to low BP.
– renin converts angiotensinogen →angiotensin which is then converted into angiotensin II (by ACE [angiotensin converting enzyme])
– angiotensin II promotes vasoconstriction and release of aldosterone (adrenal cortex)
antidiuretic hormone (ADH)
regulation of urine/fluid balance + BP: released by posterior pituitary in response to ↓BP or ↑serum osmolality
– ADH promotes fluid reabsorption from collecting duct (retains water and increases BP)
ANP and BNP (natriuretic peptides)
regulation of urine/fluid balance + BP:
– promotes excretion of Na and H2O-fluid output, reduces BP
– released by heart in response to heart stretching
acid base balance
during acidotic states, kidney promotes
– excretion of H+, Reabsorption of HCO3-, Synthesizing new HCO3-
during alkalotic states, kidney promotes
– Retention of H+
simple cysts
pocket of fluid on kidneys, single or multiple, can be unilateral or bilateral
– no signs or symptoms but maybe flank pain/hematuria
Autosomal dominant polycystic kidney disease
(ADPKD)
genetic condition and most common renal cystic disease
– two gene mutations lead to excessive growth+differentiation of epithelial cells →destructive, fluid filled cysts in the kidney and other organs (cysts detaching and growing elsewhere)
– renal tissue damage is prob due to= Inflammatory mediators or Apoptosis of renal tubule cells
– asymptomatic for yrs
true
(T/F) ADPKD can lead to issues elsewhere, such as diverticuli or aneurysms in cerebral arteries
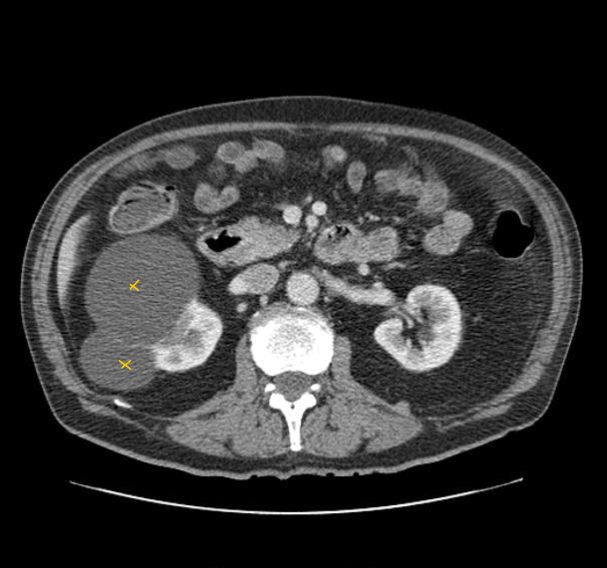
renal calculi
nephrolithiasis- kidney stones- masses of crystals, proteins, etc. that obstruct urine flow
– composed of particles usually excreted in urine. usually form in kidney but can start anyway in urinary tract
–influential factors: high concentration of ^particles in blood stream, hydration status, metabolism
renal calculi formation
requires supersaturated urine, depends on urine pH (alkaline ↑ risk) and ion concentration.
– requires nucleus that facilitates stone formation: Small crystal cluster held by ionic forces and Organic materials from epithelium
– flank pain radiating to groin+nausea
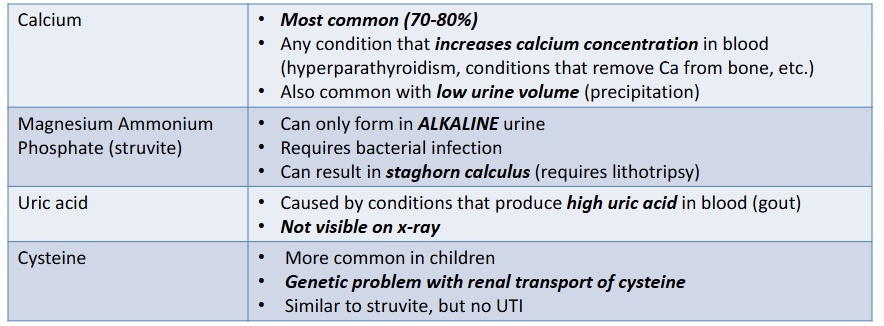
calcium stones
most common kidney stones (70-80%)—conditions that ↑serum Ca2+ or ↓fluid volume will ↑risk of calcium stones
– hyperparathyroidism or ↑reabsorption of bone
struvite stones
Magnesium ammonium phosphate (__) stones- often associated w bacterial infection/UTI (common in AFAB)
– bacteria secrete urease which converts urea →ammonia which makes urine alkaline and this promotes formation of stone
– can grow into staghorn calculi (pic)

uric acid stone
type of renal calculi: occurs in ppl who excrete large amounts of uric acid in their blood (ppl w gout/abnormal metabolism of purines)
– linked w ↑amount of purines in diet (meat/beer) and not visible on x-ray
cysteine stone
type o7f renal calculi: amino acid that precipitates more readily in acidic urine, common in kids
– conditions that ↑cysteine in blood (genes) will ↑cysteine in urine and ↑risk of __ stones
types of renal calculi
urinary tract infections
inflammation of urinary epithelium (anywhere here)
– usually caused by bacterial infection or E.Coli
– occurs from bad hygiene + prevented by urine washing out bacteria in urethra 🚽
normal host defenses
urinary protection
– Washout phenomenon: urination washes pathogen out of urethra
– Protective mucin layer: lines bladder +prevents attachment&infection
– Ureteral peristalsis: moves urine and pathogens down from kidneys
– Low urine pH inhibits bacterial growth
– Normal flora of periurethral area →lactobacillus defends against uro-pathogens
increased uti risk
factors contributing to UTI
– Pathogen’s virulence: presence of pili/fimbraie helping adherence
– ↓urinary flow, obstruction, of reflux
– catheterization, antibiotics that kill normal flora (lactobacillus), DM, or pregnancy
acute cystitis
inflammation of bladder-most common site of UTI
– often due to retrograde movement of E. Coli up urethra (coli releases inflammation inducing toxins).
– some strains’ fimbriae attach to epithelium & flagella moves it up uri tract
acute cystitis manifestations
issues associated with __
– inflammation →bladder edema →stimulates stretch receptors that create a sensation of fullness (frequency +urgency +dysuria)
– low back pain, hemorrhagic cystitis (blood in urine), foul urine
– older ppl may display mental changes
acute pyelonephritis
infection of upper urinary tracts—kidneys+ureters=often AFAB
– results from ascending infection from bladder (or from bloodstream access).
– fever, flank pain, chills, uti symptoms (stretching of bladder)
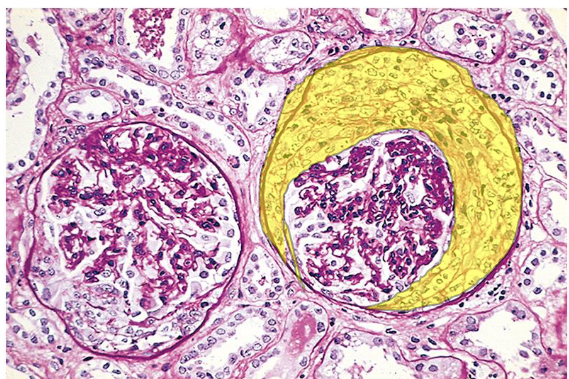
glomerulonephritis
inflammation of glomerular structures—2nd leading cause of kidney failure in US
glomerular disease
causes of __ __:
1) Immunologic (most common): antibodies reacting w glomerular antigens. or antigen-antibody complexes r trapped
2) Non-immunologic: Diabetic nephropathy, Hypertensive nephropathy, Toxic meds
3) Hereditary
– 3 main changes: Proliferation: cell number↑ and form “crescents”, Basement membrane thickens, and Sclerosis: accumulation of proteins&collagen obstructing glomerulus
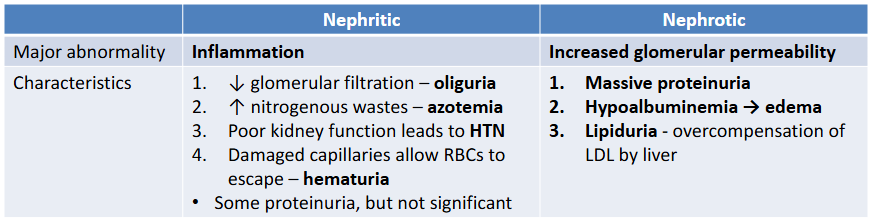
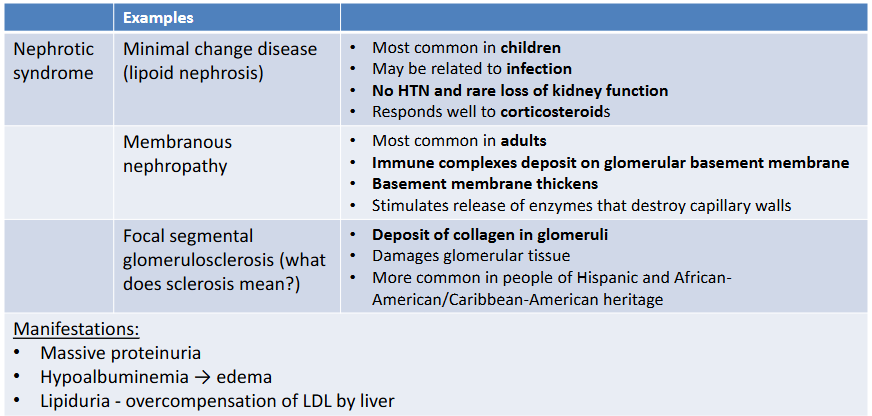
Nephritic syndrome
glomerular disease characterized by Inflammation of glomeruli
– presents as: oliguria (cant filter/produce urine)→ hypertension (BP↑), azotemia (buildup of nitrogenous waste), hematuria (from inflammation)
conditions w __ __: post-infectious glomerulonephritis or rapidly progressive (crescents) glomerulonephritis
nephrotic syndrome
glomerular disease characterized by increased glomerular permeability 🕳
– presents as: profound proteinuria, hypoalbuminemia (w/o albumin, water leaks into interstitial space) →edema, and lipiduria w compensatory hyperlipidemia
– conditions w __ __: Minimal change disease, Membraneous nephropathy, Focal segmental glomerulosclerosis
Nephritic vs. Nephrotic syndrome
post-infectious glomerulonephritis
type of nephritic syndrome: common in kids
– Follows group A β-hemolytic strep infection
– Antibodies form against strep antigens and Antigen-antibody immune complexes form
– ^ Complexes deposit in glomeruli → trigger inflammation
– Leads to glomerular cell proliferation and leukocyte infiltration
– presents w nephritic syndrome’s symptoms+fever
Rapidly progressive (crescentic) glomerulonephritis
type of nephritic syndrome: glomerular disease with crescent formation and rapid renal decline
started by either:
1) Immune complexes in glomerulus promoting inflammation
2) Anti-GBM antibodies (IgG) stimulate inflammation
– Inflammation → proliferation of Bowman’s capsule cells 🌙 + leukocyte infiltration → crescents obliterate Bowman’s space
– presents w nephritic syndrome symptoms
true
(T/F) In Rapidly progressive (crescentic) glomerulonephritis, a syndrome called Goodpasture syndrome can occur where IgG also targets alveolar basement membrane → pulmonary hemorrhage + renal failure
nephritic syndrome types
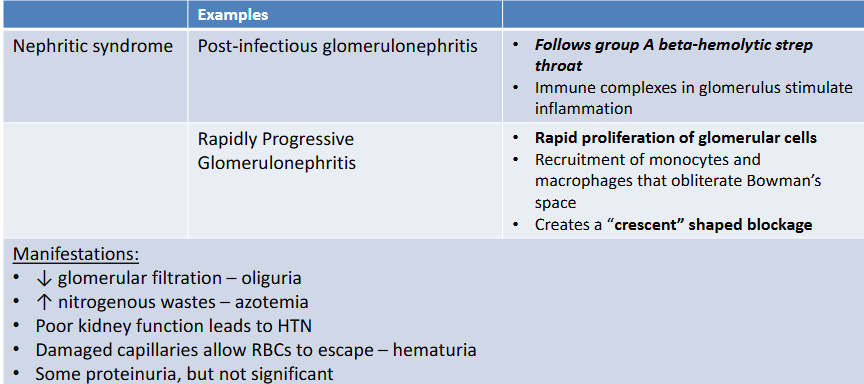
minimal change disease
or lipoid nephrosis—benign+most common cause of nephrotic syndrome in kids
– due to immune reation resulting in epithelial cell damage yielding ↑permeability + proteinuria. linked w respiratory illness
– nephrotic syndrome symptoms+good renal function remains
membranous nephropathy
type of nephrotic syndrome: inflammation/thickening of glomerular basement membrane—common cause of glomerular disease
– Deposits of antigens +IgG antibodies form
btwn basement membrane of glomerular capillaries and Bowman’s capsule→ Activation of inflammation
– yields ↑ capillary permeability and thickening of basement membrane
– presents nephrotic syndrome symptoms
focal segmental glomerulosclerosis
nephrotic glomerular disease w sclerosis of some glomeruli—common in black+hispanic ppl
– circulating cytokine induce epithelial cell injury thus plasma proteins + collagen etc. become deposited→ scar tissue forms sclerosis
– nephrotic syndrome symptoms
types of nephrotic syndrome
wilms tumor
tumor on kidney composed of elements resembling fetal tissue-due to genetic mutation (aniridia or hemihypertrophy)
–manifests as large abdominal mass and HTN (kidney issues)
– common w kids + managed w surgery/chemo
hemihypertrophy
one half of body is larger than the other half—congenital abnormalities
– associated w wilms tumor
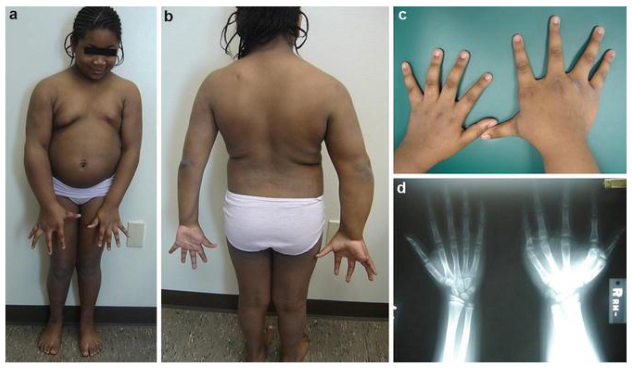
aniridia
congenital abnormality charactered by no colored iris—all black

renal cell carcinoma
cancer of kidneys, accounts for 80% of renal neoplasms
– manifests as hematuria, flank pain, palpable mass, fatigue/weightloss
– risk factors: smoking, obesity, HTN, NSAIDS
acute kidney injury
sudden decline in renal function, ↓ in glomerular filtration with ↓ urine output →↑ retention of nitrogenous wastes, K+ and PO4-
– etiologies:
Pre-renal: disorder marked by ↓renal perfusion
Intra-renal: marked by poorly functioning renal tissue (glomerular disease)
Post-renal: marked by obstruction of uri tract (kidney stones)
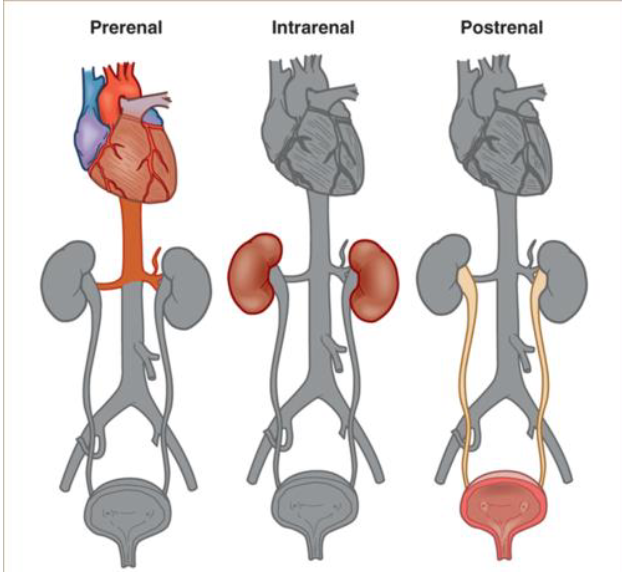
pre renal etiology
most common cause of acute kidney injury— problem getting blood to kidney
– ↓renal perfusion results in ↓filtration which promotes retention of fluids+nitrogenous wastes
– may be due to: hypovolemia, sepsis ↓cardiac output (MI or HF)
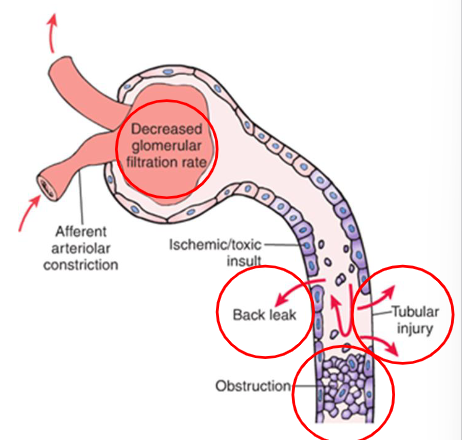
intra-renal etiology
kidney cant make urine -may cause AKI
– usually results from acute tubular necrosis (ischemic or nephrotoxic ATN)
– may also be from glomerulonephritis, vascular disease (HTN, DIC) or cancer/infection
acute tubular necrosis types
two types of ATN:
– Ischemic ATN: damage to renal cells due to prolonged ischemia and hypoxia
– Nephrotoxic ATN: damage of renal cells due to a toxin (IV contrast/antibiotics), heavy metals (mercury/arsenic), or bacterial toxins
– both results in intra-renal injury
acute tubular necrosis
destruction of renal tubule epithelial cells w suppression of renal function
– damage leads to necrosis of epithelial cells which obstruct lumen of renal tubule →↑ pressure in lumen →↓glomerular filtration. fluid leaks from nephron into interstitial tissue
post renal etiology
cant get urine out of body (uncommon)
– obstruction of urinary tract bilaterally→↑pressure in uri tract lumen, GFR gradually declines → several hrs of anuria+flank pain leads to polyuria
AKI phases
– Progressive condition:
1) Onset.
2) Oliguric phase: ↓ GFR, low urine output, fluid and nitrogenous waste retention, maybe neuro symptoms
3) Diuretic phase: healing begins, only ↑ urine output
4) Recovery phase: filtration and waste clearance return to normal & tubular edema resolves
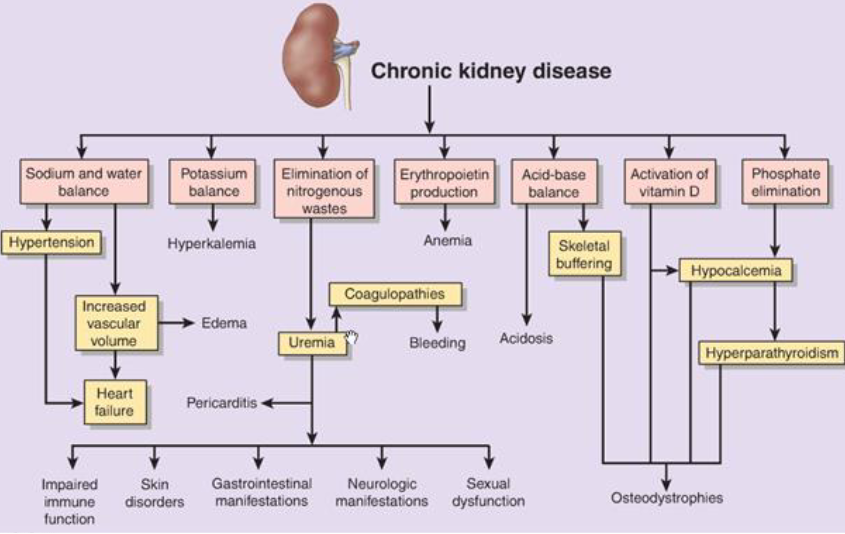
chronic kidney disease
progressive loss of kidney function due to permanent loss of nephrons (due to systemic disease-HTN, DM)
–nephron loss begins in response to severe/prolonged injury →fibroblast proliferation →focal segmental glomerulosclerosis and interstitial fibrosis
– no symptoms until renal function below 25% normalcy
CKD manifestations
manifestations of __ __ __
– Azotemia: retention of urea, creatinine+other nitrogenous wastes. can lead to uremic syndrome (nausea, diarrhea, pruritis)
– Metabolic acidosis: H+ not excreted and may require dialysis
– Fluid/electrolyte imbalance: potassium cannot be excreted, Na and H2O retention (HTN),
– – PO₄³⁻ binds to Ca²⁺ → hypocalcemia→ ↑ PTH release → bone resorption increases (bc of no free calcium)
– Proteinuria (form renal damage)
– Anemia- damaged kidney cannot secrete erythropoietin
– Neurologic complications- bc of nitrogenous wastes and K damaging neurons→ hiccups, muscle cramps, twitching, impaired memory/judgement
ckd
bladder cancer
most frequent form of uri tract cancer in US, with unknown cause
– manifests as painless hematuria, dysuria--frequency, urgency
– managed w surgery/chemo