Comprehensive Lower Limb Anatomy and Injury Review for Students
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
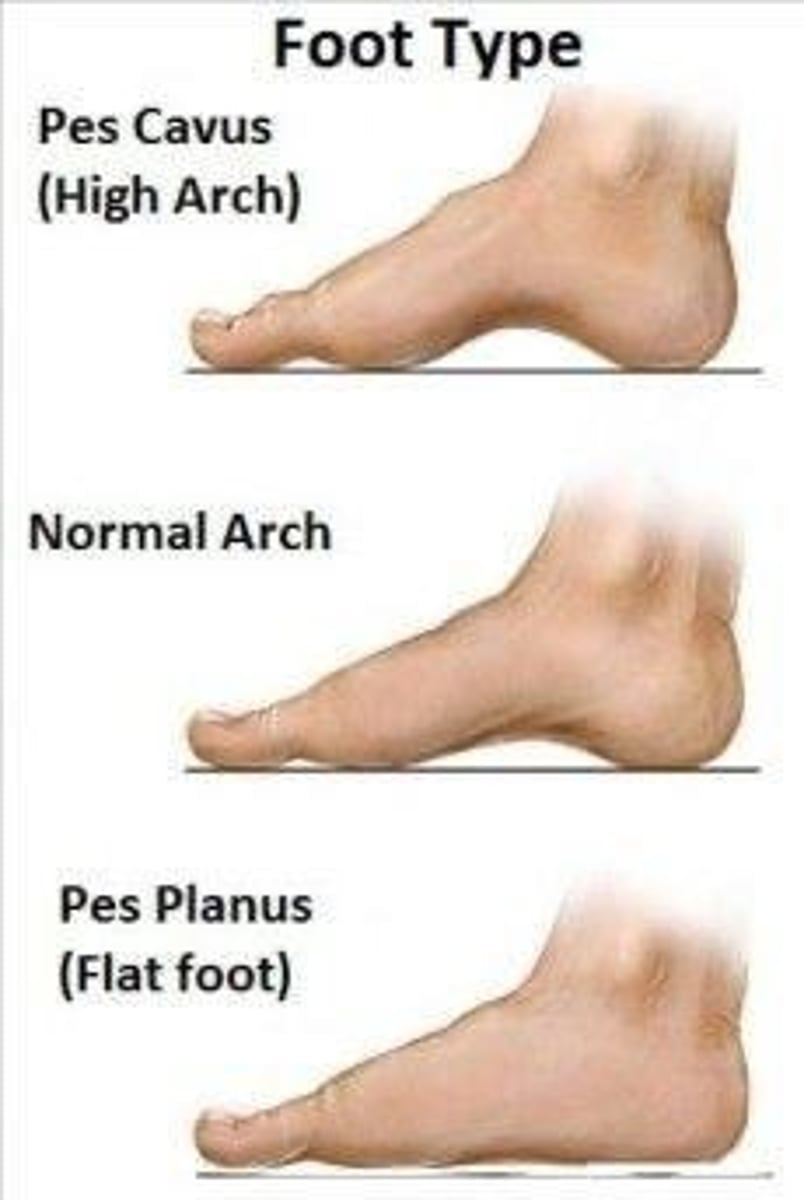
What are Pes Planus and Pes Cavus classified as?
Not pathologies per se, but factors that change normal movement patterns and can facilitate other conditions developing.
What is the most common mechanism of injury for lateral ankle sprains?
Inversion and plantarflexion.
What are the characteristics of a Grade 1 ankle sprain?
ATFL stretched ligament, slight and local edema and ecchymosis, no instability, and full weight-bearing.
What defines a Grade 2 ankle sprain?
ATFL, CFL Partial tear, moderate to local edema and ecchymosis, slight instability, and difficulties with weight-bearing.
What indicates a Grade 3 ankle sprain?
ATFL, CFL, PTFL Complete tear, significant edema and ecchymosis, definite instability, and difficulties with weight-bearing.
How does the medial ankle (deltoid ligament) sprain compare to lateral sprains?
It is much less common due to stronger ligamentous structures and differences in bony stability.
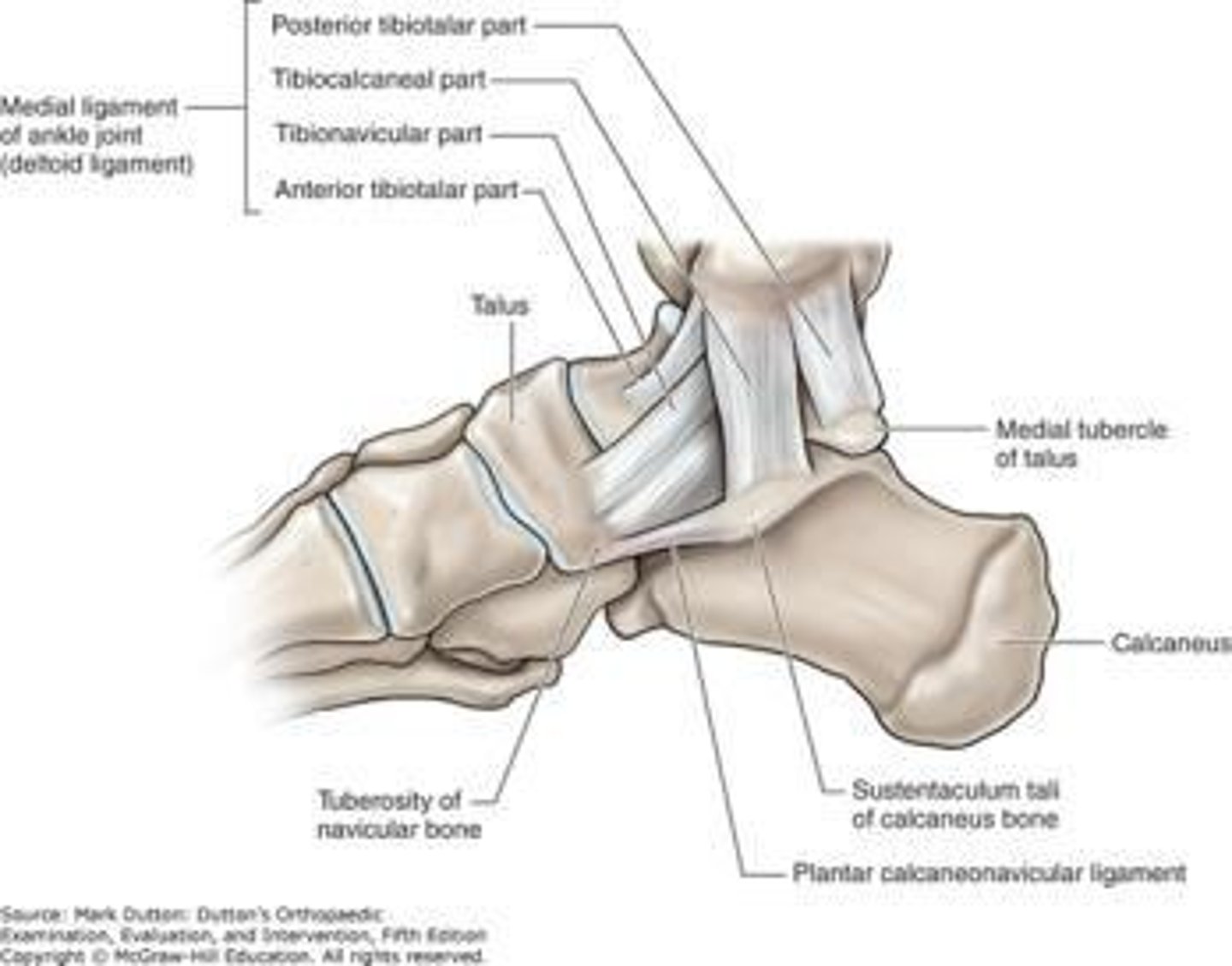
What condition can cause a lateral chip and is very hard to sprain?
Deltoid ligament injury.
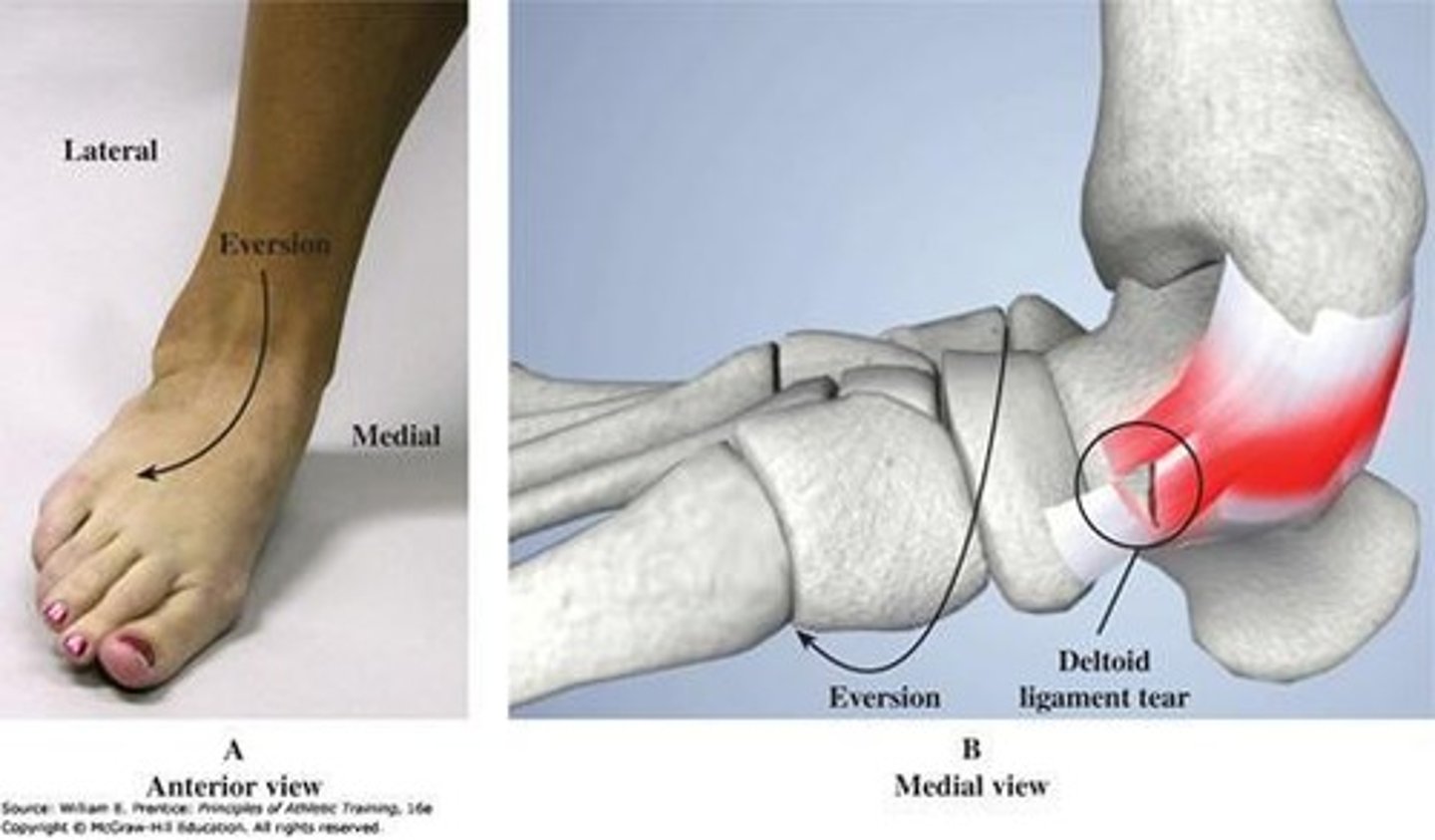
What are the difficulties associated with a deltoid ligament injury?
It can be very difficult to perform Activities of Daily Living (ADLs).
What usually contributes to a deltoid ligament injury?
Usually involves some weight over pressure that forces the incident.
What is Shin Myositis Ossificans?
A condition in the anterior shin where repeated trauma leads to bony formation in the anterior tibial muscle and sometimes the fibular muscle group.
What causes Shin Myositis Ossificans?
Repeated trauma over time with repeated blood in the muscle, leading the body to build a stronger structure.
What is the primary treatment approach for Shin Myositis Ossificans?
Supportive treatment by removing sources of trauma, addressing surrounding edema and inflammation, and ensuring muscle mobility.
What is a potential surgical option for severe cases of Shin Myositis Ossificans?
Surgical removal of the bony formation.
What is Tarsal Tunnel Syndrome?
A condition where neurovascular structures are compressed as they pass through a narrow space, leading to symptoms like numbness and pain.
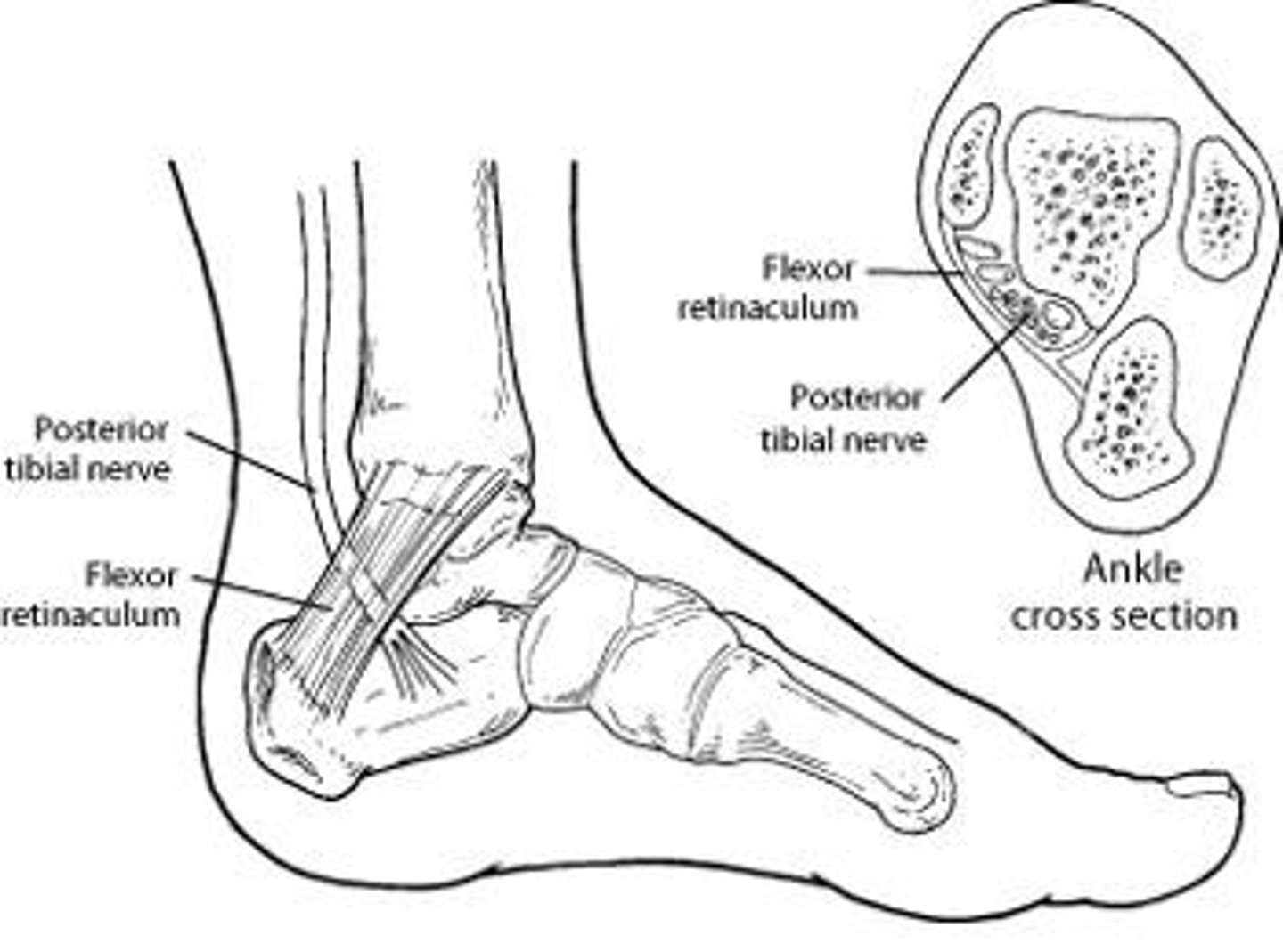
What predisposes individuals to Tarsal Tunnel Syndrome?
Conditions such as Pes Planus (flat feet) and excessive pronation that apply excess tension to medial structures.
Where is the tarsal tunnel located?
Posterior to the medial malleolus and under the flexor retinaculum.
What symptoms are commonly associated with Tarsal Tunnel Syndrome?
Numbness, sensitivity, and burning neurogenic type pain.
What happens to the nerve involvement in Tarsal Tunnel Syndrome?
There is usually an area of irritation leading to symptoms.
What can excessive movement like pronation lead to in the context of Tarsal Tunnel Syndrome?
It can lead to irritation of the neurovascular structures in the tarsal tunnel.
What is the primary focus when treating local inflammation and edema in sports injuries?
Reducing inflammation and edema through both contractile and non-contractile elements.
What condition is commonly associated with muscular imbalance and can lead to shin splints?
Medial Tibial Stress Syndrome (MTSS) is often a result of muscular imbalance.
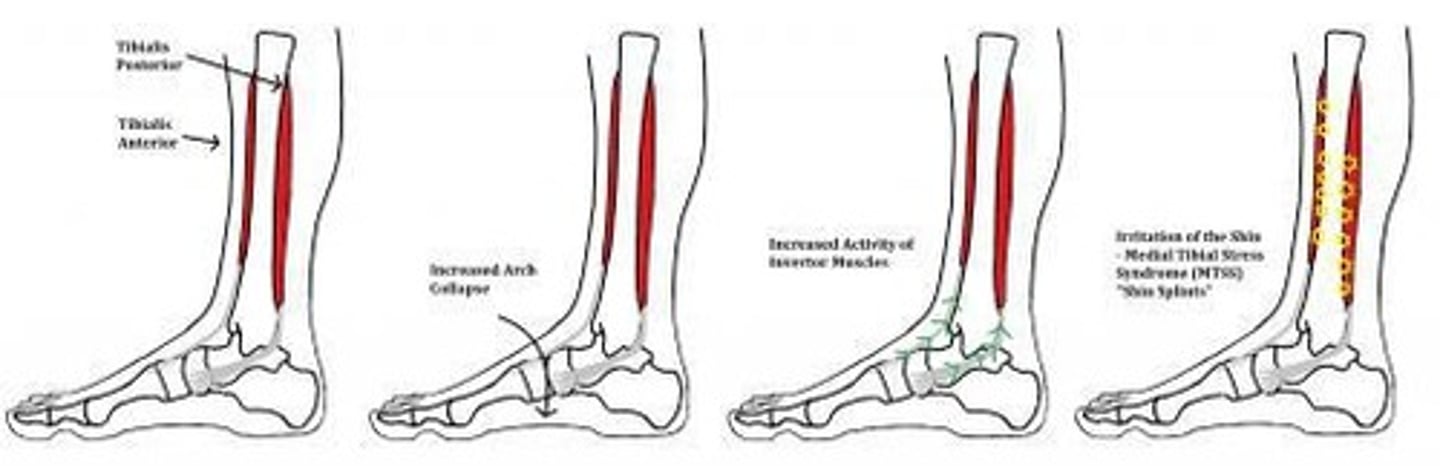
What anatomical condition can predispose individuals to shin splints?
Pes Planus (flat feet) and/or overuse.
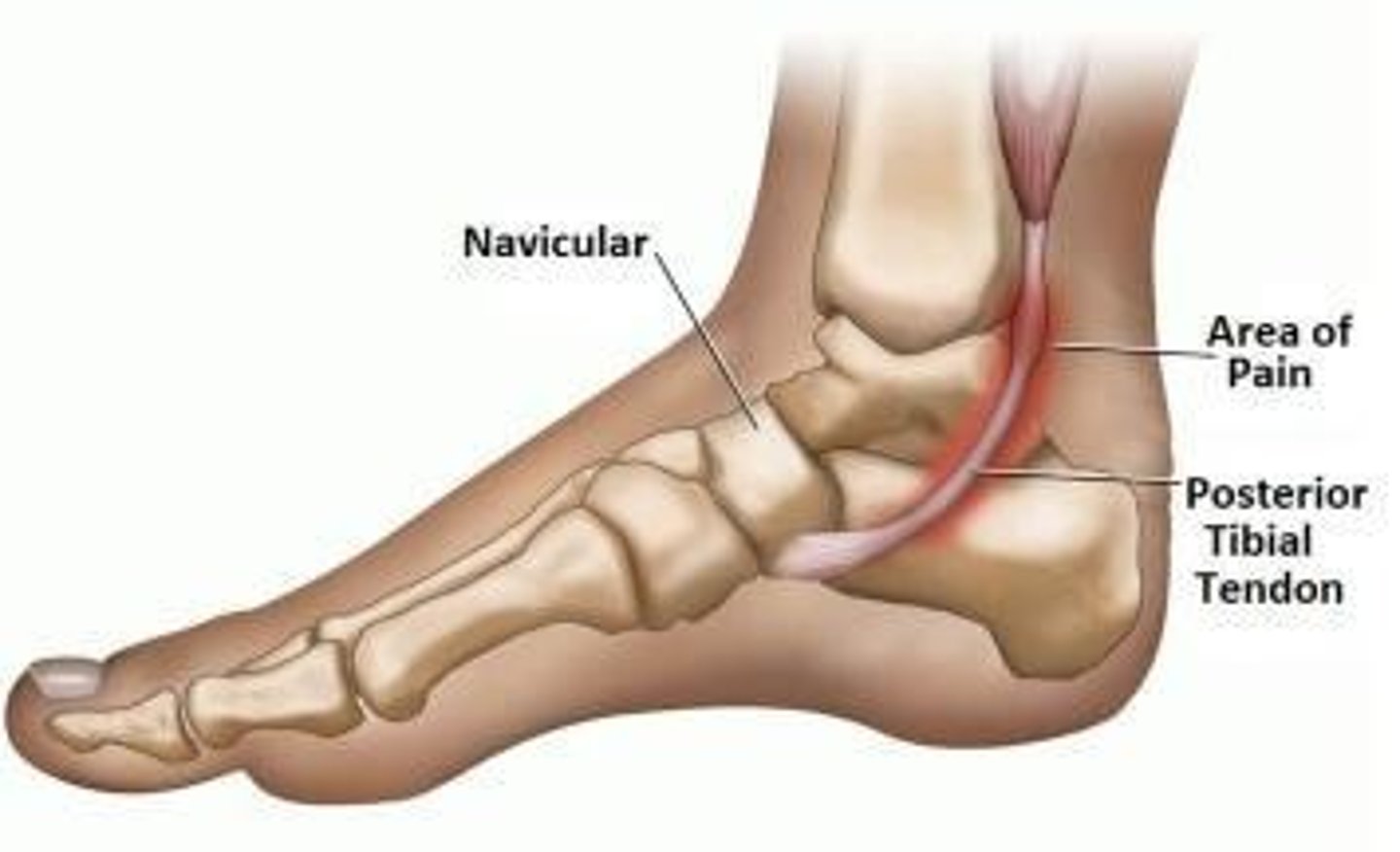
What are the similarities between Shin Splints (MTSS) and Posterior Tibial Tendinitis?
Both conditions tend to have similar causes related to muscular imbalance and foot structure.
What is a common treatment consideration for MTSS related to foot structure?
Good orthotic footwear can help manage the condition.
How does medial collapse of the arch affect muscle function in MTSS?
It requires increased activity to stabilize the arch, which can lead to discomfort in the muscle bellies.
What is a challenge in treating MTSS related to joint movement?
It is difficult to achieve enough eversion to stretch the joint effectively.
What is the recommended focus for treating MTSS?
Targeting the muscle and tendon directly rather than relying solely on joint movement.
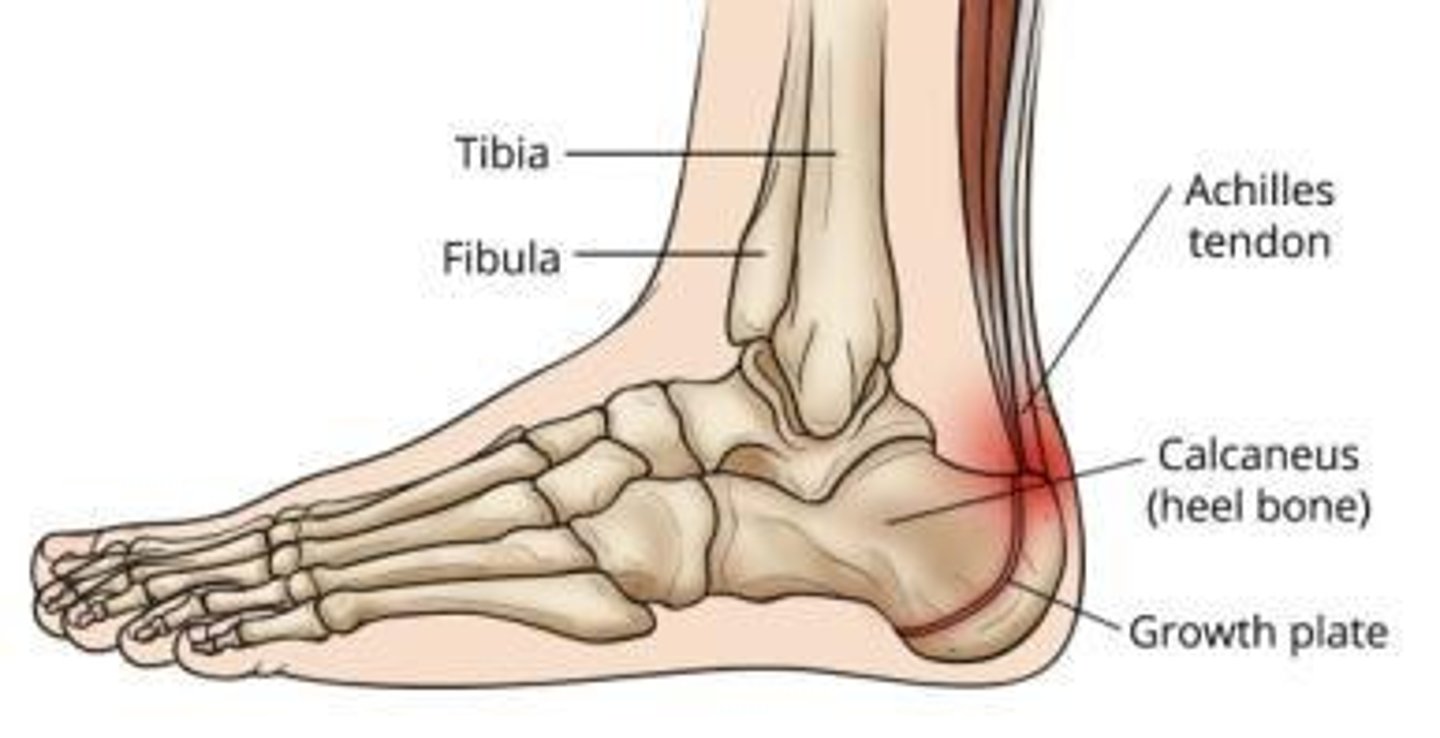
What is the primary cause of Achilles Tendinitis?
Overuse and imbalance of applied forces.
What can Achilles Tendinitis transition to over time?
It may transition to tendinopathy, leading to chronic edema and thickening due to scar tissue formation.
Where is mid-portion Achilles Tendinitis typically located?
Usually 2-6 cm proximal to the insertion of the tendon.
What is insertional Achilles Tendinitis associated with?
It occurs at the calcaneal attachment and can be related to Haglund's deformity (pump bump) from shoe pressure.
What can develop as a result of repeated pressure in insertional Achilles Tendinitis?
There can be the prevalence of bursa information and the formation of a bone spur.
What is a common symptom of MTSS?
Pain along the medial aspect of the lower leg.
What role does muscular imbalance play in shin splints?
Muscular imbalance can lead to uneven forces on the tibia, contributing to shin splints.
What is a key factor in the management of Achilles Tendinitis?
Addressing overuse and correcting biomechanical imbalances.
What can chronic Achilles Tendinitis lead to?
Maladaptive changes such as chronic edema and thickening of the tendon.
What is the relationship between shin splints and foot structure?
Foot structure, particularly pes planus, can influence the development of shin splints.
Why is it difficult to treat MTSS effectively?
The joint cannot be moved enough into eversion to achieve adequate stretching.
What is the significance of the posterior tibialis tendon in MTSS?
It usually attaches to the navicular and is often involved in MTSS symptoms.
How can footwear impact conditions like Achilles Tendinitis?
Improper footwear can exacerbate conditions like Haglund's deformity, leading to insertional tendinitis.
What is the importance of addressing both contractile and non-contractile elements in treatment?
It helps in reducing inflammation and promoting recovery in sports injuries.
What can prolonged inflammation of the Achilles tendon lead to?
It can progress to tendonopathy, where the tendon is degraded due to continuous inflammation.
What is a common result of prolonged scar tissue formation in the Achilles tendon?
Thickening of the tendon, which stabilizes the structure but leads to maladaptive changes.
What factors often contribute to Achilles tendon issues?
Overuse or an imbalance of forces, such as imbalanced stretch from plantar flexors and dorsiflexors, or changes in footwear.
How are Achilles tendon issues classified based on location?
They can be classified as mid-portion (1 or 2 inches above the insertion site) or at the insertion of the calcaneus, with the latter being less common and harder to treat.
What is the most common cause of an Achilles rupture?
Rapid eccentric loading, particularly peaking in men aged 40-45, but can occur in all age ranges.
What is a notable trend in Achilles rupture cases?
There are more cases now being treated post-operatively.
What is a risk associated with prolonged Achilles tendon apathy?
The scar tissue can become weaker over time.
What increases the likelihood of an Achilles tendon rupture?
Heavy loads and rapid eccentric movements.
What age group is most affected by Achilles tendon issues?
Men in their early 40s.
How frequently do Achilles tendon ruptures occur due to gradual weakening?
They occur more frequently due to a small amount of weakening over time.
What percentage of Achilles tendon cases can be treated non-operatively?
10-20% of cases can be treated non-operatively.
What is the body's capability regarding tendon repair in the presence of scar tissue?
The body can rebuild the gap in the tendon even with scar tissue present.
What movement precautions should be taken after an Achilles tendon injury?
Avoid pushing into dorsiflexion stretching or performing resisted loading of plantar flexion.
What is Sever's Disease?
A condition common during growth (ages 8-13) where strain from the Achilles causes apophysitis at the calcaneal growth plate.
What is the primary focus of treatment for conditions related to the Achilles growth plate?
Treatment usually focuses on support and symptom management followed by correction of force imbalances.
What can happen to the calcaneus growth plate during growth due to strain from the Achilles tendon?
The strain can cause inflammation, leading to excessive bone formation over time.
What are the recommended treatments for acute inflammation of the calcaneus growth plate?
Supportive measures, avoiding barefoot walking, running, jumping, symptom management, and edema management.
What should be addressed once the initial inflammation of the calcaneus settles down?
The root cause of the issue, such as muscle imbalance or tightness in the Achilles and calf muscles, and weakness of stabilizing muscles.
What is Complex Regional Pain Syndrome (CRPS)?
A condition characterized by multiple layers of complexity involving the nervous system and vascular considerations, typically beginning with trauma.
What are the hallmark characteristics of CRPS?
Hallmark characteristics include allodynia/hyperalgesia, trophic changes, and color/temperature changes.
What are some signs and symptoms of CRPS?
Signs include increased color, shininess of the skin, changes in nails, loss of hair, muscle wasting leading to contractures, and differences in sweat and oil production.
What is a Lisfranc injury?
An injury to the midfoot supportive ligaments (Lisfranc complex) with or without associated fractures.

What is the common cause of a Lisfranc injury?
Typically results from loaded trauma in a plantarflexed position.
What is a hallmark sign of a Lisfranc injury?
Bruising on the sole of the foot due to gravity pooling blood in the area.
What radiographic finding indicates a Lisfranc injury?
Widening of the space between the 1st and 2nd metatarsals.
What is the potential treatment for a Lisfranc injury?
Surgical fixation may be required in some cases.
How does CRPS affect sensitivity to stimulation?
Individuals with CRPS are very hypersensitive to stimulation, making normal sensations feel painful.
What are trophic changes in the context of CRPS?
Changes in skin, hair, and nail characteristics associated with the condition.
What role does the neurovascular response play in CRPS?
The neurovascular response is ramped up over time instead of being reduced after initial trauma.
What is the significance of muscle wasting in CRPS?
It can lead to contractures, further limiting mobility and function.
What are the implications of differences in sweat and oil production in CRPS?
These differences can contribute to the characteristic changes in skin appearance and health.
What is the typical mechanism of injury for a Lisfranc injury?
Injury often occurs during activities that involve loaded trauma while the foot is in a plantarflexed position.
What is the importance of addressing muscle imbalances in Achilles-related conditions?
Correcting muscle imbalances helps prevent recurrence of issues once initial inflammation subsides.
What is the typical progression of symptoms in conditions affecting the calcaneus growth plate?
Symptoms can become acute and irritable, requiring careful management.
What is the long-term concern with untreated inflammation of the calcaneus growth plate?
It can lead to excessive bone formation and chronic issues.
What is the role of radiography in diagnosing Lisfranc injuries?
Radiography helps visualize the widening of spaces between metatarsals, indicating disruption.
How does the treatment approach differ between acute inflammation and chronic issues in the Achilles area?
Acute treatment focuses on symptom management and support, while chronic treatment addresses underlying causes like muscle imbalances.
What is the initial treatment for hairline or pediatric ankle fractures?
Immobilization for 4-8 weeks.

What is the common treatment for displaced ankle fractures in adults?
Open Reduction and Internal Fixation (ORIF).

What precautions should be followed after an ankle fracture?
Weight-bearing (WB) precautions followed by a walking boot.
What is the focus of treatment after an ankle fracture?
Mitigating secondary issues before returning to full weight-bearing (FWB) and gait retraining.
What type of fracture is characterized by injuries to the lateral, medial, and posterior aspects of the ankle?
Trimalleolar fracture.
What is a common treatment for small, non-displaced fractures in children?
A cast or boot.
What is the protocol for managing stress fractures?
Relative immobilization, reduced weight-bearing, and managing secondary issues like edema and muscle atrophy.
What is plantar fasciitis commonly associated with?
Inflammation of the plantar fascia, which supports the arch of the foot.
What factors contribute to plantar fasciitis?
Obesity, frequent standing, changes in activity or footwear, and atypical biomechanics of the lower leg.
What is turf toe?
A hyperextension strain of the great toe, either traumatic or repetitive.
What structures can be involved in turf toe?
Any or all of the plantar structures across the 1st metatarsophalangeal (MTP) joint.
What is Morton's neuroma?
A condition affecting the interdigital nerves of the foot, often leading to pain between the toes.
What is a bunion (Hallux Valgus)?
A gradual change in valgus angulation of the 1st MTP joint.
What complications can arise from bunions?
They may not be limiting initially but can eventually require treatment, including surgical realignment.
What condition is often problematic when coupled with Hallux Valgus?
Hallux Rigidus, which involves loss of MTP extension and alters gait.
What is the typical presentation of plantar heel pain?
It can be described as inflammation of the plantar fascia.
What is the significance of the term 'plantar fasciopathy'?
It reflects various naming conventions depending on the suspected mechanism of injury (MOI) or chronicity.
What is the main goal of treatment for ankle fractures?
To return the patient to their prior level of function (PLOF).
What is the role of a walking boot in ankle fracture recovery?
To provide support and protection while allowing for gradual weight-bearing.
What are common symptoms of plantar fasciitis?
Pain in the heel and bottom of the foot, especially with the first steps in the morning.
What is the relationship between obesity and plantar fasciitis?
Obesity is a common contributing factor to the development of plantar fasciitis.
What is the impact of footwear on plantar fasciitis?
Changes in footwear can contribute to the onset or exacerbation of plantar fasciitis.