41. Pulmonary embolism
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
What is a pulmonary embolism
Pulmonary embolism (PE) = blockage of an artery in the lungs by substance that has moved from elsewhere in the body through the bloodstream (embolus)
Thromboembolism = consequence of thrombus formation within a deep vein of the body
What is the origin of tthe thrombus
Lower extremity veins (most common!)
Pelvic veins
Abdominal veins
Upper extremity veins
Head + cervical veins
Right heart
Left heart (septal defect or patent foramen ovale)
What causes thrombus formation
Venous stasis
Hypercoagulability
Vascular wall injury
What are the inherited risk factors of PE
Antithrombin III deficiency
Protein C deficiency
Protein S deficiency
Factor V Leiden mutation
What are the acquired risk factors
Immobilization, trauma, chronic venous insufficiency, malignancy, surgery
Oral contraceptives, obesity, stroke, age (>40 y/o), HF, smoking, pregnancy
What is the vascular pathology of PE
partial or complete blockage of peripheral pulmonary blood flow
has dual blood supply- rare necrosis
What are the haemodynamics of a PE
Thrombus blocks vessel → causes mechanical obstruction of blood flow + blood clot releases vasoconstrictor material causing further decrease in perfusion
Makes it difficult to pump blood from the right heart to the lung → causes backflow → eventually get insufficient filling of the left heart → circulatory collapse which can almost cause immediate death
What happens to the V/Q in normal regions of the lung
Hyperperfusion as the blood cannot go to where the embolism is
diverted to the normal parts of the lungs
↓V/Q ratio
functional shunt increases (more perfusion than ventilation)
hypoxemia (↓PaO2)
What happens to the V/Q in the affected region of the lung
Hypoperfusion → ↑V/Q ratio (↑alveolar dead space)
In normal conditions, V/Q = 0.8, meaning that Q is more than V
Decreasing Q will therefore increase the V/Q ratio
Hypocapnic bronchoconstriction (→ decreased ventilation = increase in CO2)
Atelectatic/necrosis due to reduced production of surfactant
What are the triad of symptoms
dyspnea
pleuritic chest pain
hemoptysis
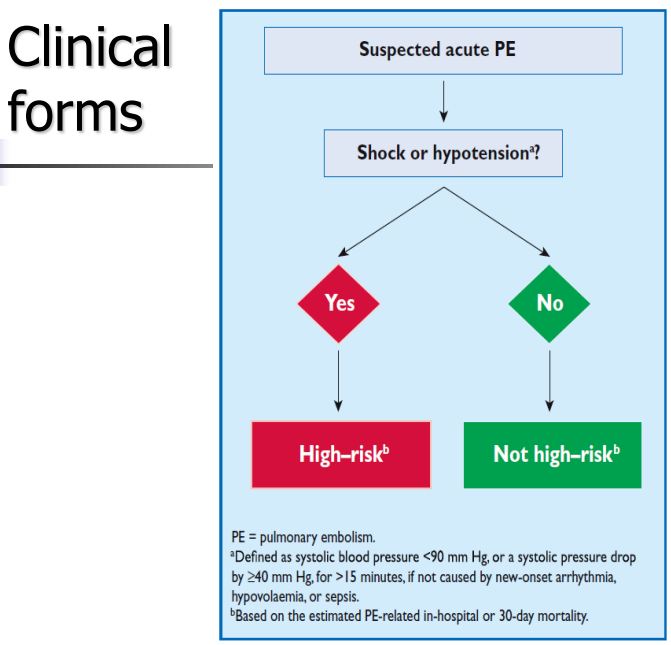
What are the clinical forms
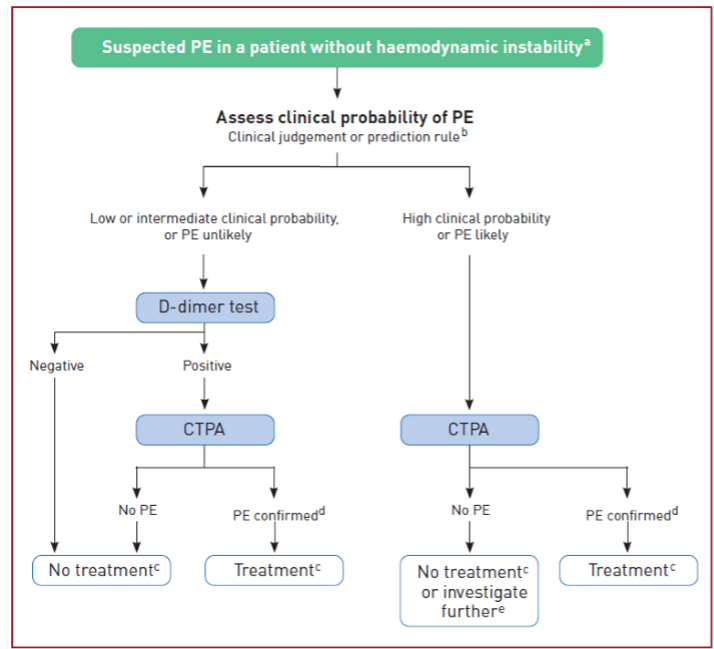
What is the diagnostic algorithm of PE
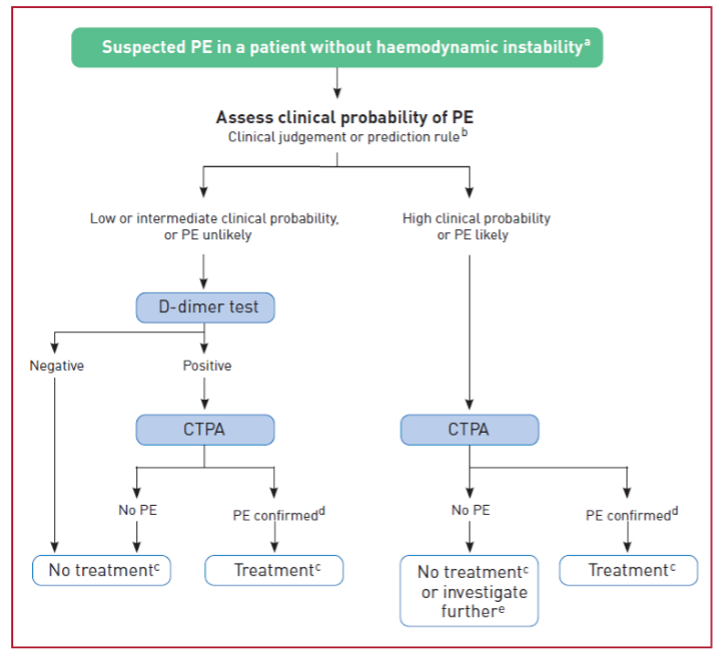
What is the diagnostics in patients with haemodynamic instability
What is seen on a CXR
non specific
can be normal
abnormal non specific findings
atelelectasis
enlarged pulmonary artery
pleural effusion
elevated hemidiaphragm
What can be seen on an ECG in PE
can be normal
Abnormal- non specific
ST depression
sinus tachycardia
negative T in V1-2
SVA
What are the lab fiindings in PE
D dimer increase
negative predictive value
excludes PE
In pulmonary infarct
increased WBC, FVC, CRP
increased troponin, LDH, serum HCO3-, SGOT
What can be seen on blood gas analysis
decreased PaO2
decreased PaCO2
due to hyperventilation
increased pH
respiratory alkalosis
What can be seen on a CT angiography
The first choice for imaging the pulmonary vasculature in patients suspected with PE
It allows adequate visualization of the pulmonary arteries down to at least the segmental level
Ventilation- perfusion scintigraphy
Labeled with technetium
Detects vessel occlusion > 3mm
Normal perfusion excludes pulmonary embolism
Specificity: tumor, pneumonia, hypoxic vasoconstriction
To be evaluated only with CXR
What are the indications of pulmonary antiography
Reference method – definitive diagnosis
Failure of other studies
Thrombolytic or anticoagulant therapy is contraindicated
What are the relative contraindications of pulmonary angiography
Contrast material hypersensitivity
Severe congestive HF, pulmonary hypertension