Smooth Muscle Physiology
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Describe the Smooth muscle contractile properties
Characteristics:
Slow cycling of myosin cross-bridges
↑ time of cross-bridge attachment.
Low energy requirement
Due to fewer cross bridge cycles, less ATP is split
Slow onset and relaxation of contraction
slow cross bridge cycling coupled with delayed
response to Ca2+ ions
Force of contraction could be higher then skeletal muscles
Stress relaxation
Allows hollow organs to expand and contract as needed
Muscle contracts or relaxes at an appropriate level to maintain pressure within the organ
ie. Filling and emptying of bladde
“latch” mechanism (a tonic contraction)
Large and sustained contraction with low energy expenditure
Describe the innervation of smooth muscles
Mechanism?
Smooth muscle innervation: unitary
Unitary: Aggregates (bundles or sheets) of hundreds or
thousands of fibers act as a single unit
Mechanism of unitary:
Membrane adherent to one another → force generated in one fiber can be transmitted to the next
Fibers are connected by gap junctions → ion flow from one fiber to another → electrical activity propagation throughout the entire tissue
Describe the difference in action potential between smooth/skeletal muscles
Difference in action potential:
Ca2+ plays a role in the generation of the AP
SM = more voltage-gated L-type Ca2+
Less participation of Na+ in action potential
Ca 2+ channels open slower and stay open longer
allowing some cells to have plateaus in their AP’s
Describe how Some smooth muscles contract without an AP
Contraction w/o AP:
Oscillations in Vm may be sufficient for tonic contraction even without an AP.
Hormones and neurotransmitters may cause contraction with no change in Vm via release of Ca2+ from SR
***MAIN POINT: ITS ALL ABOUT Ca2+ availability***
Describe the difference source of Ca2+ in SM vs skeletal muscles
Describe the difference in Calcium release from SR
Difference in Sources of Calcium in Smooth muscle
SM uses caveolae
SR = poorly developed; no T-tubes or terminal cisternae
Both extracellular and intracellular Ca2+ initiate contraction.
intracellular levels are the one regulated (ANS/hormones)
Difference Ca2+ release mechanism:
Skeletal Muscles: Voltage propogation → DHPR physically unlatching RyRs → Ca2+ release
SM; Ca2+ travels through L-type Ca2+ channel → Ca2+ BINDS to RyRs → Ca2+ release
Describe the mechanism of SM contraction:
Role of Caldesmon, tropomyosin, calponin
Role of Ca2+ to activate thick filaments
Termination of contraction
Ca2+ regulation of smooth muscle
cAMP
ROK
Role of Caldesmon, tropomyosin, calponin:
Caldesmon + tropomyosin → regulate the access of myosin to actin
Relaxed SM = caldesmon-tropomyosin complex blocks binding site on myosin
Calponin = smooth muscle-specific, actin-, tropomyosin- and calmodulin- binding protein involved in regulation or modulation of contraction.
Role of Ca2+ to activate thick filaments:
Four Ca2+ binds calmodulin (CM) → CaCM complex activates myosin light chain kinase (MLCK) → phosphorylates regulatory light chain (on myosin head) → increases ATPase activity of myosin
***OVERALL MESSAGE: Contraction requires the phosphorylation of the myosin regulatory chain***
Termination of contraction
Even w/ removal of Ca++, MLCK = inactive, but as long as the MLC is phosphorylated, contraction can continue.
Relaxation requires de-phosphorylation of the MLC by MLC phosphatase.
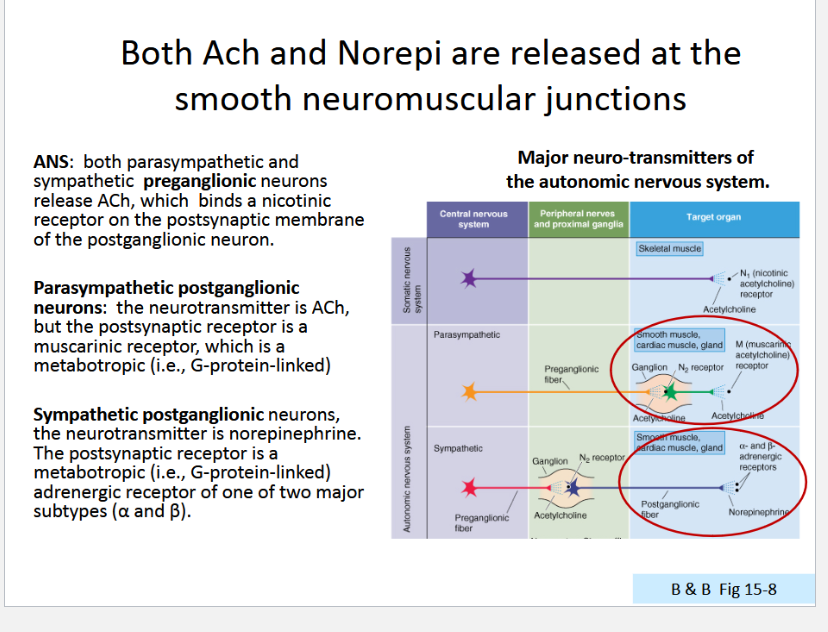
Ca2+ regulation of smooth muscle:
cyclic AMP-dependent(PKA)
NE acting on β receptors
Phosphorylates MLCK → inactivates it
reduces the sensitivity to Ca2+ and can
decrease force production and relax tonic
smooth muscle***Note that this does not affect Ca2+ levels***
Rho-associated protein kinase (ROK)
NE, 5-HT, histamine
phosphorylates MLCP → inactivates it
prolonging the effect of MLCK and contributing to tonic contraction
***Note, this does not alter [Ca2+ ]***
Describe the cross-bridge cycle of SM (similar to skeletal muscles so review)
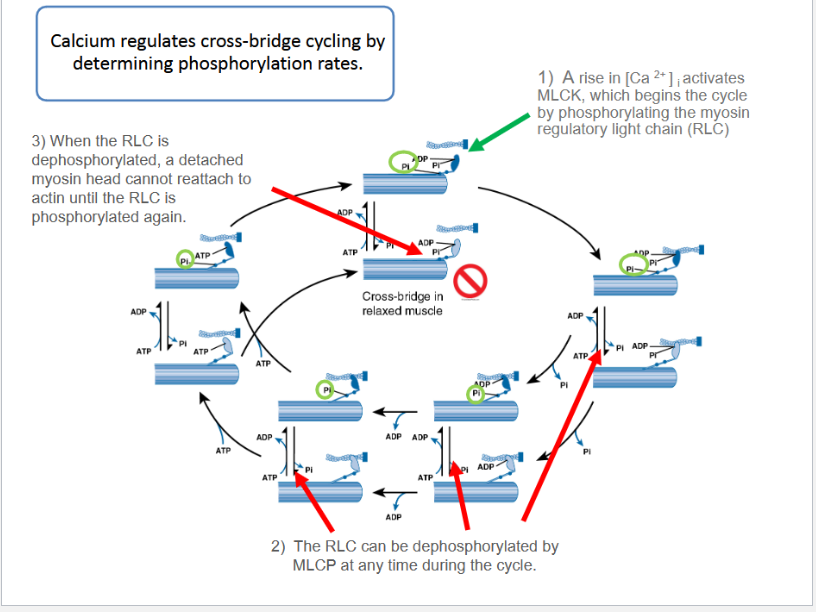
How does dephosphorylation affect myosin atpase?
De-phosphorylation slows activity of myosin ATPase
dephosphorylated myosin dissociates from actin very slowly, producing slow cross-bridge cycline
This maintains tension via tonic contraction

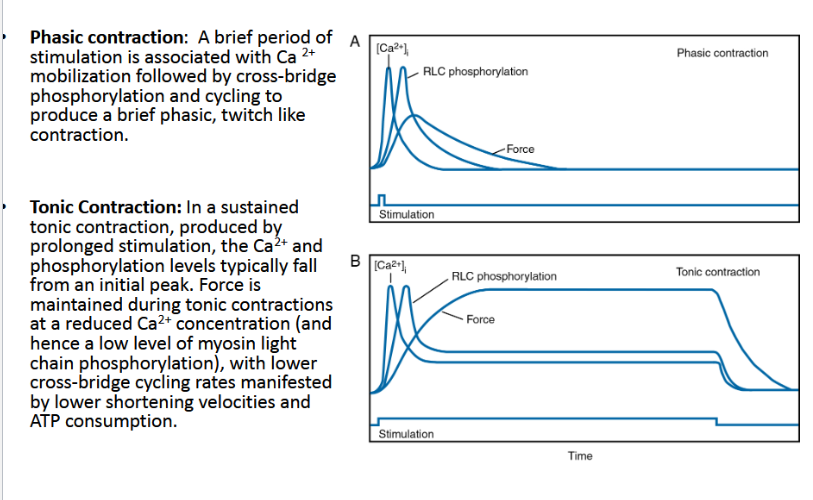
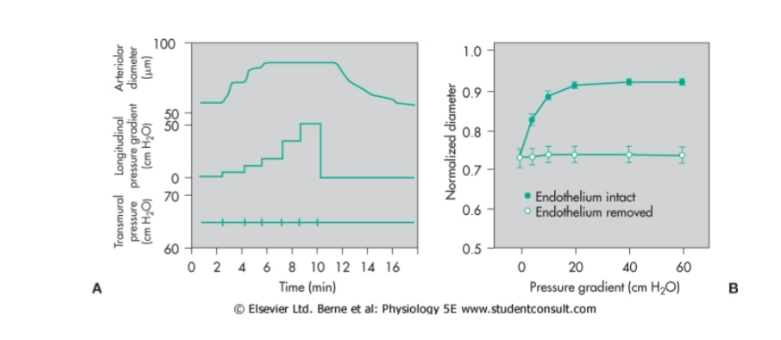
Describe these two images
Describe the Latch Mechanism
Dephosphorylation of the myosin light chain by MLCP
helps maintains tonic contraction with reduced cross bridge cycling and therefore extremely low energy expenditure
[REVIEW] NT release from para/sympathetic pre/post ganglioninc neurons
Describe how hormones can excite or inhibit Smooth Muscles
Excitation:
hormone binds ligand gated Na+ or Ca2+ channels → depolarize the membrane.
Inhibition:
ligand gated Na+ or Ca2+ channel is closed
the normally closed K+ channel is opened (Ca2+ activated K+channels).
In both cases → membrane potential → more negative→ more difficult to initiate contraction
Hormone may bind to membrane and indirectly inhibit via
cAMP and cGMP second messenger systems.Indirectly activates Ca2+ pump in cell membrane and SR
Net effect is decreased Ca2+ in sarcoplasm
Describe how stretch can excite SM
What does this allow
Excitation of unitary muscle due to stretch
Stretching → spontaneous action potentials via
Stretch-activated cation-permeable channels
Decrease in overall negativity of the membrane caused by the stretch itself
Allows:
gut wall to contract automatically and rhythmically when stretched excessively (ie peristaltic waves).
Describe the transport systems that participate in the regulation of [Ca 2+ ] i in smooth muscle cells:
What brings Ca2+ into the cell?
What extrudes Ca2+
What pumps Ca2+ into the SR?
How is Ca2+ released from SR
Ca2+ transport systems in SM:
Brings Ca2+ inside:
ROCs: receptor operated calcium channels
SOCs: stretch activated calcium channels
NCX: Sodium-calcium exchanger
L-Type Ca Channels
Extrudes Ca2+
PMCA: plasma membrane calcium ATPase
NCX:
Pumps Ca2+ into SR:
SERCA: sarcoplasmic reticulum calcium ATPase
Ca2+ released from SR:
IP 3 Rs: channels gated by IP 3
RyRs
In general, how is vasoconstriction/vasodilation mediated?
Vasoconstriction: Increase in Ca2+ concentration (intracellularly)
Vasodilation: Decrease in Ca2+ concentration or decrease phosphorylation of MLC
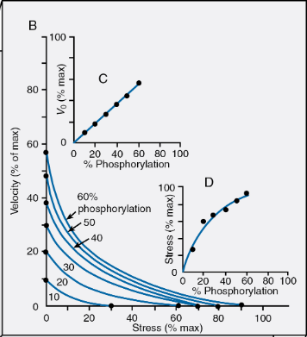
Describe the force-velocity relationship in smooth muscles
SM’s force-velocity relationship
Force-Velocity relationship is dependent on level of phosphorylation
still, Force is inverse of Velocity
Maximal shortening velocities are dependent on phosphorylation (proportional)
Force generation is dependent on Phosphorylation
What does flow-induced vasodilation require?
Flow induced vasodilation requires an intact epithelial lining
What do endothelial cells of vasculature synthesize and secrete?
Endothelial cells synthesize and secrete local factors (endothelium-derived vasoactive substances):
Local vasodilators: ↓vascular tone (under normal conditions)
Local vasoconstrictors: ↑ vascular tone
***Usually endothelium-derived vasoconstrictors are released under pathological conditions***
List out some endothelial factors that result in vasodilation/contraction
Vasodilators:
Nitric oxide (NO)
Prostacyclin (PGI2)
Endothelium-derived hyperpolarizing factor (EDHF)
Vasoconstrictions:
Endothelin (ET)
Endothelin derived constricting factor-1 and 2 (EDCF1, EDCF2)
describe the syntehsis of NO
What are its two forms?
NO synthesis:
produced from the L-arginine via nitric oxide synthase (NOS).
Two Forms:
constitutive NOS (cNOS; type III):
Ca++ -dependent
always produced
inducible NOS (iNOS; type II):
Ca++ independent
present during times of inflammation
induced by bacterial endotoxins and cytokines
Describe the mechanism in which NO leads to vasodilation
Mechanism:
NO → SM → activages cGMP → SM relaxation
Effects of cGMP:
inhibits calcium entry into cell, and decreases intracellular calcium concentrations
activates K+ channels, which leads to hyperpolarization and relaxation
stimulates cGMP-dependent protein kinase activating MCLP
Describe the vascular actions of NO
Vascular actions of NO:
Direct vasodilation (flow dependent and receptor mediated)
Indirect vasodilation by inhibiting vasoconstrictor influences (e.g., inhibits angiotensin II and sympathetic vasoconstriction)
Anti-thrombotic effect - inhibits platelet adhesion to the vascular endothelium
Anti-inflammatory effect - inhibits leukocyte adhesion to vascular endothelium; scavenges superoxide anion
Anti-proliferative effect - inhibits smooth muscle hyperplasia
What are some stimuli for NO release
Stimuli for NO release:
Acetylcholine,
bradykinin,
substance-P,
↑K+,
histamine,
adenosine,
↑H+(acidosis)
Differentiate between the effects of AcH and No
NO: vasodialtion
AcH: vasoconstriction
on normal endothelial: can make NO release
Describe the possible effects of NO impairment
impairment or reduction in the bioavailability of NO:
Vasoconstriction (e.g., coronary vasospasm, elevated
systemic vascular resistance, hypertension)Thrombosis due to platelet aggregation and adhesion
to vascular endotheliumInflammation due to up-regulation of leukocyte and
endothelial adhesion moleculesVascular hypertrophy and stenosis