Innate Immunity, Inflammation, and Wound Healing: Key Concepts for Nursing
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
Innate Immunity
Present at birth, before any exposures; non-specific and immediate.
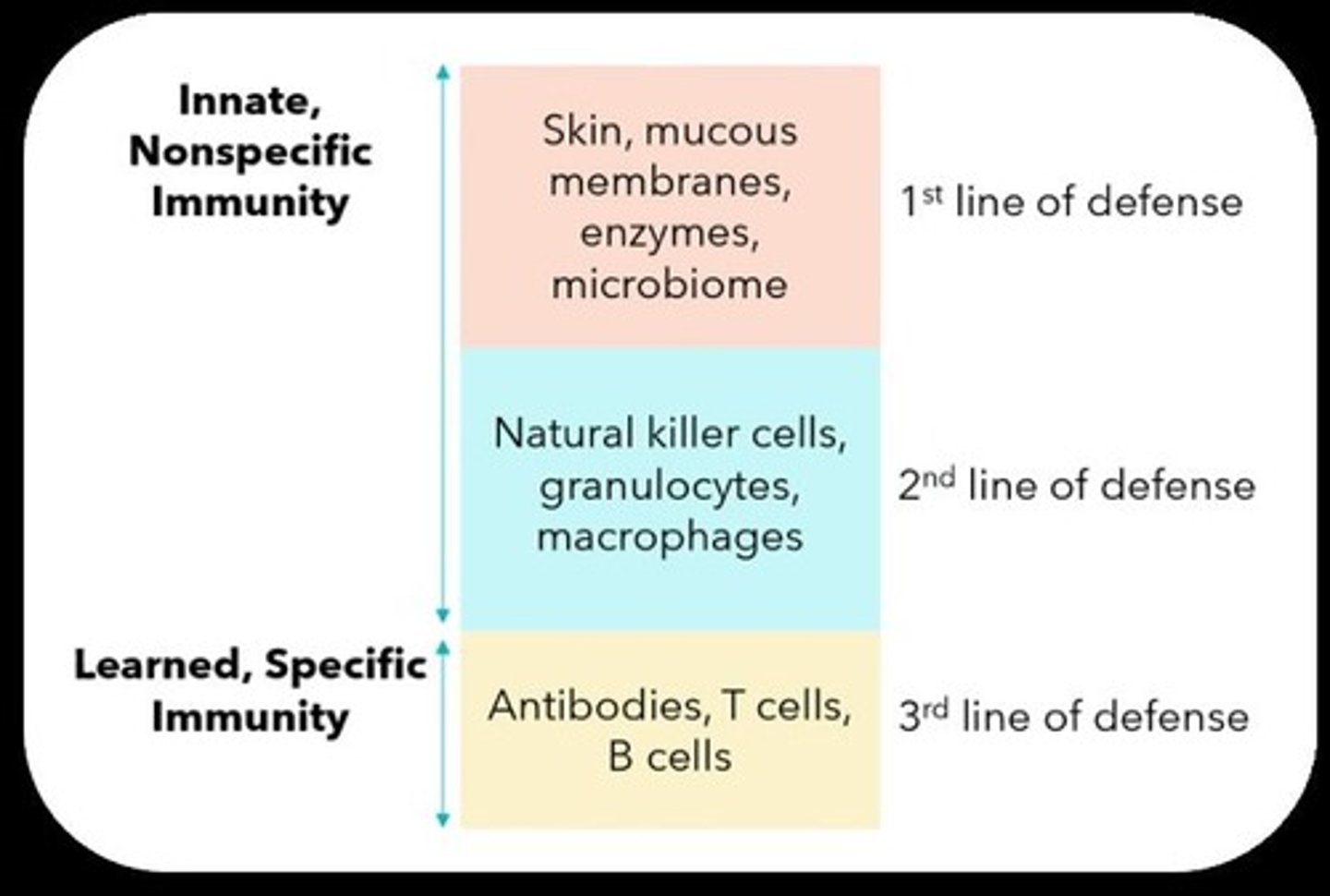
Nonspecific Immune Response
A type of immune response that does not target specific pathogens.
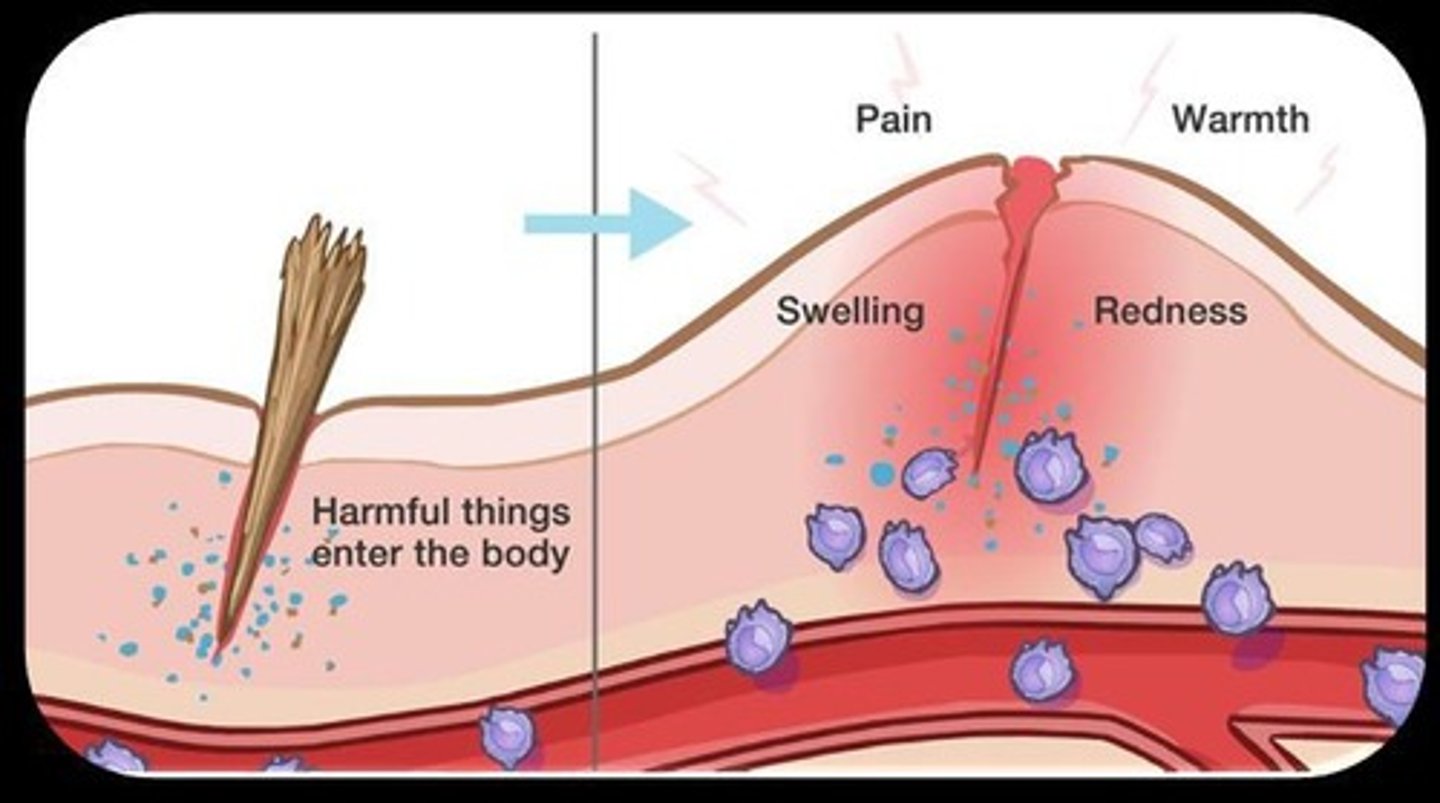
Inflammatory Response
A biological response to harmful stimuli, aimed at removing damaged cells and pathogens.
Adaptive/Acquired Immunity
A specific immune response developed after exposure to pathogens.
Physical Barriers
Structures such as skin and mucous membranes that prevent pathogen entry.
Biochemical Barriers
Substances like saliva, tears, and sweat that help to inhibit pathogen growth.
Normal Flora
Non-pathogenic microorganisms that reside in our body and compete with pathogens.
Vascular Response
The first stage of the inflammatory response characterized by increased blood flow and permeability.
Cardinal Signs of Inflammation
Heat, redness, swelling, pain, and loss of function.
Cellular Stage of Inflammatory Response
The second stage involving white blood cells and other cellular components.
Mast Cells
Cells that live in tissues and release histamine and other substances during inflammation.
Neutrophils
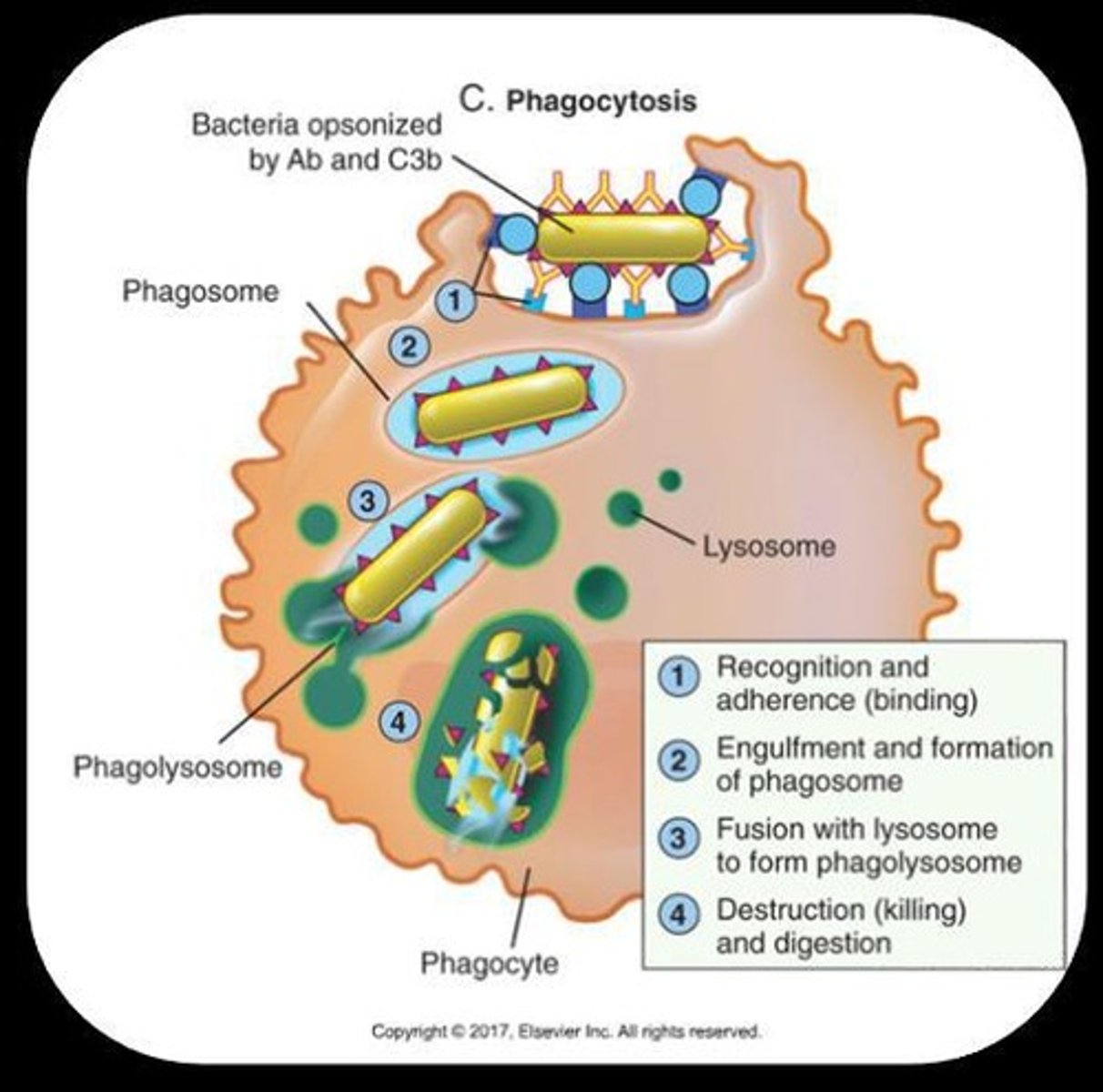
Phagocytes that engulf pathogens and are the primary white blood cells in early inflammation.
Macrophages
Large phagocytic cells that remove debris and pathogens.
Monocytes
A type of white blood cell that differentiates into macrophages and dendritic cells.
Platelets
Cell fragments that help stop bleeding and initiate scab formation.
Phagocytosis
The process by which cells engulf and digest foreign particles or pathogens.
Chemotaxis
The movement of cells towards the site of injury in response to chemical signals.
Lysosomes
Organelles that contain enzymes to break down cellular waste and pathogens.
Antimicrobial Peptides
Small proteins that can kill bacteria and fungi.
pH of Certain Areas
The acidity or alkalinity of body areas that can inhibit pathogen growth.
Cilia
Hair-like structures that help move mucus and trapped pathogens out of the respiratory tract.
Phagocytes
Programmed to destroy foreign cells.
Interferons
Chemicals that keep the inflammatory response local and eventually stop it.
Natural killer lymphocytes
Elimination of viral and cancer cells.
Mast cells and basophils
Degranulate to release chemotactic factors and to direct WBC to kill pathogens.
Lymph system
Bone marrow, spleen, lymph nodes- drain extra fluids and cellular waste out of the area.
Complement System
Leads to increased phagocytosis, mast cell release of histamine, and neutrophil migration.
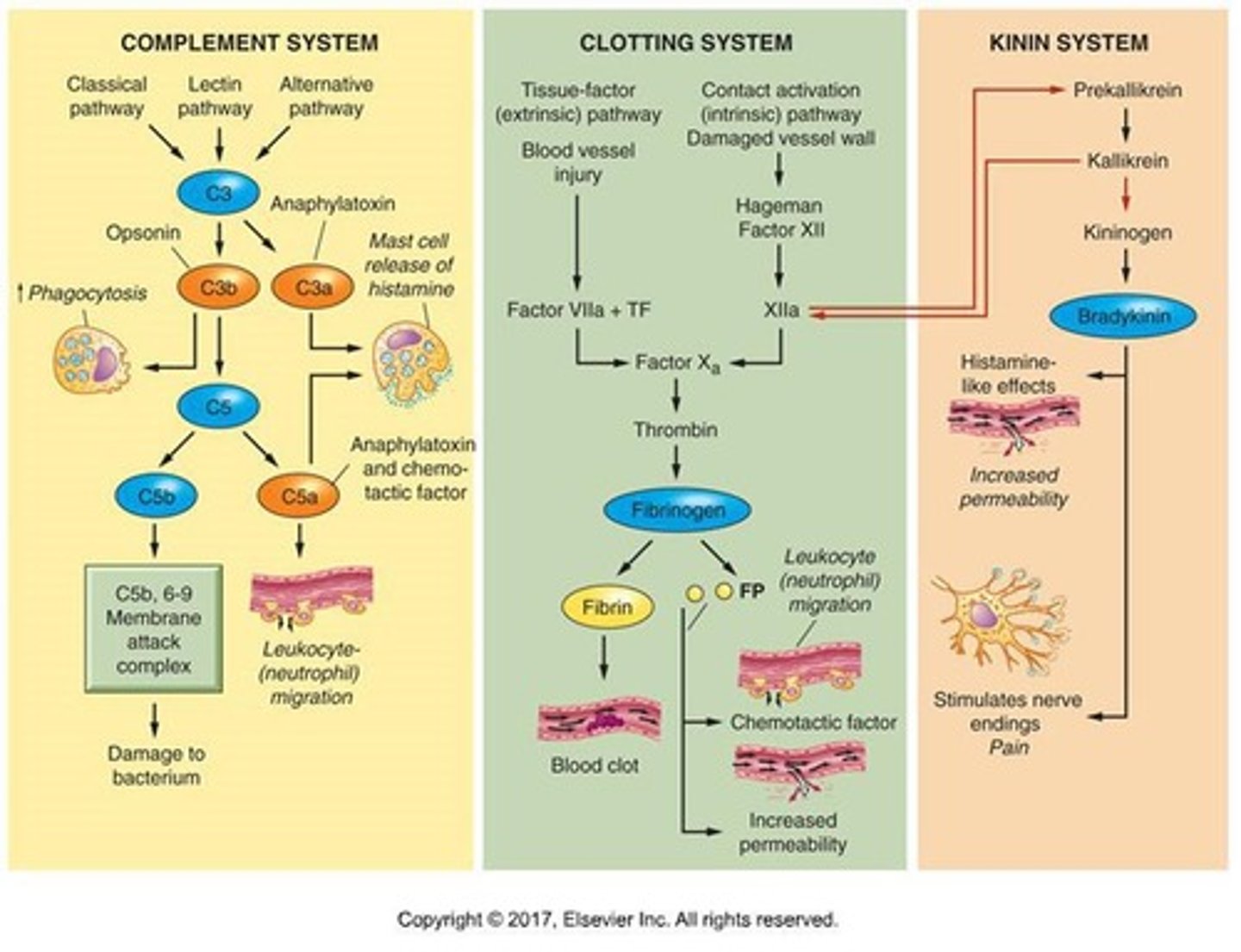
Clotting System
Leads to blood clot formation and attracting neutrophils to the area.
Kinin System
Primary substance bradykinin; leads to dilation of blood vessels and interacts with prostaglandins to create pain through stimulation of nerve endings.
Vasodilation
Clinical manifestation resulting in warmth.
Increased vascular permeability
Clinical manifestation resulting in swelling.
Increased RBC concentration
Clinical manifestation resulting in redness and warmth.
WBC migration
Clinical manifestation may see drainage or exudate.
Plasma Protein System activation
Clinical manifestation resulting in pain and loss of function.
Acute Inflammation
Self-limiting, short duration, starts immediately to 24 hours after injury.
Chronic Inflammation
Lasts two weeks or longer (years), usually happens due to unsuccessful acute response.
Causes of chronic inflammation
Ability of microorganism or other insult to survive in macrophage, irritation from toxins or physical contact.
Increased serum WBC count
Systemic response in inflammation.
Increased plasma protein synthesis
Systemic response in inflammation.
Fever
Systemic response where pyrogens tell the hypothalamus to increase temperature.
Detrimental effects of fever
If too high, causes denaturation of vital proteins, leading to disruption of biological processes.
White Blood Cell Count Differential
A test that includes CBC with differential and fibrinogen to assess inflammation.
Neutrophil
A type of white blood cell that may indicate bacterial infections or stress when elevated.
Erythrocyte Sedimentation Rate (ESR)
A non-specific indicator of inflammation.
Lymphocyte
A type of white blood cell that may indicate viral infections when elevated.
Monocyte
A type of white blood cell that may indicate fungal infections, malaria, or TB when elevated.
C-Reactive Protein (CRP)
A non-specific indicator of inflammation.
Eosinophil
A type of white blood cell that may indicate allergic reactions, parasitic infections, or autoimmune diseases when elevated.
Basophil
A type of white blood cell that may indicate cancers when elevated.
Bands (immature neutrophils)
Indicates an overwhelming infectious process.
Culture and Sensitivity
A test where a sample of the pathogen is taken and allowed to grow in the lab to identify it and test which antibiotics are most effective against it.
Inflammation Resolution
The ideal progression includes regeneration, debridement, and healing.
Wound Healing Phase 1
Inflammation phase where clotting and cleaning occur.
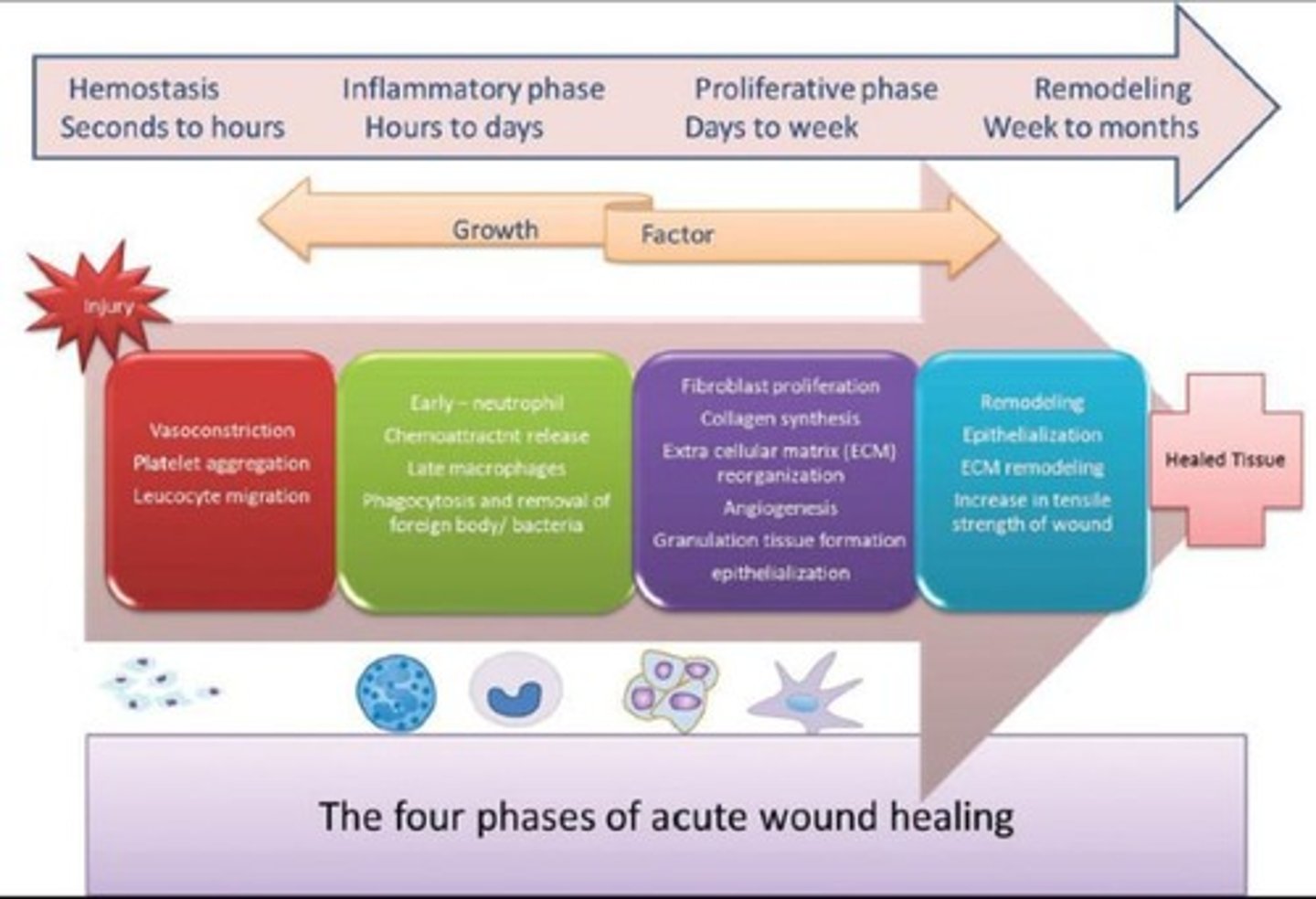
Wound Healing Phase 2
Proliferation and new tissue formation (granulation) phase.
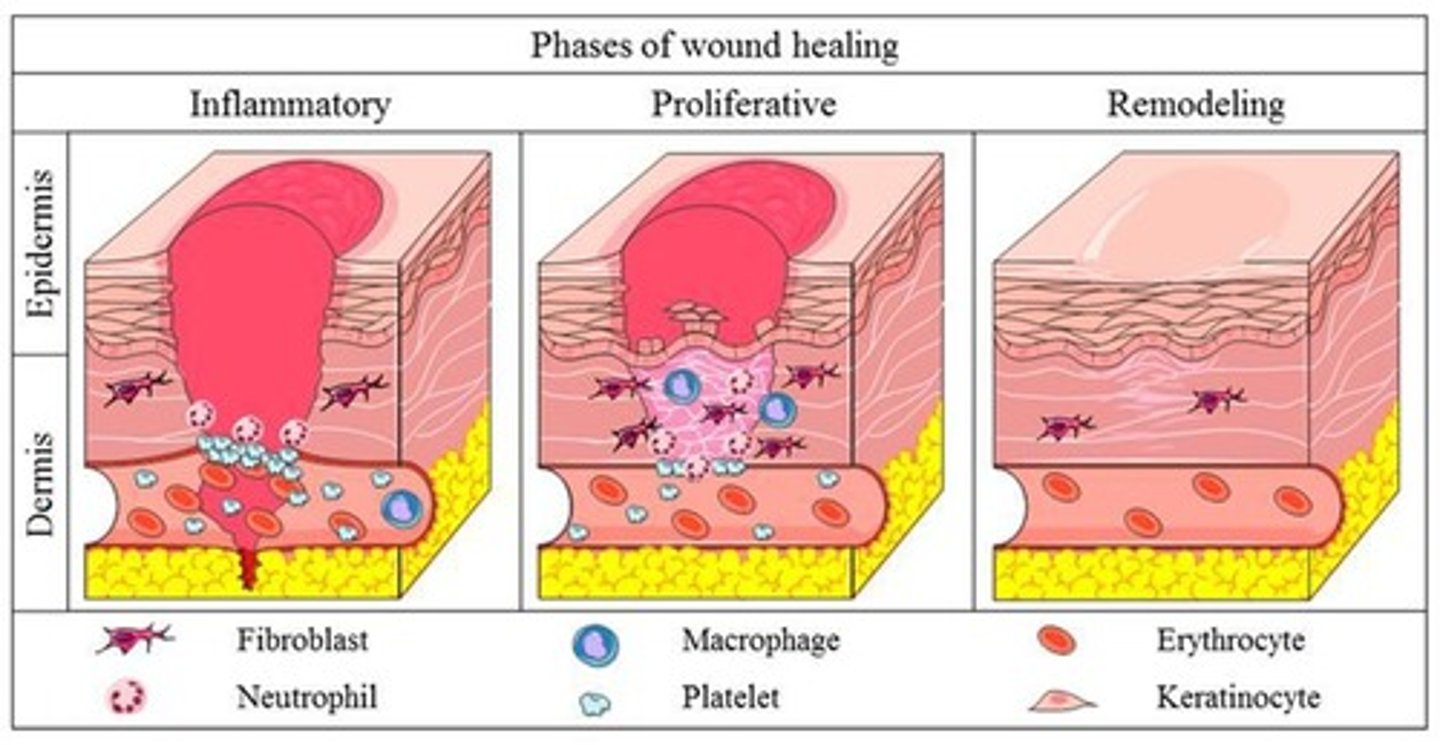
Wound Healing Phase 3
Remodeling and maturation phase.
Clotting and Cleaning
The initial response in the inflammatory phase of wound healing.
Fibrin
A component that stops bleeding and provides a framework for clot with platelets.
Neutrophils and macrophages
Cells that remove foreign materials and pathogens during the inflammatory phase.
Tissue Growth Factor
A biochemical mediator that promotes healing.
Angiogenesis Factor
A biochemical mediator that promotes new blood vessel growth.
Collagen Synthesis
The process of producing collagen, the most abundant protein in the body and a major component of skin, ligaments, tendons, and teeth.
Epithelialization and granulation
The process of new tissue growing in during wound healing.
Wound Dehiscence
A condition where a wound that was once closed has edges that are pulled open.
Dysfunctional Wound Healing
A condition characterized by impaired collagen matrix assembly, hypertrophic scars, keloids, and impaired epithelialization.
Hypertrophic Scar
A dark, raised scar that may regress over time.
Keloid
A larger scar that will not go away and may return if removed.