BPK 142 2nd part after first midterm
1/213
Earn XP
Description and Tags
I AM LITERALLY GOING TO SHOOT MYSELF NO KIZZY ON SIGMA FR FR FR FR FR FR FR FR FR I AM GOING CRAZY
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
214 Terms
Anthropometry
quantitative measurement of body size and proportions
Transport of oxygen
98 percent of oxygen is carried by hemoglobin
He+O2→ HbO2
Other 2 percent in plasma
One gram of hemoglobin saturated with O2 when combined with 1.34 ml of O2
Hemoglobin concentration equals 15.0 grams per 100ml of blood
O2 carrying capacity 15.0g x 1.34ml/g=20.1 ml of O2 per 100ml of blood
Percent saturation of O2 related the amount of O2 combined with hemoglobin to max O2 capacity of hemoglobin
Arterial blood at sea level
Hemoglobin is 97.5 percent saturated with O2
Venous blood at rest at sea level:
75 percent saturated with O2
Arteriovenous oxygen difference
Reps how much oxygen is extracted or consumed by the tissue for each 100ml of blood perfuming them
Oxyhemoglobin dissociation curve
hemoglobin act as tissue oxygen buffer system
Level or alveolar oxygen varies from 60 to more than 500 mm Hg but saturation is maintained
Due to flat shape of the curve
PO2 in tissue doesn’t vary more than a few mm Hg but saturation varies widely due to steep portion of curve
Bohr effect
increased body temperature
Increases PCO2
Decreased PH
Shift oxyhemoglobin curve right which releases more oxygen at tissue level for given PO2
PO2 levels at lungs and tissues
Total O2= dissolved O2 + HbO2
in tissues, PO2 is low
drives O2 exchange out of plasma
Low plasma PO2 drives O2 release form Hb
in lungs, PO2 is high
drives O2 exchange into plasma
Hugh plasma PO2 drives O2 binding to Hb
Stroke volume
Amount of blood pumped by either left or right ventricle per beat
Cardiac output
Amount of blood pumped by either the left or right ventricle of the heart per MINUTE
both left and right ventricles must have SAME cardiac output so that blood flow through pulmonary and systemic circuits is maintained equally
Cardiac output= heart rate x stroke volume
When cardiac output increase, more O2 transported to working muscles
Fick equation
When cardiac output increase, more O2 transported to working muscles
Expressed in VO2=HR x SV x (a-vO2) diff
VO2= oxygen uptake or utilization by tissues in body
(a-vO2) diff= arterial mixed venous oxygen difference- amount of O2 extracted at tissue capillary beds
To increase O2 uptake, increase cardiac output and or extract more O2 from arterial blood
Cardiac output rises with work rate
CARDIAC OUTPUT required for a given workload is reasonably similar for trained and untrained subjects
Heart rates increases linearly with work rate and O2 consumption
Max HR= 220 - Age (standard deviation is plus or minus 12 bpm)
For any given workload
trained subjects have a lower exercise heart rate
Trained subjects have higher stroke volume than untrained (cardiac output HR x SV)
Stroke volume
stroke volume= end diastolic volume minus end systolic volume
Diastole= resting phase of cardiac cycle between heart rates
Systole= contraction phase of cardiac cycle when ventricles pump out their stroke volume
End systolic volume; volume of blood remainsing in ventricle after ventricles have finished contracting
50 ml in an untrained person at rest
End diastolic volume: volume of blood in each ventricle at end of diastole ( after heart fills up)
120 ml in an untrained person at rest
Ejection fraction
percent of end diastole volume ejected with each contraction
Ejection fraction= stroke volume/ end diastolic volume
Ejection fraction increases with exercise
Mechanism of increase in stroke volume during exercise
greater systolic emptying= greater ejection fraction
Heart has functional residual volume
rest in upright, 50-60 percent of blood in ventricle is pumped out of ventricle during contraction- 50-80ml of blood remains in ventricle
During graded exercise, heart progressively increases stroke volume by means of a more complete emptying during systole due to sympathetic hormones
Distribution of blood flow during exercise (also talk about increase blood flow)
At rest 15-20 percent of systemic blood flow goes to skeletal muscles
During maximal exercise 85 percent of cardiac output can be diverted to working skeletal muscles
Increases blood flow is caused by
Increased blood pressure
Constriction of arterioles in gut area( liver, intestines, stomach, kidneys) and non working muscles due to sympathetic nervous system stimulation
Dilation of arterioles in working muscles due to relaxation of smooth muscle in walks of arterioles
release local factors as result of muscle contraction
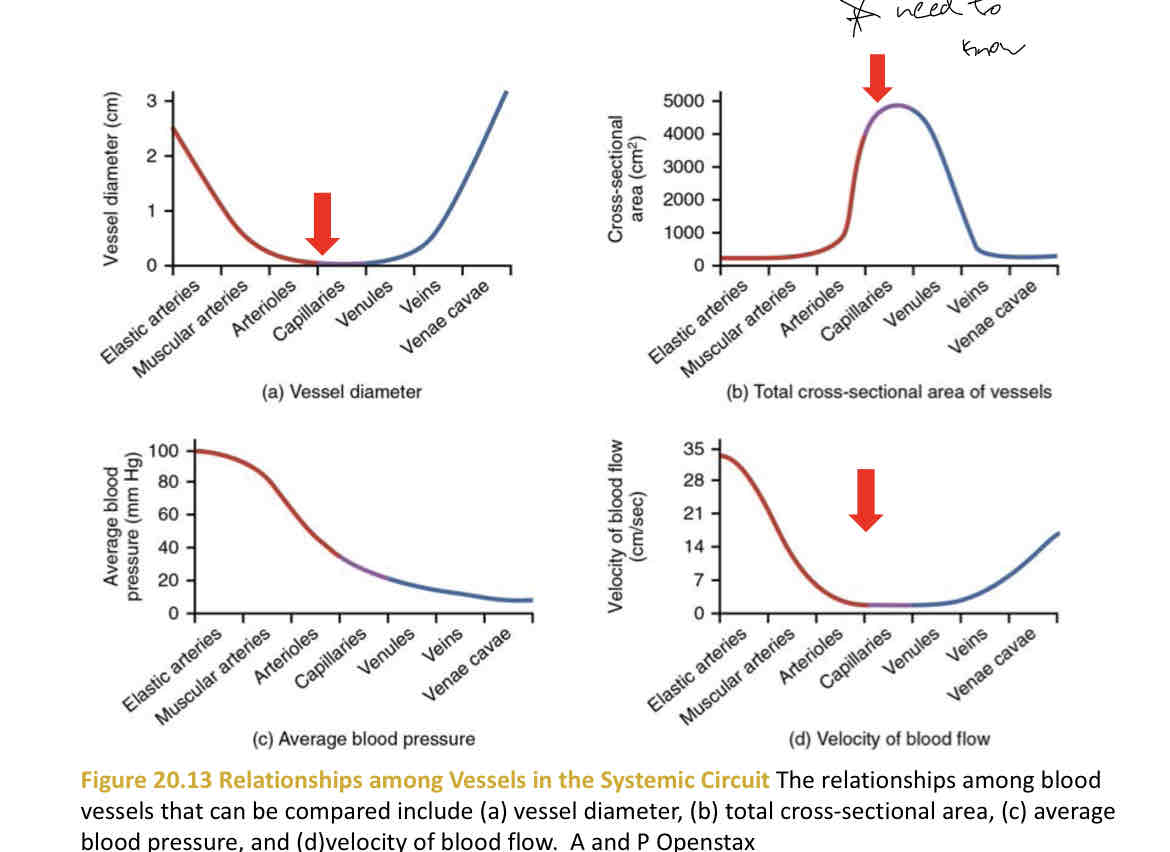
Poiseuille’s law
resistance to flow= (fluid viscosity x tube length )/ radius of tube
Decreasing tube radius by factor of 2 increases resistance flow by factor of 16, decreasing flow by factor of 16
33 percent decrease in radius of arterioles will produce 40p percent increase in resistance to flow
Small change in blood vessel radius will DRAMATICALLY ALTER BLOOD FLOW
Physiological determinants of VO2 max (WHAT DOES IT SAY ABOUT UR BODY)
VO2 max provides an integrated measurement of capacity of your physiological systems that contribute to O2 transport and utilization
Including cardiovascular
Respiratory
Neural
And muscular systems
While maintaining body homeostasis
Important factors that determine VO2 max
as duration of event requiring continuous energy expenditure becomes longer, aerobic metabolism will contribute higher percentage of ATP regeneration
Ability to ventilate lungs and oxygen the blood passing through lungs
Ability of heart to pump blood- cardiac output
Oxygen carrying capacity of blood
Ability of working muscles to accept large blood supply
Ability of muscle fibres that extract oxygen from capillary blood and she it produce energy- oxidative enzyme levels
VO2 max test protocols
Test protocol should exceed 6 minutes but be less than 15 minutes
Incorporate a warm up period- first stage of test
The test protocol should be arranged in stages, with each stage progressively increasing intensity until termination criteria is reached
Criteria of attainment of VO2 max
Oxygen consumption ceases to increase linearly with increasing work rate and approach plateau as at some point body switches from aerobic to anaerobic, last 2 values differ with plus 2 ml/kg/min
Heart rate should be close to age predicted max (220 - age). Test is protocol dependent
Blood lactate levels should be 8millimoles/litre or greater 3-5 minutes post exercise
indicates significant contribution from anaerobic metabolism
Respiratory exchange ratio (VCO2 divided by VO2) should be greater than 1.15
indicates anaerobic metabolism
Metabolic acidosis
Subjective observations- is subject exhausted at end
Mode of exercise
most subjects, highest VO2 max values obtained during uphill treadmill running-5-7 percent higher due to activation of larger muscle mass on treadmill
But competitive athletes able to achieve VO2 max values equal to or higher than their treadmill scores doing their sport
Due to muscle capillarization and aerobic enzyme levels are important determinants of VO2 max
Athletes should ideally be tested in mode of exercise used in their sport
Types of bicycle ergometers
Bicycle ergometers are of 2 types
Mechanical- monarch ergometers
Electrically braked bicycle ergometers- resistance is provided by moving a conductor through a magnetic field
Pros to ergometers to treadmill for exercise testing
Cheaper
Portable
Doesn’t require electricity
Patient more stable and body weight supported- easier to collect physiological data during exercise- heart rate, blood pressure, oxygen uptake, blood samples
Easier to quantify work rate
Cons to bicycle ergometers
Can’t obtain as Hugh VO2 max as on treadmill
Cycling not common mode of movement for individuals. Walking more common
Heredity
identical and fraternal twins, current evidence indicates that VO2 is 40-50% genetically determined
Improvements in aerobic capacity with training normally range between 6 and 20%
Age and sex
VO2 max (litres/min) increases with age
Peaks between 18 and 25 years old
VO2 max declines 1% per year
By 55, VO2 max on average 25-30% lower than 20 year olds
Before puberty, no significant difference in VO2 max between boys and girls
After puberty, average male has VO2 max that is 20-25 percent higher than average female
There are many females who have VO2 max scores higher than less fit males
reasons for sex difference
Differences in body composition- male has more muscle and less fat- muscle is metabolically a more active tissue
Average male has 10-14% higher hemoglobin concentration
Reasons for decrease in VO2 with age
Decrease in max heart rate, stroke volume and cardiac output in addition to negative changes in other components of oxygen uptake and transport systems
As person grow older, less physically active
active individual maintain higher VO2 max as they age compared to sedentary individuals
endurances trained 60 year olds can have higher VO2 max then sedentary 20 yr old
Why predictive tests for VO2
Cheaper and less specialized equipment required
Test can be submaximal-safety
Some test can be administered to large groups
Less motivation is required
Predictions based on heart rate during exercise
VO2 max predicted from submaximal HR within 10-20% of persona’s actual value for normal subjects
Type of subject for whom these tests are poor predictors are those in very high or low VO2 max categories
Error is 4-5%
procedures which use sub max exercise heart rate to predict VO2 max are based one:
linear relation heart rate and oxygen uptake
true over wide range of exercise intensities but in some at heavy work rate VO2 increases relatively more than heart rate
Similar max heart rate for all subjects- standard deviation is approx plus or minus 10 beats/min about the average max heart rate for ppl of same age group
max HR declines with age- must use age correction factor. Estimate HR with 220-Age
in cases where VO2 is predicted from work rate. A fixed mechanical efficiency is assumed
Mechanical efficiency may vary 6% on bike ergometer
Day to day variation in HR- even under highly standardized conditions (temperature, time of day, diet etc.) the variation in sub maximal HR is approx plus or 5 beats/min with day to day testing at same work rate
Efficiency of muscular work
efficiency of muscular work is percentage of chemical energy converted to mechanical energy, with remainder lost as heat
Computation of mechanical efficiency
%EFF= (work performed (kcal)/energy expended (kcal)) x 100
Efficiency of large muscle activities such as walking, running and cycling is usually 20-25 percent.
Parts of respiratory system
Nose, pharynx, larynx, trachea, bronchi(includes primary, secondary and tertiary), lungs, terminal and respiratory bronchioles, alveolar ducts, and alveoli
anatomy of the respiratory system
with branching, supportive cartilage is gradually replaced by smooth muscle
Contraction and relaxation of this smooth muscle constricts or dilates the bronchioles which majorly affects airway resistance
Conducting airways lead inspired air to alveoli
Volume of conducting airways= anatomic dead space around 150mL
Alveoli
thin small walled sacs that have capillary beds in their walls
Sites of gas molecule (O2 and CO2) exchange between air and blood
Millions of alveoli
Respiratory membrane
Very large surface area
70 square meters in the normal adult-size of one side of a tennis court
separates the air molecules in the alveoli from the blood in the capillaries
average thickness is 0.6 micrometers
Very thin- optimized for diffusion
Pulmonary ventilation
movement of air into and out of the lungs
Mechanics of breathing
pulmonary ventilation: movement of air into and out of lungs
Molecules move from high pressure to areas of low pressure
Boyle’s law: pressure of gas is inversely proportional to its volume ie: as one increase other decreases, pressure increase, volume decrease
P1V1=P2V2
Movement of air in and out of lungs results from pressure difference between pulmonary air and atmospheric air
Compliance: the amount of volume change in the lung for a given change in alveolar pressure
During exercise, mouth breathing tends to replace nasal breathing-less resistance to airflow
Air that enters either through nose or mouth is quickly saturated with vapour and warmed to body temperature, 37 degrees centigrade, even under conditions where very cold air is inspired
Tidal volume
volume of gas inspired or expired with each breath at rest or during any stated activity
500 mL per inspiration or expiration at rest
Look at slides week 8 slide 21
Stages of breathing
At rest: diaphragm is relaxed
Inspiration: thoracic volume increases
Expiration: diaphragm relaxes, thoracic volume decreases
Inspiration
diaphragm descends and external intercostal muscles contract which increases volume of thoracic cavity which decreases pressure in thoracic cavity
Pressure moves relative to gradient which is high to low pressure
Decreases pressure in thoracic cavity which is 1-2 mm Hg decrease in intraalveolar pressure at rest vs atmospheric pressure
pressure drop during hard exercise can produce -30 mm Hg below atmospheric pressure
Expiration(passive)
passive process at rest
Diaphragm and external intercostal muscles relax which decreases volume of thoracic cavity
Pressure in thoracic cavity increases above atmospheric pressure
Air molecules move out of the lung following pressure gradient
Expiration( active)
secondary muscles such as abdominal muscles and internal intercostals become involved in exercise
Forced expiration can produce intra-alveolar pressure as great as +50mm Hg above atmospheric pressure
Breathing frequency
-12-16 breaths per minute
Minute ventilation
Gas volume inspired or expired (not both) per minutes
tidal volume x breathing frequency
Max exercise
(Vt x Fr)
(3 L x 60breaths/min)
180 litres/min
Rest
(Vt x Fr)
Ex: .5L x 12-16 breaths/min
6-8 litres/min
Expiratory reserve volume
maximal volume that can be exhaled from resting end expiratory position
Approx 25% of vital capacity at rest
Inspiratory capacity
maximal volume of gas that can be inspired from resting end expiratory position
Approx 75% of vital capacity at rest
Vital capacity
greatest volume of gas that can be expelled by voluntary effort after maximal inspiration
Vital capacity is the sum of inspiratory capacity and the expiratory reserve volume
Residual volume
volume of gas remaining in the lungs after forced expiration
Functional residual capacity
volume of gas remaining in the lungs at the end of a quiet exhalation
Composed of expiratory reserve volume plus residual volume
Total lung capacity
total lung capacity= vital capacity plus residual volume
Forced vital capacity
subject is instructed to expire as hard and fast as possible for 4 seconds
Forced expiratory volume in one second (fev1.0)
volume of air expired during the first one second of forced vital capacity manoeuvre
Alveolar ventilation (Va)
volume of air that reaches alveoli per minute
Only air that participates in gas exchange with the blood
Anatomical dead space(Vd) is subtracted from tidal volume (Vt ) to obtain Va
Rest
Va= Fr x Vt-Vd
= 12x(500-150ml)
=4200 ml/min
Max exercise
Va= Fr x Vt-Vd
=60 x (3000 ml - 150 ml)
= 170000 ml/min = 170L/min
Lung volume (decrease)
most volumes and capacities decrease when a person lies down and increase when standing
Reasons:
Abdominal contents push up against diaphragm
There is an increase in intrapulmonary blood volume in horizontal position which decreases the space available for pulmonary air
Ventilation during incremental exercise
during exercise, minute ventilation increases linearly with increasing exercise intensity (oxygen consumption) until approx 50%-60% of VO2 max in untrained subjects
75%-80% of VO2 max in endurance athletes
Ventilatory threshold- point at which minute ventilation increases disproportionately with oxygen consumption during graded exercise
Ventilators threshold
point at which minute ventilation increases disproportionately with oxygen consumption during graded exercise
Respiratory disorders
Obstructive disorders- blockage or narrowing of airways caused by increased airway resistance
more difficult to move air in and out
Blockage due to inflammation and Edelman, smooth muscle contraction or bronchioles secretion
Asthma, bronchitis, emphysema
Restrictive disorders: damage to lung tissue
loss of elasticity and compliance limiting expansion of lung
Pulmonary fibrosis, pneumonia
Obstructive disorders
difficulty moving air rapidly in and out of lungs
FEV1.0
FEV1.0/VC much less than 80%
Decreased MBC (maximal breathing capacity)
Restrictive disorders
all lung volumes are reduced- VC, RV, FRC, TLC
Lung tissue is stiff and can’t be expanded very far
FEV1.p and MBC are reduced
But FEV1.0/VC ratio is frequently 90% or greater
function of circulatory system
Composed of heart, blood vessels and blood
transports essential materials throughout the body to cells
oxygen
White blood cells
Nutrients
Signaling molecules
Collects waste materials from body’s metabolic activity
Sections of circulatory system
Pulmonary circuit
blood vessels going to and from lungs
Systemic circuit
blood vessels going to and from the rest of the tissues of the body
Heart
a 4 chamber muscular pump which propels blood through the blood vessels
Atria- 2 upper chambers of heart
Ventricles- 2 lower chambers
Septum: divides left and right sides of the heart
Right ventricle pumps blood through pulmonary circuit
Left ventricle pumps blood through systemic circuit
Wall of LEFT VENTRICLE THICKER THAN WALL OF RIGHT VENTRICLE
Direction of blood flow through the heart is controlled by unidirectional valves
Heart murmur: valve is damaged or doesn’t close properly causes blood regurgitate which causes noise
Heart muscle (myocardium) is specialized type of muscle = cardiac muscle
Unlike skeletal muscle, all fibres or cells in cardiac muscle are anatomically interconnected which means when one finer contract, all contract
Fibers of atria are electrically separated from fibres of ventricles
Heart murmur
valve is damaged or doesn’t close properly which causes blood to be regurgitate causing noise
Cardiac muscle
also known as myocardium
All fibres are interconnected, so when one fibre contracts, all fibres contract
Fibres of atria are electrically separated from fibres of ventricles
Electrical conduction in myocardial cells
auto rhythmic cells spontaneously fire action potentials
Depolarization then spreads through gap junctions
Action potentials in contractile cells
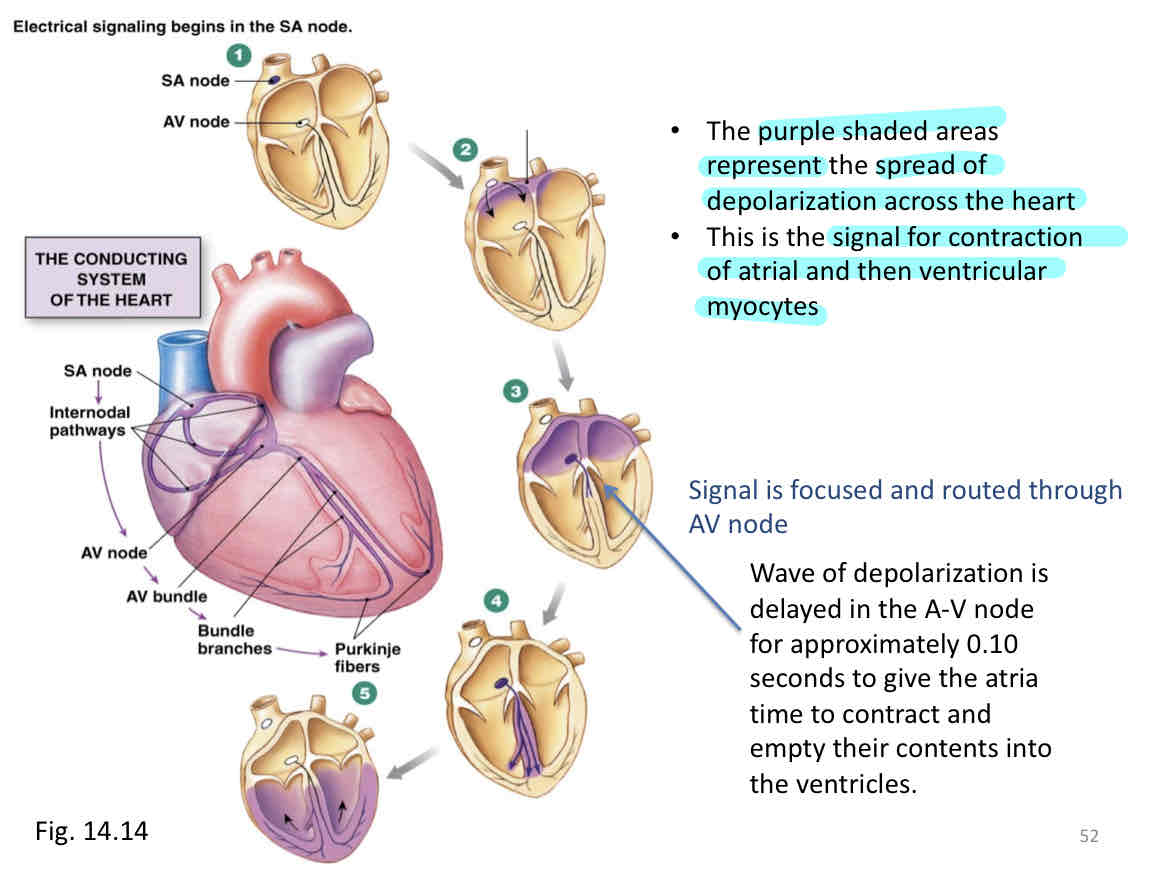
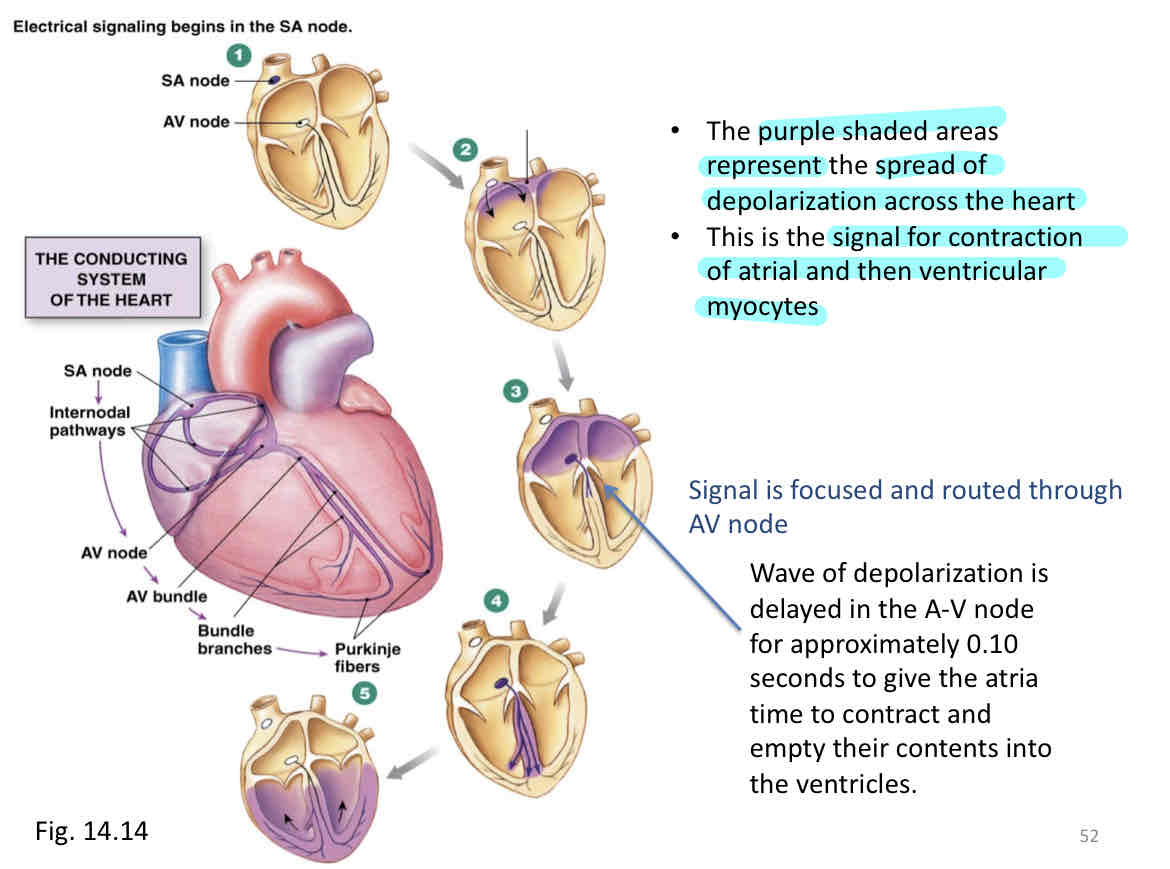
Conduction system of heart
heart inherent contractile rhythms originates in an area of specialized tissue located in the posterior wall of the right atrium
Sino atrial mode is S.A. node
process
Sino atrial node
Internode, pathways spread across both atria
Atrio ventricular (AV) node lies in the inter atrial septum
only pathway for electric, conduction across connective tissues between atria and ventricles
ventricular conduction system: AV node then AV bundle then left and right bundle branches then 2 bundles branch to many strands of purkinje fibers (spread through ventricles)
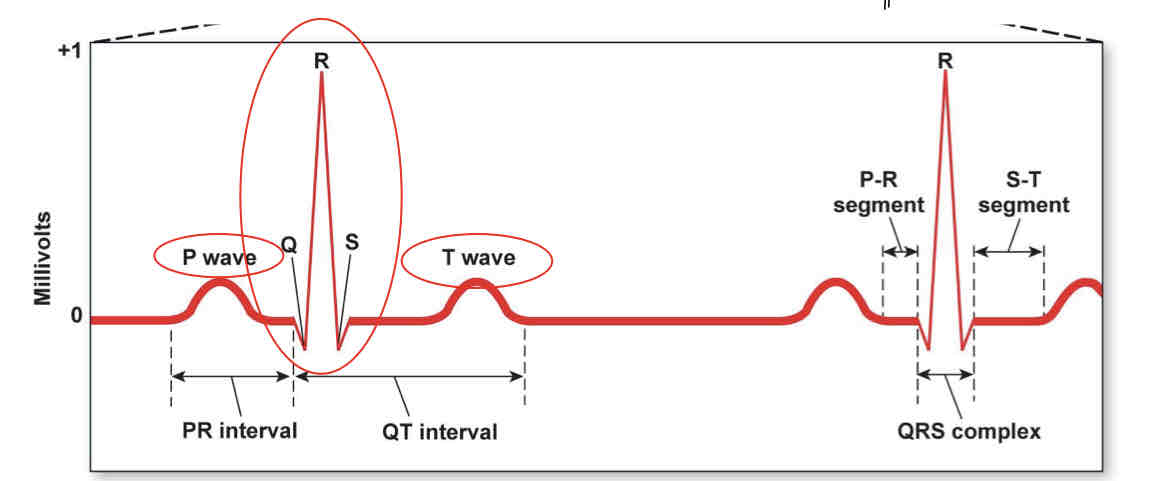
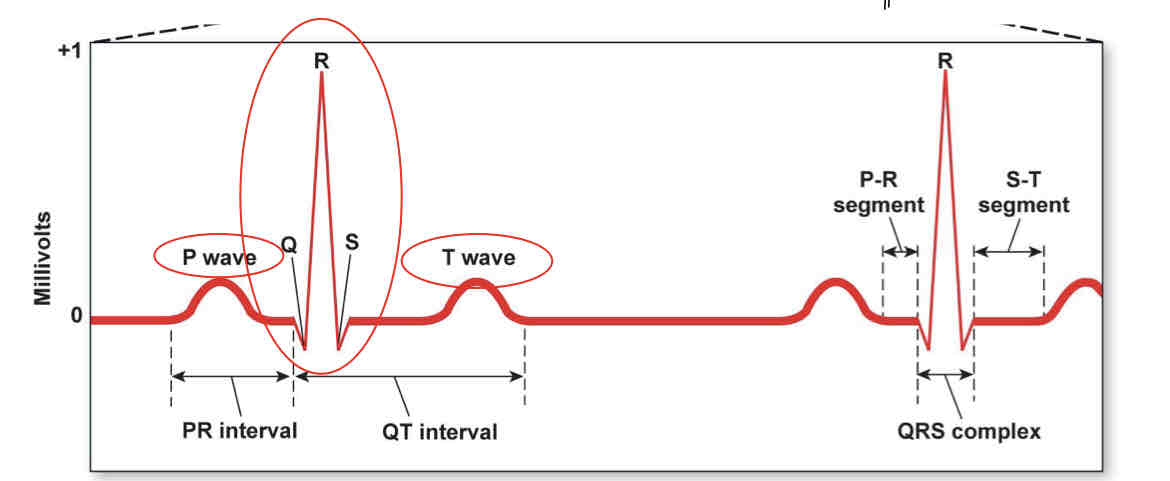
electrocardiography (ecg)
records the wave of depolarization as it passes across the heart using electrodes on the surface of the body
P wave= atrial depolarization
QRS= atrial repolarization and ventricular depolarization
T wave= repolarization of ventricles
PR interval= time between onset of atrial and ventricular depolarization
QT= duration of ventricular depol and repol
PR segment= conduction through AV node and bundle
ST segment= ventricular contraction
Arrhythmia
irregularity in rhythm of heartbeat
To diagnose looke at heart rate, amplitude and shapes of components of the ecg waveform and time intervals
Tachycardia- hr faster than norm
Over 100 bpm at rest
Bradycardia-hr slower than normal
Lower than 60 bpm at rest
Fibrillation- electrocardiography is disorganized
atrial fibrillation heart still functions as a pump
Upside down regular ecg ie QRS peaks are on the bottom
Ventricular fibrillation- heart does not function as effective pump
Messy ecg
Blood supply to the heart
heart muscle supplied by 2 major arteries which originated from aorta just above the aortic valve
Left coronary artery and right coronary artery
Large veins of the heart converge and empty into the right atrium
Cardiac muscle is highly dependent on aerobic metabolism, it requires a rich blood supply.
At rest, normal blood flow to the myocardium is 4% of total cardiac output
During exercise, blood flow to heart stays about the same 4% of cardiac output. Cardiac output increases substantially with exercise, increasing flow of blood to the heart
Approx 70-80% of oxygen is extracted from blood flowing in the coronary vessels compared to average 30% of other tissues
Blood vessel types
artery
Arterioles
Capillary
Venue
Vein
Artery
muscular and highly elastic
Receives and propel high pressure blood flow
Arterioles
muscular and well innervatee
Vary resistance to blood flow
Arteries under 0.5mm in diameter
Through constriction or relaxation of the thick layer of smooth muscle in walls of arterioles, blood flow can be increased or decreased to various capillaries
Arteries and arterioles constitute the High pressure part of circulatory system
Capillary
thin walled and highly permeable vessels
Exchange of materials such as nutrients/wastes and gases between blood and tissues
All other organs of circulatory system exist to serve capillary beds
Venule
thin walled and some fibrous tissue
Collect blood from capillaries
Small vessels that conduct venous blood from capillaries to veins
The venules and the veins constitute the low pressure part of the circulatory system.
Vein
fairly muscular and highly distensible
Easily collapse or expand to maintain venous return
Convey blood towards the heart
Greater in diameter but thinner walled than arteries with which they travel
Superficial and deep veins
Have smooth muscle in their walls which allow them to change their diameter.
Veins and venules constitute the low pressure of circulatory system
Pulse pressure
difference between systolic and diastolic pressure readings in arteries
Valves
found in those veins which carry blood against the force of gravity especially the veins of the legs
Mechanisms involved in return of blood to the heart
pressure difference between left and right atrium-120 mm Hg - 3mm Hg= 117mm Hg driving pressure
skeletal muscle pump: active muscles squeeze the veins and push blood towards the heart
Respiratory pump: decreased in thoracic cavity during inspiration which allows for easier blood return from lower portions of body via inferior vena cava to thoracic cavity then to right atrium of heart
Blood
composed of red blood cells, white blood cells and platelets
Suspended in a liquid plasma which makes up 50-60% of body volume
Blood volume of average adult with a normal body composition is approx 8% of body mass
Therefore, a person with a body mass of 70kg has a blood volume of approx 5.6 litres
Blood volume is greater for larger, more endurance trained and heat acclimatized people
Plasma
composed of 90% water and 10% solutes
Red blood cells(erythrocytes)
biconcave discs about 7 microns in diameter
Hematocrit: ratio of volume of blood cells to total volume of blood
Expressed as percentage
Usually 37-47% in females and 42-52% in males
Red blood cells are made in red bone marrow in ends of long bones and flat bones
Lifespan of RbC is 120 DAYS
Contains hemoglobin which transport O2 and Co2
Hemoglobin consists of 4 subunits, each contains one molecule of iron
Normal values for hemoglobin
male: 140-160 grams per 1000 ml blood
Female: 120-140 grams per 1000 ml blood
Blood doping
increasing RBC count and/or oxygen carrying capacity of blood
Types
blood transfusion
EPO (or synthetic hormones)
Synthetic oxygen carriers
alternative ways to increase RBC count
Hypoxia tents
Altitude training
polycthemia vera= too many rbcs which lead to increased blood viscosity and clotting
Diffusion
molecules go from high concentration to low concentration
Movement of molecules across respiratory membrane are driven by diffusion
Rate of diffusion can be increased by:
higher concentration gradient
Shorter diffusion distance
Higher temperature
Greater surface area
Sites of gas exchange
Alveolar capillary membrane in lung
net diffusion of O2 from alveoli to blood
Net diffusion of CO2 from blood to alveoli
Tissue capillary membrane in tissue
net diffusion of O2 from blood to tissue
Net diffusion of CO2 from tissue to blood
Partial pressure of gas in gas mixture
partial pressure of a gas- pressure of a gas in a gas mixture is dependent on
total (barometric) pressure
Fractional concentration of that gas
Example: at sea level, total pressure of all dry a,Brent atmospheric gas is 760mm Hg which equals to the barometric pressure
Most important factor in determining gas exchange is the partial pressure (concentration) gradients of gasses involved
Ambient air vs tracheal air vs alveolar air- partial pressure differences
Functional residual capacity (frc) serves as a damper so that each incoming breath of air has only a small effect on the composition of the alveolar air
Partial pressure of gasses in alveoli remains relatively stable
Henry’s law
amount of gas that dissolves in a fluid is a function of 2 factors:
Pressure of the gas above the fluid which is given by the gas concentration times the barometric pressure
Solubility coefficient of gas-CO2 is 20.3 times more soluble in water than O2
Lung diffusing capacity
diffusing capacity for oxygen is volume of oxygen that crosses the alveolar capillary membrane per minute per might between the alveolar air and pulmonary capillary blood
Aside partial pressure gradients, diffusing capacity can be affected by other factors
The thickness of respiratory membrane- length of the diffusion path
diffusing capacity is decreased in restrictive lung diseases such as pulmonary fibrosis or pneumonia
Number of red blood cells or their hemoglobin concentration or both
Surface area of respiratory membrane available for diffusion- diffusing capacity is decreased in emphysema
Diffusing capacity can increase up to 3 times during heavy aerobic exercise
Mechanisms:
Increased lung volumes during exercise which increased surface area for diffusion
Opening up of more capillaries in the lung and greater volume flowing through the lung
Transport of oxygen by blood
98% of oxygen in blood is carried by rbcs in chemical combination with hemoglobin
Hb+O2= HbO2 (oxyhemoglobin)
Other 2 percent in plasma
One gram of hemoglobin saturated with 1.34 ml of O2
In lungs PO2 is high
drives O2 exchange into plasma
High plasma PO2 drives O2 binding to Hb
In tissues, PO2 is low
drives O2 exchange out of plasma
Low plasma PO2 drives O2 release from Hb
Hemoglobin concentration equals 15.0 grams per 100ml of blood
O2 carrying capacity would be 15.0 × 1.34ml/g= 20.1 ml of O2 per 100 ml of blood
Percent saturation of hemoglobin with O2 relates the amount of O2 actually combined with hemoglobin to the maximum O2 capacity of hemoglobin
Arterial blood at rest at sea level
hemoglobin is 97.5% saturated with O2
97.5% × 20.1= 19.5 ml O2 per 100ml blood
Venous blood at rest at sea level
hemoglobin is 75% saturated with O2
75% x 20.1=15.1 ml O2 per 100ml blood
Arteriovenous oxygen difference- (a-v)O2
Represents how much oxygen is extracted or consumed by the tissues for each 100ml of blood perfusing them
At rest
(a-v)O2=19.5-15.1= 4.4 ml O2 per 100ml blood
Hemoglobin acts as tissue oxygen buffer system
Level of alveolar oxygen may vary greatly, from 60 to more than 500 mm Hg but saturation is maintained
Due to the flat shape of oxyhemoglobin dissociation curve
PO2 in tissue doesn’t vary more than a few mm Hg but saturation can vary widely due to steep portion of curve
Bohr effect
increased body temperature
Increased PCO2
Decreased pH
Shift oxyhemoglobin right which releases more oxygen at the tissue level for a given PO2
Divisions of nervous system
Central nervous system-brain and spinal chord
Peripheral nervous system-after ent and efferent divisions
Spinal chord
long cylinder of nerve tissue which extends down from brain stem to second lumbar
45cm long and 2cm in diameter
Protected by vertebral column and associated ligaments and muscles
Spinal meninges (consists of Dura mater(outer layer), arachnoid membrane (middle layer) and pia mater (inner layer))
The cerebrospinal fluid
Provide 2 way conduction pathway to and from brain and its major reflex Center
Paired spinal nerves arise from spinal chord
31 pairs of spinal nerves are attached to spinal chord
8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal
Enlarged in 2 regions
cervical enlargement which extends from C4 through T1 segments of spinal chord
Lumbosacral enlargement which extends from T11 through L1 segments of spinal cord
Plexus= network of converging and diverging nerve fibers or blood vessels.
Brain and spinal chord are composed of gray matter and white matter
Nerve cell bodies lie and constitute the gray matter
Interconnecting tracts of nerve fibers (axons) form white matter
Each spinal nerve has a dorsal root and a ventral root connected to spinal chord
Dorsal roots contain Afferent (sensory) fibers that carry info from periphery to spinal chord and brain
Central roots contain efferent (motor) fibers to skeletal muscle
Cell bodies of motor axons making up the ventral roots are located in ventral gray horns of spinal cord
Cell bodies of sensory axons making up dorsal roots are outside of spinal cord in dorsal root ganglia
Ganglion: collection of nerve cell bodies located outside of CNS
Spinal cord injury
often result of trauma to spinal cord but can also be associated with congenital or degenerative disease
Causes include
Motor vehicle accidents
Violence
Falls
Recreational activities
Transecting (complete cut) of spinal cord
results in loss of all sensation and voluntary movement inferior below point of damage
Quadriplegic- if cord transected superior to C5
If transaction above C4, patient may die of respiratory failure
Patient paraplegic
paralysis of both lower limbs- transaction occurs below cervical segment of spinal chord
Deficiency of blood supply to spinal chord caused by fractures, dislocations, atherosclerosis affect its function and can lead to muscle weakness and paralysis
When brain or spinal cord damages, most cases injured axons don’t recover
Muscle sense organs
proprioceptors
conduct sensory information to the CNS from muscles, tendons, ligaments and joint - kinesthetic sense
Kinesthetic sense: gives info about location of parts of our body in relation to environment
Types
muscle spindles- change in length
Golfi tendon organ- change in tension
Joint receptors- change in angle
Muscle spindles (ex: patellar tendon tap)
structure- several modified muscle fibers
Spindle fibers lie parallel to regular muscle fibers
Function: sends info to CNS regarding degree of muscle stretch- activation of exact number of motor units to overcome a given resistance
With increasing degrees of stretch of muscle spindle, frequency of impulse transmission up the Afferent neuron to spinal chord increases
3 methods of activating alpha motor neurons to contract muscles
Tonic stretch: concerned with final length of muscle
Physic stretch: spindle responded to velocity of change of length
Gamma system- gamma efferent fibers innervate contractile ends of intramural fibers
when alpha motor neurons activated, gamma motor neurons also activated (coactivation)
Gamma system provides mechanism for maintaining the spindle at peak operation at all muscle lengths
Help maintain muscle spindle sensitivity
Stretch reflex
muscle spindles distributed throughout muscle. Densities vary with degree of control required by muscle
Reflex Arc- reflex pathway
5 components
Receptors(muscle spindle)
Afferent neuron
Integrating Center(spinal cord)
Efferent neuron (both gamma and alpha)
Effector (muscle contraction)
Stretch reflex
muscle spindles distributed throughout muscle. Densities vary with degree of control required by muscle
Reflex Arc- reflex pathway
5 components
Receptors(muscle spindle)
Afferent neuron
Integrating Center(spinal cord)
Efferent neuron (both gamma and alpha)
Effector (muscle contraction)
Golgi tendon organs
Location- encapsulated in tendon fibers near junction of muscle and tendon fibers
In series with muscle fibers rather than in parallel as are muscle spindles
When muscle contracts, GTO is stretched
Functions- firing rate if GTO is very sensitive to changes in tension of muscle
Sensory input from GTO about tension produced by muscles is useful for variety of motor acts such as maintaining a steady grip on an object
When stimulated by excessive tension or stretch-send sensory information to CNS which cause the contracted muscle to relax( reflex inhibition)
protect muscle and it’s connective tissue harness from damage due to excessive loads
Joint receptors
supply information to CNS concerning joint angle, acceleration of joint, pressure and pain
Control of motor functions
cerebral cortex and cerebellum are main centres employed in learning new motor skills. These areas of brain initiate voluntary control of movement patterns
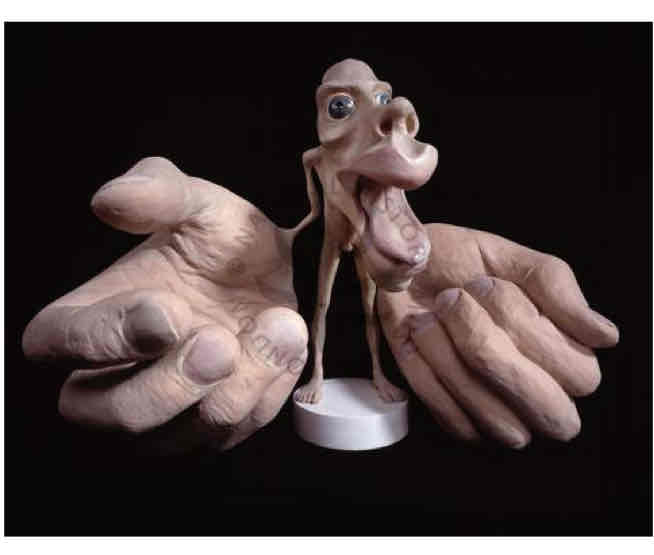
Primary motor cortex
located at the rear of the frontal lobe of the cerebral cortex.
Stimulation of different areas of the primary motor cortex brings about movement in different, specific areas of the body.
Contains the motor homunculus. However, no coordinated movement can be elicited.
The motor cortex on each side of the brain primarily controls muscles on the opposite side of the body.
The primary motor neurons cross over in the pyramids of the medulla
Cerebral cortex
motor homunculus
Parts of the body that are affected by cerebral cortex
Corticospinal tract
long axons which carry impulses from the primary motor corteX where their cell bodies are located directly to lower motorneurons in spinal cordàspinal nerves
The corticospinal system primarily mediates performance of fine, discrete, voluntary movements of the hands and fingers.
Premotor cortex
One of the three higher areas that command the primary motor cortex.
Located on the lateral surface of each cerebral hemisphere in front of the primary motor cortex.
Somatosensory cortex
The site for initial cortical processing of pressure, touch, heat pain and proprioceptive input
• Located in the anterior section of the parietal lobe, immediately behind the central sulcus.
• Each region within the somatosensory cortex receives sensory input from a specific area of the body.