Reporting Patient Safety Events: A Quick Reference Guide, Home Hemodialysis Study Guide for Annual Exam Preparation, Hemodialysis Procedures and Emergency Protocols, Hemodialysis Patient Care and Safety Protocols, Fresenius Dialysis Exam Preparation…
1/1319
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
1320 Terms
Near Miss
Near Miss does not result in patient clinical harm, either through early detection or sheer luck. It is an unsafe situation that is indistinguishable from a safety event except for the outcome.
Safety Event
Safety event resulting in mild to moderate patient clinical harm, not due to an underlying disease or condition. Requires additional monitoring, intervention, and or medical care.
Serious Safety Event
Serious safety event that results in severe to life threatening patient clinical harm, not due to an underlying disease or condition. Requires lifesaving or major medical intervention that may result in hospitalizations and/or death.
Continuous Improvement
Identify learning opportunities that can lead to the enhancement of providing safe patient care.
Reporting Process
Report Patient Safety Event to Clinical Services, Complete Root Cause Analysis and '5 Whys' Fishbone, Identify facility trends, opportunities for improvement, and create action plans, Update action plans in eQUIP minutes, monthly, Sustain the action plan, Ensure the Patient Safety event is reviewed during QAPI meeting with the discussion documented.
Goals of hemodialysis
Removal of fluids, Removal of toxins, Correct electrolyte balance
What can NOT be replaced in hemodialysis?
Replacement of hormones that the kidney no longer produces: Renin, Erythropoietin, and Calcitriol.
Diffusion
Movement of solutes through a semipermeable membrane from an area of greater concentration to an area of lesser concentration.
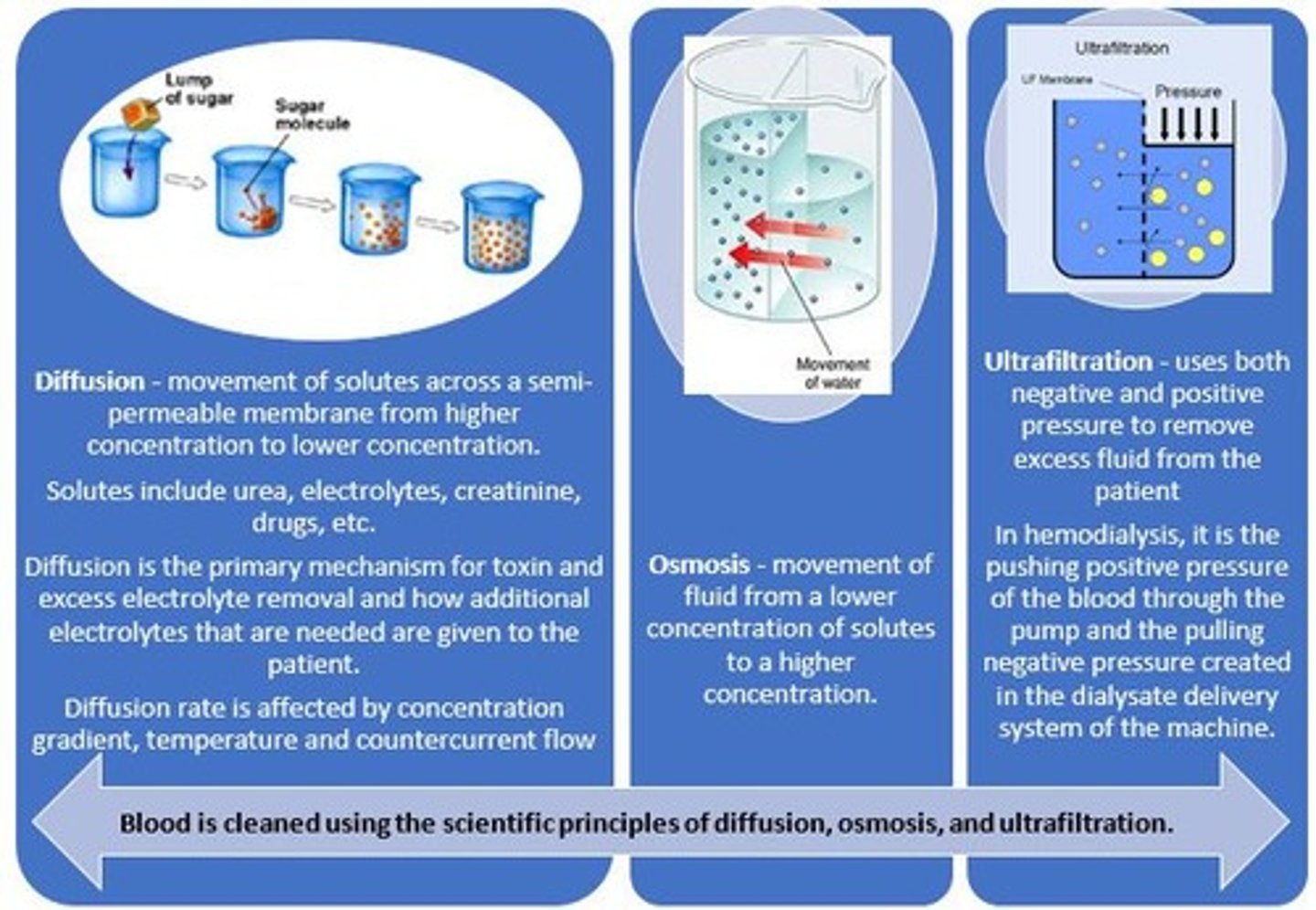
Factors affecting the rate of diffusion
Concentration gradient, Molecular weight of the solutes, Temperature, Membrane Permeability, Surface area, Flow geometry.
Concentration gradient
The difference in the concentration of solutes on each side of the semi-permeable membrane. The greater the difference, the higher the rate of diffusion.
Molecular weight of the solutes
Small molecules move faster.
Temperature
Particles move faster at higher temperatures.
Membrane Permeability
Number and size of pores.
Surface area
The more surface area, the more opportunity there is for diffusion to occur.
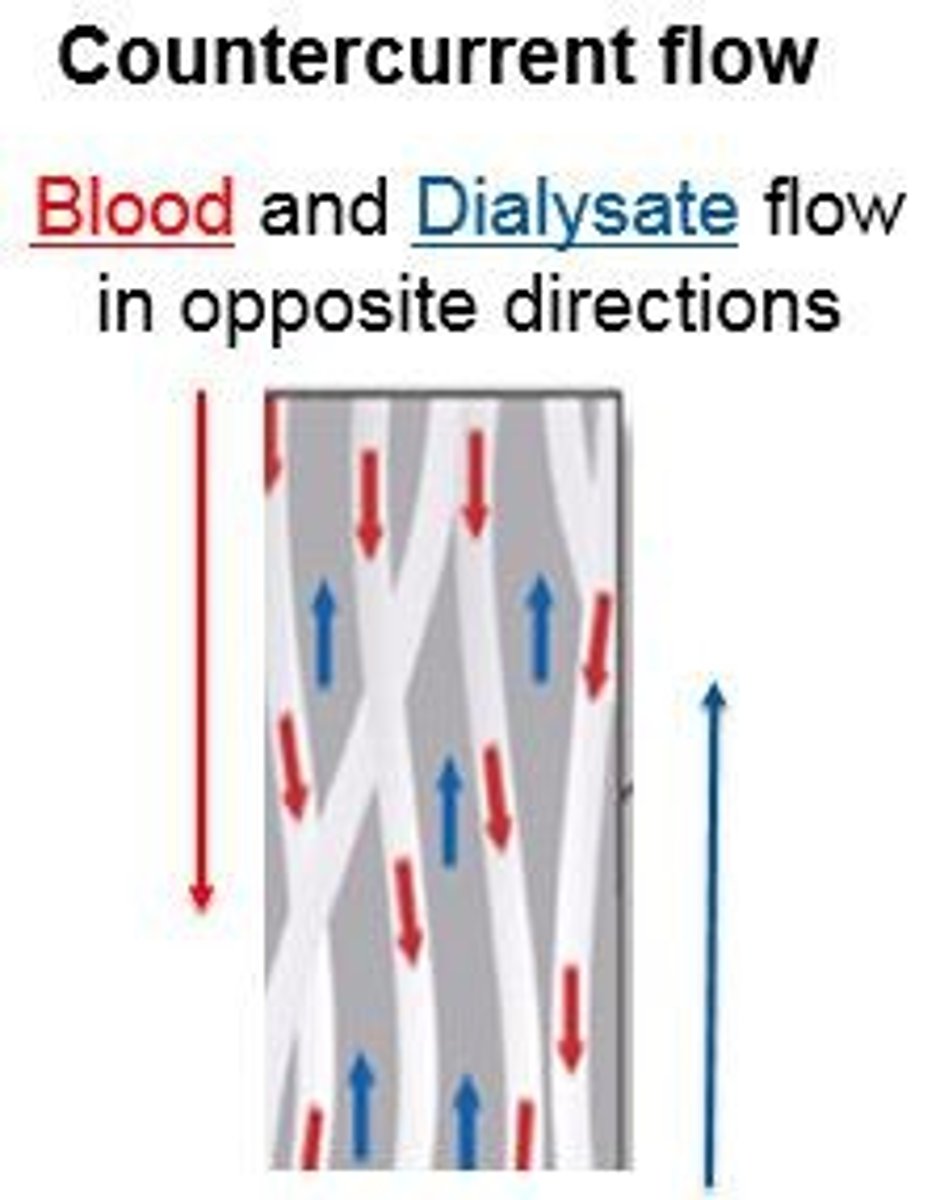
Flow geometry
Counter current flow; blood flows in one direction while dialysate flows in the opposite direction, establishing a concentration gradient.
Osmosis
Movement of fluid from an area of lesser concentration of solutes to an area of greater concentration of solutes.
Filtration
Fluid removal due to the molecular weight of the molecule and hydrostatic pressure of the fluid against the membrane.
Ultrafiltration
Fluid removal from the blood due to added pressure gradient across the membrane.
Transmembrane Pressure (TMP)
The difference in pressure; the blood side minus the dialysate side. The blood side is always positive, while the dialysate side may be positive or negative.
Characteristics of the dialyzer
Biocompatibility, Molecular weight cut off, Surface area, Ultrafiltration coefficient, Clearance.
Biocompatibility
The property of being biologically compatible by not causing an immune response in living tissue.
Adequacy
A measurement of how well wastes are clearing from the patient's blood.
Dialysis adequacy measurements
URR, Kdt/V, SpKdt/V, EKdt/V, EKdrt/V.
URR
Urea reduction ratio.
Kdt/V
Urea removed by dialysis.
SpKdt/V
Single pool.
EKdt/V
Double pool (Equilibrated).
EKdrt/V
Total equilibrated (includes residual renal function).
Test for URR
By obtaining blood samples pre and post treatment for BUN. FMS goal is: URR > 70%.
Kt/V
K stands for clearance of urea, t stands for time in minutes, V stands for total volume of waste (urea) that exists in the patient.
Measures to improve dialysis adequacy
Prime the dialyzer at BFR of 150 ml's/min.
SpKt/V
The amount of urea cleared from one space, the blood stream, measured on-line during dialysis by the rate of sodium removal during an On-Line Clearance test (OLC/AMP), using the conventional 2008 Fresenius Dialysis Machines. FMS goal is a minimum of 1.4L.
Post Treatment Lab Work Procedure
When the RTD clock reaches zero, turn off the UF rate, turn off the dialysate flow, and decrease the blood flow rate to 100 ml's/min. for 15 seconds. The blood pump is then stopped and the arterial and venous blood lines are clamped.
Pre Dialysis Assessment Factors
Vital signs (temperature, apical pulse, respiratory status, blood pressure), fluid status (weight, edema, respiratory rate and quality, blood pressure), access condition (bruit, thrill, signs and symptoms of infection, and bleeding), internal bleeding, GI status, mental status changes, and general complaints.
Estimated Dry Weight (EDW)
The medically prescribed weight of the patient if the kidneys functioned properly and no signs of fluid overload or dehydration, with normal breathing and clear lungs, and normal blood pressure for the patient.
Available Weight
The pre-treatment weight minus the Estimated Dry Weight (EDW).
Target Weight
The Available Weight plus the addition of prime, rinseback and any additional fluids received during the treatment, including blood, antibiotics, oral fluid intake, and routine normal saline flushes.
Common Pre-Treatment Questions
Questions to ask include: 'Any hospitalizations, chest pain, SOB?', 'How is your appetite, any nausea, vomiting or diarrhea?', 'How have you been sleeping?', 'What medications have you taken today, any new medications?', 'How have you been feeling between treatments?', 'Have you had any unusual bleeding?', 'Are you experiencing any pain?'.
Fresh Fill Procedure Volume
Immediately prior to connection of the blood lines to the patient's access, fill the circuit with 300 ml's of fresh saline solution, with 50 ml's for the arterial line by gravity, and 250 ml's for the venous line via the blood pump.
Blood Pump Speed for AVF/AVG
A blood pump speed of 150 ml's/min. is used for AVF/AVG.
Blood Pump Speed for CVC
A blood pump speed of 200 ml's/min. is used for CVCs.
Correct dialyzer
The specific dialyzer that matches the treatment prescription.
Correct dialysate
The dialysate solution that is appropriate for the patient's treatment.
Arterial end of dialyzer position
The arterial end of the dialyzer must be in the upright position.
Secure connections
All connections must be secure and visible.
Blood lines attachment
Blood lines must be securely attached to the dialyzer and in line guides.
Venous line security
The venous line must be secure in the air detector and occlusion clamp.
Transducers security
Transducers must be secure and dry.
High-low limits
Arterial and venous high-low limits must be acceptable.
Dialysate temperature limits
The dialysate temperature must be within specified limits.
BFR and DFR settings
Blood Flow Rate (BFR) and Dialysate Flow Rate (DFR) must be set according to prescription.
Heparin pump status
The Heparin pump must be on and the line unclamped if applicable.
UF goal
The Ultrafiltration (UF) goal must be correct and set.
Pre-treatment safety checks
Checks include correct dialyzer, dialysate temperature, manually checking conductivity and pH.
Dialyzer priming
Dialyzer and lines must be primed with saline.
Hanson connectors
Hanson connectors must be attached to the dialyzer.
Blood lines security
Blood lines must be secured in line guides with no kinking, twisting, or indentations.
Blood pump segment position
The blood pump segment must be correctly positioned.
Saline clamping
Saline must be clamped with at least 300 ml's in the bag.
Air/foam detector
The air/foam detector must be verified as armed.
Automatic testing
The machine must pass automatic testing (Alarm and PHT).
Dialysate flow setting
Dialysate flow must be set per physician's orders.
Venous limits
Venous pressure should never be greater than the blood flow rate.
Pre-pump arterial pressure limit
Pre-pump arterial pressure must not be more negative than -250 mm/Hg.
Transducer backside check
Checking the backside of a transducer wet with blood is important as it may affect pressure readings and cause cross-contamination.
Signs of hypotension
The partner of the home hemodialysis patient should monitor for signs and symptoms of hypotension, chest pain, and shortness of breath.
Emergency response
In an emergency, dial 911 first and follow instructions for treating hypotension, such as administering normal saline.
Vascular access integrity checks
Checks include secure connectors, intact tape, no change in appearance, enough slack in blood lines, and access being uncovered and visible.
HemoSafe® clip
The HemoSafe® clip must be attached to both venous and arterial limbs.
Reverse Osmosis (R.O.) checks
Total chloramines must be less than 0.1 ppm, and percent rejection must be equal to or greater than 90%.
RO disinfection frequency
ROs are disinfected monthly and after being shut off for more than 72 hours.
Aquaboss RO filter change frequency
Pre-treatment filters should be changed monthly or if the delta pressure is greater than 10 psi.
Causes of low pre-pump arterial pressure
Potential causes include clamped transducer monitor line, unclamped saline line, low blood pump setting, leaks, or arterial bloodline separation.
Causes of high pre-pump arterial resistance
Potential causes include hypotension, vessel spasm, needle against access wall, small needle size, arterial stenosis, low access flow, infiltration, mechanical obstruction, and clotted needle or access.
High pre-pump arterial resistance complications
Loss of dialyzer efficiency due to formation of micro-bubbles which can cause clotting of fibers, vascular access trauma and hemolysis of red blood cells from 'Shear Stress'.
Transmembrane Pressure (TMP) factors
Blood and dialysate flow rate, size of dialyzer, fluid goal, treatment time, needle size, access function and needle placement.
Muscle cramps management
Dietary control of salt and fluids, treat hypotension, treat hypokalemia, use pressure against cramping muscle (DO NOT MASSAGE), accurate assessment of EDW, and accurate calculation of UF goals.
Unresolved chest pain action
Instruct the caregiver to discontinue dialysis and call 911.
Signs and symptoms of angina
Pressure and pain which may radiate to the neck, jaw, shoulder or arms; apprehension, choking sensation, squeezing/crushing sensation, nausea, pallor, and cool clammy skin.
Infection management
Assess for source of infection (access, respiratory, UTI, dialysate/water), cultures, antipyretics for fever, and antibiotics per physician's order.
Signs and symptoms of septicemia
Headache, fever and chills, vomiting, malaise, dizziness, hypotension (not responsive to normal saline), and shock.
Pyrogenic reaction cause
Caused by the presence of dead bacteria endotoxins.
Prevention of pyrogenic reaction
Use aseptic technique to prepare machine, supplies, and for initiation of dialysis. Prepare bicarbonate according to policy and procedure. Disinfect the bicarbonate jugs, caps, wands, and/or mixing tank, dialyzer and blood lines used within 4 hours of set up.
Hypertension management
Monitor vital signs closely, adjust UFR for optimal fluid removal (careful assessment is a must), antihypertensive medications, and establish an accurate dry weight.
Causes of hypertension
Fluid overload, non-compliance with blood pressure medications, anxiety and nervousness, and Renin overproduction.
Hypotension management
Decrease UF goal, administer saline according to unit policy, place patient in Trendelenburg position, check BP, and administer oxygen as per policy.
Hemolysis complication
Hemolysis is the destruction of red blood cells releasing hemoglobin and potassium into the blood stream, causing ischemia and hyperkalemia.
Causes of hemolysis
Mechanical: Over occlusion of the blood pump segment, deformity in the lines, excessive negative pressure, and improper needle size with high BFR's. Chemical: Hypotonic dialysate, chemical agents (bleach), inadequately treated water, reaction to blood transfusion and some medications. Thermal: Overheated dialysate (greater than 40° degrees Celsius).
Interventions for hemolysis
Turn off the blood pump, DO NOT return the blood, notify RN/MD, call 911 if patient is at home, treat patient symptoms, draw blood from venous line and spin to check for positive hemolysis. Draw dialysate samples from the effluent line.
Crenation definition
Destruction of red blood cells due to hypertonic dialysate bath.
Signs and symptoms of crenation
Very dark red blood, sudden thirst, flushed face, headache, nausea, vomiting, shortness of breath, chest pain, blood pressure changes, abdominal cramps, agitation, seizures, coma, and death.
Causes of hyperkalemia
Wrong dialysate potassium, dietary indiscretion, hemolysis or crenation, frequent infections or excessive tissue breakdown, sepsis, or recent blood transfusion.
Foods high in potassium
Potatoes, tomatoes, citrus fruits, and melons.
Hyperkalemia
Signs and symptoms may include: muscle weakness, numbness, tingling around mouth, tongue, hands and feet, dysrhythmias, slow pulse, chest pain, and cardiac arrest.
Hypokalemia
Low serum potassium may be caused by: blood loss, nausea, vomiting, diarrhea, blood pressure medications, diuretics, excessive dialysis, and low potassium dialysate.
Signs and symptoms of hypokalemia
May include: muscle weakness, muscle aches or cramping, palpitations, and cardiac arrhythmias (irregular heartbeats).
Vascular access complications
Causes could stem from: improper needle placement, inadequate Heparin, immature fistula, venous or arterial stenosis, biofilm lining the walls of the catheter, hypotension, and catheter kinks.
Extracorporeal circuit clotting reasons
Might clot due to: inadequate Heparinization, air in the circuit, inadequate blood flow, high hemoglobin and/or hematocrit, low dialysate temperature, infection, and dehydration.
Blood Leak
Perforation of the dialyzer membrane large enough to allow blood to cross over the membrane into the dialysate.
Management for blood leaks
Stop the blood pump, clamp the lines. Verify the blood leak with a blood leak test strip. Adjust dialysis time, set up new circuit and dialyzer if positive results. Notify home therapy nurse.