Abdomen Semiotics
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
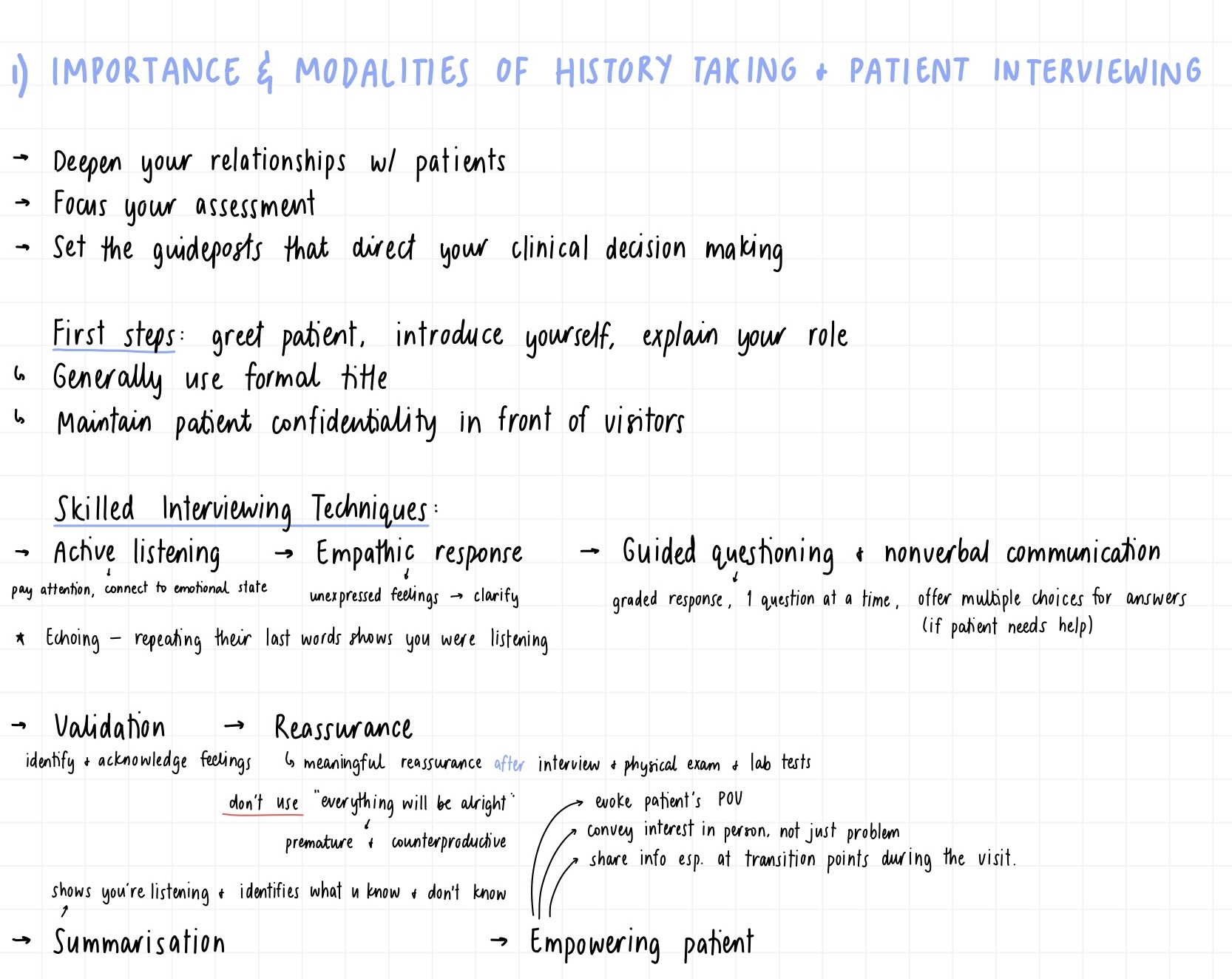
Importance and modalities of history taking and patient interviewing
hypothetico-deductive model: collect information, form hypothesis, test it against evidence
logical, evidence based approachneed to gather information to determine the patients problem to make an accurate diagnosis
establish trust and rapport with patient to gather necessary information to make a correct diagnosis
Essential elements of clinical care:
empathetic listening
able to interview all backgrounds and cultures
process of clinical reasoning to find diagnosis
need to be adaptable and able to improvise based on patient
establish good relationship, introduce yourself
let them decide about whether visitor stays or not
open ended questions (not leading)
active listening, empower the patient
avoid bias, use multiple choice responses
History taking (9 steps)
1 - chief complaint
2 - history of present illness (OPQRST-A)
3 - past medical history (e.g. previous digestive diseases, infectious diseases, malignancy)
4 - past surgical history (operations in chronological order)
5 - allergies (medication, latex, food, seasonal)
6 - medications (even over-the-counter + herbal; dosage, medical reason for each)
7 - social history (occupation, marriage status, tobacco/alcohol/illicit drug use)
8 - familial history (major medical conditions)
9 - review of systems (general, skin/breast, eyes/ears/nose/mouth/throat, CVnR, GI, GU, MS, neurological/psychiatric, allergic/immunologic/lymphatic/endocrine)
Signs vs symptoms
signs are objective findings from physical examinations
symptoms are subjective concerns from the patient
OPQRST-A
O - onset: when did these symptoms first occur
P - prior occurence
Q - quality: is it stabbing or throbbing pain
R - radiation: does the pain 'spread' to other areas
S - severity: 1-10 scale
T - timing: when does the pain occur
A - associated symptoms like fever/ jaundice
order of medical examination steps
inspection
auscultation
palpation
percussion
- listen before palpation so you don’t move contents
Anatomical regions
4 quadrants: line from xiphoid process to pubic bone, line across along the umbilical region
9 regions: right hypochondriac, epigastric, left hypochondriac, right lumbar, umbilical, left lumbar, right iliac, hypogastric, left iliac
right hypochondriac region
liver, gallbladder (and most of the biliary tract), hepatic flexure of colon, right kidney (upper pole)
left hypochondriac region
spleen - completely under the costal elements if spleen not enlarged
fundus of stomach
tail of pancreas
left kidney (upper pole)
splenic flexure of colon
epigastric region
stomach
left liver lobe
duodenum
pancreas (head and body)
right lumbar region
ascending colon
right kidney
small intestine
(if liver is enlarged the gallbladder may be here)
umbilical region
small intestine (jejunum and ileum)
transverse colon
left lumbar region
Left kidney
descending colon
Small intestine
right iliac region
appendix
caecum
ovary
hypogastric region
bladder
uterus (below bladder; if enlarged)
sigmoid colon
small intestine
left iliac region
Sigmoid colon
Left ovary and fallopian tube
diverticulitis normally found here
Possible findings in abdominal inspection
skin changes
colour/ scars/ rashes/ stretch marks (straie) (purple straie can indicate crushing syndrome - overproduction of corticosteroids)
Portocaval venous patterns - caput medusae/prominent veins (portal hypertension)
visible peristalsis or pulsations (intestinal obstruction, aortic aneurysm)
localised bulges of abdominal wall: ventral hernias (umbilical, incisional, epigastric) + subcutaneous tumours (lipoma)
diastasis recti (separation of rectus abdominis muscles; clinically benign; seen only when patient raises head and shoudlers)
distended abdomen (obesity, ascites, organomegaly, bowel obstruction)
Protuberant abdomen
Bruising
Grey Turner sign =
Pancreatitis causes bleeding in the flank areaCullen’s sign = bruising in periumbilical region = ectopic pregnancy or acute pancreatitis
Protuberant abdomen
Fat - dull sound
Cancer - if tumour protrudes it is already very serious
Gas - will hear tympanic percussion sounds that move when patient lies on side
Pregnancy
Protuberant abdomen with bulging flanks:
Ascites: fluid retention: taut and shiny skin
Possible findings in abdominal auscultation
Provides info about bowel motility
Bowel sounds
clicks and gurgles (5-34/min)
occasionally, prolonged gurgles of hyperperistalsis from “stomach growling” called borborygmi
bowel sounds may be increased → diarrhoea, early intestinal obstruction
bowel sounds may be decreased then absent (listen for at least 2 mins before deciding they’re absent) → adynamic ileus, peritonitis
High-pitched tinkling sounds → intestinal fluid + air under tension in a dilated bowel
Rushes of high-pitched sounds + abdominal cramp → intestinal obstruction
Venous hum
soft humming sound with systolic + diastolic components
increased collateral circulation between portal and systemic venous systems → hepatic cirrhosis
Vascular bruits
Hepatic bruit → liver carcinoma, cirrhosis
Arterial bruit w/ systolic + diastolic components → partial occlusion of aorta/large arteries
In epigastrium → renal artery stenosis, renovascular hypertension
Friction rubs
Rare grating sounds w/ respiratory variation
Inflammation of peritoneal surface of an organ → liver cancer, chlamydial or gonococcal perihepatitis, recent liver biopsy, splenic infarct
Systolic bruit + hepatic friction rub = liver carcinoma
Possible findings in abdominal percussion
Tympanic (high pitched and hollow) = air, found at fundus of stomach or over intestines
Localised tympany = trapped gas
Excessive tympany = pneumoperitoneum = very dangerous
Dull = solid → found over solid organs e.g. liver and spleen
Hepatomegaly = dull sounds below the costal margin
Ascites = moving dullness as fluid moves
Giordano’s sign
Percussion tenderness of kidneys
Giordano’s sign
If kidneys tender to palpation, assess percussion tenderness over CVAs. Place the ball of one hand in CVA + strike with ulnar surface of fist
Possible findings in abdominal palpation
Start with light palpation and on the opposite side to where they are experiencing pain
detects abdominal tenderness, muscular resistance, some superficial organs + masses
McBurney's + Lanz Point: Appendicitis.
Murphy's (gallbladder) Sign: Acute cholecystitis.
Superior + inferior ureteral points
Rovsing's Sign: Referred pain in RLQ on palpation of LLQ (appendicitis).
Cullen's Sign: Periumbilical tenderness with discoloration (pancreatitis, retroperitoneal haemorrhage).
Grey Turner's Sign: Flank tenderness with discoloration (retroperitoneal haemorrhage).
Deep Palpation → to delineate the liver edge, kidneys + abdominal masses
palpation point: gallbladder
Firmly palpate RUQ subcostal region, pushing under ribs. Ask patient to take deep breath - pain = cholecystitis → Murphy’s sign
Visceral pain
Occurs when hollow abdominal organs (e.g. intestine or biliary tree) contract unusually forcefully or are distended or stretched.
Solid organs (e.g. liver) can become painful when their capsules are stretched.
May be difficult to localise
Typically palpable near midline (levels vary according to structures involved)
Ischemia also stimulates visceral pain fibres
Parietal pain
Originates from inflammation of the parietal peritoneum i.e. peritonitis.
Steady, aching pain that is usually more severe than visceral pain
More precisely localised over involved structure.
Typically aggravated by movement or coughing.
Patients with parietal pain usually prefer to lie still.
In contrast to peritonitis, patients with colicky pain from a renal stone move around frequently trying to find a comfortable position.
Characteristics and main causes of gallbladder pain
Causes (Clinical): Biliary colic, cholecystitis, ascending cholangitis
Onset: Can appear after meals, especially if abundant/rich (e.g. fats, eggs)
Quality: Acute, in waves (colicky pain; increasing intensity), in the right hypochondriac region and epigastrium.
Radiation: Possible radiation to the homolateral shoulder and to the back.
Associated Symptoms:
Nausea (common)
Vomiting (common)
Bloating (common)
Sweating, fever, chills (if infection)
Jaundice (if cholangitis or biliary obstruction)
Underlying Causes (Pathophysiological):
Gallstones are most asymptomatic - they cause symptoms when they cause obstructions .
Obstruction of the gallbladder (in the cystic duct)
Biliary colic (nausea, pain, vomiting)
Acute cholecystitis (fever)
Obstruction of the bile duct
Obstructive jaundice
Cholangitis (jaundice, fever)
Pancreatitis (jaundice, fever, pancreatic pain)
Gallstone ileus is a rare complication after a long history of large gallstones causing pressure on gallbladder wall with the formation of a fistula with the duodenum.
Characteristics & Main Causes of Pancreatic Pain
Pancreatic pain is primarily caused by pancreatitis, which is an inflammation of the pancreas.
Under normal circumstances, pancreatic enzymes activate only within the duodenum to aid digestion.
However, during pancreatitis, these enzymes activate prematurely inside the pancreas itself due to the blockage of the pancreatic duct. As these enzymes are designed to digest proteins, they effectively begin to digest the pancreatic tissue, leading to a self-destructive cycle.
This condition can escalate quickly and become life-threatening.
Causes: Choledocolithiasis, alcohol abuse
Onset: Can appear after meals, especially if abundant/rich (e.g. fats, eggs)
Quality: Starts in waves (colicky pain) in epigastrium, then becomes constant
Radiation: Belt-like radiation, to the back
Associated Symptoms:
Nausea
Vomiting
Sweating
Fever
Chills
Jaundice
Characteristics of Pain Related to Abdominal Aorta Aneurysms
Aortic aneurysms often grow slowly and usually without symptoms. Predicting how fast an aortic aneurysm may enlarge is difficult.
Symptoms of abdominal aortic aneurysm enlargement:
Pulsating feeling near the navel
Deep, constant pain in abdomen
Back pain
Impending Aneurysm Rupture
Onset: Sudden, intense and persistent abdominal or back pain → often reported as a tearing sensation
Radiation: To the back of the legs
Associated Symptoms: Dizziness, sweatiness (forehead), nausea and vomiting
Physical Examination:
Low blood pressure with fast pulse
Asymmetric peripheral pulse in the lower limbs
Characteristics of Splenic Pain, Palpation of the Spleen, and Causes of Splenomegaly
Not in slides: Normally, the spleen is not palpable unless significantly enlarged. Examiner starts palpation in the RLQ and moves diagonally towards the LUQ (following splenic enlargement). With deep inspiration, a large spleen may be felt descending below the costal margin.
Pain originating from the spleen is a rare phenomenon. The spleen‘s parenchyma, similar to that of the liver, lacks nocicepters, making it incapable of directly sensing pain. However, pain may arise from the capsule or the peritoneum surrounding the spleen when these regions are affected. For pain to manifest, the sub-capsular region of the spleen must be involved.
Splenomegaly
Causes of Splenomegaly:
Portal hypertension (e.g. liver cirrhosis → increased pressure in portal vein)
Hematologic diseases (e.g. leukemia, lymphoma)
Metabolic and congenital diseases (e.g. Gaucher disease → lipid infiltration of the spleen)
Infections (e.g. mononucleosis → spleen is a key player in immune system)
Enlargement of the spleen itself does not cause pain, but it can increase the risk of:
Infarctions (due to disrupted blood flow).
Ruptures or lacerations (as an enlarged spleen is more fragile).
Infarction (spleen)
Cause: Blockage of the splenic artery, often from metastatic septic emboli (e.g., from endocarditis)
Sudden-onset pain in the LUQ (left upper quadrant) and posterior ribs.
Referred to the left shoulder (Kehr’s sign).
Pain can range from a dull ache to a sharp, stabbing sensation.
Rupture (spleen)
Leading cause: Trauma (e.g., direct blow to the abdomen, car accidents).
Symptoms:
Severe internal bleeding → Signs of shock (hypotension, rapid pulse, sweating).
Pain may not be immediately obvious, as general symptoms (shock) can mask abdominal discomfort.
If due to trauma, rib fractures may be the primary source of pain.
Signs & Symptoms of Peritonitis and Possible Causes
Steady, aching pain
Can be localised or generalised
Generalised Peritoneal Pain
Primary Peritonitis (liver cirrhosis with ascites, complications from peritoneal dialysis)
Secondary Peritonitis (bowel perforation, abscesses or other infectious conditions)
Localised Peritoneal Pain
Arises from local irritation of the peritoneum, usually due to an infectious process (cholecystitis, colonic diverticulitis, appendicitis)
It is well-localised and typically in close proximity to the affected organ.
Rebound Tenderness (Blumberg Sign)
Definition: Rebound tenderness is felt when the abdominal wall is compressed slowly and then released rapidly, causing a sudden stab of pain.
This may make the patient wince or moan in response. Observing the patient’s facial expression during this test is crucial.
Mechanism of Pain: The pain occurs due to a tuning-fork action, where inflamed visceral and parietal peritoneum come into contact during the release, creating a vibratory-like movement.
Possible Manifestations/Characteristics of Periumbilical Abdominal Pain
Early appendicitis
Mesenteric ischemia
Gastroenteritis
Small bowel obstruction (SBO)
Meckel’s diverticulitis
Umbilical hernia
Abdominal aortic aneurysm (AAA)
Acute Appendicitis: Signs & Symptoms
Dull pain starting the umbilical region.
As time passes, the pain increases and becomes localised in the RLQ (with aching features)
Associated symptoms: nausea, fever, loss of appetite, weakness
McBurney sign: tenderness at McBurney’s point (might not be present at the symptoms’ start)
Rovsing sign: Palpation in the LLQ elicits pain in the RLQ
Dunphy’s sign = pain when patient coughs
Rebound tenderness
Dyspepsia
Going from most to least common diagnoses in patients with dyspepsia (upper abdominal discomfort):
Functional dyspepsia
GERD
Peptic ulcer
Esophago-gastro-duodenal malignancies
Alarming signs in Dyspepsia
Age > 50 years (malignancies more prevalent)
Unintentional weight loss
Dysphagia (difficulty swallowing)
Anemia
Persistent vomiting
Gastrointestinal bleeding (in vomit or stool)
Jaundice (yellow skin/sclera)
Possible Manifestations/Characteristics of RUQ Abdominal Pain
(Not in slides)
Characteristics:
Steady or sharp pain that is persistent or intermittent; radiates to back
Tenderness to palpation
Referred pain in right scapula
Biliary colic: intermittent, cramping pain
Nausea, vomiting, fever, chills
Jaundice, pale stool, bloating, swelling
Murphy’s sign
Pain aggravated by fatty foods
Liver enlargement, ascites
Potential Causes
Gallstones
Cholecystitis
Cholangitis (bile duct inflammation)
Hepatitis
Liver abscess
Hepatic cysts
Liver tumours
Duodenal ulcers
Hernia
Definition & Related Causes of Heartburn and Regurgitation
Heartburn: Rising retrosternal burning pain or discomfort.
Can be aggravated by foods e.g. alcohol, chocolate, citrus fruits, coffee, onions, and peppermint
Can be aggravated by positions e.g. bending over, exercising, lifting, or lying supine.
Pain may radiate up to throat
Regurgitation: Rise of oesophageal or gastric contents without nausea or retching.
Regurgitation is a passive act.
Both usually go hand in hand, caused by GERD
Definition & Related Causes of Dysphagia and Odynophagia
Dysphagia: Difficulty swallowing
Odynophagia: Painful swallowing
Food that seems to stick or “not go down right” suggests motility disorders or structural anomalies.
The sensation of a lump or foreign body in the throat, unrelated to swallowing, is called a globus sensation; it is not true dysphagia.
Ask the patient to point to where the dysphagia occurs.
Ask which types of food provoke symptoms: solids, or solids and liquids?
Establish the timing.
When does the dysphagia start?
Is it intermittent or persistent?
Is it progressing? If so, over what time period?
Are there associated symptoms and clinical conditions?
Esophageal Dysfunction (Mechanical Obstacles) | Neurological Disorder |
Cancer
| Swallowing liquids requires more coordination than solids.
|
Normal Bowel Movements & Stool Shapes
Bristol Stool Chart (not used in a clinical setting; useful for patients and students)
Type 1: Separate hard lumps (severe constipation)
Type 2: Lumpy and sausage-like (mild constipation)
Type 3: A sausage shape with cracks in the surface (Normal)
Type 4: Like a smooth, soft sausage or snake (Normal)
Type 5: Soft blobs with clear-cut edges (lacking fibre)
Type 6: Mushy consistency with ragged edges (mild diarrhoea)
Type 7: Liquid consistency with no solid pieces (severe diarrhoea)
The range of normal frequency for bowel function is broad: 3 times a day to 3 times a week.
Abnormal Stool Colours and Related Causes
Acholic stools: White, cretaceous stools due to lack of stercobilinogen (complete biliary occlusion -> gallstone/cancer)
Mucus: Can be found as yellow flakes in a series of non-concerning situations (irritation of muciparous glands)
The combination of liquid stools with blood, pus and mucus suggests infectious or ulcerative colitis
Steatorrhea: Loose, greasy, yellowish stools due to lipid malabsorption. Might be bulky and hard to wash. Usually found in pancreatic failure (chronic pancreatitis, cystic fibrosis)
Black = melena
Red = hematochezia
Silver stools (Thomas’s sign): Extremely rare due to the coexistence of melena and acholic stools. Reported in biliary tract cancer.
Definition & Causes of Melena
Melena: Black, tarry (and usually liquid) stools indicating the presence of digested blood
Upper GI bleed (proximal to ligament of Treitz → oesophagus, stomach, duodenum)
Causes:
Esophageal varices (from cirrhosis, portal hypertension)
Gastritis
Peptic ulcer disease
Definition & Causes of Haematochezia
Haematochezia: Passage of fresh, bright red blood in the stool (often as coating stripes, at the end of evacuation)
Lower GI bleed (colon, rectum, anus)
Diverticular diseases
Haemorrhoids
Anal fissures
Polyps
Rectal cancer
Definition & Types of Diarrhoea
Definition: Painless loose or watery stools during at least 75% of defecations (at least 3 evacuations per day) for the last 3 months, with symptom onset at least 6 months prior to diagnosis.
Duration:
Acute diarrhea: Less than 2 weeks.
Infections (viral, bacterial)
Chronic diarrhea: 4 or more weeks.
4 types: secretory, osmotic, inflammatory, motor
Types of diarrhea
Secretory diarrhea: Increase of intraluminal salt secretion (recourse liquids -> water drawn into intestines)
Causes: Bacterial toxins, drugs, malignancies (NHL, colonic cancer), bile acid malabsorption
Usually > 1L / day
Frequency does not reduce with fasting
Osmotic diarrhea: Presence of non-absorbable compounds, e.g. certain sugars draw water into the intestines, e.g. lactose intolerance
Usually < 1L/day
Disappears with fasting
Inflammatory diarrhea: Damage to the integrity of intestinal barrier
Causes: Infections (e.g. cholera), drugs
Usually > 1L / day
Frequency does not reduce with fasting
Motor diarrhea: Alteration in bowel motility
Drugs, electrolyte imbalance, endocrine diseases (e.g. hypothyroidism, hyperthyroidism, diabetes)
History Taking in Patients with Diarrhoea
Duration (to decide if acute or chronic)
Volume, frequency, consistency
Is there mucus, pus or blood?
Does it occur at night? (Nocturnal diarrhoea is usually pathological; not functional)
Is there associated tenesmus - a constant urge to defecate (but no evacuation) - accompanied by pain, cramping and involuntary straining?
Are the stools greasy or oily? Frothy?
Constipation identification + what to ask patient
Stool characteristics identified by the Rome III criteria:
Constipation should be present for the last 3 months
Symptom onset at least 6 months prior to diagnosis and meets at least two of the following conditions:
Fewer than 3 bowel movements per week
25% or more defecations with either straining or sensation of incomplete evacuation
Lumpy or hard stools
Manual facilitation
Check if the patient actually looks at the stool and can describe its color and bulk.
What remedies has the patient tried?
Do medications or stress play a role?
Are there associated systemic disorders?
Classification of Constipation
Episodic Acute Constipation
Contingent situation
Lifestyle modification (environment, diet)
Iatrogenic (e.g. after surgery)
Immobilisation
Acute diseases
Pregnancy (especially in last month)
Chronic Constipation
a. Secondary Constipation
Reversible
Stenosis
Hypothyroidism
Hypercalcemia
Drugs
Irreversible
Neurological diseases
Myopathies (muscle disease)
Cognitive disorders
b. Functional Constipation
No organic diseases
Alternation in mechanisms of colorectal-anal motility and sensitivity.
Constipation - medical history + physical examination
Medical History
Evaluate if symptoms are consistent with the definition of constipation and require further investigation.
Investigate about diet and habits.
Rule out systemic diseases or drugs causing constipation.
Physical Examination
Look for alarming signs and indications for further testing (colonoscopy)
Age > 50 years (oncologic prevention)
Blood in stool
Recent worsening of symptoms
Nocturnal pain
Unsatisfactory response to cathartics (laxatives)
Fever
Anemia
Pathological findings at rectal examination (especially rectal exploration)
Rectal examination for hemorrhoids, polyps, fecal impaction (hard lump of feces), etc.
Ileus
Ileus is the disruption of the normal propulsive ability of the intestine (fails to guarantee the normal progression of its content from mouth to anus).
Do not confuse it with constipation. Constipation is slowed transit/evacuation with no associated symptoms (except bloating). Ileus is disrupted motility or obstruction and is always associated with clinical manifestations apart from merely “no evacuation”, i.e. absence of flatus, colicky pain, vomiting, etc.
Paralytic Ileus
Loss of normal intestinal contraction
Causes: Abdominal surgery (sliced peritoneum needs time to heal), drugs (opioids; contribute, but not direct cause), peritonitis, hypokalaemia (low serum potassium)
Symptoms: Nausea, vomiting, mild abdominal discomfort
Physical examination: No bowel sounds
Mechanical Ileus (aka Bowel Obstruction)
Normal contraction, but obstacles are obstructing the intestine
Causes: Tumors, peritoneal adhesions, hernias, diverticulitis (inflammation of last part of colon), volvulus (strangles part of intestine), gallstone (rare)
Symptoms: vomiting, abdominal colicky pain, no bowel function (no flatus, no stool)
Physical examination: Hyperactive, high-pitched bowel sounds
Causes, Signs and Symptoms of Bowel Obstruction
Bowel obstruction = mechanical ileus
Symptoms
Pay attention to the order of the symptoms
Proximal Obstruction
Vomiting
Pain
No bowel function
Medium-Level Obstruction
Pain
No bowel function
Vomiting
Distal Obstruction
No bowel function
Pain
Vomiting
Causes, Signs & Symptoms of Bowel Perforation
Bowel perforation is an insult or injury to the mucosa of the bowel wall causing a violation of the closed system.
Causes:
Bowel obstruction
Bowel ischemia (inadequate blood supply)
Gastric or duodenal ulcer disease
Diverticular disease
Infection
Gastrointestinal tumors
Trauma: blunt or penetrating
Iatrogenic, e.g. perioperative
Clinical Presentation:
Sudden and severe abdominal pain
Sometimes with localised peritonism (symptoms suggesting peritoneal inflammation or irritation) or a rigid abdomen on examination.
There may be an initial relief of pain as the dilated bowel collapses.
The pain begins again when peritonitis develops.
X-ray will show free air in the peritoneum - surgical emergency
Definition & Types of Jaundice
Yellowish color of skin and sclerae from increased levels of bilirubin
Normal range:
Total bilirubin (direct/conjugated + indirect/unconjugated) = 0.2-1.2 mg/dL
Direct (conjugated) bilirubin = 0.1-0.4 mg/dL
Bilirubin levels > 2.0-2.5 mg/dL (visible on sclerae)
Bilirubin levels > 3 (visible on skin)
Total bilirubin (with high direct bil) >= 9.5 mg/dL (obstructive jaundice)
Types of Jaundice
Pre-hepatic
Heme overflow: hemolysis
Genetic error in liver uptake → Gilbert disease
Hepatic
Liver diseases: hepatitis and cirrhosis
Genetic error in conjugation → Crigler-Najjar syndrome (infants; rare)
Post-hepatic
Bile duct obstruction
Genetic error in secretion → Dubin-Johnson and Rotor disease
Painful jaundice does not point to stones, but rather compressive obstruction (often pancreatic or biliary tumors) or cirrhosis (but in these cases, mixed bilirubin).
Associated Symptoms with Bile Duct Obstruction and Jaundice
Color of urine (dark red/brown)
Skin itch without other explanation (in cholestatic or obstructive jaundice)
Pain (distended liver capsule, biliary colic, pancreatic cancer)
Acholic stool (briefly in viral hepatitis, common in obstructive jaundice)
Jaundice + acholic stool = obstructed bile duct
Symptoms Potentially Associated with Jaundice
Severe abdominal pain and tenderness → cholecystitis, pancreatitis
Changes in mental function (drowsiness, agitation/confusion) → cirrhotic liver failure
Blood in stool or tarry black stool (melena), blood in vomit (hematemesis) → portal hypertension
Fever → cholangitis
Weight loss, anorexia → pancreatic cancer
Jaundice due to haemolysis…
Jaundice due to haemolysis results in an increase of indirect (unconjugated) bilirubin, which cannot pass in the urine.
The excess unconjugated bilirubin is metabolised as urobilinogen, which can pass in the urine.
Urobilinogen is colourless, but if the urine is exposed to light, it may assume a bright orange colour
Signs & Symptoms of Inguinal Hernia
Inguinal hernia occurs when part of intestine protrudes through a weak spot in abdominal muscles to create a bulge
More common in men than women
There are 2 types:
Indirect: most common, all ages, both sexes, above inguinal ligament near midpoint, often courses to scrotum
Direct: less common, older men, rare in women, above inguinal ligament close to pubic tubercle, rarely courses to scrotum
Signs and symptoms:
visible bulge in groin area especially when standing or straining
groin discomfort, pain or discomfort when coughing
localised swelling
tenderness to touch, feeling pressure or heaviness in groin
increased pain with physical activity
changes in bowel movements: in some cases hernia become strangulated and compromise blood supply
Definition & Causes of Dysuria, Urgency and Frequency in Urinary Bladder Voiding
Dysuria: painful urination (UTI, STI, urinary stones, intestinal cystitis)
Urgency: sudden need to void (bladder infection, OAB, bladder stones, neurological conditions)
Frequency: frequent voiding (diabetes, UTI, diuretic medications, bladder disorders, bladder outlet obstruction)
Alterations in urinary frequency + causes
Polyuria: urine output > 2L/day
Causes: excess water intake, diabetes insipidus, renal diseases, drugs (diuretics)
Oliguria: urine output < 1L/day
Causes: Reduction of renal blood flow (shock, haemorrhages, severe infections, heart failure), renal diseases
Anuria: urine output < 100 cc/day
Same causes as oliguria but indicates a severe condition. The kidneys are not able to produce urine.
Anuria vs urinary retention
Anuria: The bladder is empty because the kidneys are not producing urine.
Urinary retention: The bladder is full and cannot empty because of an obstruction.
Urinary colours + causes
brown - conjugated bilirubin in urine = severe liver disease/ obstructive jaundice
purple - bacterial infection causes sulphatase/ phosphatases in urine, occurs in constipated women
clear to dark yellow indicates level of dehydration
orange urine can be caused by B12 / A
Definition & Characteristics of Hematuria
Blood in urine
haemoglobinuria = haemoglobin, not intact RBCs, in urine - looks more pale than haematuria
Causes: UTI, kidney stones, cancer
Definition & Classification of Urinary Incontinence
Unintentional urination
Stress incontinence (momentary leakage of small amounts of urine with coughing, laughing, sneezing while person is in upright position; urine loss unrelated to conscious urge to urinate)
Urge incontinence (involuntary urine loss preceded by an urge to void; moderate volume)
Overflow incontinence (detrusor contractions insufficient to overcome urethral resistance, causing urinary retention)
Functional incontinence (on the way to toilet or only in the early morning)
Signs & Symptoms of Reno-ureteral Colic
acute, severe pain caused by obstruction of urinary tract, ureter and pelvis distention
Signs and symptoms:
location: flank pain begins in lower back and radiates to lower abdomen
quality: sharp and intense
onset: sudden
duration: intermittent episodes
aggravating factors: physical activity
relieving factors: rest and change in positions
urinary symptoms: hematuria, frequency, urgency
associated symptoms: nausea, vomiting, flank tenderness, fever and chills
Signs & Symptoms of Epididymitis
inflammation of epididymis, can be due to infection or other inflammatory conditions
sexually transmitted diseases are a common cause of epididymitis
Signs and symptoms:
testicular pain: localized to one testicle and may be gradual or sudden onset, may radiate to lower abdomen or groin
swelling: tenderness and swelling in affected testicle
redness of scrotal skin
dysuria: painful urinating
frequency and urgency of urination
discharge from penis
fever and chills
enlarged lymph nodes in groin
pain during ejaculation and physical activity
Prehn’s sign: relief of pain when scrotum is elevated