1. blood + fluid compartments
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Which of the following has a very high concentration in plasma, but a much lower concentration in the interstitial fluid?
1. Sodium
2. Proteins
3. Potassium
4. Bicarbonate
2. Proteins
blood makes up what % of the bodily fluids
8% of the bodily fluids
composition of blood
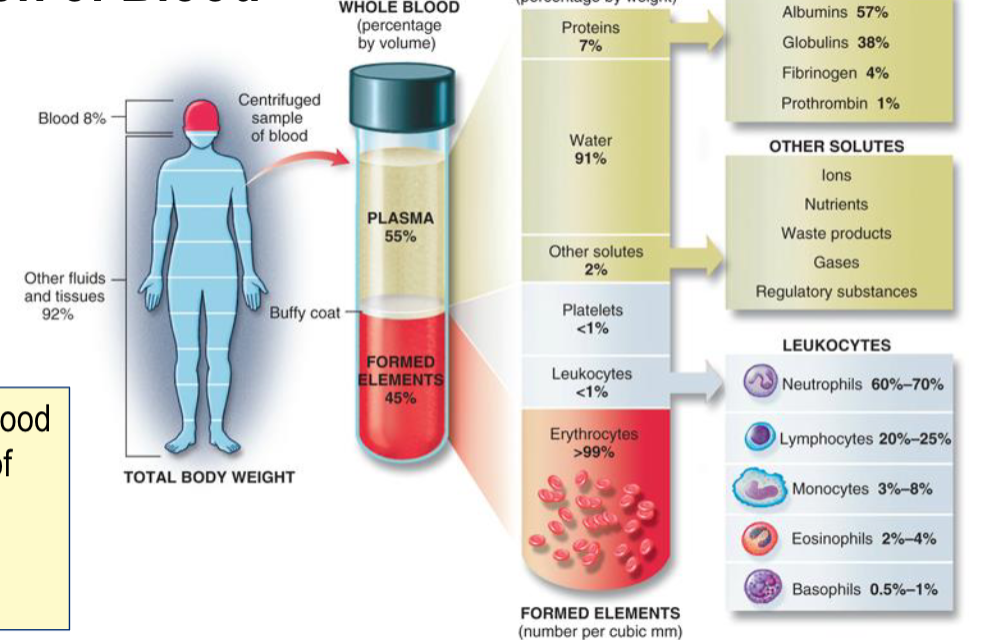
Hematocrit
% of blood volume composed of erythrocytes
Men = 45%
Women = 40%
formed elements
erythrocytes
no nucleus so not cells
common plasma proteins
Albumin
Globulins
Fibrinogen & Clotting Factors
transthyretin
a1-antitrypsin
B- lipoprotein (LDL)
transferrin
complement proteins
Plasma proteins: Albumin
Most abundant plasma protein
Binds to many substances in plasma – important for transport
steroids, bile, salts, fatty acids
Maintains osmotic (oncotic) pressure
oncotic pressure
osmotic pressure specific to plasma proteins
Plasma proteins: Globulins
Carrier proteins
immunoglobulins (antibodies)
what type of immunity is antibodies (immunoglobulin)?
humoral immunity
plasma proteins: transthyretin
Binds T3/T4 and Vitamin A
plasma proteins: a1-antitrypsin
Protease inhibitor
plasma proteins: B- lipoprotein (LDL)
Binds lipid
plasma proteins: transferrin
Binds iron
plasma proteins: complement proteins
Innate immunity
To measure a specific compartment what are the conditions?
solute must be freely permeable throughout compartment, but confined to only that compartment
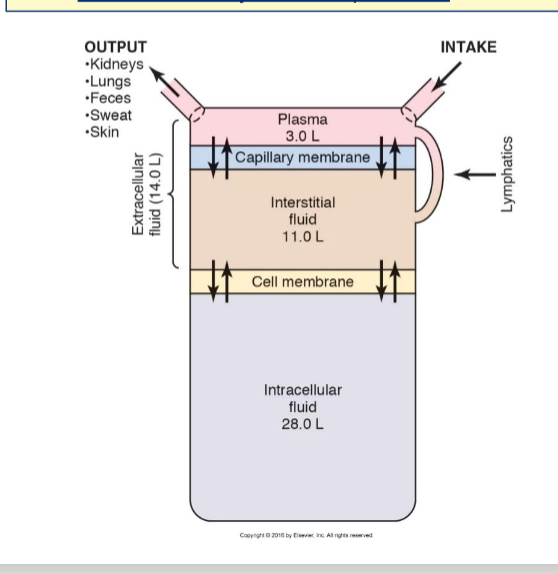
how to measure body fluid compartments: Total body water
3H2O (tritiated water)
how to measure body fluid compartments: Extracellular Fluid
22Na+, Inulin
how to measure body fluid compartments: Intracellular Fluid
Can't be measured directly
ICF = TBW – ECF
how to measure body fluid compartments: Plasma
125I-albumin, Evan's Blue dye
how to measure body fluid compartments: Interstitial Fluid
Can't be measured directly
ISF = ECF – plasma
other fluid compartments
Lymph
Bone and dense connective tissue fluids
Transcellular fluid
other fluid compartments: Lymph
Component of interstitial fluid
other fluid compartments: Bone and dense connective tissue fluids
~ 15% of total body water
other fluid compartments: Transcellular fluid
Fluids contained completely within epithelial-lined spaces
Synovial (joints), intrapleural, aqueous humor, peritoneal
OR
‘Functional’ ECF
Cerebrospinal fluid, saliva, GIT secretions, sweat
Fluid ‘spaces’: First space
Intravascular fluid (plasma)
Fluid ‘spaces’: Second space
Interstitial and Intracellular fluid
Edema is accumulation in second space (interstitial)
Fluid ‘spaces’: Third space
Fluid compartments not easily exchanged with ECF
Peritoneum
Intrapleural
Patients with severe burns will often have ‘third spacing’ where fluid accumulates at the burn site, outside of interstitial fluid
ascites
Peritoneum Fluid accumulation
pleural effusion
Intrapleural Fluid accumulation
Ions balanced between ECF and ICF
Sodium is major cation in ECF
Balanced with chloride and bicarbonate
Potassium is balanced with organic ions and proteins
Fluid losses
Sweat
Insensible water loss
Gastrointestinal secretions
Fluid losses: Sweat
Variable: water loss of 100 – 8,000 mL/day
Fluid losses: Insensible water loss
800 mL/day
Through skin (trans-epithelial) as well as through the respiratory tract
Cannot be prevented
Fluid losses: Gastrointestinal secretions
98% of water from secretions is reabsorbed
200 mL H2O lost in feces
Important factors in fluid balance
Osmolarity
Osmolality
Hydrostatic Pressure
Sodium balance
Water balance
Osmolarity VS Osmolality
Osmolarity = osmoles/L solution
Osmolality = osmoles/kg H2O
Similar (interchangeable) in dilute physiological solutions
Hydrostatic Pressure
pressure that pushes fluid through
caused by plasma proteins → main reason for oncotic pressure
Sodium balance
Primary osmolite in the ECF
Water + sodium balance
Together maintain ECF volume and osmolarity
Fluid exchange occurs at
capillaries
Capillaries
consist of single layer of endothelial cells surrounded by basement membrane
Endothelial cells linked together by interendothelial junctions
Adhering junctions or tight junctions
Effect of inflammation on capillary leakiness
Endothelial tight junctions regulated by a variety of signaling mechanisms
Cytokines, extracellular calcium, G proteins, etc.
E.g.: Histamine causes transitory gaps of 100 to 400 nm between adjacent endothelial cells
Increased endothelial permeability due to inflammatory response
Cytoskeletal contractility can change the shape of cells and pull individual endothelial cells apart
Breakdown or modulation of the intercellular junctions
Capillary exchange of solutes: transcellular
Gases and other small non-polar molecules
Capillary exchange of solutes: water-filled pores
Small, polar molecules can only traverse through water-filled pores
Low permeability
Capillary exchange of macromolecules
Molecules with a radius >1 nm (e.g., plasma proteins)
Cross through wide intercellular clefts, fenestrations, and gaps (when present and large enough)
Caveolae
Caveolae
facilitate transcytosis of macromolecules across endothelial cell
Capillary exchange of water
Fluid transfer across capillaries is convective
Through aquaporins and interendothelial clefts
Depends on net hydrostatic and osmotic forces
Plasma osmotic pressure “pulls” fluid back into capillary
Much higher in capillary due to plasma proteins
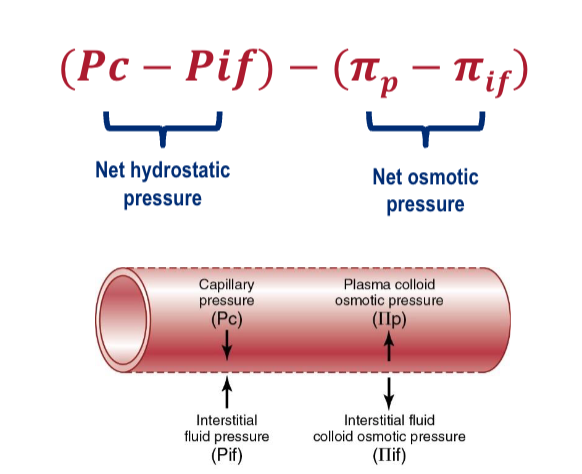
Starling forces
At arterial end, hydrostatic pressure exceeds other forces → Favors filtration
At venous end, capillary oncotic pressure exceeds → Favors reabsorption
Regulation of Extracellular fluid (2 ways)
Fluid movement between ECF and ICF is passive
Therefore, ECF must be tightly regulated
Two ways:
ECF fluid osmolarity is regulated by changing the amount of water
ECF fluid volume is regulated by changing the amount of sodium
These two operate in tandem, but have some distinctions
Two mechanisms for sensing fluid abnormalities
1) Baroreceptors
2) Osmoreceptors
Two mechanisms for sensing fluid abnormalities: 1. Baroreceptors
Respond to increased hydrostatic pressure due to increased blood volume
Regulate sodium
Two mechanisms for sensing fluid abnormalities: 2. Osmoreceptors
Respond to the osmolarity of the ECF
Regulate water
The primary osmoreceptors are located in:
1. Medullary collecting duct of kidney
2. Aortic arch
3. Hypothalamus
4. Lungs
3. Hypothalamus ADH
Mechanisms for regulating plasma volume
Renin-Angiotensin-Aldosterone (RAAS)
Atrial Natriuretic Peptide (ANP)
Anti-diuretic hormone (ADH)
Mechanisms for regulating plasma volume: Renin-Angiotensin-Aldosterone (RAAS) effects + mechanism
Aldosterone causes Na+ to be reabsorbed
in response to low blood pressure (stimulus), low ECF volume kidney secretes renin → converts angiotensinogen to angiotensin 1 → ACE converts angiotensin 1 to angiotensin 2
angiotensin 2
causes massive vasoconstriction
causes aldosterone to be released from the adrenal cortex
aldosterone
acts on kidneys to increase the amount of sodium that is absorbed back into the blood → ECF + blood pressure increase
Mechanisms for regulating plasma volume: Atrial Natriuretic Peptide (ANP) effects
Opposite” hormone to aldosterone
↑BP stimulates release from atria
Causes excretion of sodium and water.
Mechanisms for regulating plasma volume: Anti-diuretic hormone (ADH) effects
AKA Arginine Vasopressin
Vasoconstriction + Increased H2O reabsorption
where is ADH synthesized
in the hypothalamus
where + when is ADH released?
Release from posterior pituitary is increased by:
High plasma osmolarity (MAIN)
Low central blood volume
Alterations in sodium and water balance (3 types)
Isotonic alterations
hypertonic alterations
hypotonic alterations
Alterations in sodium and water balance: Isotonic alterations
Gain or loss of ECF volume but osmolarity is normal (280-294 mOm)
Isotonic fluid loss or isotonic fluid excess
Isotonic alterations: Isotonic fluid loss (results in, caused by, treated with)
Results in dehydration and hypovolemia
Caused by hemorrhage, diaphoresis (sweating), inadequate fluid intake
Treated with 0.9% NaCl (i.v. fluids)
Isotonic alterations: Isotonic fluid excess (results in, caused by, treated with)
Results in increased BP, pulmonary edema, heart failure
Caused by excessive iv. fluid administration, abnormal aldosterone secretion
Treated with diuretics
Alterations in sodium and water balance: Hypertonic alterations Consequence
Osmolarity of ECF greater than normal
Hypernatremia → Cell Shrinkage
Hypernatremia is caused by
Loss of H2O: hyperosmotic dehydration
OR
Gain of NaCl: hyperosmotic overhydration
Hypertonic alterations: hyperosmotic dehydration
Loss of H2O
Most common – could result from vomiting, diarrhea, inadequate water intake
Diabetes insipidus – lack of ADH
Hypertonic alterations: hyperosmotic overhydration
Gain of NaCl
Rare – results from oversecretion of aldosterone or hyperosmotic iv. fluid
Rarely due to excess salt consumption in healthy individuals
Alterations in sodium and water balance: Hypotonic alterations types + Consequence
Osmolarity of ECF below normal
Hyponatremia → Cell Swelling
Hyponatremia is caused by
Loss of Na without loss of water: hypoosmotic dehydration
OR
Loss of water, but greater loss of Na
OR
Gain of pure water: hypoosmotic overhydration (water intoxication)
Hypotonic alterations: hypoosmotic dehydration
Loss of Na without loss of water
Syndrome of inappropriate ADH (SIADH)
Rarely due to low-sodium diet
Hypotonic alterations: Loss of water, but greater loss of Na
Adrenal insufficiency (aldosterone deficiency)
Hypotonic alterations: hypoosmotic overhydration (water intoxication)
Gain of pure water
Interstitial ‘Gel fluid’
resists volume change
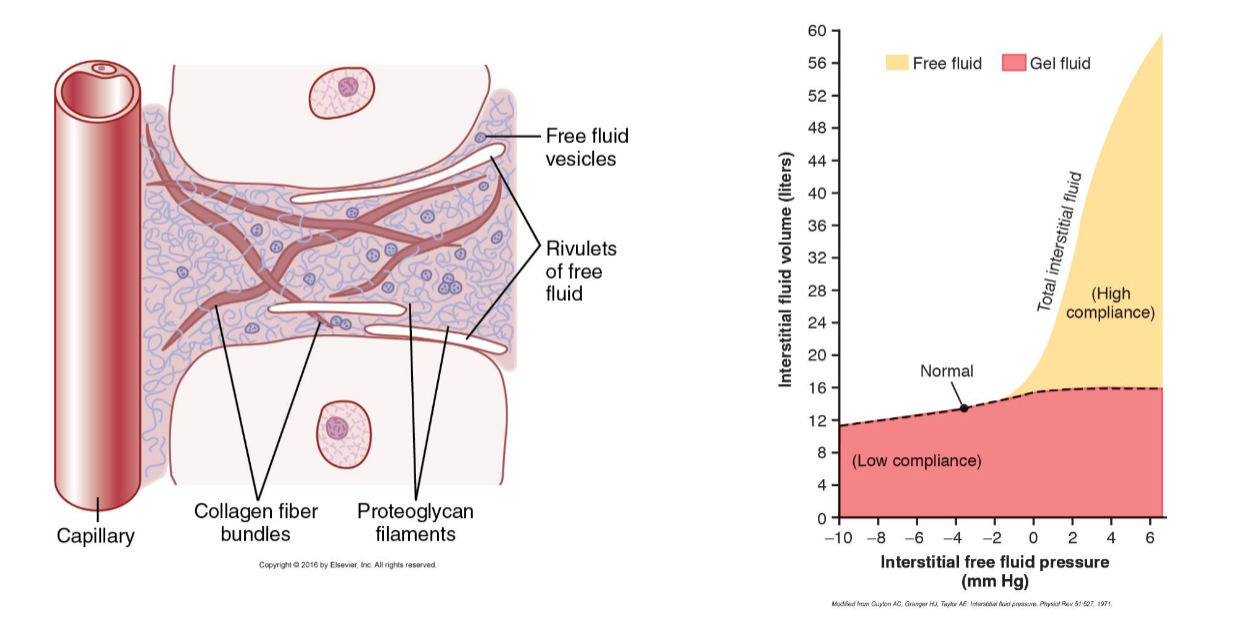
Interstitium
Fluid-filled interstitial space identified because of improved fixation and microscopy techniques
In dermis and many submucosal tissues
“Pre-lymph
Lymphatic circulation
Filtration at capillaries exceeds absorption by ~ 2 L per day
Lymphatics remove excess fluid and protein from interstitium
Keeps interstitial colloid pressure low
Drains back into circulation at inferior vena cava
Flow into lymphatics
Lymphatic capillaries are a type of ‘pressure release valve’
Series of one-way valves ensures lymph moves in one direction only
Edema
excess fluid in body tissues
Intracellular edema causes
Intracellular edema is particularly problematic for CNS
Hyponatremia
Reduced tissue metabolism or lack of nutrition
Na-K pump slows and Na+ builds up inside cell (water follows)
Inflammation → Increases membrane permeability
Extracellular edema causes
most common
Increased capillary pressure
Decreased plasma proteins
Increased capillary permeability
Blockage of lymph return
Increased capillary filtration is caused by
Increase filtration coefficient
Increase hydrostatic pressure
Decrease colloid osmotic pressure
Extracellular edema causes: Increased capillary pressure
leads to increased hydrostatic pressure
Increased blood volume (hypernatremia)
High venous pressure
due to Heart failure or venous obstruction/failure
Decreased arteriolar resistance
due to Impaired sympathetic nervous system or vasodilator drugs
Extracellular edema causes: Decreased plasma proteins
leads to decrease in colloid osmotic pressure
Loss of proteins in urine
Liver failure
Extracellular edema causes: Increased capillary permeability
leads to increase filtration coefficient
Immune reactions
Bacterial infections/toxins
Extracellular edema causes: lymphedema
Failure of lymphatic system → blockage of lymph return
Cancer or infection
Surgery or congenital absence
Which of the following are forces that favor filtration in
systemic capillaries? (Check all that apply)
1. Capillary hydrostatic pressure
2. Interstitial fluid hydrostatic pressure
3. Plasma osmotic pressure
4. Interstitial fluid osmotic pressure
1. Capillary hydrostatic pressure
2. Interstitial fluid hydrostatic pressure