Pharmacology of Benzodiazepines, Z drugs, and Barbiturates
1/169
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
170 Terms
What is sedation?
a state of reduced tension and anxiety
What does it mean if a drop is hypnotic?
It induce drowsiness and sleep
What is the difference in newer drugs (benzodiazepines and modern hypnotics) compared to older hypnotics (barbiturates and others) in regards to their dose-response curve.
Newer hypnotic drugs level off eventually requiring more drug to achieve a state beyond the hypnotic effect.
Older hypnotic drug and barbiturates do not level off. These drugs see a dose-dependent increase in effect reaching past hypnosis into coma.
What is the benzodiazepine ceiling effect?
increasing the dose of a benzodiazepine does not produce additional therapeutic benefits or greater CNS depression beyond a certain point. (unless combined with other substances)
What are the three classes of sedative-hypnotic drugs we focus on?
Benzodiazepines (BZDs)
Benzodiazepine-receptor agonists (these are newer, referred to as “Z” drugs)
Barbiturates
What are the three Z drugs we focus on?
Zolpidem
Zaleplon
Eszopiclone
True or False: All BZDs cross the placental barrier and can be detected in breast milk?
True
What is the general absorptivity of BZDs?
BZDs tend to be well absorbed in the GI. Higher lipophilicity relates to greater absorption and brain access.
What CYP are most benzodiazepines metabolized by?
Most BZDs are CYP3A4 metabolized
Are BZD metabolites generally active or inactive?
BZDs are metabolized via phase one reactions into pharmacologically active intermediates.
What is the difference between phase one metabolism of BZDs and Z drugs?
BZDs are metabolized into active products, whereas Z drugs are inactivated when metabolized in phase one.
What effect do barbiturates have on CYPs?
Barbiturates are strong inducers of multiple CYPs.
What subunits of GABAA- receptors can BZDs bind to?
BZDs will Bind to a1,2,3,5 subunits.
What GABAA receptor subunits can Z drugs bind to?
Z-drugs will only bind to GABAA receptors that contain alpha-1 subunits.
What effect do BZDs have on GABAA receptors?
These drugs act as positive allosteric modulators/ potentiators. They increase the frequency of channel-opening events.
What effect do barbiturates have on GABAA receptors?
These drugs increase the duration of GABA-gated chloride channel openings.
They act allosterically.
What effect do barbiturates have on GABA receptors at high doses that results in these drugs not having a ceiling?
At high doses, these drugs can act as GABA-mimetics and directly activate chloride channels.
They can also effect other receptors at high doses:
Barbiturates can also depress actions of excitatory glutamate receptors by binding to AMPA receptors.
What ligands can bind to the GABAA receptor?
Agonists
BZDs, Z drugs
Antagonists
flumenazil
Inverse agonists
Carbolines
What is the role of flumenazil?
Flumenazil binds to GABAA and prevents the binding of BZDs and Z drugs to activate the receptor.
How do some BZDs (such as diazepam) and barbiturates achieve anticonvulsive effects?
Anticonvulsive effects are achieved via inhibition of epileptiform electrical activity without pronounced CNS depression.
What characteristics of sedative-hypnotic drugs do Z-drugs lack?
Z-drugs do not have anti-convulsive effects.
Z-drugs do not have muscle relaxation effects
Why do Z-drugs lack certain BZD effects?
Z-drugs only bind to GABAA receptors that contain alpha-1 subunits.
BZDs bind to a wider range (alpha-1,2,3,5) of subunits, owing to a wider array of effects.
What effect do sedative-hypnotic drugs have on the respiratory system?
overall depression of respiration function
mostly pronounced in patients with pulmonary disease
Depression of medullary respiration center is the usual cause of death in overdoses of sedative-hypnotic drugs.
What effect do sedative-hypnotic drugs have on the CVS?
pronounced depression in patients with CV disease
at toxic doses, depression of contractility and vascular tone leads to circulatory collapse.
inhibitory action upon medullary vasomotor centers
What effect do BZDs and older hypnotic drugs have on sleep?
decreased latency of sleep onset
increased duration of stage 2 NREM
will not feel well rested.
decreased duration of REM
results in a need for rebound sleep
decreased duration of deep sleep (stage 4 NREM)
What effect do newer hypnotics (z drugs) have on sleep?
decreased latency to fall asleep
decreased affect on REM and stage 4 NREM at therapeutic doses compared to BZDs
What is tolerance?
decreased responsiveness to a drug after repeated administration
What kind of tolerance to BZDs exhibit between each other?
There is a partial cross-tolerance between different kinds of BZDs.
If you develop tolerance to one BZD you may have some tolerance to another BZD.
what is psychological dependence?
characterized as addiction. compulsive use of a substance.
What is physiological dependence?
taking a substance to prevent the withdrawal symptoms
What are some side effects of BZDs?
motor incoordination
impairment of mental functions
confusion
anterograde amnesia
What increases the risk of impaired driving with BZD use?
Ethanol usage combined with BZDs increases risk of driving impairment.
What kind of agonist is flumazenil?
Flumazenil is a competitive antagonist which binds with high affinity to BZD site on GABAA
What is flumazenil used for?
reversing the CNS depressive effects of BZD overdose
Speeding up recovery following the use of BZDs and Z-drugs as anesthetics.
What is thiopental? What is it used as? Why?
Thiopental is a barbiturate. This drugs has a very short action of effect, and is used as an intravenous anesthetic.
What is phenobarbital used for?
it is used as an anticonvulsive drug
What are ramelteon and tasimelteon?
These drugs are used to induce sleep. They are MT1 and MT2 (melatonin) receptor agonists.
These drugs have no effect on GABA neurotransmission
What are the benefits of ramelteon and tasimelteon?
Reduced sleep latency with
no effect on sleep architecture
no rebound insomnia
no significant withdrawal symptoms
What is buspirone?
a slow-onset anxiolytic drug
What receptors does Buspirone target?
Buspirone targets HT1A and D2 receptors
What are benefits of using Buspirone?
does not caused hypnotic or euphoric effects
produces less psychomotor impairment compared to BZDs
Does not potentiate effects of sedative-hypnotic drugs
does not cause rebound anxiety or withdrawal
What are the molecular targets of the following:
Flumazenil
Oxazepam
Ramelteon
Thiopental
Flumazenil targets GABAA alpha-1 subunits
Oxazepam targets alpha-1 GABA subunits
Ramelteon targets MT1 and MT2 receptors
Thiopental (barbiturate) targets GABA alpha-1,2,3,5 subunits.
What are the two divisions of the peripheral nervous system?
Sensory (afferent (away from extremities))
Motor (efferent)
What are the two divisions of the motor nervous system?
autonomous and somatic
What are the two divisions of the autonomic nervous system?
sympathetic and parasympathetic
How do the lengths of pre-ganglionic neurons compare between the sympathetic and parasympathetic nervous system?
Pre-ganglionic neurons of the Sympathetic Nervous System are short compared to their post-ganglionic neurons
The parasympathetic nervous systems synapse with the ganglia much closer to the target organ. Resulting in long pre-neurons and short post-neurons.
What is the primary neurotransmitter and receptor for autonomic ganglia?
Acetylcholine as the neurotransmitter, and nicotinic receptors
What is the other name for the sympathetic nervous system?
the thoracolumbar division
What is the other name for the parasympathetic nervous system?
the craniosacral division
What are the two kinds of sympathetic preganglionic fibers?
Paravertebral ganglia and prevertebral ganglia
What is characteristic of paravertebral ganglia?
these chains lie on either side of the spinal column
most sympathetic ganglia are these
What is characteristic of prevertebral ganglia?
these chains lie in front of the vertebrae
Where do parasympathetic preganglionic fibers originate?
mostly in the brainstem and sacral spinal cord
Where do parasympathetic fibers terminate?
in or near the wall of innervated organs (most)
in parasympathetic ganglia located outside of the innervated organs.
What kind of fibers (cholinergic or adrenergic) are all preganglionic efferent, autonomic fibers?
All of these fibers are cholinergic.
What do most sympathetic, postganglionic fibers synthesize and secrete?
most of these neurons produce and secrete norepinephrine (adrenergic)
What is an example of sympathetic innervation via acetylcholine?
sweat glands are innervated by sympathetic cholinergic fibers
What do dopaminergic fibers innervate?
These fibers innervate renal vascular smooth muscle
What kind of fibers innervate somatic muscle?
skeletal muscle is innervated by cholinergic post-ganglionic fibers
What toxin can block the vesicle release process of acetylcholine?
botulinum toxin
What is the half life of acetylcholine?
<1/2 a second
What enzyme converts tyrosine to Dopa?
tyrosine hydroxylase (rate limiting step)
What drug can block VMAT transporters that move dopamine into transport vesicles?
reserpine
What transporters allow for the reuptake of norepinephrine?
NET (norepinephrine transporter)
What drugs may block norepinephrine reuptake transporters (NET)?
cocaine and tricyclic antidepressants
What are two enzymes involved in catecholamine degradation?
Monoamine oxidases and Catechol-o-methyltransferase (COMT)
What is the signaling type of M1,3,5 receptors?
These muscarinic receptors operate via IP3/DAG pathways and an increase of intracellular calcium (generally excitatory)
What is the signaling type of M2,4 receptors?
These muscarinic receptors operate via opening K+ channels and inhibiting adenylyl cyclase (Generally inhibitory)
Where are M2 muscarinic receptors found?
myocardium, smooth muscle, some presynaptic sites, CNS neurons
Where are M1 receptors found?
CNS neurons, sympathetic postganglionic neurons, some presynaptic sites.
Where are M3 receptors found?
exocrine glands, smooth muscle and endothelium of blood vessels, CNS neurons
Where are M4 receptors found?
CNS neurons, possibly vagal nerve endings
Where are M5 receptors found?
vascular endothelium (cerebral vessels), CNS neurons
What is the result of ligand binding in adrenoreceptors?
most adrenoreceptors trigger GPCR pathways
What is the affect of stimulation of Dopamine 1 and 5 receptors?
stimulation of adenylyl cyclase and increased cAMP (Gs)
What is the affect of stimulation of Dopamine 2,3,4 receptors?
Gi coupled responses. inhibition of adenylyl cyclase.
What additional affect does dopamine D2 have?
increased potassium conductance
What are the main types of adrenergic receptors? Explain their signaling mechanism.
adrenergic receptors tend to be alpha or beta receptors, or dopamine receptors. These tend to operate via Gi or Gs related GPCR pathways.
What are the main types of cholinergic receptors? Explain their signaling mechanisms.
cholinergic receptors are either muscarinic or nicotinic in nature and respond by altering cellular concentrations of ions
opening sodium or potassium channels
increasing cellular calcium levels
Which fibers are cholinergic fibers?
sympathetic and parasympathetic preganglionic fibers
almost all parasympathetic post-ganglionic fibers
sympathetic fibers that innervate sweat glands
motor neurons
What are cholinoreceptor-activating drugs?
These drugs, also known as direct-acting cholinomimetics, directly stimulate muscarinic or nicotinic receptors
What are cholinesterase-inhibiting drugs?
These drugs, also known as indirect-acting cholinomimetics operate by decreasing the activity of ACHE thus increasing the effective half life of acetylcholine.
What is the other name for M2 receptors? Where are they predominantly found?
these receptors may also be known as Cardiac M2 receptors and are found on the SA/AV node.
What are the four kinds of covered choline-esters of direct-acting cholinomimetics?
acetylcholine
methacholine
carbachol
bethanechol
What are the three kinds of covered alkaloids of direct-acting cholinomimetics?
muscarine
nicotine
pilocarbine
What component of bethanechol and methacholine make them selective for muscarinic receptors?
these two compounds contain a beta methyl group that increases selectivity for muscarine receptors
What is the affect of the carbamyl group on carbachol and bethanechol?
the added carbamyl group is stronger than the normal ester of ACH and thus these compounds will not be acted upon by ACHE
Of the choline-esters, rank them from most to least susceptible to hydrolysis.
acetylcholine > methacholine > carbachol > bethanechol
Are alkaloids susceptible to ACHE? Why or why not?
Alkaloids are not susceptible to hydrolysis because they lack an ester group.
What kind of cholinergic receptors do pilocarpine and muscarine activate?
These compounds specifically activate muscarinic receptors
What kind of receptors does atropine antagonize?
muscarinic receptors are blocked by atropine

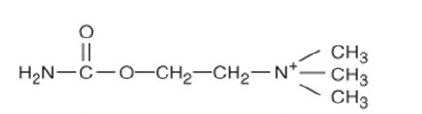
Is this drug a nicotinic receptor agonist, muscarinic receptor agonist, and/or cleaved by ACHE? What is the name of this drug.
This compound is acetylcholine. It can activate both muscarinic and nicotinic receptors and is highly susceptible to acetylcholine esterase.
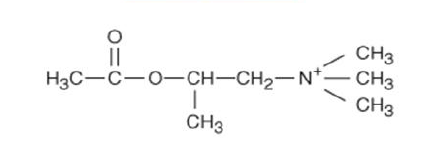
Is this drug a nicotinic receptor agonist, muscarinic receptor agonist, and/or cleaved by ACHE? What is the name of this drug.
This drug is carbachol. It is a nicotinic and muscarinic agonist. It is not cleaved by acetylcholine esterase.
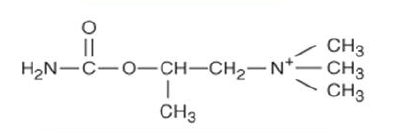
Is this drug a nicotinic receptor agonist, muscarinic receptor agonist, and/or cleaved by ACHE? What is the name of this drug?
This drug is methacholine. It is a selective agonist for muscarinic receptors and is cleaved by acetylcholine esterase
Is this drug a nicotinic receptor agonist, muscarinic receptor agonist, and/or cleaved by ACHE? What is the name of this drug?
This drug is bethanechol. It is a selective muscarinic agonist and is not susceptible to acetylcholine esterase.
What other nervous stimulation do muscarinic receptors mimic?
Muscarinic effects are most similar to those of the parasympathetic nervous system.
What effects on the eye does stimulation of muscarinic receptors trigger?
miosis (constriction of the pupil)
reduction of intraocular pressure
accommodation for near vision.
What effect, in general, do muscarinic agonists have on the cardiovascular system?
reduction in peripheral vascular resistance (vasodilation)
reduction in heart rate
What effect does muscarinic stimulation of SA and AV nodes have on heart rate?
Stimulation of the SA and AV node by M2 receptors and parasympathetic vagal fibers results in an overall decrease in heart rate.
has little effect on contractile strength, mostly affects rate of contraction.