all bbl
1/783
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
784 Terms
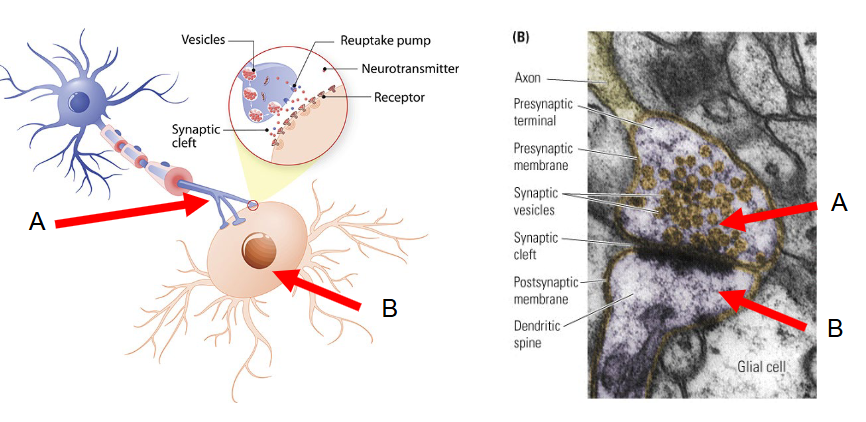
How do Neurons communicatie?
Through synapses.
Neuron A = presynaptic (sender)
Neuron B = postsynaptic (receiver)
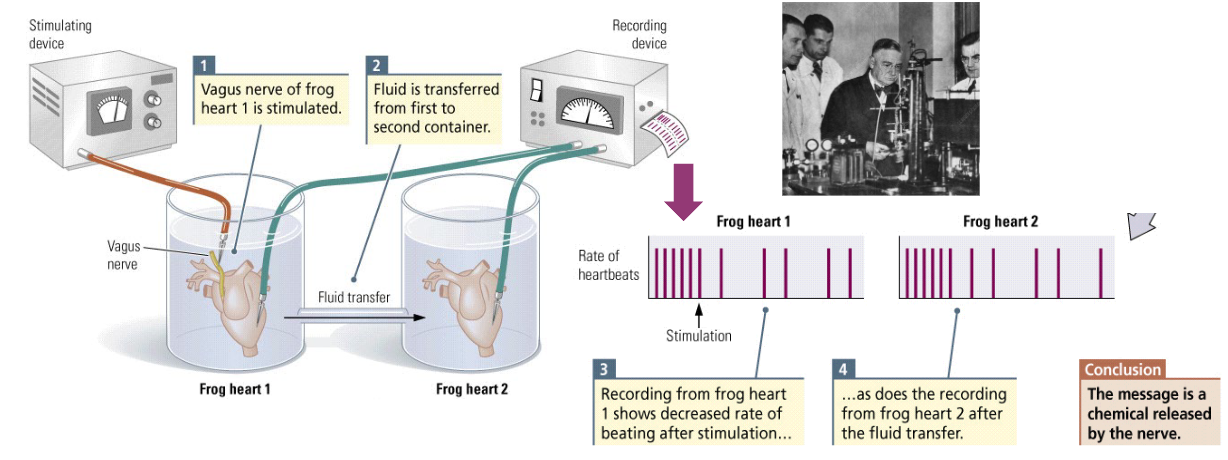
What is the conclusion of Loewi’s experiment?
Transmission of information between neurons happens chemically (de rest is niet belangrijk voor examen).
The chemical messenger is later identified as Acetylcholine (Ach).
What is Acetylcholine (Ach)?
The chemical messenger between two vessels. This chemical appears to activate skeletal muscles in the somatic nervous system, and to excite or inhibit internal organs in the autonomic nervous system.
What is Epinephrine (EP)?
aka. Adrenaline; speeds up the heartbeat.
What is Norepinephrine (NE)?
aka. Noradrenaline; a chemical messenger that increases heart rate in mammals.
What are Neurotransmitters?
Chemical messengers that are released by a neuron on a target to cause an excitatory or inhibitory effect.
Outside the CNS, many of these chemicals circulate through the blood as hormones.
The presynaptic neuron secretes a chemical into the synaptic clef (the neurotransmitter), which then binds to the postsynaptic receptors on the postsynaptic membrane.
What is the difference between Neurotransmitters and Hormones?
The distance they travel before they reach their receptors; Hormones travel longer distances, so their effects are slower.
What is Parkinson’s disease?
A disease of the motor system associated with a loss of substantia nigra neurons, which contain dopamine, and is characterized by tremors and reduction of voluntary movement.
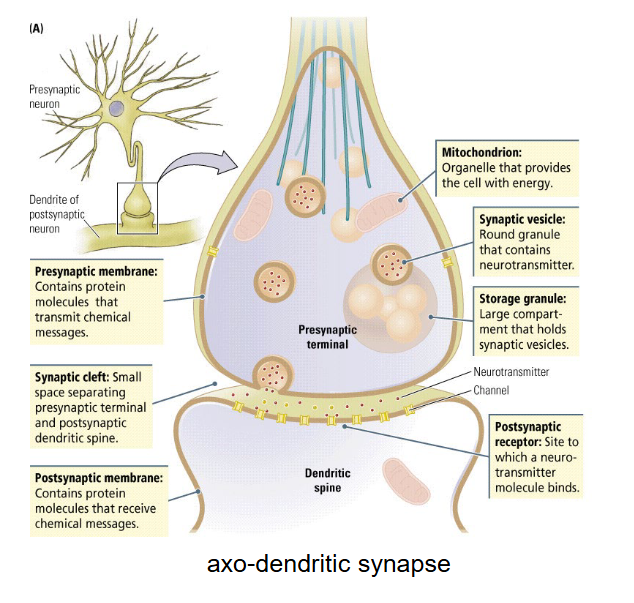
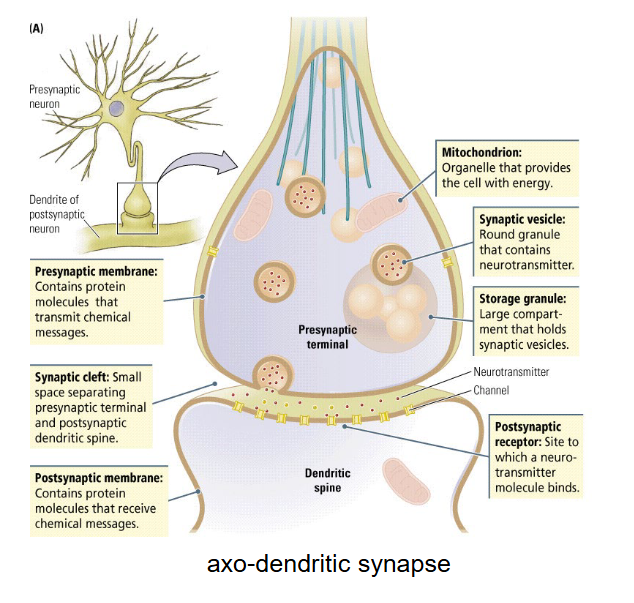
What do Synapses consist of?
Presynaptic terminal button (terminal of an axon)
Synaptic cleft (place where neurotransmitters are released)
Postsynaptic membrane (target)
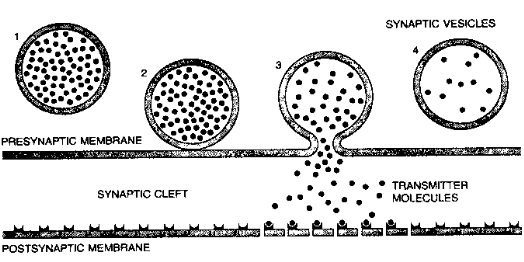
What happens when a neurotransmitter is released?
An action potential generated by the presynaptic neuron leads to exocytosis of a neurotransmitter from the presynaptic terminal button into the synaptic cleft.
What happens when the neurotransmitter binds to the postsynaptic membrane?
It will cause a change in the resting potential of the postsynaptic neuron (EPSP or IPSP).
What are Synaptic vesicles for?
They contain the neurotransmitters in the presynaptic cell.
What is a Quantum?
The number of neurotransmitter in each vesicle (content of 1 synaptic vesicle).
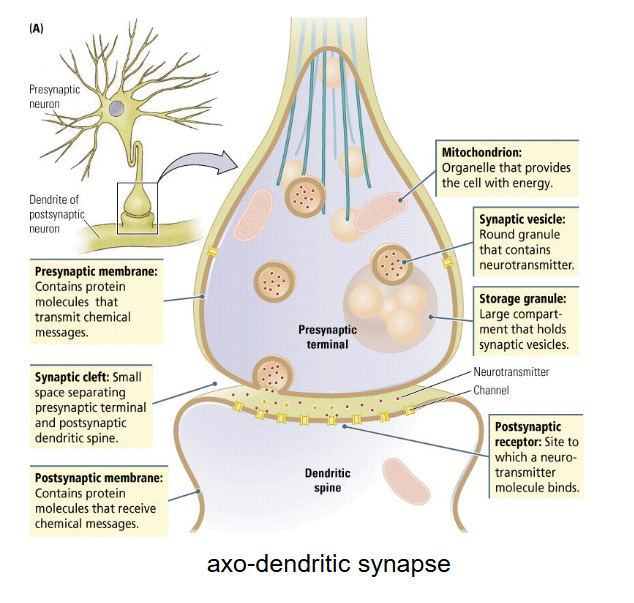
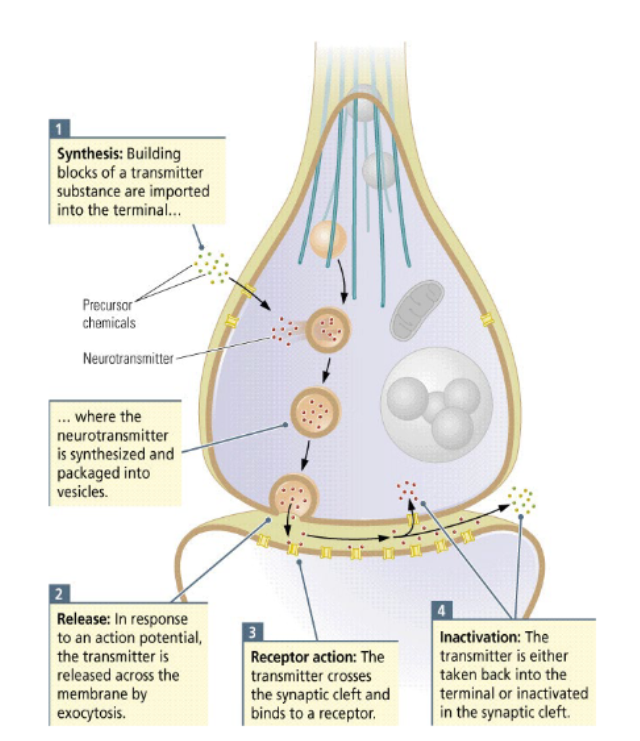
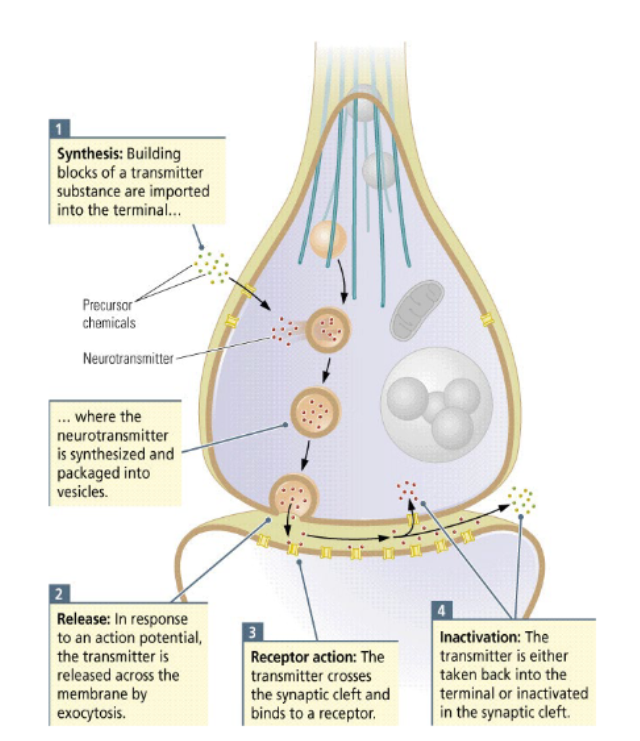
In what 5 steps can Neurotransmission be described?
Synthesis: the neurotransmitter is synthesized somewhere in the neuron.
different types of neurotransmitters are synthesized in different ways.
ex. peptide transmitters are synthesized in the cell body (DNA, mRNA), through transcription and translation (like protein synthesis).
small-molecule transmitters are synthesized directly in the axon terminal, using food-derived substances.
Packaging + Storage: the synthesized neurotransmitters are packaged and stored in vesicles.
Release: the vesicles containing neurotransmitters dock near release sites on the presynaptic membrane.
Receptor action at the postsynaptic membrane: neurotransmitters that are released into the synaptic cleft reach the postsynaptic membrane, where they bind to its transmitter-activated receptors.
the effect of neurotransmitters on the postsynaptic cell depends on the type of receptor.
in general, there can be an excitatory effect (the cell is brought closer to the firing threshold) or an inhibitory effect (the cell is brought further away from the firing threshold).
Inactivation: neurotransmitters must be inactivated after they have done their work.
if neurotransmitters remained in the synaptic cleft indefinitely, they would continue to bind to receptors, so the cell could not respond to new signals.
What happens during the Release step of Neurotransmission?
The vesicles containing neurotransmitters dock near release sites on the presynaptic membrane.
Many voltage-activated calcium (Ca2+) channels are embedded in the presynaptic membrane.
When an action potential reaches the membrane, it opens the voltage-sensitive calcium channels, enabling an influx of calcium ions into the terminal button.
The incoming calcium ions form a complex that binds to vesicles, triggering the release of neurotransmitters into the synaptic cleft.
The amount of neurotransmitter released depends on the amount of Ca entering the axon terminal, and the number of vesicles docked at the membrane.
Many quanta are needed to induce action potential at the postsynaptic cell.
What are the 3 steps of Neurotransmitter release?
When an action potential reaches the voltage-sensitive terminal, it opens calcium channels.
Incoming calcium ions bind to calmodulin, forming a complex.
This complex binds to vesicles, releasing from filaments and inducing others to bind to the presynaptic membrane and to empty their contents by exocytosis.
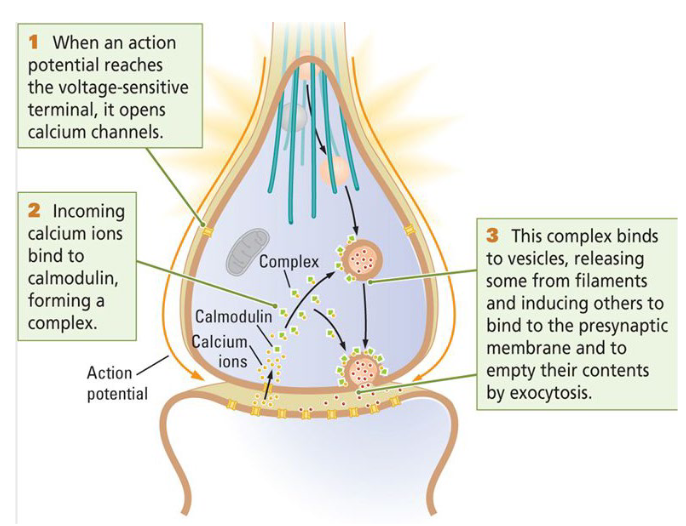
What does the amount of Neurotransmitters that are released depend on?
The amount of Calcium entering axon terminal.
Number of vesicles docked at the membrane.
Many quanta are needed to induce action potential at postsynaptic cell.
What are the 4 steps of Synaptic transmission?
Synthesis & packaging
cell body (DNA, mRNA)
axon terminal (precursor chemicals derived from food)
Release
Calcium influx triggered by action potential
release into synaptic cleft (exocytosis)
Receptor action at postsynaptic membrane
depolarization (excitation)
hyperpolarization (inhibition)
modulation (inhibit or excite other chemical reactions)
Inactivation
diffusion away from synaptic cleft
degradation by enzymes
reuptake in presynaptic cell (these neurotransmitters are picked up by the presynaptic membrane and reused).
uptake by glial cells (astrocytes)
What is a Synapse?
An area where two neurons come close enough to one another that they are able to pass chemical signals from one cell to another.
What are the 4 ways in which Inactivation occurs?
Diffusion
Neurotransmitters diffuse away from the synaptic cleft towards areas of lower concentration.
Degradation
Neurotransmitters are broken down by enzymes.
Reuptake
Neurotransmitters (and/or the residues of their enzyme degradation) can return to the presynaptic cell, where they can be reused.
Astrocyte uptake
Neurotransmitters can be taken up by astrocytes, which can then provide them once again to the presynaptic cell.
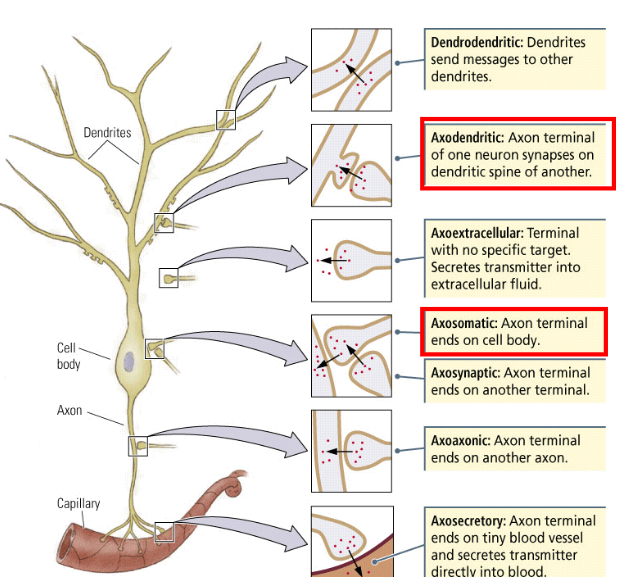
What are the two different types of synapses we need to know?
Axo-dendritic (from axon to dendrite)
Axo-somatic (from axon to cell body)
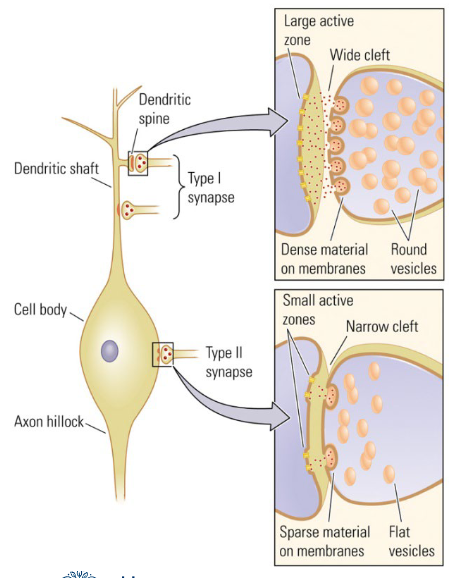
What is the difference between Excitatory and Inhibitory synapses?
Excitatory
at dendrites (on top)
round vesicles
high density (both pre- and postsynaptical)
wide synaptic cleft
large active zone
they need a lot of power to counteract the distance from the axon hillock and the action of inhibitory synapses.
Inhibitory
at cell body — soma (axon)
because the closer they are to the initial segment on the axon hillock, the better they can stop the firing of an action potential.
flat vesicles
low density (both pre- and postsynaptical)
narrow synaptic cleft
small active zone
NB: Neurotransmitters themselves do not determine excitation or inhibition.
Do Neurotransmitter determine excitation or inhibition?
NO; the postsynaptic membrane decides whether there is excitation or inhibition.
The gates where neurotransmitters travel through, is either positively or negatively charged.
Neurotransmitters are just messengers.
What does an Excitatory effect do?
It brings the cell closer to the firing threshold, thus making it more likely to fire an action potential.
What does an Inhibitory effect do?
It brings the cell further away from the firing threshold, thus making it less likely to fire an action potential.
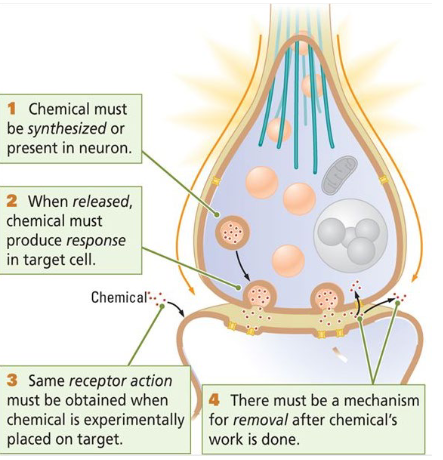
What are the 4 ‘classical’ identifying criteria to determine whether a chemical substance is a neurotransmitter?
The transmitter…
Must be synthesized or be present in the neuron.
Must be released and produce an effect when the neuron is active.
Must produce the same effect when experimentally place don the target.
There must be a mechanism for removing the transmitter after its effect.
What are Putative neurotransmitters?
The substances that do not meet the requirements to determine whether a chemical is a neurotransmitter.
Putative = supposed.
What do ‘classical’ neurotransmitters do?
They cause a potential difference at the postsynaptic membrane (EPSP, IPSP).
The term ‘neurotransmitter’ is used more broadly now. To what chemicals does this apply?
To chemicals that:
change the structure of the synapse.
are transmitted from post- to presynaptic membranes.
retrograde messages (move in opposite direction).
only work in combination with other substances (cocktail).
function as a neurotransmitter and as a hormone.
What are the five Classifications of neurotransmitters?
(based on chemical composition)
Small-molecule transmitters
Peptide transmitters
Lipid transmitters
Gaseous transmitters (not required for exam)
Ion transmitters (not required for exam)
What are the 4 most important small-molecule transmitters in the central nervous system?
Acetylcholine (ACh)
Dopamine (DA)
Norepinephrine (NE) = Noradrenaline
Serotonin (SE)
What are Small-molecule transmitters?
These are small molecules that are synthesized in the axon terminal from food-derived nutrients and are ready for use. Once they have been released in the synaptic cleft, they can be replaced quickly at the presynaptic membrane.
What are Peptide transmitters?
= Neuropeptides: these are chains of amino acids that function as neurotransmitters.
They are synthesized through DNA/mRNA transcription and translation.
Typically, they are synthesized in the cell body and are transported to the axon terminal by microtubules.
So, they are slow and not quickly replaced.
What are Lipid transmitters?
The main lipid transmitters are cannabinoids, which can be either generated by the body (endocannabinoids) or by plants (phytocannabinoids).
Endocannabinoids are synthesized at the postsynaptic membrane, where they are derived from arachidonic acid (found in poultry and eggs).
They are synthesized on demand, rather than stored in vesicles, so their effect is slow.
All cannabinoids act on the CB1 receptors on the presynaptic membrane (retrograde neurotransmitters).
They affect many processes, such as appetite, pain, sleep, mood, memory, anxiety, and stress responses.
They act as neuromodulators, by inhibiting the release of both GABA and glutamate, and thus dampening both inhibitory and excitatory neural activity.
What is the Small-molecule transmitter Acetylcholine synthesized from?
From acetate (vinegar, lemon juice) + choline (egg yolk, avocado, salmon, olive oil) by enzymes.
Is found at the junction between neurons and muscles, as well as in the CNS.
What is the Small-molecule transmitter Serotonin synthesized from?
From L-tryptophan (pork, turkey, milk, peanuts, bananas).
It regulates mood and aggression, appetite and arousal, respiration and pain perception.
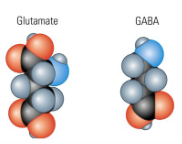
What is the Small-molecule transmitter GABA synthesized from?
It is formed by a simple modification of the glutamate molecule (Parmesan cheese, seaweed, miso soup, mushrooms).
in forebrain and cerebellum: Glutamate main excitatory & GABA main inhibitory transmitter
in brainstem and spinal cord: Glycine more common inhibitory transmitter.
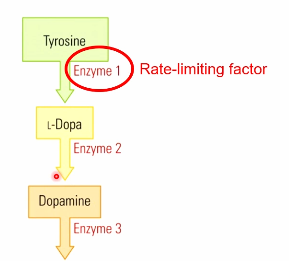
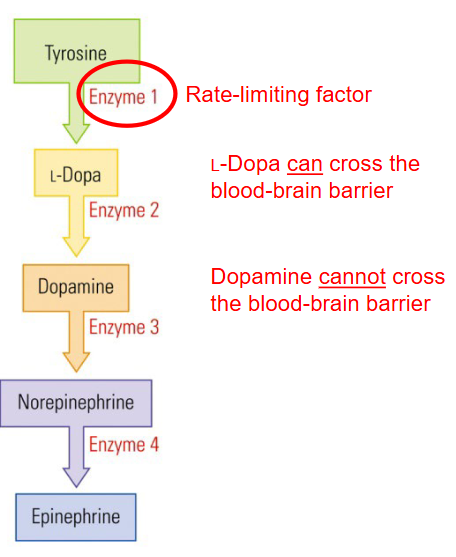
Which 3 Small-molecule transmitters are all synthesized from the precursor chemical Tyrosine (e.g. hard cheese and bananas)?
Dopamine
Norepinephrine
Epinephrine
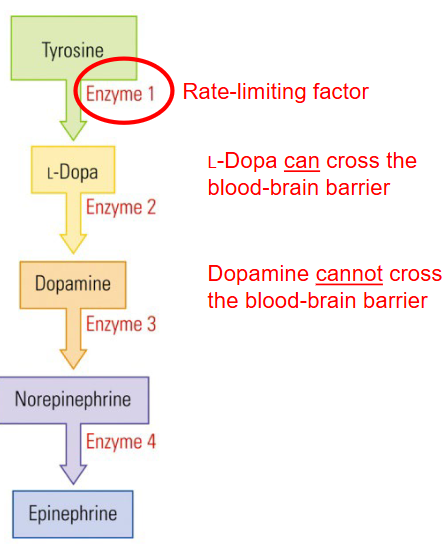
What is the Rate-limiting factor?
Enzyme 1 restricting L-Dopa from Tyrosine is limited and thus restricts the pace at which other chemical can be synthesized.
L-Dopa is the precursor chemical for dopamine. It needs to be “converted” into L-Dopa first before it can become Dopamine.
Parkinson disease means having too little Dopamine, so we would want to change the Dopamine levels in the body. We don’t administer Dopamine directly into the body though, why is that?
Dopamine cannot cross the blood-brain barrier, but L-dopa (which is the precursor of Dopamine) can cross the blood-brain barrier.
We use oral administration of L-Dopa (Levodopa) to treat Dopamine insufficiency in Parkinson.
Via which route do Neuroactive drugs reach the brain?
Many neuroactive drugs are designed to reach the brain by the same route that small-molecule transmitters, or their precursor chemicals follow: the digestive route.
What are Peptide transmitters?
Short chains of amino acids.
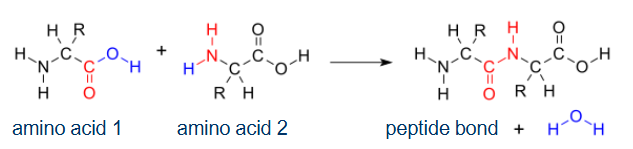
How are Peptide transmitters synthesized?
Through the transcription of DNA and translation of mRNA (like protein synthesis; ch3).
What is the difference between the synthesis of Small-molecules and Peptide transmitters?
The synthesis of Peptide transmitters is slower compared to small-molecule transmitters.
What do Peptide transmitters act like?
They act like hormones » Important for stress response, bonding (oxytocin), eating and drinking, pain (ch6).
Peptide transmitters: Endogenous opioids
» Beta-endorphin (strong analgesic (pain inhibitor), runners-high) met-enkephalin, dynorphin (pain suppresser).
Peptide transmitters: Exogenous opioids
» Opium, morphine, diamorphine (heroin).
Are Neuropeptides taken orally?
No, digestive processes degrade Neuropeptides so they are not orally taken as drugs but through other routes (e.g. intravenous).
What are the main lipid transmitters?
Endocannabinoids.
Where are Lipid transmitters synthesized at?
At postsynaptic membrane to act on CB1 receptors at the presynaptic membrane » Retrograde neurotransmitters.
What do Lipid transmitters affect?
Appetite, pain, sleep, mood, memory, anxiety, and stress response.
Lipid transmitters are Lilophilic; what does this mean?
They are fat-loving and thus not stored in vesicles » synthesized on demand (slow).
What do Lipid transmitters act as?
They act as Neuromodulators: inhibit release of Glutamate and GABA » dampen both neuronal excitation and inhibition (ch6).
What are Endocannabinoids and Phytocannabinoids (lipid transmitters) generated by?
Endocannabinoids → generated by the body (anandamide; derived from arachidonic acid in e.g. poultry, eggs).
Phytocannabinoids → hemp plants (THC, CBD).
How many neurotransmitters does a neuron secrete?
In general a neuron secretes a single or a very limited number of neurotransmitters.
So: not e.g. sometimes DA, then GABA. Once DA » Always DA.
Does a neurotransmitter have excitatory (EPSP) or inhibitory (IPSP) effect?
Depends on the postsynaptic receptor.
But in general:
DA, NE, EP » Excitatory (activating)
Glutamate » Excitatory (activating)
GABA » Inhibitory (dampening)
NB: Neurotransmitters themselves do NOT determine excitation or inhibition.
What are the 2 Postsynaptic receptor classes we have to know?
Ionotropic receptors
Metabotropic receptors
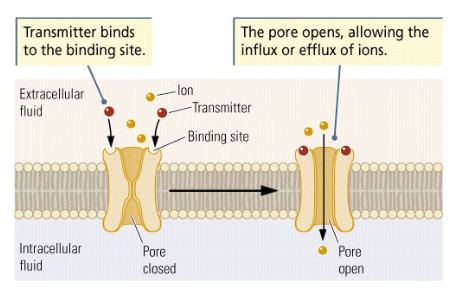
Postsynaptic receptor classes: Ionotropic receptors
tropic ~ moving forward / guiding.
Binding site for neurotransmitter + ion channel
Fast ~1 ms
Direct effect, rapidly change membrane voltage
Usually excitatory » may trigger action potential
e.g. Na+, K+, Cl- and Ca2+ ligand-gated channels
NB: structure similar to voltage-sensitive channels that propagate action potential.
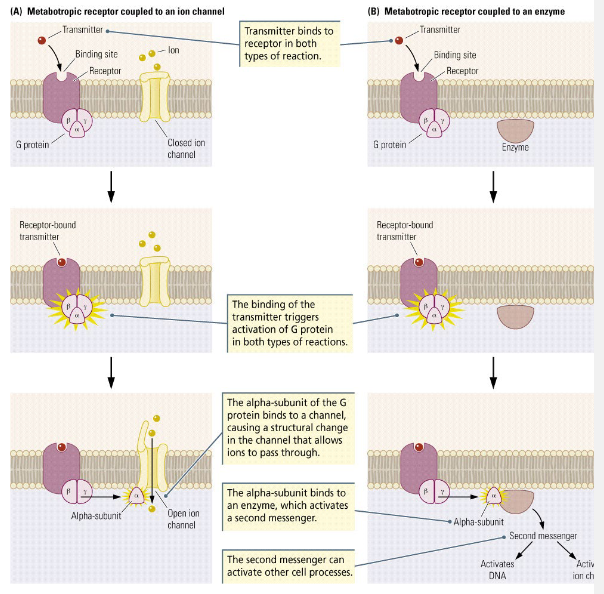
Postsynaptic receptor classes: Metabotropic receptors
Binding site only, no ion channel
Slow: some hundreds of ms
Indirect effect, change the condition of a cell via G-protein inside the cell membrane
Alpha subunit of G-protein may:
activate nearby ion channel
or bind to enzyme, which in turn activates another chemical (second messenger): may lead to amplification cascade
e.g. peptide transmitters
NB: Receptor subtypes (table 5-3) NOT required for exam.
What neurotransmitters are in the Somatic nervous system (muscles)?
Acetylcholine (ACh)
Nicotinic acetylcholine receptor nAChr (also binds with nicotine)
What neurotransmitters are in the Autonomic nervous system?
Sympathetic division (fight or flight).
Preganglionic: Acetylcholine (ACh)
Postganglionic: Norepinephrine (NE)
Parasympathetic division (rest and digest)
Acetylcholine (ACh)
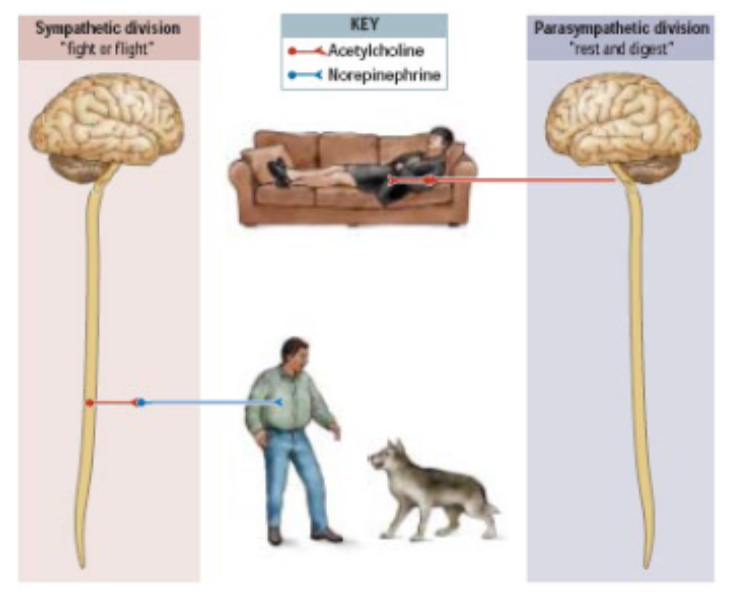
What does ACh do and what does NE do in the Peripheral nervous system?
ACh decreases (inhibits) heart rate but increases (excites) digestion.
NE increases (excites) heart rate but decreases (inhibits) digestive functions.
NB: Neurotransmitters themselves do not determine excitation or inhibition.
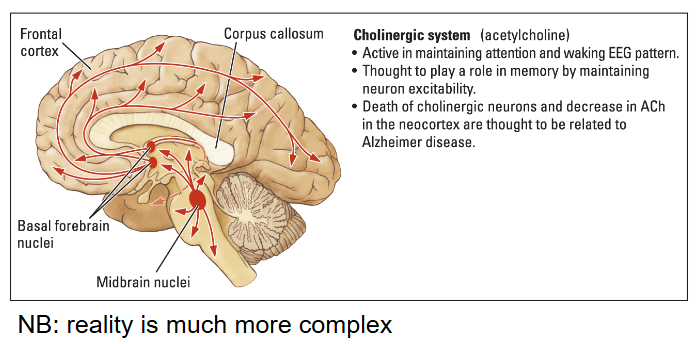
Cholinergic - Acetylcholine
Where is it located?
What function does it regulate?
What disorder is an insufficiency of this linked to?
Located in the Nucleus basalis of Meynert.
regulates Wakefulness, attention, memory.
An insufficiency of Acetylcholine is linked to Alzheimer.
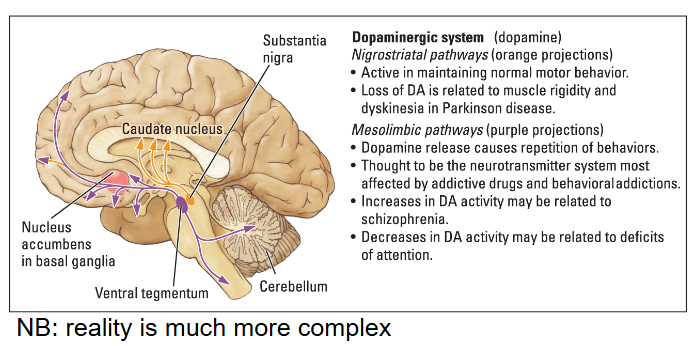
Dopaminergic - Dopamine
Where is it located?
What does it regulate?
What disorder is an insufficiency or abundancy of Dopamine linked to?
Located in the Basal Ganglia.
Nigrostriatal pathway
Dopamine regulates motor behavior.
An insufficiency leads to Parkinson
Mesolimbic pathway
Dopamine regulates reward and pleasure
An abundancy is linked to Schizophrenia
An insufficiency is linked to ADHD
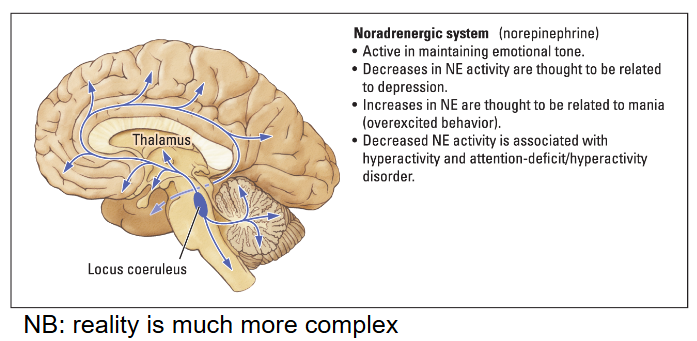
Noradrenergic - Norepinephrine
Where is it located?
What does it regulate?
What disorder is an insufficiency / abundancy linked to?
Located in the Iocus coeruleus.
Norepinephrine regulates emotional tone (mood).
An abundancy is linked to Mania (overexcited behavior).
An insufficiency is linked to Depression, ADHD
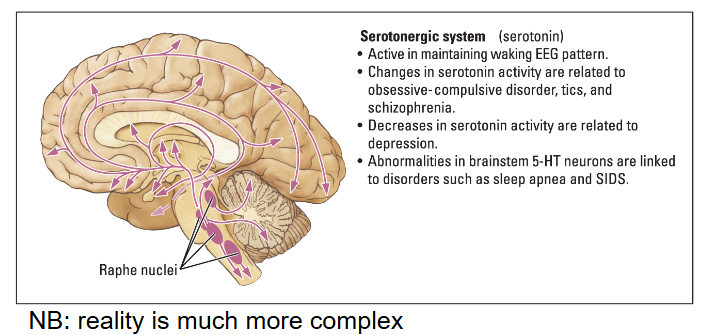
Serotonergic - Serotonin
Where is it located?
What does it regulate?
What disorder is an increase / decrease linked to?
Located in the Raphe nuclei.
Serotonin regulates Wakefulness during movement.
An increase is linked to Schizophrenia.
A decrease is linked to Depression, ODC, SIDS, sleep apnea.
What is the difference between Chemical and Electrical synapses?
Chemical synapses (involves neurotransmitters).
~5 ms slower.
Enable neural plasticity because they can:
amplify or diminish signals.
change with experience to mediate learning.
Electrical synapses have ‘gap junctions’.
~5 ms faster (no synapses)
Regulated gates (can either be open or closed):
allow glial cells and neurons to exchange substances.
allow groups of neurons to synchronize their firing rhythmically.
NB: in gap junctions, ions may flow in both directions.
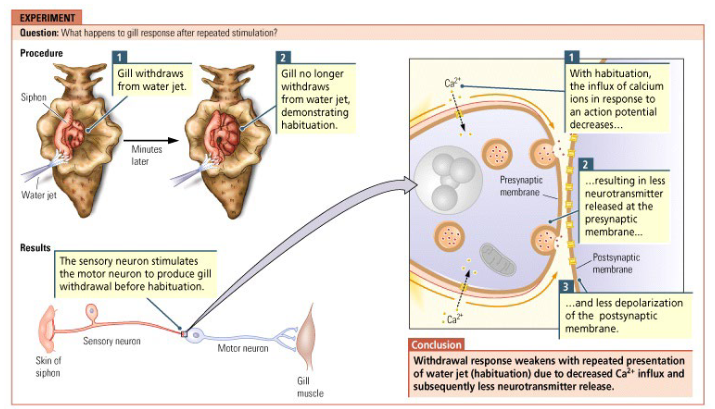
What is Habituation? What happens regarding Neural plasticity?
A decreased neural response following repeated stimulation (e.g. ignoring ambient noise).
Voltage-sensitive calcium channels become less sensitive to voltage channels.
Decreased Ca2+ influx » less neurotransmitter in synaptic cleft.
Result: EPSPs become smaller due to less neurotransmitter released in synaptic cleft causing less depolarization of postsynaptic membrane.
NB: Habituation may eventually stop neurons from ‘firing’ altogether » we make fast and small random eye movements (saccades) to prevent habituation.
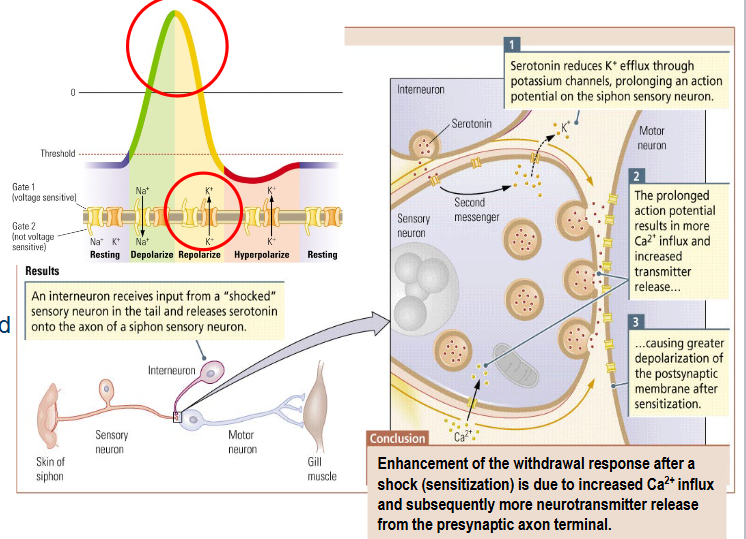
What is Sensitization? What happens regarding Neural plasticity?
Increased neural response to stimuli (e.g. PTSD).
Serotonin released by interneuron makes potassium channels less responsive.
reduced K+ efflux.
prolonged action potential.
Increased Ca2+ influx
increased neurotransmitter release
Result: EPSPs become larger due to increased amount of neurotransmitter in synaptic cleft causing greater depolarization of postsynaptic membrane.
NB: Sensitization = opposite of habituation (but both are unconscious forms of learning).
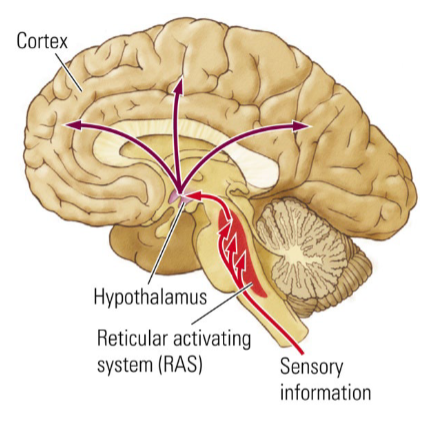
What does the Reticular activating system (RAS) do?
It regulates wakefullness.
What are the 4 Biological Rhythms we have and what do they regulate?
Circannual — yearly
hibernation, fat metabolism, migration of birds, mating in animals.
Infradian — longer than a day, shorter than a year
menstrual cycle
Circadian — daily
sleep-wake cycle, body temperature, blood pressure, stress and growth hormones
Ultradian — shorter than a day
eating
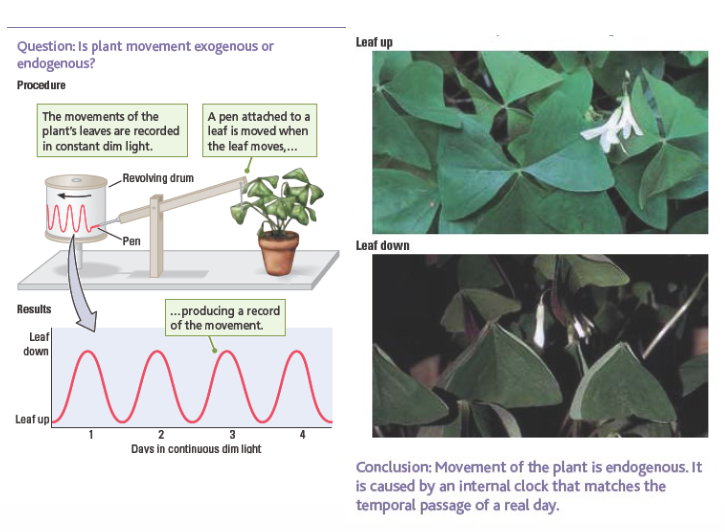
What are the 2 types of Biological rhythms we have?
Endogenous rhythms
are driven internally (biological clock)
from within the body
Exogenous rhythms
are driven externally
e.g. by the sun or the seasons
How can you test if a rhythm is endogenous or exogenous?
Keep the external conditions constant.
e.g. put someone 24/7 in continuous (dim) light or darkness and keep the temperature constant.
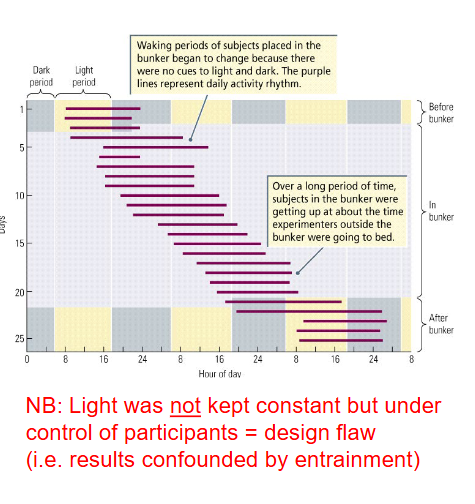
What happens if humans determine their own sleep-wake rhythm?
Day-night period extended to 25-27 hours and shifted 1-2 hours every night → free-running rhythm.
New experiment in constant twilight showed that humans have an endogenous free-running period; this is somewhat longer than 24h (24h 11m).
humans do have a biological clock, but this is slightly defect.
How does the length of free-running period vary across species?
Diurnal animals: darkness extends, lightness contracts (more active).
Nocturnal animals: darkness contracts (more active), lightness extends.
What are Zeitgebers?
Environmental events that provide a clock-setting cue (e.g. daylight).
Periodical synchronization to such environments (zeitgebers) keeps our biological clock on the 24-hour track.
What is Entrainment?
The synchronization (resetting) process to zeitgebers.
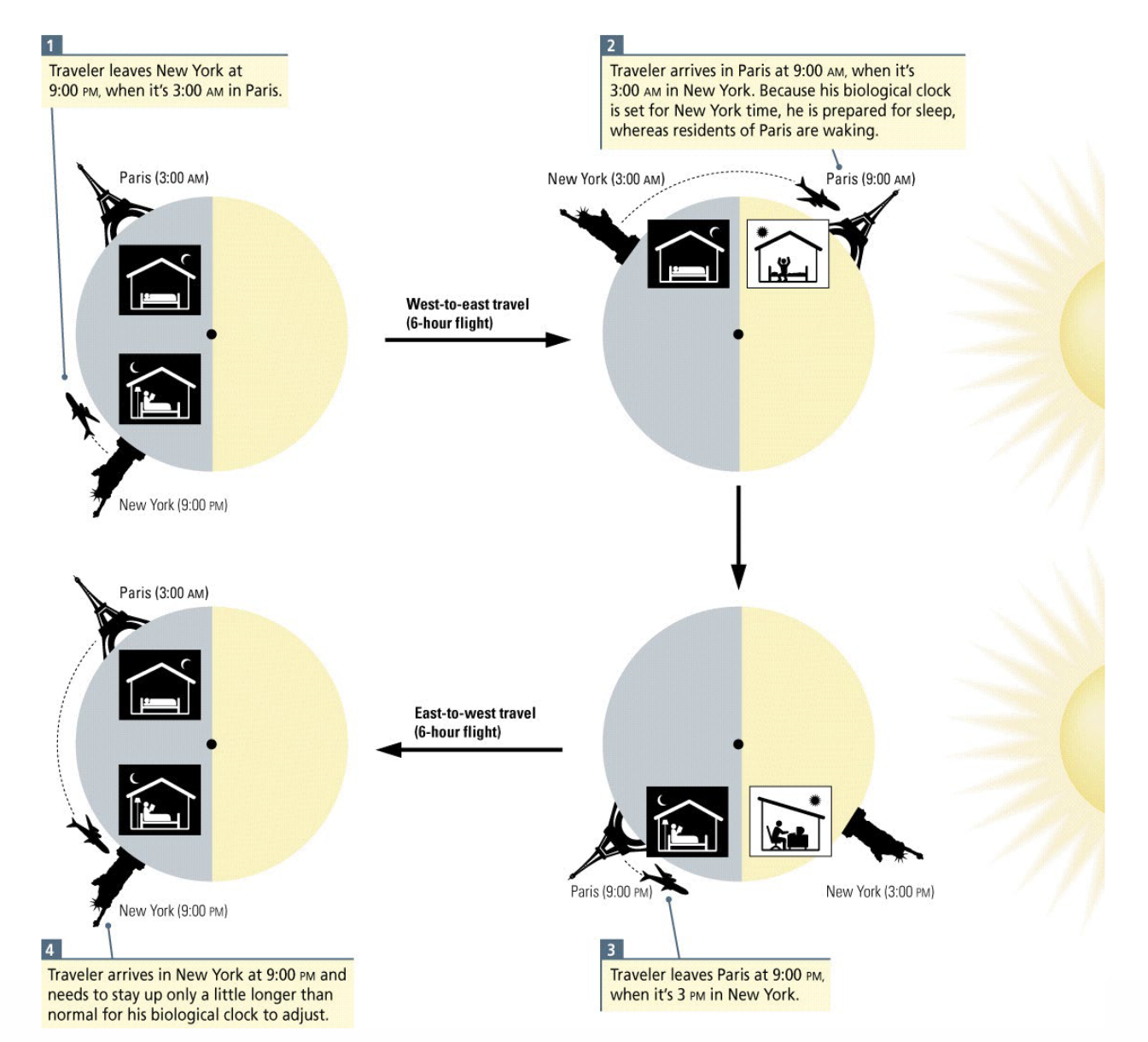
When does Jet leg arise?
When the Zeitgeber (daylight) is not synchronized with the biological clock.
The clock must be entrained to a different time-zone.
Entrainment works best if the adjustment is not too large.
NB: adjustment is more difficult from west to east than from east to west.
What is the most important biological clock structure? Where is it located?
Suprachiasmatic nucleus (SCN)
Part of the hypothalamus.
The SCN is located just above the optic chiasm
Supra chiasma
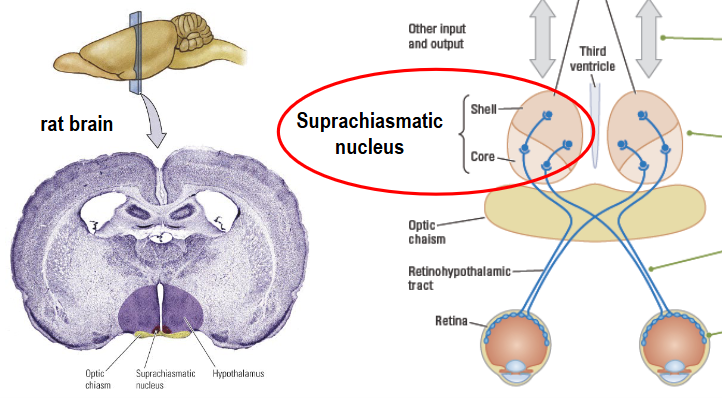
What does the SCN receive input from? Via which tract does this travel?
From photosensitive retinal ganglion cells (pRGCs).
Via the retinohypothalamic tract.
Core neurons are not rhythmic; is this statement correct?
YES; they entrain shell neurons which are genetically programmed for rhythmicity.
note: being a night owl or early bird is caused by a preference from the entrain shell neurons.
if you want to change the time you wake up, you need to change your environment.
What is the SCN’s circadian rhythm usually entrained by?
By morning and evening light, but can also be entrained or disrupted by nonphotic events, including:
Arousal
Movement
Feeding
By what are nonphotic events signaled to the SCN?
By the intergeniculate leaflet (lateral thamalus) and Raphé nuclei (serotonergic pathway, see ch5).
NB: explains why late-night snacking might disrupt circadian rhythm.
The SCN produces behavior.
Is this statement correct?
NO; the SCN itself does not produce behavior.
e.g. eating still occurs after lesion, but not at regular times.
What does the SCN act as?
A biological “Master Clock”.
it contains pacemaker cells that have an endogenous rhythm of ~24h.
What are “Slave Oscillators”?
It follows the “Master Clock”; the pacemaker cells in there entrain “Slave Oscillators”; other brain structures with circadian rhythmic activity.
e.g. during night (darkness): pineal gland → melatonin.
e.g. during day (lightness): pituitary gland → adrenal glands → cortisol
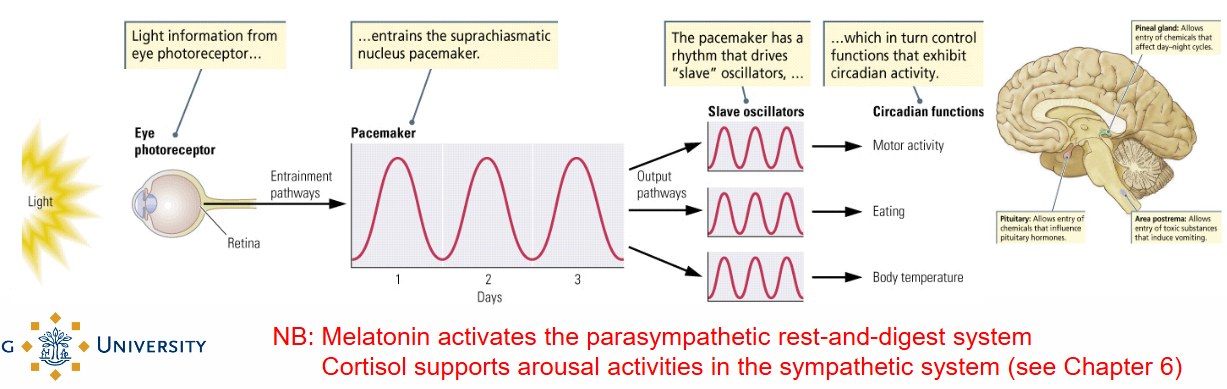
What does Melatonin do? What does Cortisol do?
Melatonin = activates the parasympathetic rest-and-digest system.
Cortisol = supports arousal activities in the sympathetic system (see ch 6).
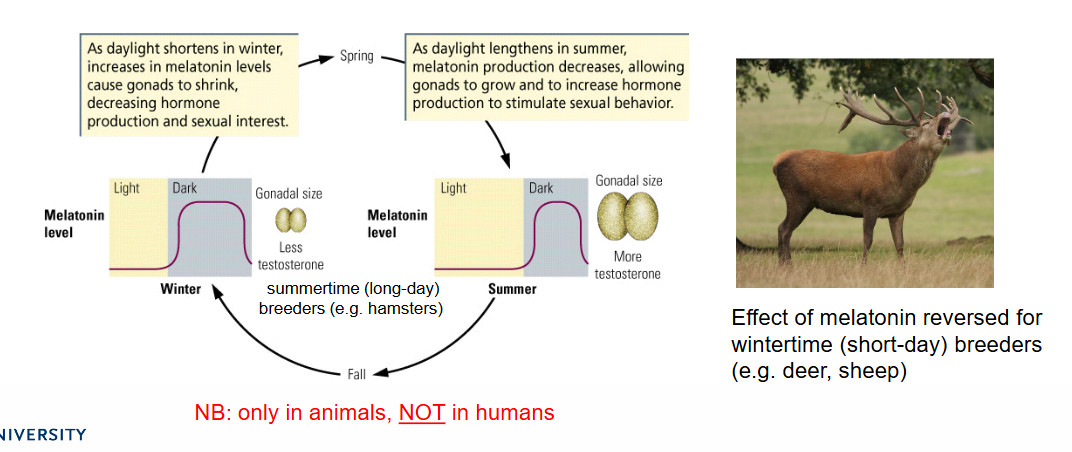
What is Melatonin secreted by and what role does it have?
Secreted by the pineal gland and plays a role in:
The circadian sleep-wake cycle (animals and humans)
In many animals also in circannual cycles (e.g. bird migration, reproduction, hibernation, etc.).
What are the 3 main electrical body signals that are required to reliably record sleep?
Brain activity
Electro-encephalography (EEG)
Muscle activity
Electro-myogram (EMG)
Eye movement
Electro-oculogram (EOG)
Additional measures: body temperature, circulating hormones, blood glucose levels.
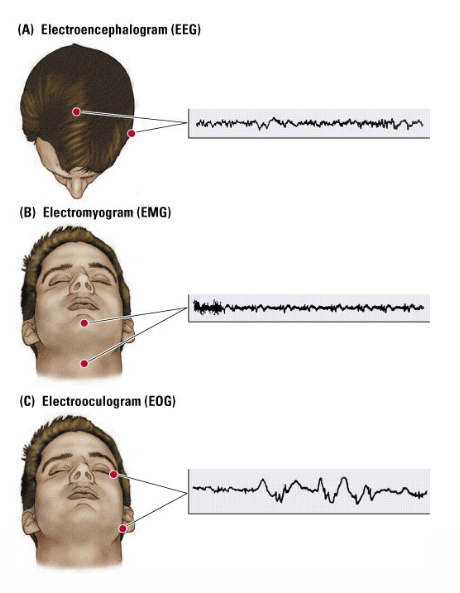
What are the sleep stages based on?
On the analysis of EEG, EMG and EOG activity (amplitude and frequency).
Based on EEG activity, there appear to be five different states of activation (states of consciousness).
Based on EEG activity, there appear to be five different states of activation (states of consciousness).
What are these 5 stages?
W Waking
beta rhythm (eyes open)
alpha rhythm (eyes closed)
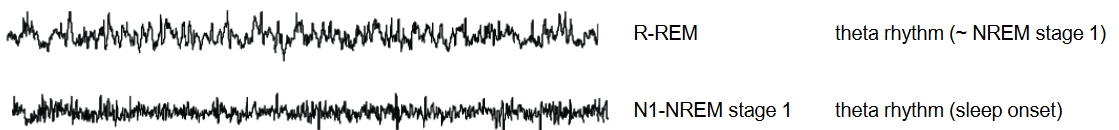
N1 NREM Stage 1
theta rhythm (sleep onset)
N2 NREM Stage 2
sleep spindles, K-complexes (asleep)
N3 NREM Stage 3
delta rhythm (deep/slow-wave sleep)
R REM
beta/theta rhythm (~Waking/NREM Stage 1)
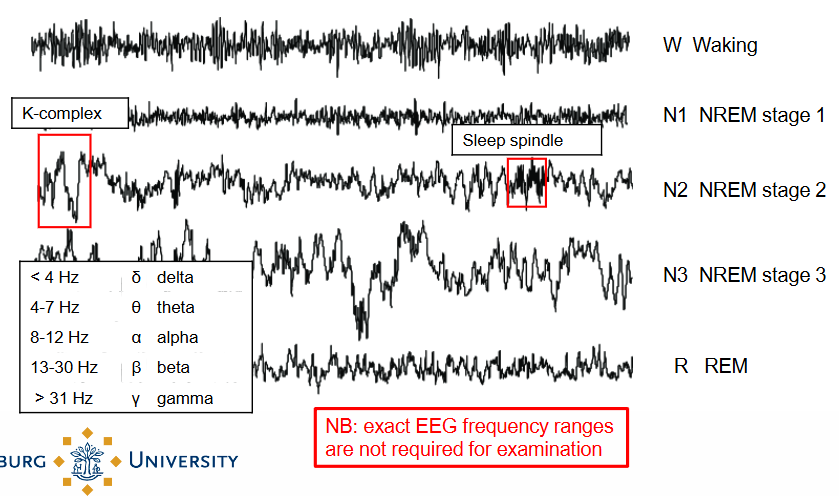
What are the 3 (strange) things that happen After NREM Stage 3?
The brain seems to wake up (EEG frequency increases, and looks similar to Waking/NREM Stage 1).
The muscles are maximally relaxed (atonia), suggesting deep sleep.
The EOG shows (horizontal) Rapid Eye Movement (REM), and mouth, fingers and toes may twitch.
NB: Movement of eyes, face, fingers and toes during REM sleep help maintain blood flow and may be related to development of coordinated movements and tuning of neural motor circuits (esp. in children)
What happens when the EEG frequency increases?
The brain seems to be waking up; there is more activity.
What is Atonia?
When the muscles are maximally relaxed.
What is the Paradoxical sleep?
The REM Sleep stage is also called paradoxical sleep because of the ‘awake’ EEG and ‘sleeping’ EMG.
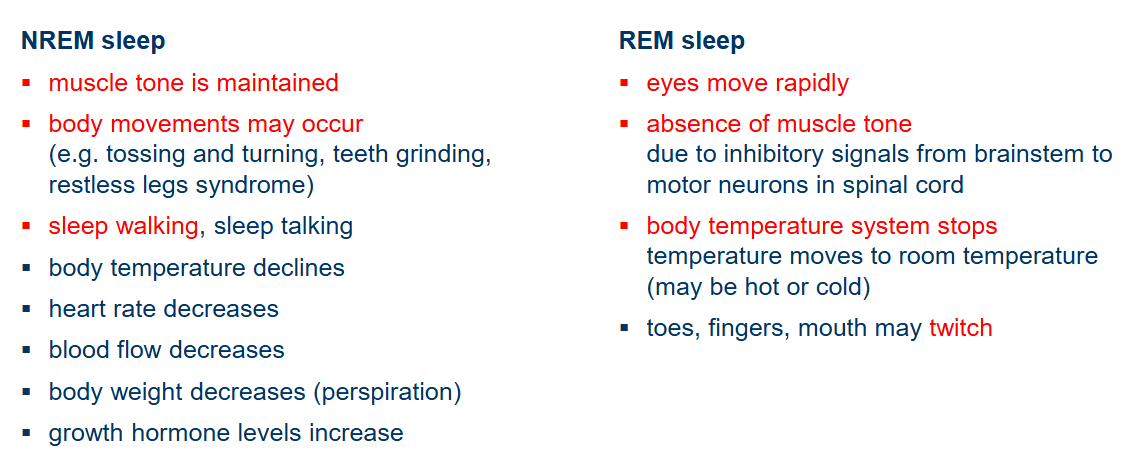
What are the differences in NREM sleep and REM sleep?
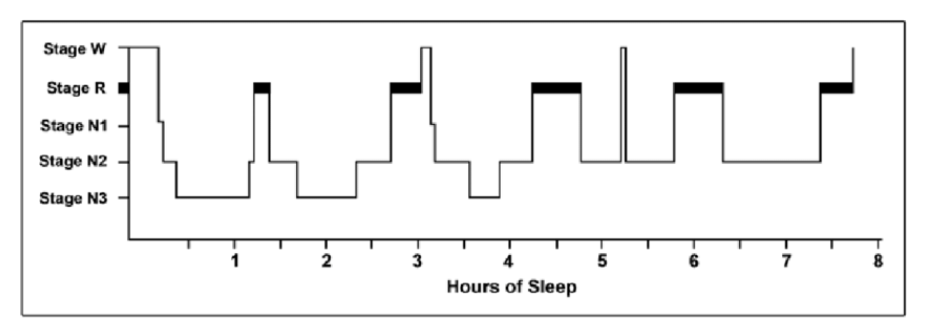
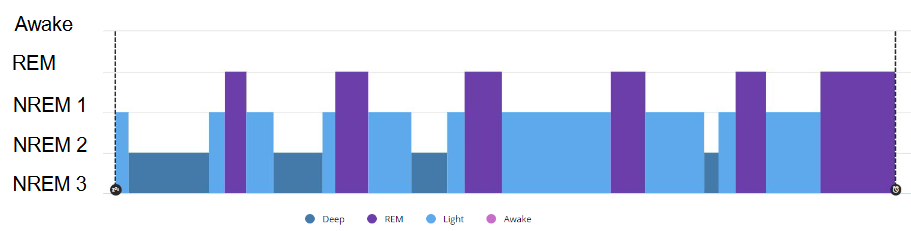
What is a Hypnogram?
A graph that represents the stages of sleep as a function of time.
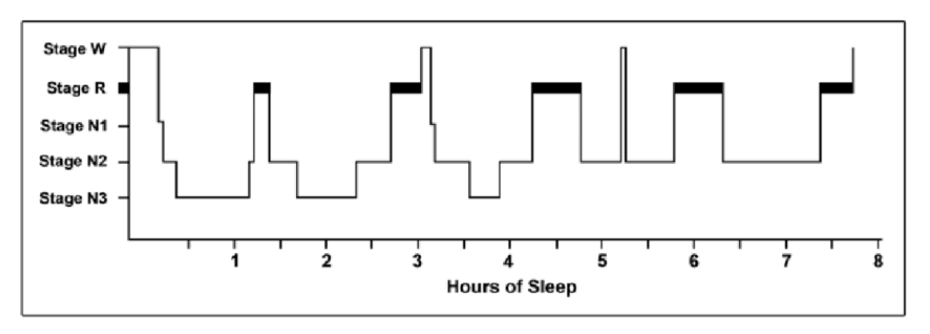
How can the Sleep stages of a night be expressed in a Hypnogram?
First halve of a typical night is mainly characterized by NREM sleep, second halve mainly REM sleep.
NREM-REM sequence last ~90 minutes and occurs ~5 times a night.
When does REM-rebound happen?
If you do not sleep long enough (or at all) one night, the REM sleep occurs at the beginning of the following night → REM-rebound.
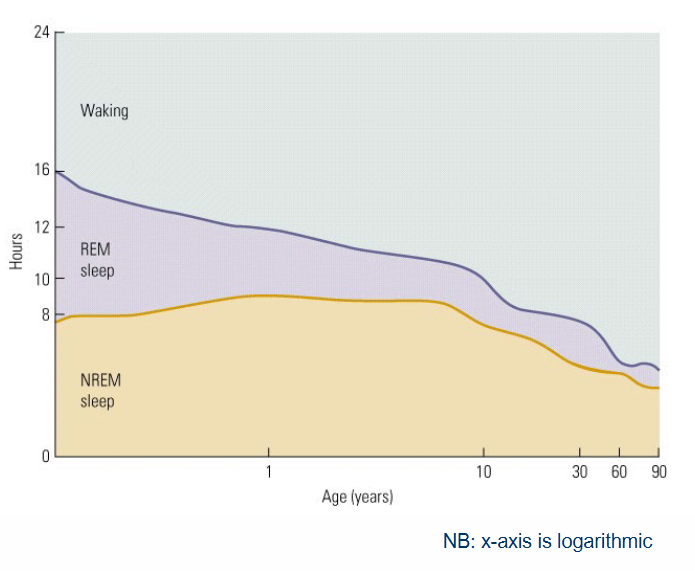
How does Sleep change over the Life span? Name 3 changes.
Most people sleep less as they grow older.
The amount of REM sleep decreases significantly with age.
Children from the age of ~2 years show a REM sleep pattern that resembles that of adults.
From roughly this age onwards, they also start to dream and remember things.
The hippocampus is largely myelinated around this age.
NB: These findings support the relationship between REM sleep, dreaming and memory.