Exam #2
1/179
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
180 Terms
What is blood pressure?
The force exerted by the blood against the walls of the blood vessel. This maintains perfusion during activity and rest.
Describe the mechanisms that maintain BP
Maintenance of BP and tissue perfusion requires both systemic factors and local peripheral vascular effects. Primarily a function of CO and SVR!
What is HTN?
Increased BP beyond what may be considered “normal” (healthy, safe, non-problematic)
What is a normal BP?
120/80 or less
Systolic BP
Heart contracting - blood exerting pressure on vessels
Diastolic BP
Heart relaxing - How much pressure in the system during relaxation
What is considered elevated BP?
Systolic 120-129
Diastolic: more than 80
What BP is considered HTN?
Systolic: 130 or higher
Diastolic: 80 or higher
Blood pressure formula
BP = CO x systemic vascular resistance
What is cardiac output (CO)? What affects it?
CO = SV x HR
Total blood flow through the systemic or pulmonary circulation (out of the heart) per minute
Effects:
Cardiac system
heart rate, contractility, conductivity
Renal fluid volume control
RAAS
Renin (angiotensin-aldosterone system)
retains water, increases fluid volume (ultimately increases BP)
Converts angiotensin 1 to angiotensin 2
A 2 increases BP (vasoconstrictor and stimulates adrenal cortex to secrete aldosterone)
Natriuretic peptides
Controls sodium excretion and extracellular fluid volume
What is systemic vascular resistance?
The pressure of veins and arteries. The force opposing the movement of blood within the blood within the blood vessels. Think of cholesterol and how that gunk will turn from mushy to hardened. Greater resistance equals increased BP.
What affects the systemic vascular resistance? (SVR)
sympathetic nervous system
alpha 1 and alpha 2 adrenergic receptors (vasoconstrictors)
Increased SNS increases HR and contractility producing the vasoconstriction and promotes the release of renin (increase BP)
beta 2 adrenergic receptors (vasodilator)
Baroreceptors in carotid arteries and aorta sense BP changes and send signals to brainstem that then sends signals to brainstem that then sends message through neurons to excite or inhibit efferent nerves that innervate cardiac and smooth muscle cells
neurohormonal
vasoconstrictors (angiotensin & norepinephrine)
Increased BP: Inhibition of the SNS results in decreased HR, force of contraction, and vasodilation in peripheral arterioles to decrease BP
Decreased BP: Activation of the SNS results in constriction of the peripheral arterioles, increased HR and contractility to increase BP
Causes of secondary HTN
Cirrhosis
Coarctation or congenital narrowing of the aorta
Drug related (estrogen replacement therapy, oral contraceptives, corticosteroids, non steroidal anti-inflammatory drugs, sympathetic stimulants such as cocaine)
Endocrine disorders
Cushing syndrome, thyroid disease
Neurologic disorders
Brain tumors
Pregnancy
Renal disease
Sleep apnea
Risk factors of HTN
Age, alcohol consumption, tobacco use, diabetes mellitus, elevated serum lipids, excess dietary sodium, gender, family hx, obesity, ethnicity, sedentary lifestyle, socioeconomic status, stress
Manifestations of HTN
Fatigue, reduced activity tolerance, dizziness, palpitations/angina, dyspnea
Complications of HTN
Target organ diseases occur most frequently in:
Heart - CAD, LVH, HF
Brain - cerebrovascular disease, increased risk of CVA
Kidney - CKD
Eyes - retinal damage
Treatment of HTN
Overall goals
Control BP
Reduce
Primary (essential or idiopathic) HTN
Elevated BP without an identified cause
Most common! 90-95% of HTN cases
Secondary HTN
Elevated BP with a specific cause! 5-10% of adult cases. Clinical findings will relate to an underlying cause.
HTN diagnostic studies
Bilateral BP measurement (remember, highest in morning and lowest at night) Use arm with highest reading!
UA, creatinine clearance
Serum electrolytes, glucose (uncontrolled diabetes)
BUN and serum creatinine
Serum lipid profile
EKG
Echocardiogram
Effects of HTN on the heart
HTN increases the workload on the heart inducing structural and functional changes in the myocardium. These changes include hypertrophy of the left ventricle which can lead to HF. Heart attacks, chest pain, and arrhythmias can occur because of changes to blood vessels.
Effects of HTN on the blood vessels
Thickens the walls of blood vessels and makes them less elastic. Alongside cholesterol deposits in the blood vessels, the risk of a heart attack is increased because there is trouble supplying blood to the heart. Chest pain (angina) and arrhythmias can occur as well. Blood flow is limited throughout the body in general! Kidneys are damaged and unable to work! Kidney failure can occur.
Effects of HTN on the kidneys
HBP can damage the blood vessels leading to the kidneys. Kidney scarring can occur because the tiny blood vessels within the kidneys become scarred and are unable to effectively filter fluid and waste from the blood. Glomerulosclerosis can lead to kidney failure! Damaged blood vessels prevent the kidneys from effectively filtering waste from the blood, allowing dangerous levels of fluid and waste to collect. Treatment may include dialysis or transplant.
List the major classes of antihypertensives
B-adrenergic blockers (beta blockers)
Angiotensin Converting Enzyme (ACE) inhibitors
Angiotensin II receptor blockers (ARBs)
Calcium channel blockers
Diuretics
Direct vasodilator
Mechanism of action, side effects, nursing considerations: B-adrenergic blockers (beta blockers)
-sins & -lols
Action
decrease peripheral resistance of blood vessels by unknown mechanism
heart: block beta 1 receptors which decreases HR and contractility, decreases CO, and suppresses reflex tachycardia
kidney: block renal beta receptors which decreased angiotensin I related vasoconstriction as well as aldosterone related fluid retention
Side effects
Bradycardia
SOB
Edema
Nursing considerations
monitor HR (report if less than 60bpm)
monitor for signs of HF (SOB, peripheral edema of extremities, night cough) and report
Tapering if discontinued
Examples
Metoprolol (take with food at same time every day)
Atenolol (before meals - AC, or bedtime)
Propanolol
Mechanism of action, side effects, nursing considerations: Angiotensin Converting Enzyme (ACE) inhibitors
-ils
Action
Blocks production of angiotensin II (from angiotensin I) causing vasodilation as well as urinary excretion of sodium/water and retention of potassium
Side effects
Dry, non-productive cough due to increase in bradykinin
hypotension
rash
metallic taste in mouth
hyperkalemia, neutropenia (decrease WBC, increased risk of infection)
Nursing considerations
Start at low dose and gradually increase
Diuretics may be temporarily stopped
Monitor BP
Monitor and report dry cough
Monitor and report for angioedema
monitor potassium levels
monitor WBC count
Examples
lisinopril, fosinopril
Mechanism of action, side effects, nursing considerations: Angiotensin II receptor blockers (ARBs)
-ans
Action
Blocks angiotensin II receptors which causes angiotensin II to be unable to bind to those receptor sites, resulting in: arteriolar vasodilation, urinary excretion of sodium and water, and retention of potassium
Less able to protect patients from acute cardiovascular events (myocardial infarction) making them 2nd choice after ACE inhibitors for treatment of hypertension
Side effects
angioedema
dizziness
hypotension
headache and insomnia
Nursing considerations
Monitor BP
prepare to treat angioedema with IV epi
monitor and report CNS effects
Oral only
With or without food
Examples
Losartan
valsartan (Diovan)
irbesartan (Avapro)
candesartan (Atacand)
Mechanism of action, side effects, nursing considerations: Calcium channel blockers
-ines
Action
Bock calcium channels in vascular smooth muscle cells of peripheral arterioles and minimally block calcium channels in cardiac arteries
This results in vasodilation (then lowered BP)
Side effects
Reflex tachycardia
Can cause increased anginal pain in clients with angina
Mainly with fast-acting tabs
Headache, lightheadedness, dizziness, facial flushing, perception of heat, peripheral edema, arrhythmias
Not common: Gingival hyperplasia (overgowth of gum tissue and easy-bleeding gums)
Nursing considerations
Monitor HR, lightheadedness/dizziness, assist with ambulation
Monitor for development of peripheral edema (report, diuretic may be needed)
Monitor BP
Regular dental checkups
Examples
Nifedipine, amlodipine
Mechanism of action, side effects, nursing considerations: Diuretics
Action
remove water and electrolytes from the body by increasing urination
Side effects
headaches
dizziness, lightheadedness
increased sensitivity to light
muscle weakness or cramping
electrolyte abnormalities
severe dehydration
irregular heart rate
Nursing considerations
Monitor weight, intake, output, serum electrolyte levels
Examples
spironolactone/ hydrochlorothiazide
triamterene/ hydrochlorothiazide
Where do thiazide diuretics affect?
Distal tube of henle
Mechanism of action, side effects, nursing considerations: Direct vasodilator
Action
Open/dilate blood vessels and prevent the muscles of arteries and veins from tightening and the walls from narrowing
Side effects
tachycardia
palpitations
Edema
Nausea/vomiting
headache
excessive hair growth
joint pain
chest pain
Nursing considerations
Remain flat for 1 hour after admin
examples
Hydralazine
Minoxidil
nitroglycerin
What is coronary artery disease (CAD)?
A type of blood vessel disorder in the general category of atherosclerosis. Soft deposits of fat accumulate in the arteries and harden with age. This can occur in ANY artery in the body.
What are atheromas?
Fatty deposits
Pathophysiology of CAD
Atherosclerosis (major cause)
Characterized by a focal deposit of cholesterol and lipid, primarily within the intimal wall of the artery
Endothelial lining becomes altered as a result of inflammation and injury \
Collateral circulation
Normally, some arterial anastomoses exist within the coronary circulation
Risk factors of CAD
Non-modifiable
Age
Sex
Ethnicity
Family Hx
Genetic predisposition
Modifiable
Elevated serum lipids
Hypertension
Tobacco/substance use
Physical inactivity
Obesity
Diabetes
Metabolic syndrome (r/t insulin resistance)
Psychological states
Homocysteine level
Manifestations of CAD
dizziness/lightheadedness
fatigue
SOB
chest discomfort
chest pain
Chronic stable angina (nitroglycerin is the treatment)
acute coronary syndrome
CAD diagnostics
ECG
Blood pressure
Cardiac catheterization
Shows presence of atherosclerotic lesions
Nursing management/Collaborative care/Treatment of CAD
BP meds
Nitrates
Lipid lowering
Oxygen
Complications of CAD
Chest pain (angina)
Heart attack
Heart failure
Arrhythmias
Clinical manifestations of CAD: Chronic Stable Angina
Reversible! The O2 demain is greater than the O2 supply. This can be caused by increase in demand (ex - exertion) or decrease in supply (ex - hematologic or respiratory pathways)
Chest pain, usually lasts 3-5 min and will. subside when the precipitating factor is relieved. ECG reveals ST-segment depression and/or T wave inversion
Silent ischemia! Can occur in the absence of any subjective symptoms. Associated with diabetic neuropathy and is confirmed by the ECG
Treatment of Chronic Stable Angina
A - antiplatelet/anticoagulant therapy
B - Beta blocker, BP control
C - Cigarette smoking cessation, cholesterol (lipid) management, calcium channel blockers, cardiac rehabilitation
D - diet (weight management), Diabetes management, Depression screening
E - Education, Exercise
F - flu vaccine
NITRO
Clinical manifestations of CAD: Acute Coronary Syndrome
Unstable angina (UA)
Non-ST segmenet elevation myocardial infarction (NSTEMI)
ST-segment elevation MI (STEMI)
Signs and symptoms of unstable angina - why is it a medical emergnecy?
Chest discomfort or pain caused by an insufficient flow of blood and oxygen to the heart!
Change in usual pattern of stable angina
New in onset
Occurs at rest
Has a worsening pattern
UA is unpredictable and represents a medical emergency because the unstable plaque can rupture into thrombus (can be dislodged and lead to STEMI or NSTEMI)
Signs and symptoms of chronic stable angina
Stable angina (angina pectoris) is a type of chest pain that happens when your heart muscle needs more oxygen. It occurs intermittently, over a long period of time, with a similar pattern of onset, duration, and intensity of symptoms
Can happen when you are exercising or when it is cold outside
Temporary chest pain BUT can lead to acute coronary syndrome
Chest pain that feels like pressure or indigestion.
Pain that radiates to your left shoulder or down your left arm
SOB
Dizziness.
Nausea.
Exhaustion
Relieved with nitroglycerin
What is acute coronary syndrome (ACS)?
a term for a group of conditions that suddenly stop or severely reduce blood from flowing to the heart muscle. When blood cannot flow to the heart muscle, the heart muscle can become damaged
Non-ST-elevation myocardial infarction (NSTEMI), ST-elevation MI (STEMI), and unstable angina are the three traditional types of ACS.
Pathophysiology of ACS
develops when ischemia is prolonged and not immediately reversible!
Deterioration of once stable plague —> rupture —> platelet aggregation —> thrombus
Results in partial occlusion of coronary artery: UA or NSTEMI
Total occlusion of coronary artery: STEMI
Manifestations of ACS
Unstable angina
Myocardial infarction
Nursing/collaborative care/Treatment/interventions for ACS
ECG monitoring
IV access
O2 therapy
Medications (MONA)
Morphine sulfate
Vasodilator and pain relief
Reduces anxiety
Decreases contractility, BP, HR
Oxygen
Nitroglycerin
Reduces pain
Improves coronary blood flow
Aspirin
anti-platelet
Antidysrhythmics
Prevent them
Lipid lowering drugs
Statins
Rest and comfort to balance rest and activity while beginning cardiac rehab
ambulatory and home care
Patient and caregiver teaching
Physical exercise
Diagnostic studies for ACS
cardiac biomarkers
EKG
Coronary angiography
Opens up occluded artery and limit infarction size
What is a myocardial infarction?
The result of sustained ischemia! Causes irreversible myocardial cell death and eventual necrosis of myocardium. The degree of altered function depends on area of the heart and size. Most involve the LV.
Signs/symptoms of MI
Cardiovascular
Increased HR, BP (then BP lowers secondary to decreased CO)
Crackles as a result of LV dysfunction
JVD as result of RV
Abnormal heart sounds (S3 or S4), new onset murmurs
Nausea and vomiting
Fever
systemic inflammatory process caused by cell death
Myocardial infarction (MI) - healing process
Within 24 hours, leukocytes infiltrate the area of cell death.
Enzymes are released from the dead cardiac cells (important indicators of MI).
Proteolytic enzymes of neutrophils and macrophages remove all necrotic tissue by the second or third day.
Development of collateral circulation improves areas of poor perfusion.
Necrotic zone identifiable by ECG changes and nuclear scanning
10 to 14 days after MI, scar tissue is still weak and vulnerable to stress.
By 6 weeks after MI, scar tissue has replaced necrotic tissue.
Area is said to be healed, but less compliant.
Ventricular remodeling
Normal myocardium will hypertrophy and dilate in an attempt to compensate for the infarcted muscle.
Complications of MI
Dysrhythmias
Heart failure
Cardiogenic shock
Acute pericarditis
What is the treatment of choice for a confirmed MI?
Emergent PCI - non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup, a condition known as atherosclerosis.
STEMI - What is it? Causes? Signs and symptoms?
ST-elevated MI - FULLY occluded artery
Caused by chest pain, pallor, SNS stimulation, N/V, fever, SOB
ST elevation on EKG
Cell death
Emergent and must be treated within 90 minutes with PCI or thrombolytic therapy
NSTEMI - What is it? Causes?Signs and symptoms>?
Non-ST elevated MI - PARTIALLY occluded artery
Caused from deterioration of stable plaque that ruptures and forms a thrombi —> MI
Elevated troponin
St depression on ECG or T wave inversion
Cell death
Not emergent but must go to cath lab within 12-72 hours
What is sudden cardiac death?
Unexpected death from cardiac causes! Rapid CPR, defibrillation with AED, and early advanced cardiac life support increase survival. There is abrupt disruption in electrical function of cardiac muscle, resulting in acute loss of CO and cerebral blood flow. Death is usually within one hour of onset of acute symptoms (angina, palpitations)
Sudden cardiac death - etiology and pathophysiology + causes + risk factors
Most SCD caused by ventricular dysrhythmias (e.g.,ventricular tachycardia), i.e., an electrical problem
SCD occurs less commonly as a result of LV outflow obstruction (e.g., aortic stenosis).
Primary risk factors
Left ventricular dysfunction (EF 30%)
Ventricular dysrhythmias following MI
Depolarization of the cardiac muscle causes a contraction. Immediately following depolarization, the heart enters a(n) ___________ during which it cannot be stimulated, prior to a(n) ___________ during which a significantly strong impulse may excite it. With repolarization, the heart muscle enters a period of ___________.
absolute refractory phase (it can't beat again)
relative refractory period (can be if the stimulus is great enough)
full excitability
List the 3 muscular layers
endocardium (inner)
Myocardium (muscle layer)
Epicardium (outer layer)
Pericardium
sac that surrounds the heart
The left ventricular wall is 2-3x thicker than the right ventricular wall - why?
This is because the left ventricle pumps oxygenated blood round the entire body while the right ventricle only pumps blood to the lungs which is a much shorter distance.
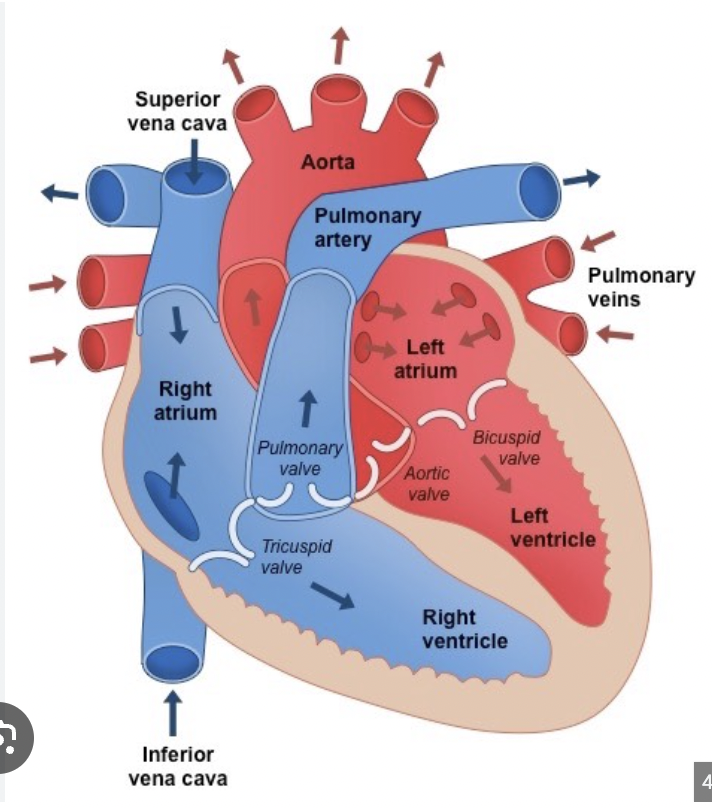
Explain the circulation of blood throughout the heart
Deoxygenated blood enters RA (from SVC and IVC)
Tricuspid valve (AV valve)
Right ventricle
Pulmonary semilunar valve
pulmonary artery
lungs (gas exchange in the capillaries)
Pulmonary veins
left atrium (oxygenated blood from lungs)
Bicuspid (mitral) valve (AV valve)
Left ventricle
aortic semilunar valve
aorta
What does lub and dub stand for?
Lub - associated with closure of the tricuspid and mitral valves
Dub - associated with the closure of the aortic and semilunar valves
What is mean arterial pressure? How do you calculate it?
Average pressure within the arterial system that is felt by the organs in the body
SBP + 2DBP / 3
Discuss electrical conduction in the normal heart (pathway of the action potential)
SA node
Internodal pathways
AV node
Bundle of His
Left and right bundle branches
Purkinje fibers
What are the three natriuretic peptides?
atrial natriuretic peptide (ANP) from the atrium
B-type natriuretic peptide (BNP) from the ventricles
BNP is the marker of choice for distinguishing a cardiac or respiratory cause of dyspnea
C-type natriuretic peptide from the endothelial and renal epithelial cells
Automaticity
Ability to initiate an impulse spontaneously and continuously
Excitability
ability to be electrical stimulated
Conductivity
Ability to transmit an impulse along a membrane in an orderly manner
Contractility
Ability to respond mechanically to an impulse
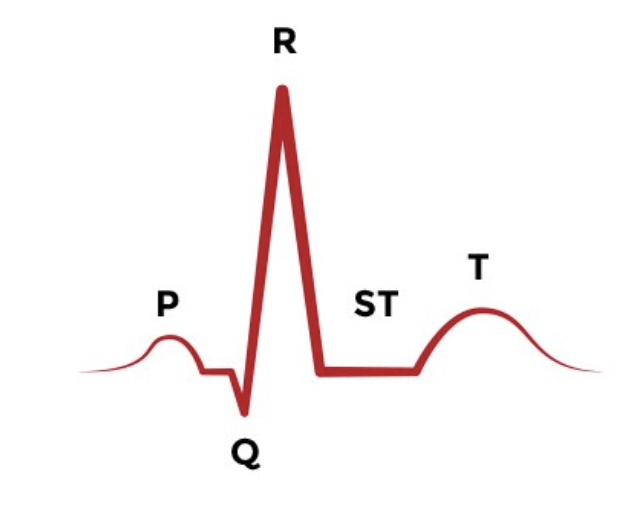
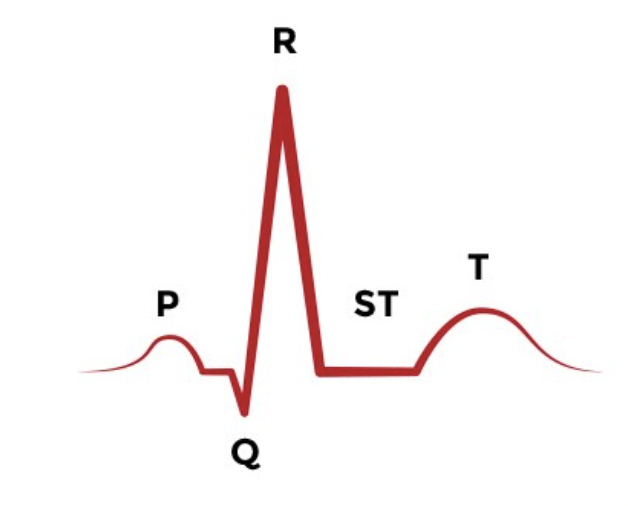
P wave
Atrial depolarization (contraction)
Firing of the SA nod
Should be upright
Normal duration: 0.06-0.12 seconds
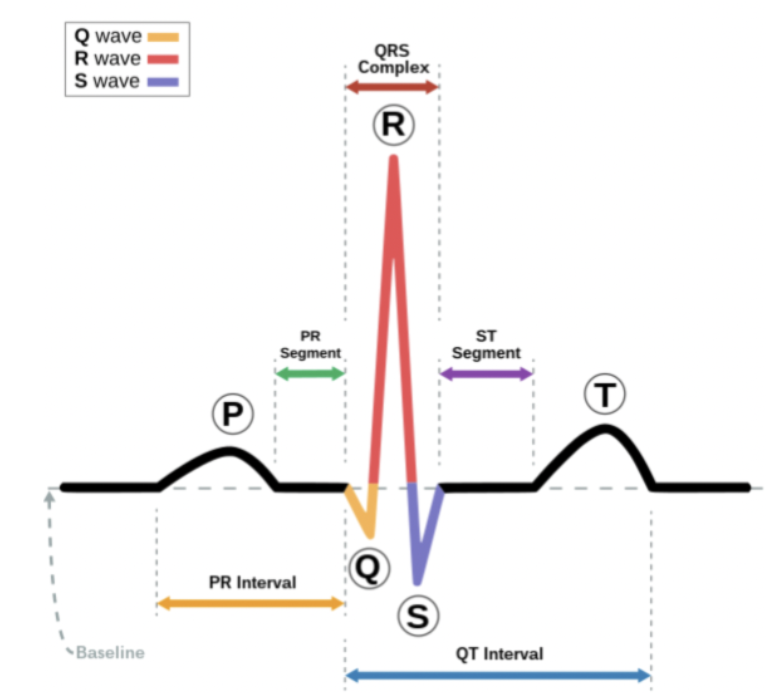
PR interval
Measured from beginning of P wave to beginning of QRS complex
Represents time taken for impulse to spread through the atria, AV node and bundle of His , bundle branches, and purkinje fibers, to a point immediately before ventricular contraction
Normal duration: 0.12-0.20 sec
Duration could vary due to disturbance in conduction usually in AV node, bundle of His, or bundle branches but can be in atria as well
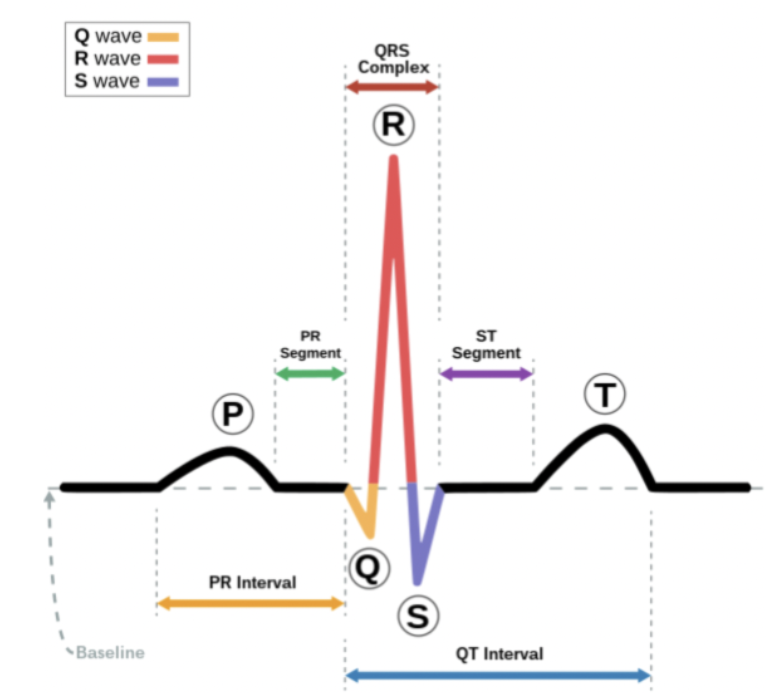
QRS interval
Measured from beginning to end of QRS complex
Represents time taken for depolarization of ventricles (systole)
Duration: <0.12 sec
Variation could be due to disturbance in conduction in bundle branches or in ventricles
Q wave
First negative (downward) deflection after the P wave, short and narrow, not present in several leads
Duration: <0.03 seconds
MI may result in development of a pathologic Q wave that is wide (greater than or equal to 0.03 seconds) and deep (greater than or equal to 25% of the height of the R wave)
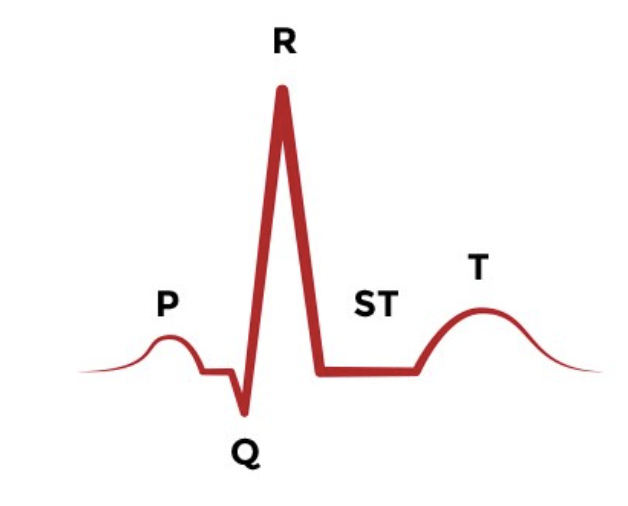
T wave
Represents time for ventricular repolarization
Should be upright
Duration: 0.16 sec
Disturbances (ex - tall, peaked, inverted) usually caused by electrolyte imbalances, ischemia, or infarction
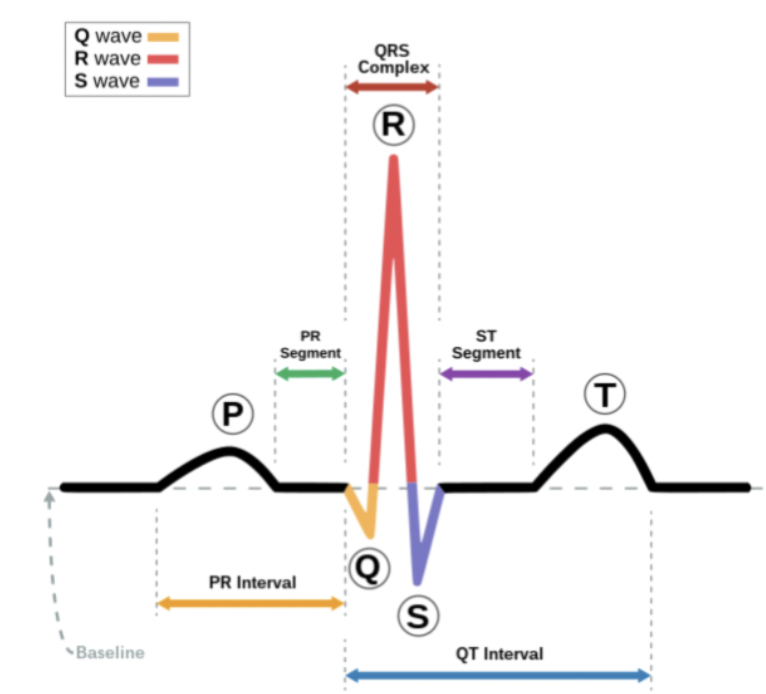
ST segment
Measured from the S wave of the QRS complex to the beginning of the T wave
Represents the time between ventricular depolarization and repolarization (diastole)
Should be isoelectric (flat)
Duration: 0.12 seconds
Disturbances (like elevation, depression) usually caused by ischemia, injury, or infarction
QT interval
Measured from the beginning of QRS complex to end of T wave
Represents time taken for entire electrical depolarization and repolarization of the ventricles
normal adult women have slightly longer QT intervals than men
Duration: 0.34-0.43 seconds
Disturbances usually affecting repolarization more than depolarization and caused by drugs, electrolyte imbalances, and changes in heart rate
How to determine HR from a 6 second strip
1500 method (most accurate)
1500/# of small boxes between R waves
300 method
300/# of large boxes between R waves
Lazy way
Count the number of QRS complexes in a strip and multiply by 10

Identify the rhythm! Discuss nursing and collaborative care
Normal sinus rhythm
Heart rate is 60-100 bpm
P wave appears normal and precedes each QRS (1:1 ratio)
PR interval is 0.12-0.20 seconds
QRS complex is 0.06-0.10 seconds
P waves and QRS complexes are evenly spaced

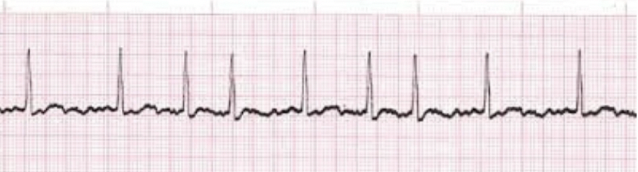
Identify the rhythm! Discuss nursing and collaborative care
Sinus bradycardia
50 bpm
P wave, PR interval, and QRS complex are same as NSR
May or may not represent a problem
Clinical assessment
Cap refill
Hypotension
Decreased perfusion
Altered LOS
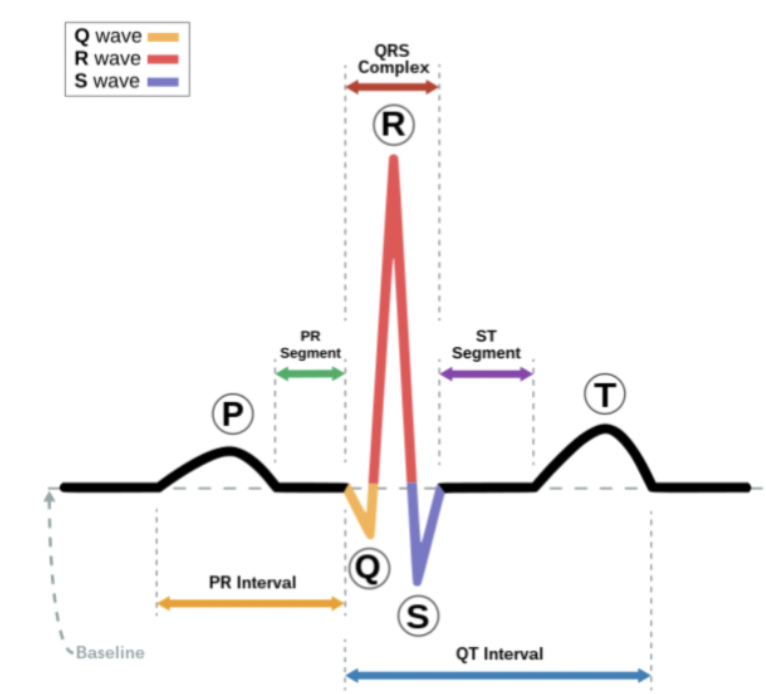
Identify the rhythm! Discuss nursing and collaborative care
Sinus tachycardia
130 bpm
Heart rate >100 bpm
P wave is normal but may merge with T wave at very fast rates
PR interval and QRS complex are same as NSR
QT interval narrows with increasing heart rate
May or may not present a problem
During exercise, tachycardia may be benign
Ominous sign - decreased cardiac output and hypotension due to blood loss, or conditions such as sepsis
If we decided it was a problem:
Depends on the problem!
Fever: antipyretic (ibuprofen, tylenol)
Chest pain: Nitro, oxygen, aspirin
Blood loss: Blood transfusion, stop the bleeding
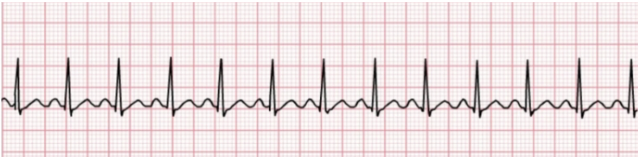
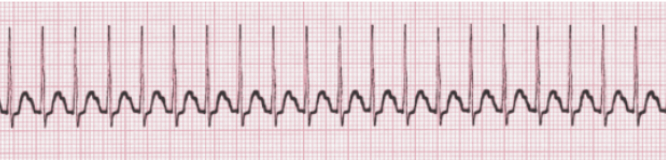
Identify the rhythm! Discuss nursing and collaborative care
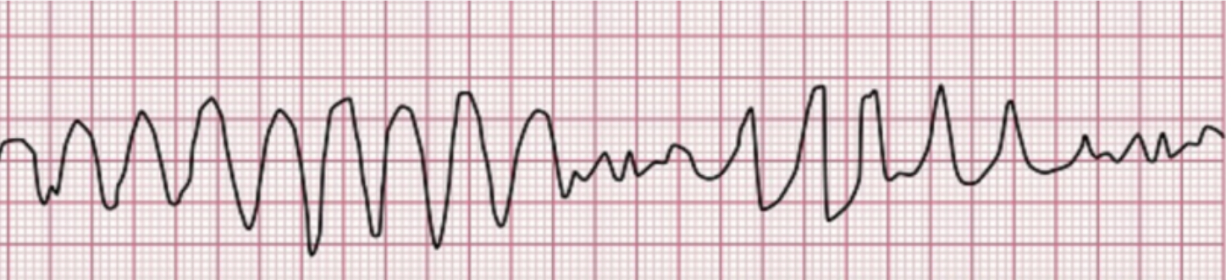
Ventricular tachycardia (VT)
Heart rate is usually 100-250 bpm
P wave is absent, PR interval is not measurable, and QRS complex is typically wide > 0.10 seconds and unusual in appearance
Life threatening and can develop into VF
Stable (pulse) unstable (pulseless)
if pulseless: CPR and rapid defibrillation
If unconscious and pulse is present, maximize oxygenation and prepare for cardioversion with synchronized defibrillation.
Identify the rhythm! Discuss nursing and collaborative care
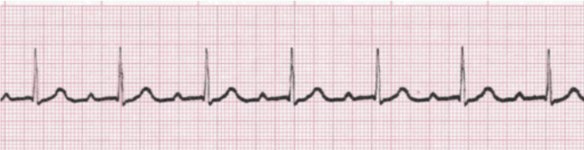
Atrial fibrillation (AF or Afib)
Rhythm appears irregular
Atrial rate is variable and may be very fast (> 350 bom), but ventricular rate may be slow, normal, or fast
P wave features are absent - erratic waves are present
PR interval is absent
QRS complex is normal or may be widened due to conduction delays
May represent a problem with the SA node and/or conduction across the atria and/or the presence of multiple pacemaker cells. Asynchronous contraction of the atria decreased “atrial kick” by inhibiting complete contraction and by stimulating rapid ventricular repolarization (“rapid ventricular response” or RVR) which decreases passive filling time. Inadequate ventricular filling results in decreased cardiac output
Patients should be assessed for hypotension, perfusion, and use of anticoagulant medication. New onset Afib may be converted chemically or electrically once anticoagulation is established or maintained for 24 hours
What do you do?
Ask if they have had it
Ask if they are on a blood thinner (they should be)
Usually occurs because of poor cardiac health (typically seen in older patients)
Treatment: calcium channel blockers, beta blockers and digoxin, amiodarone and ibutilide, electrical cardioversion, anticoagulants
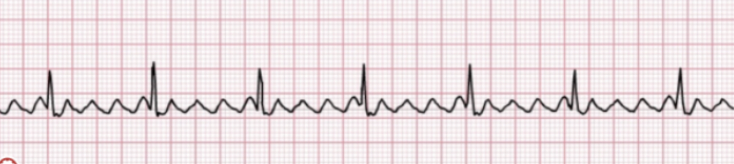
Identify the rhythm! Discuss nursing and collaborative care
Atrial flutter (A-flutter)
Atrial rate is rapid (250-350 bpm) but ventricular rate is slower
Rhythm appears more regular than A-fib
P wave and PR interval are not observable
“Sawtooth” flutter waves are present
QRS complex is typically normal (0.06-0.10 seconds)
Can be asymptomatic or symptomatic (decreased exercise, tolerance, palpitations, lightheadedness, fatigue, SOB)
Can lead to cardiomyopathy and heart failure because of high ventricular rates and loss of atrial kick (P wave) decrease CO
Treatment: electrical cardioversion, beta blockers, calcium channel blockers, and anticoagulants
Identify the rhythm! Discuss nursing and collaborative care
Supraventricular tachycardia (SVT)
Heart rate is fast (150-250)
P wave is often merged with T wave
PR interval is normal (0.12) but can be difficult to measure
QRS complex will typically be normal (0.10 sec)
SVT may be asymptomatic but may also present with anxiety, palpitations, chest pain, lightheadedness, syncope, SOB upon exertion and/or exercise intolerance. Intermittent SVT without provoking factors (medications, caffeine, alcohol, nicotine, or stress) referred to as pSVT, is more common among women
Cardioversion of SVT can be achieved biomechanically (ex - carotid massage, vagal or valsalva maneuver), chemically (adenosine), or electrically (synchronized defibrillation). Hemodynamic instability (hypotension, hypoxia, SOB, chest pain, shock, evidence of poor end-organ perfusion, or altered mental status) should be treated quickly without synchronized cardioversion. Like defibrillation, adenosine disrupts myocardial conduction but has a short half life (less than 6 seconds) so must be administered rapidly. Vagal maneuvers may be accompanied by encouraging an alert patient to increase intrathoracic pressure against a closed glottis (ex - bear down)

Valsalva maneuver
Used for supraventricular tachycardia (SVT)
Exhale against obstruction
Hold breath and “bear down”
Produce emotional shock
Peds
Infants - ice water to face
Blow through a 5cc syringe
Adenosine function
SVT
Slows conduction through AV node
Rapid IV push followed by 20 cc saline flush
Pre administration procedure
Oxygenate patient (NC, etc), have RT present
Ensure continuous cardiac monitoring
Attach defibrillator pads or have paddles at ready
Patient teaching - explain that the drug may slow or stop the heart and can produce anxiety/panic and may lead to loss of consciousness
Half life is 10 seconds - this means the heart will start up (hopefully)

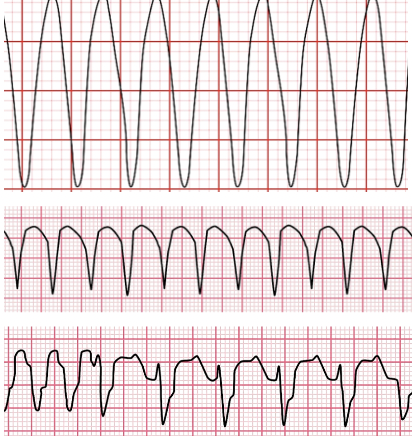
Identify the rhythm! Discuss nursing and collaborative care
ventricular fibrillation
Doesn’t really have any characteristic waveforms
Heart rhythm is irregularly irregular and heart rate is not measurable
P wave is absent, PR interval is not measurable, and QRS complexes are absent
VF is incompatible with a palpable pulse because the ventricles are quivering, not contracting.
Assess patient for LOC, if unconscious initiate CPR and prepare for immediate unsynchronized defibrillation. If conscious check your monitor
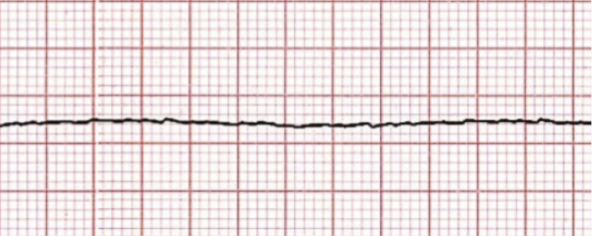
Identify the rhythm! Discuss nursing and collaborative care
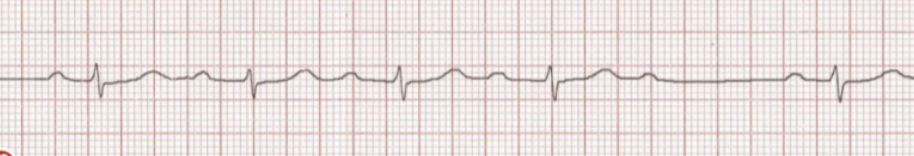
asystole
No discernable wave forms
Change monitor leads to confirm in a second lead
Assess LOC and pulse, if either exists check monitor
Beware of agonal heart beats (erratic, non-sustainable electrical impulses that are residual to life. Also note that implanted pacemakers can produce electrical waveforms despite death of patient)
Many think to defibrillate the patient but NO! Why stop a heart when its already stopped? You want to start compressions to mimic the heart
Identify! what precipitates them, and their medical and nursing management and treatment
Torsades de pointe
Rhythm appears to undulate (big and then small) and heart rate is not measurable
Cause: Low magnesium
P waves are absent, PR interval is not measurable, and QRS complexes appear abnormal
Indicates irritability of the myocardium
Assess patient for LOC and pulse. If no pulse is present, initiate CPR and prepare for unsynchronized defibrillation. If unconscious with pulse, prepare for cardioversion with synchronized defibrillation and assess serum magnesium. If conscious with pulse, maximize oxygenation and, administer iV magnesium, and prepare for cardioversion with synchronized defibrillation with conscious sedation and/or pain management
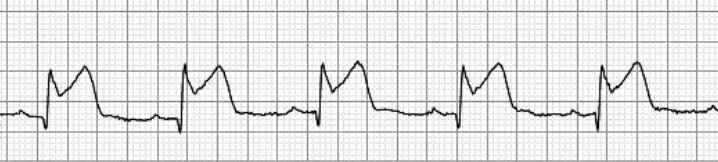
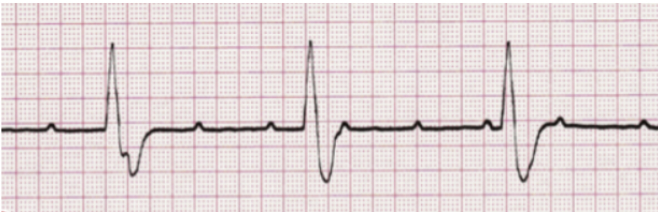
Identify what type of heart block is shown! Discuss symptoms
1st degree heart block
Heart rate is unaffected, typically 60-100
P wave present, PR interval is prolonged (0.21-0.48 seconds usually - should be less than 0.2 seconds), QRS is normal
Typically asymptomatic, assess patient for potential cause
Ischemia/myocardial infarction
Medications
Athletic predisposition
Typically seen in well conditioned athletes
Can or can’t be a problem - ask about symptoms
Identify what type of heart block is shown! Discuss symptoms
2nd degree heart block - Mobitz type 1 (Wenckebach)
After the 4th, there us a pause
PR interval gradually increases until a QRS does not follow a P wave (drops) after which the cycle repeats
Typically asymptomatic if heart rate is adequate
Identify what type of heart block is shown! Discuss symptoms
2nd degree heart block - Mobitz type 2
P waves are normal and consistent, PR is constant if QRS is present, but some P waves do not initiate a QRS. QRS may be normal or wide depending upon when conduction is blocked
More serious than Mobitz type 1, it may progress to 3rd degree block without warning. May be symptomatic (angina, SOB, lethargy) if ventricular rate is slow
Anticipate the need for transcutaneous pacing and the placement of an internal pacemaker
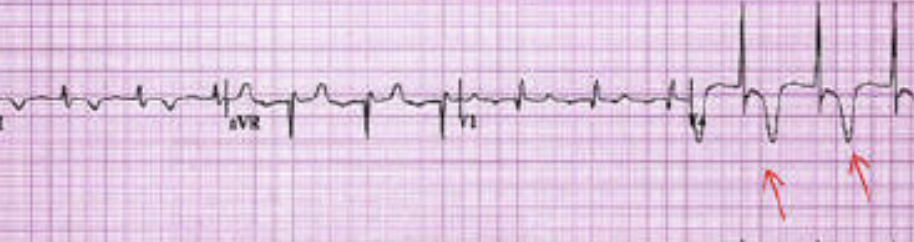
Identify what type of heart block is shown! Discuss symptoms
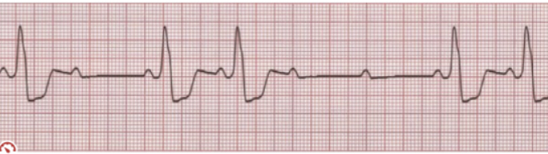
3rd degree heart block
P waves are present and consistent
PR interval is inconsistent
QRS is present and consistent
No relationship between P and QRS. Atria and ventricles beat independently and at different rates
Symptomatic if slow ventricular rate affects cardiac output
Anticipate the emergent need for transcutaneous pacing and eventual placement of an internal pacemaker
What is pacing?
Turn AED/defibrillator to pacer mode
Two controls: rate & amplitude
How fast the pacer stimulates beats (70 bpm ex)
How much energy is needed to achieve ventricular response
Two concepts
Electrical capture = pacer spike followed by a QRS
Mechanical capture = pacer spike and QRS and a palpable pulse
For transcutaneous pacing
Address pain control and/or LOC
What is pulseless electrical activity (PEA)? What causes it?
A condition in which an organized rhythm, is seen on the monitor, but the patient is unconscious and has no pulse
Pulseless VT is a form
VF does not represent PEA either because by definition is not an organized rhythm, and the patient is presumed pulseless
Used to be called Electrical-mechanical dissociation
A name that aptly describes what is going on
The electrical system of the heart is functioning but is not stimulating the mechanical system to function, they are not associated, and therefore myocardial contraction does not occur
Without immediate treatment, it is lethal!
Causes: Hs & Ts
Hypovolemia (not enough blood makes it hard for the heart to contract
Hypothermia (too cold for too long) or hyperthermia
hypo/hyper kalemia
Hydrogen ions (acidotic)
Cardiac tamponade (trauma to chest, something is pushing on pericardial sac and it can’t beat or contract because it is being squished) (bleeding in pericardial sac)
Pneumothorax (collapsed lung) (can be due to broken rib that punctures the lung)
What is heart failure?
The heart muscle is unable to deliver adequate CO to meet the body’s metabolic needs due to inadequate ventricular filling or ventricular ejection
Most common reason for hospitalization of adults >65 years old
Primary risk factors of HF
CAD
HTN
Valvular & congenital disorders
Myocarditis
Advanced age
Diabetes
Tobacco use
Vascular disease
Systolic failure (HFrEF) - What is it? What is it caused by?
**heart failure with reduced ejection fraction **
Impaired ability of left ventricle to pump sufficient volume with each contraction
Distinguishing Characteristic: Decreased left ventricular ejection fraction (EF) less than 40% (normal is 55–65%)
Caused by
Impaired contractile function (e.g.,MI - ischemic, injured, necrotic)
Increased afterload (e.g., hypertension)
Cardiomyopathy
Mechanical abnormalities (e.g., valve disease)