chapter 5 pt. 1 - host-microbe relationships
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
what is the root cause of infectious disease?
the inability of positive relationships to form between microbes and their host organisms
do organisms live in a purely chemical or physical environment?
no, they live in association with other individuals of their own and different species
what is a symbiotic organism and its 3 forms?
when organisms live in close nutritional relationships required by one or both members. the 3 types are:
mutualism, when both members benefit from the relationship
commensalism, when one member benefits but the other remains unharmed but does not benefit from the relationship
parasitism, where the parasitic member benefits to the harm of the host member
what are normal microbiota?
the microbes that form either commensual or mutual relationships with the body
what do normal microbiota of the upper respiratory tract include?
they include those found in the nose, mouth, trachea, and occasionally the bronchi. examples are Streptococcus mutans, which is found in the oral cavity and on the surface of the teeth
the lower respiratory tract, which includes the alveoli of the lungs, are generally free of
microorganisms because of the activity of the mucociliary escalator and alveolar macrophages
what is a non-symbiotic organism and its 2 forms?
organisms that are free-living and don’t require relationships to survive. its 2 forms are:
synergism, where members cooperate and share nutrients
antagonism, where some members are inhibited/destroyed by others
describe the process of a tapeworm (taenia) infection. what is the lifecycle of a parasitic tapeworm?
eggs or tapeworm segments in feces are passed into the environment
eggs/segments are ingested by pigs or humans
tapeworm embryos hatch and penetrate the intestinal wall, then circulate to the musculature of pigs or humans
embryos develop into larvae in the muscles of pigs or humans. humans can acquire the infection by ingesting raw/undercooked meat from an infected animal host
tapeworm attaches itself to the intestine via hooks on the scolex. cysts can develop in any organ and are most common in subcutaneous tissue as well as in the brain and eyes
what kind of microbes constitute the body’s normal microbiota?
the ones that colonize bodily surfaces without normally causing disease
what are resident microbiota?
microbiota that remain a part of the body’s normal microbiota throughout life
resident flora include
the skin and mucous membrane, parts of the inner surface of the GI tract, and opening to the cutaneous surface from the urinary, respiratory, and reproductive tracts
what are transient microbiota?
microbiota that only remain in the body for a few hours, days, or months before disappearing
where are transient microbiota found?
they are in the same places as resident members of the normal microbiota, but they can’t survive because of competition from other microorganisms, elimination by the body’s defense cells, or chemical/physical changes in the body that dislodge them
how is an infant exposed to microbes?
just before birth, the uterus and its contents (which are normally sterile during embryonic and fetal development and usually remain germ-free) will become unsterile. the fetal membranes will break and microbes from the mother’s vagina will enter the womb, exposing the infant to microbes
explain how comprehensive exposure occurs during the birth process, when the baby unavoidably comes into intimate contact with the birth canal.
within 8-12 hours after delivery, the newborn has typically become colonized by bacteria such as streptococci, staphylococci, and lactobacilli (which was primarily acquired from the mother). the skin, GI tract, and portions of the respiratory and genitourinary tracts will all continue to be colonized as the baby comes in contact with family members, health care personnel, the environment, and food
how are normal microbiota maintained?
the flora live in balance with their host, creating an environment that prevents infection and enhances certain defenses. the microbes replace themselves on a regular basis to maintain the types/numbers in their zones. however, because the exact content of the microbiota isn’t fixed, many changes can disrupt this balance
what changes can disrupt the balance between normal microbiota and their host?
the use of broad spectrum antibiotics, changes in diet, and underlying disease can alter the makeup of the microbiota and cause disease.
how does estrogen help the vagina to maintain normal microbiota?
estrogen stimulates the vaginal mucosa to secrete glycogen, which certain bacteria (such as lactobacillus) ferment, and this lowers the pH to around 4.5. before reaching puberty, a small amount of estrogen and glycogen are produced, increasing vaginal pH to around 7. as hormone levels rise during puberty, the vagina begins depositing glycogen and the microbiota shift to the acid-producing lactobacilli. it is thought that the acidic pH of the vagina during this time prevents the establishment and invasion of microbes with potential to harm a developing fetus. the estrogen-glycogen effect continues throughout childbearing years until menopause, where microbiota return to a mixed population (similar to that of prepuberty)
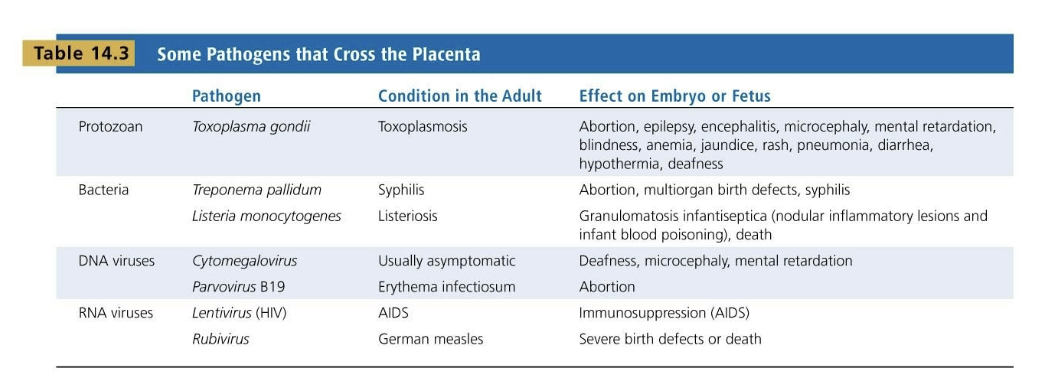
these are lists of pathogens, the condition they cause in an adult, and their effects on embryos/fetuses
what are the 2 categories of pathogenic microbes?
true/primary pathogens, which are capable of causing infection and disease in healthy people with normal immune defenses
opportunistic pathogens, which can cause disease when the host’s defenses are compromised or when they become established in a part of the body that isn’t natural to them. these usually aren’t considered pathogenic to a normal, healthy person and don’t usually have well-developed virulence properties
what is the difference between contamination and infection?
contamination is the mere presence of microbes in/on the body. some microbial contamination can reach the body via food, drink, or the air, while others are introduced through wounds, biting arthropods, or sexual intercourse
infection is the successful invasion of the body by a pathogen. these pathogens overcome the body’s external defenses, multiply, and become established in the body
what is the difference between symptoms, signs, and syndromes?
symptoms are the subjective evidence of a disease as sensed by the patient
signs are any objective evidences of disease as noticed by the observer
syndrome is when a disease can be identified by a certain complex of signs and symptoms
why do asymptomatic/subclinical infections go unnoticed?
because they have no symptoms
what is etiology?
the study of the cause of a disease
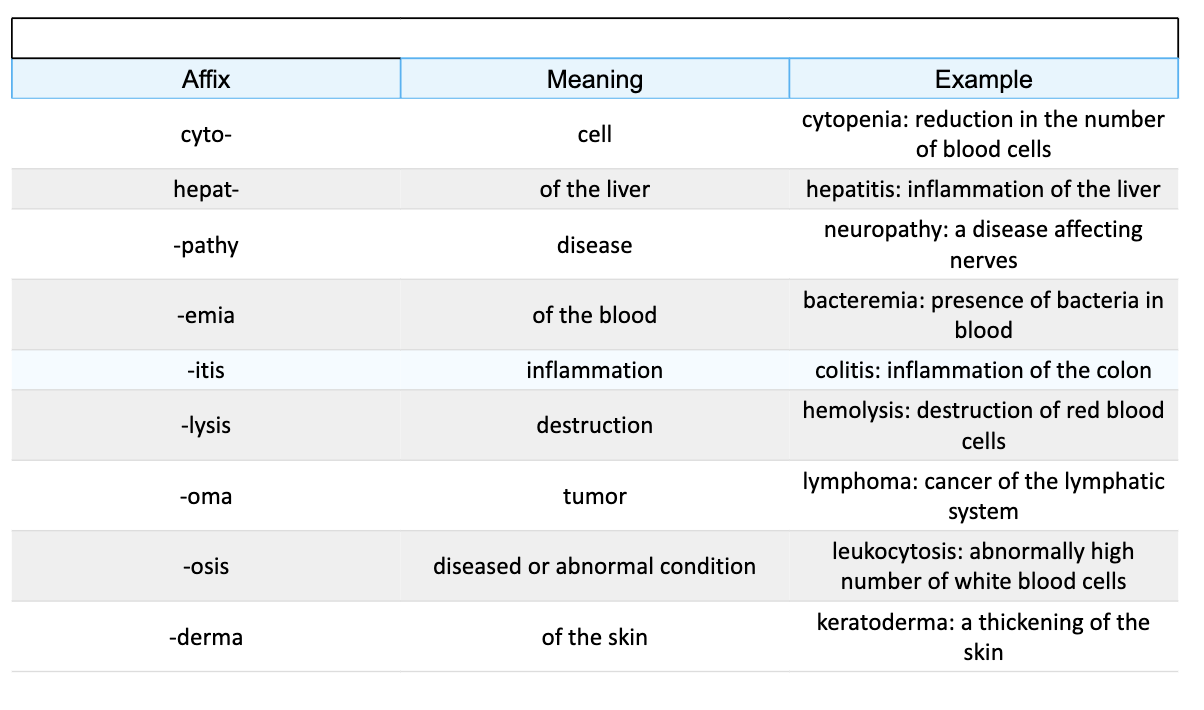
this is the nomenclature of symptoms
what is pathogenicity and its 2 factors?
it is the ability to cause disease. its 2 factors are:
infectivity, or the ability to invade/colonize sterile body compartments
virulence, or the ability to damage host tissues
infection only proceeds when
the minimum number (or infectious dose/ID) is present
following entry of the pathogen, the next stage of infection requires that the pathogen..
binds to the host
penetrates its barriers
becomes established in the tissue
what is adhesion?
a process by which microbes gain a more stable foothold at the portal of entry
bacterial pathogens usually attach by adhesion factors such as
fimbriae (pili), flagella, and adhesive slimes or capsules
viruses usually attach by adhesion factors such as
specialized receptors
helminths usually attach by adhesion factors such as
suckers and hooks
how do protozoa use adhesion?
they infiltrate by means of their organelle of locomotion
what are the virulence factors from a microbe’s perspective?
any adaptations it uses to invade and establish itself in the host
define avirulent
the bacterial cells and viruses have lost the ability to make adhesins (attachment proteins)
some bacterial pathogens don’t attach to host cells directly, so what do they do instead?
they interact with each other to form a sticky web of bacteria and polysaccharides called a biofilm, and that adheres to a surface within a host
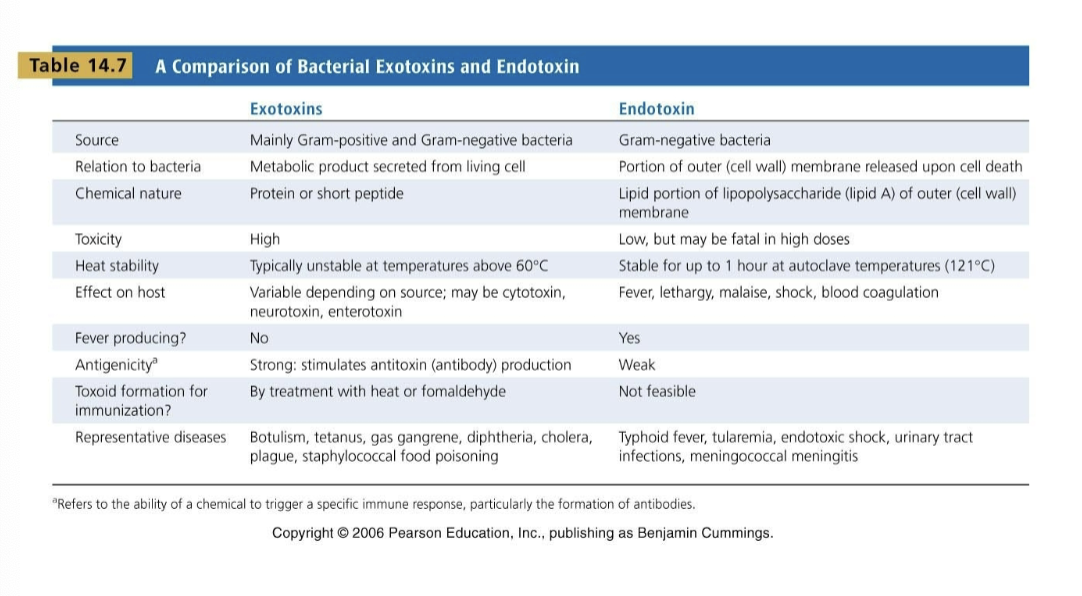
these are a few differences between exotoxins and endotoxins