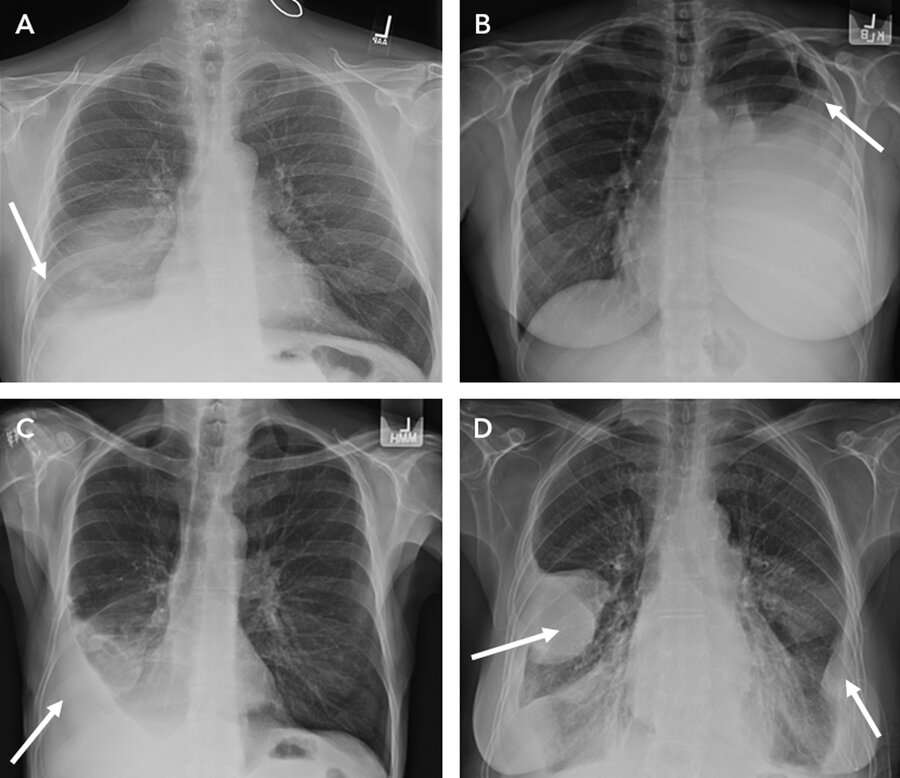
Pleural Effusion and Pneumothorax
1/6
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
7 Terms
What are the 2 main pathologies for pleural disease?
Pleural effusion and pneumothorax.
What is the first test to perform and evaluating pleural effusion?
What is more sensitive than that imaging study?
Outline the indication for thoracentesis.
Chest x-ray.
Ultrasound, particularly in semirecumbent/supine patient's.
Pleural fluid of unknown cause greater than 1 cm
Pleural fluid analysis:
– MOA of transudative effusion.
– MOA of exudative effusion.
Outline lights criteria.
When thoracentesis is done, in addition to Gram stain and cultures, why do we need the following labs:
– Cell count/differential?
– pH/glucose level?
– Pleural triglyceride level?
– Pleural amylase level?
Hydrostatic and oncotic pressure and balances typically in heart failure and cirrhosis.
Inflammation causes increased capillary permeability and reduced lymphatics.
LIGHTS:
A) 1/more of the following 3:
– Ratio of pleural fluid protein to serum protein greater than 0.5
– Ratio of pleural fluid LDH to serum LDH greater than 0.6
– Pleural fluid LDH greater than 2/3 upper limits serum LDH.
B) pleural cholesterol greater than 55.
C) ratio of pleural cholesterol to serum cholesterol greater than 0.3.
– Neutrophil predominance suggest parapneumonic effusion [2/2 PNA]. Lymphocyte predominance suggest cancer or tuberculosis.
– A pH less than 7.2 in a parapneumonic effusion = complicated pleural effusion. Chest tube drainage needed. If pleural glucose is less than 60, it supports complicated parapneumonic effusion/empyema or malignancy.
– Triglyceride of pleural fluid greater than 110 suggest chylothorax.
– Pleural amylase levels if there is concerns for effusion 2/2 pancreatitis.
What is a parapneumonic effusion [PNApneumonic effusion][?
At what point is it considered empyema?
What is the treatment for empyema/complicated parapneumonic effusion?
Pleural effusion due to PNA.
If effusion is complicated [bacteria invades pleural space] and infection starts resulting in purulent fluid and confirmatory Gram stain, this is empyema.
Drainage is required if stains come back remarkable, or if pH is less than 7.2. Drainage can either be via chest tube or via VATS. Combined use of tPA dornase warranted.
In patients with malignant pleural effusion, how do you treat?
Treat with indwelling pulmonary cath or chemical pleurodesis with talc. Do not place cath if poor prognosis of less than 3 months. May repeat thoracentesis for symptomatic improvement.
3 most common causes of recurrent nonmalignant pleural effusion?
Heart failure, cirrhosis and kidney failure.
What are the 2 main causes of pneumothorax?
What is the difference between primary spontaneous versus secondary spontaneous?
Which has a higher recurrence rate?
At what point is tension pneumothorax considered?
What is the initial diagnostic test and what classifies a large pneumothorax?
What is signs seen in ultrasound?
What is the management of tension pneumothorax?
When should prevention recurrence be considered for PSP and SSP? What are the options for recurrence prevention?
Spontaneous VS trauma.
PSP in patients without lung disease, SSP in patients with lung disease like COPD.
SSB.
When there is hemodynamic compromise: Hypotension, absent breath sounds, tracheal deviation.
Chest x-ray, if margin pulls away greater than 2 cm, this is large.
Sliding lung sign, absent/lung point suggest pneumothorax.
Needle decompression and thoracostomy/chest tube placement.
On the second pneumothorax and PSP patient, and the first one and SSP patient.
Chemical pleurodesis with tPA dornase, mechanical pleurodesis with VATS/CT surgery.