Actions
1/54
Earn XP
Description and Tags
Action
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
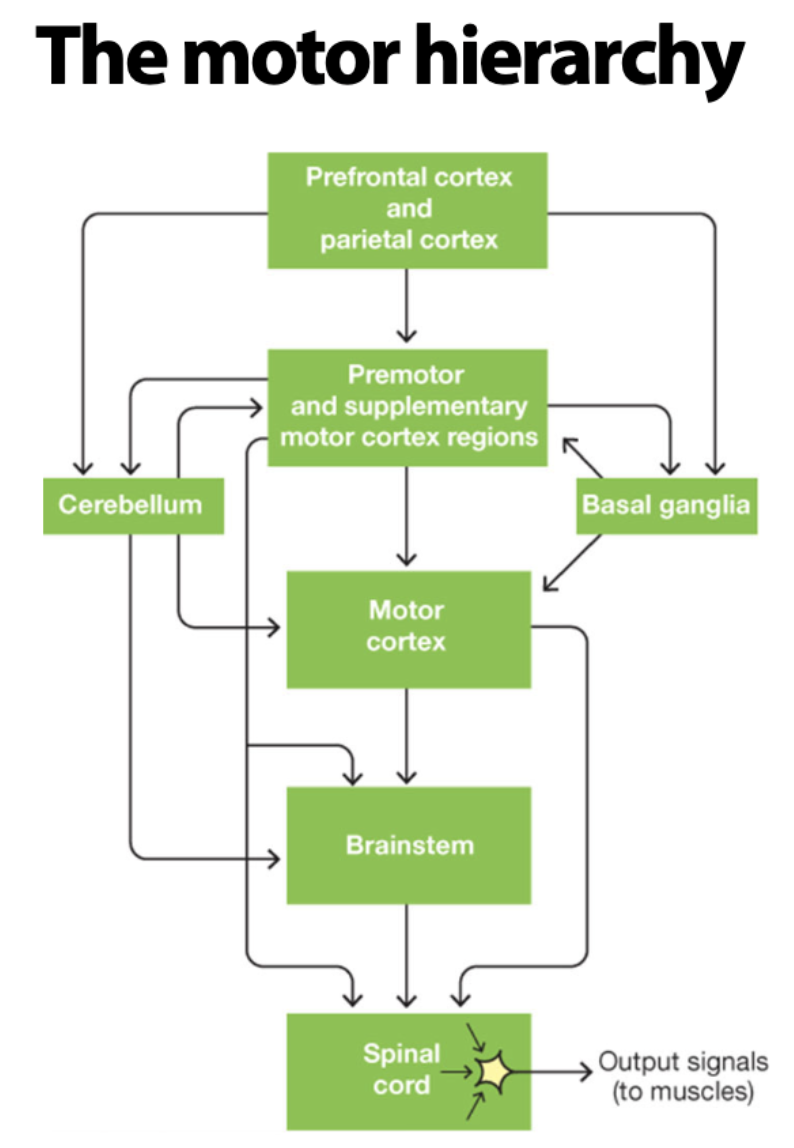
What is the Motor Hierarchy?
Literally just the traveling path of signals to create action in the body.
Top Part of the Motor Hierachy
Cortical Associations, Premotor, and Supplementary Motor Areas in the brain.
Translates intentions and goals into action plans and movement patterns.
Middle Part of the Motor Hierarchy
Primary Motor Cortex, Brainstem, Basal Ganglia, and Cerebellum Areas in the brain.
Converts action plans and movement patterns into commands for the muscles.
Bottom Part of the Motor Hierarchy
Spinal Motor Neurons and Spinal Sensory Neurons in the Spinal Cord.
Innervate muscles and combine to produce simple reflexes.
Motor Hierarchy Diagram
What is Muscle Innervation?
The process by which nerves supply muscles, allowing them to contract and relax through signals sent from the nervous system.
Antagonist Pairs
Flexor and Extensors - If one muscle is flexed/contracted, the other is extended/relaxed.
Neurotransmitter for Muscle Contraction
Acetylcholine released by firing of alpha motor neurons
Force of Muscles - Determiner
Firing frequency of alpha motor neurons and number of muscle fibres.
Alpha Motor Neurons
Originating in the spinal cord, specifically the ventral horn, and exits through the ventral root.
Muscle Spindles
Detect the stretch/contraction of the muscle.
Process of Postural Stability & Stretch Reflex (Hammer Example)
Hammer hits knee → Causes relaxation in knee.
Muscle spindle detects relaxation → Sends signal to counterbalance this relaxation.
Sensory neurons in muscles go up dorsal root to the dorsal horn, then through interneuron to the alpha motor neurons.
Alpha motor neuron exits ventral horn, then ventral root, to muscle.
Releases acetylcholine to contract the muscle and results in the stretch reflex and thus postural stability.
Gamma Motor Neurons
The use of these is to keep the muscle spindle taunt to be able to detect any changes.
Without this the muscle spindle would be slack and unable to detect changes like overstretching.
Flexor/Extensor Inhibitory vs Excitatory
Inhibitory signals relax the muscle, excitatory signals contract the muscle.
Spinal Patterns of Movements
There are certain patterns in the spinal cord that the brain simply activates such as walking - doesn’t require the brain to fully monitor it.
12 Cranial Nerve are Important For:
Breathing, eating, eye movements, facial expressions, etc. Critical Reflexes!
Key Structure in the Brainstem
Substantia Niagra, Vestibular Nuclei, Reticular Formation Nuclei.
Extrapyramidal Tracts
Projections to the spinal cord responsible for functions such as controlling posture, muscle tone, and movement speed.
Cerebellum Information
Contains 75% of all neurons in the CNS.
Important for error correction (forward models).
Damage results in ataxia: deficit in controlling coordinated movements and maintaining balance.
Basal Ganglia Information
Contains 5 nuclei with outputs to the cortex via the thalamus.
Key role in movement selection and initiation (gating function).
Damage can result in Parkinson’s or Huntington’s disease.
Primary Motor Cortex (M1/BA4)
Key area for motor initiation and activation of lower levels.
Main output: pyramidal (corticospinal) tract.
Secondary Motor Areas
Key areas for movement planning and control.
Premotor cortex (lateral part of BA6)
Supplementary Motor Area (medial part of BA6)
Additional Key Cortical Areas
Broca’s Area (BA 44/45)
Inferior Parietal Lobule (BA 39/40)
Superior Parietal Lobule (BA 5/7)
Frontal Eye Fields (BA8)
Primary Motor Cortex (M1)
Key area for motor initiation. Controls the contralateral side via the corticospinal tract. Injury leads to Hemiplegia.
Hemiplegia
Loss of control of movement on contralateral side.
Somatotopic Organization of M1
Different regions of the primary motor cortex represent different parts of the body.
This representation is coarser than in the somatosensory cortex (S1).
This representation can be mapped with MRIs and TMS.
Secondary Motor Areas
Premotor Cortex & Supplementary Motor Area.
Both involved in planning and control of movements.
Premotor Cortex
It has connections with the parietal cortex (spatial location) and important for sensory guided movement sequences.
Supplementary Motor Areas
It has connections with the medial frontal cortex (preferences and goals), important in deciding which object to choose and for memory-guided sequences.
Two Dorsal Streams to Premotor Cortex
Dorso-Dorsal & Ventro-Dorsal!
Dorso-Dorsal Stream
All about reaching!!! Optic Ataxia (inability to reach through vision) if damaged.
From SPL (Superior Parietal Lobule).
Ventro-Dorsal Stream
All about transitive (manipulation of objects) & intransitive (signifying intentions) gestures! Apraxia (inability to use objects and link gestures to meaningful actions) if damaged.
From IPL (Inferior Parietal Lobule).
Parietal Links To…
Motor Intention
Premotor Links To…
Motor Execution
SMA Lesions Result In…
Impairment of actions with both hands required.
Also results in Alien Hand Syndrome
Alien Hand Syndrome
A limb does something, but the individual denies responsibility to it.
If corpus callosum is lesioned, the hands can still work together.
Mirror Neurons
Activated by both doing and seeing expected, goal orientated actions.
Mirror Neurons Debate:
Activation for understanding actions? Or only from the priming effect (reflecting automatic action planning when a familiar stimuli is present).
Basal Ganglia
The gatekeeper! Key in movement initiation.
Basal Ganglia Direct Pathway
Cortex activates Striatum which sends inhibitory signal to the Internal Globus Pallidus (GPi) which sends an inhibitory signal to the thalamus which then sends an excitatory signal to the cortex.
Activates Cortex & Starts Movement
Basal Ganglia Indirect Pathway
Cortex activates Striatum which sends an inhibitory signal to the External Globus Pallidus (GPe) which either sends a less inhibitory signal to the GPi OR goes to the Subthalamic Nucleus (STN) which sends an excitatory signal to GPi.
Both paths result in a stronger inhibition of the thalamus, leading to…
Inhibits Cortex & Stops Movement
Basal Ganglia Pathways Diagram
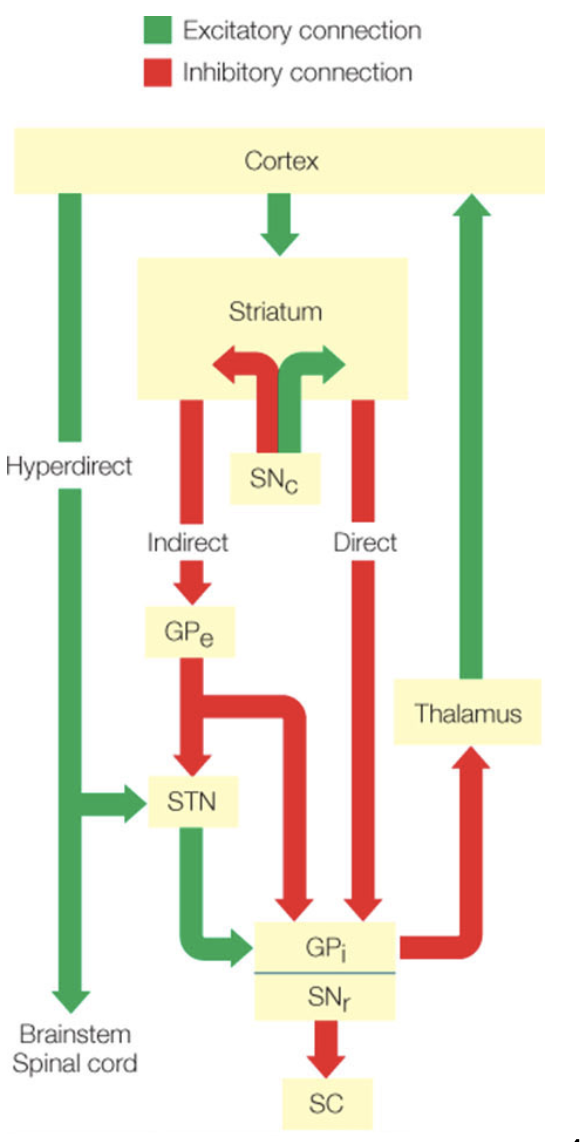
Basal Ganglia Disorders
Huntington’s Disease & Parkinson’s Disease
Huntington’s Disease
Reduced inhibition of the indirect pathway, meaning the GPe becomes very strong, which highly inhibits the GPi, meaning the signal sent to inhibit and stop movement to the thalamus is weak, so the thalamus then becomes strong because nothing inhibits it, so there is hyperkinesia!
Huntington’s Disease: A neurodegenerative and genetic disorder that results in clumsiness, hyperkinesia, chorea, and abnormalities in normal mental attitude.
Parkinson’s Disease
Opposite of Huntington’s disease! The signal from the cortex to the GPe is extremely strong, meaning the signal from GPe to the GPi is weak, so the GPi is extra strong and highly inhibits the thalamus, meaning that there is not very much activation of the cortex, so very little movement.
Parkinson’s Disease: Involved with hypokinesia and bradykinesia.
Akinesia
A = Not, Kinesia = Movement, thus Akinesia = Inability to voluntarily move.
Hyperkinesia
Hyper = Excessive, thus Hyperkinesia = Excessive movements.
Hypokinesia
Hypo = Under, thus Hypokinesia = reduced ability to initiate movements.
Bradykinesia
Brady = Slow, thus Bradykinesia = slow movements.
Forward Model
About how our motor system makes predictions of the anticipated sensory consequences of the movement.
Efference Copy
A copy of the movement is sent from the cortex to the muscles which is used to make predictions.
Sensory Prediction Error
When the predicted and actual sensory feedback do not match, there is learning!
Key Structure for Forward Models
Cerebellum - Involved in the prediction that are temporarily precise (one debate).
Habitual Learning is Controlled by What?
The subcortex! With enough learning motor controls shift from the cortex to the subcortex (such as the cerebellum and basal ganglia).
Population Vector
The sum of preferred directions of neurons.