DSA27 - Sleep Disorders
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
Period in which the brain is engaged in several necessary activities:
-2 stages = Non-REM & REM
-"Cleans out brain"
Describe "Sleep"
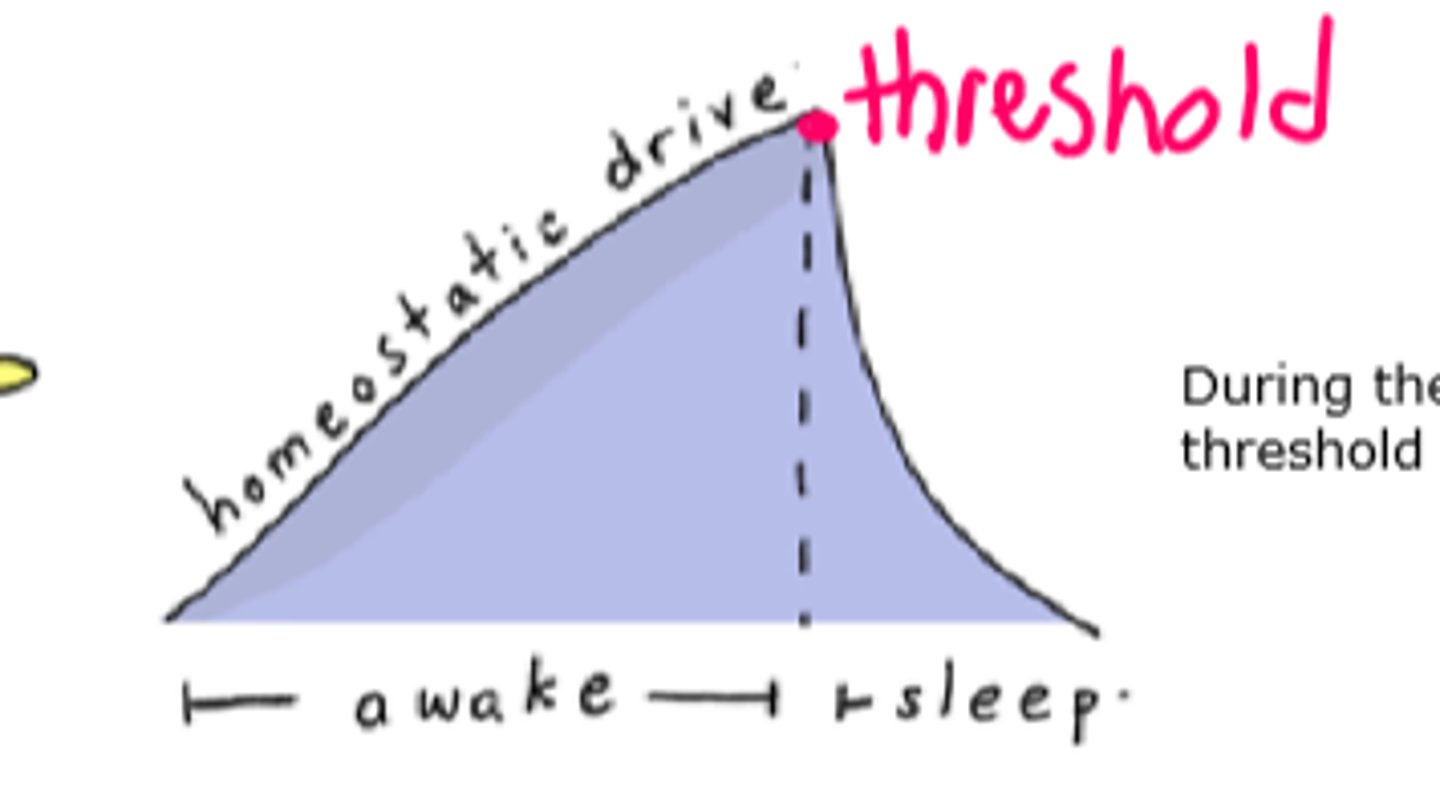
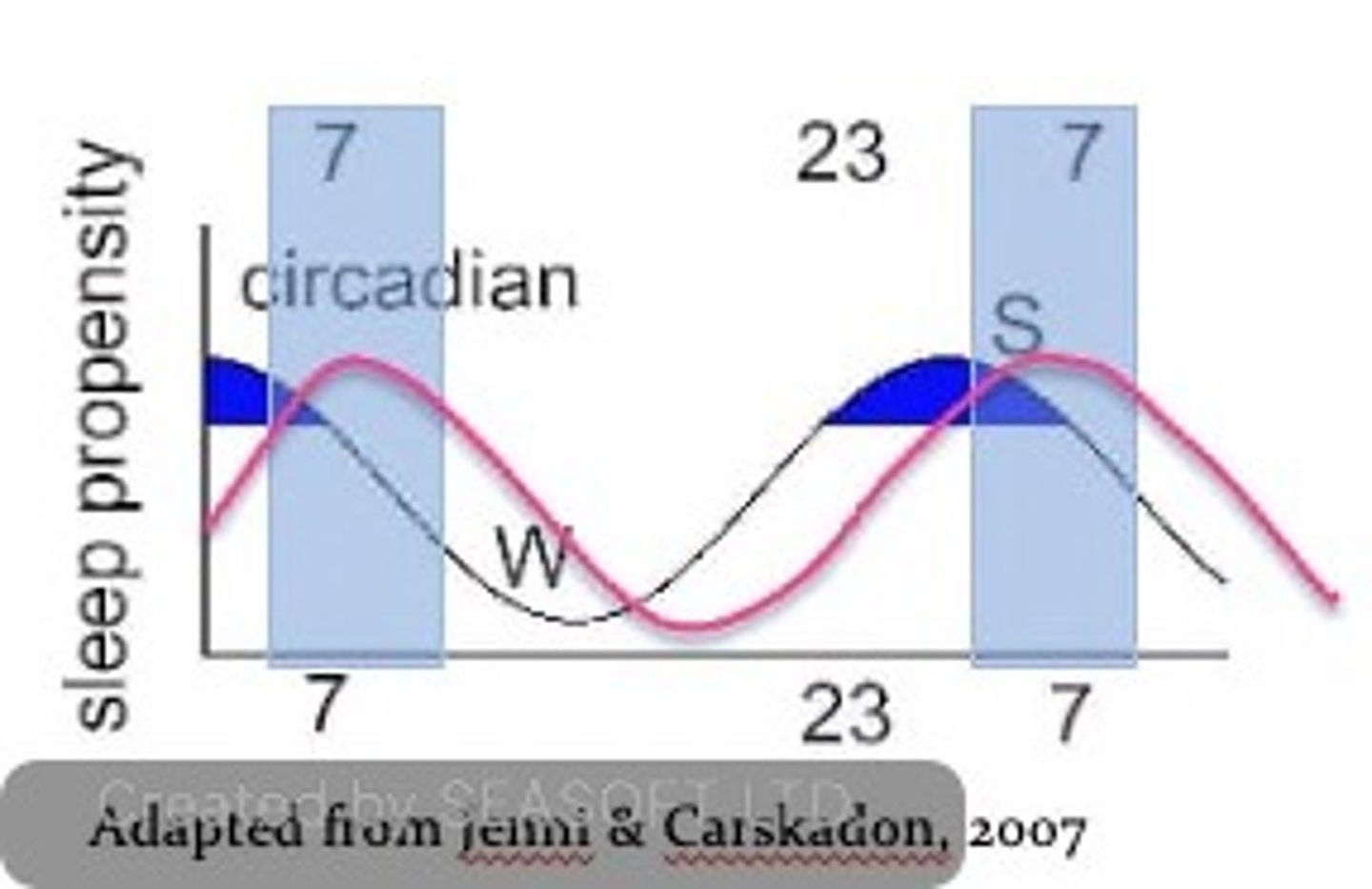
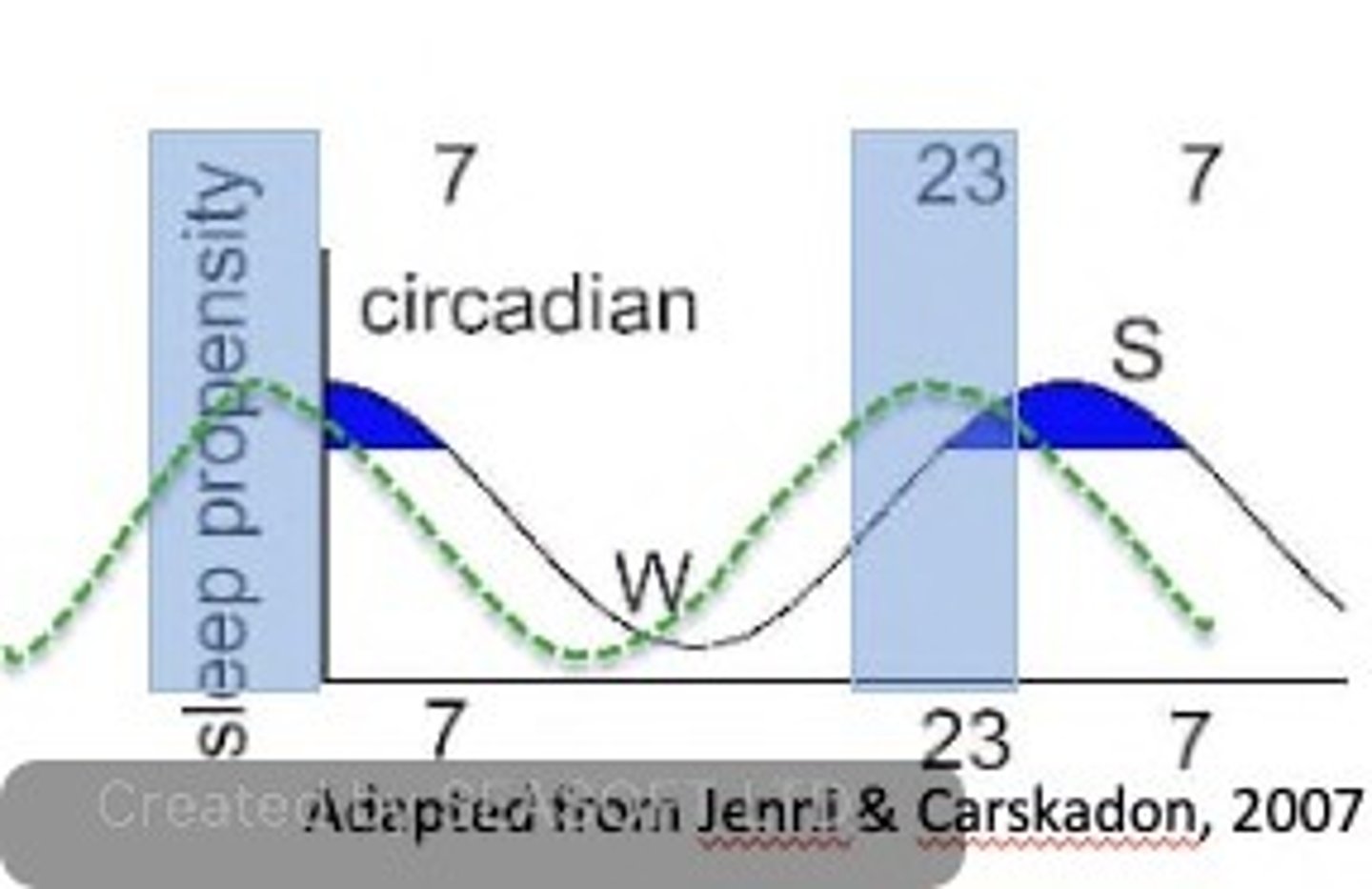
Sleep-wake DEPENDENT process of sleep/wake regulation; influenced by the DURATION OF WAKEFULNESS (longer you're awake --> more pressure built for sleep)
Define the Homeostatic Sleep Drive
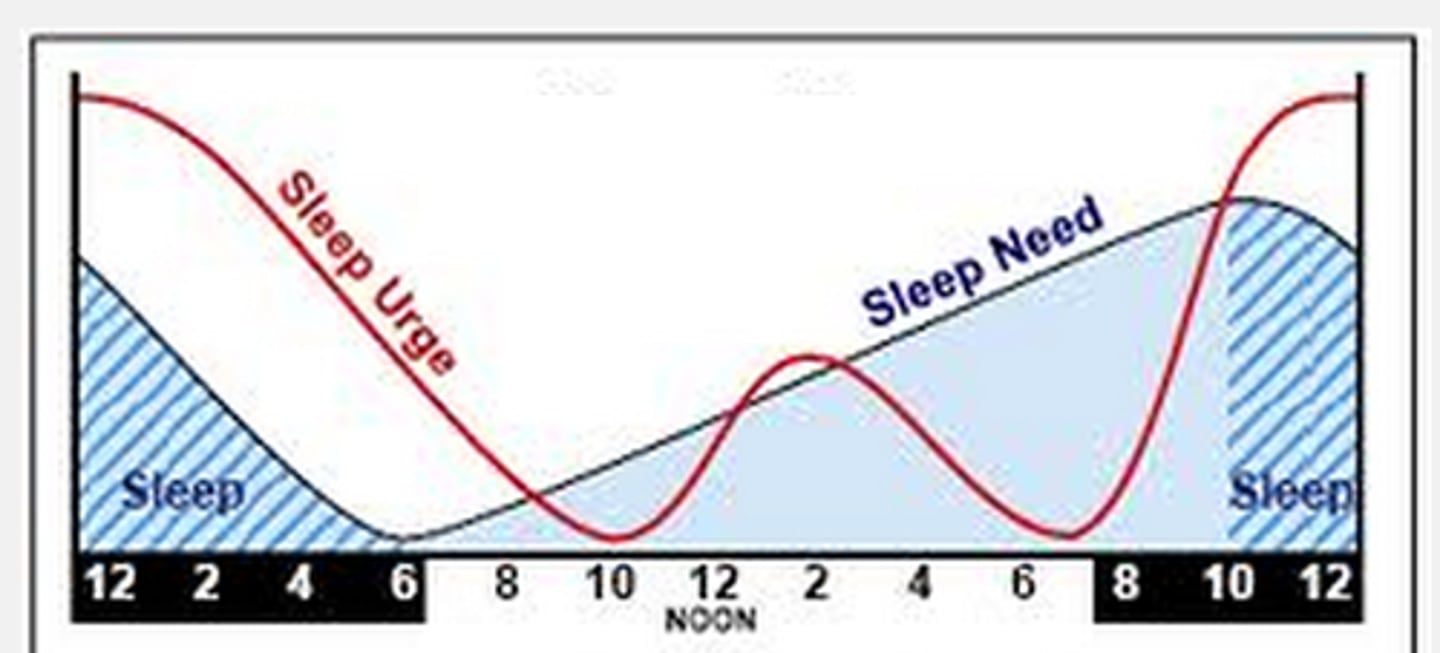
Sleep-wake INDEPENDENT process of sleep/wale regulation; Transmits stimulatory signals to AROUSAL networks to PROMOTE WAKEFULNESS IN OPPOSITION to homeostatic drive for sleep (regulates SLEEPINESS and ALERTNESS)
Define the Circadian Biological Clock Process
•Histaminergic cells in the tuberomammillary nucleus (TMN) in the posterior hypothalamus
•Norepinephrine-producing neurons in the locus coeruleus (LC) (norepinephrine)
•Serotonergic neurons in the dorsal raphe nuclei (DRN)
•Dopaminergic neurons in the ventral tegmental area (VTA)
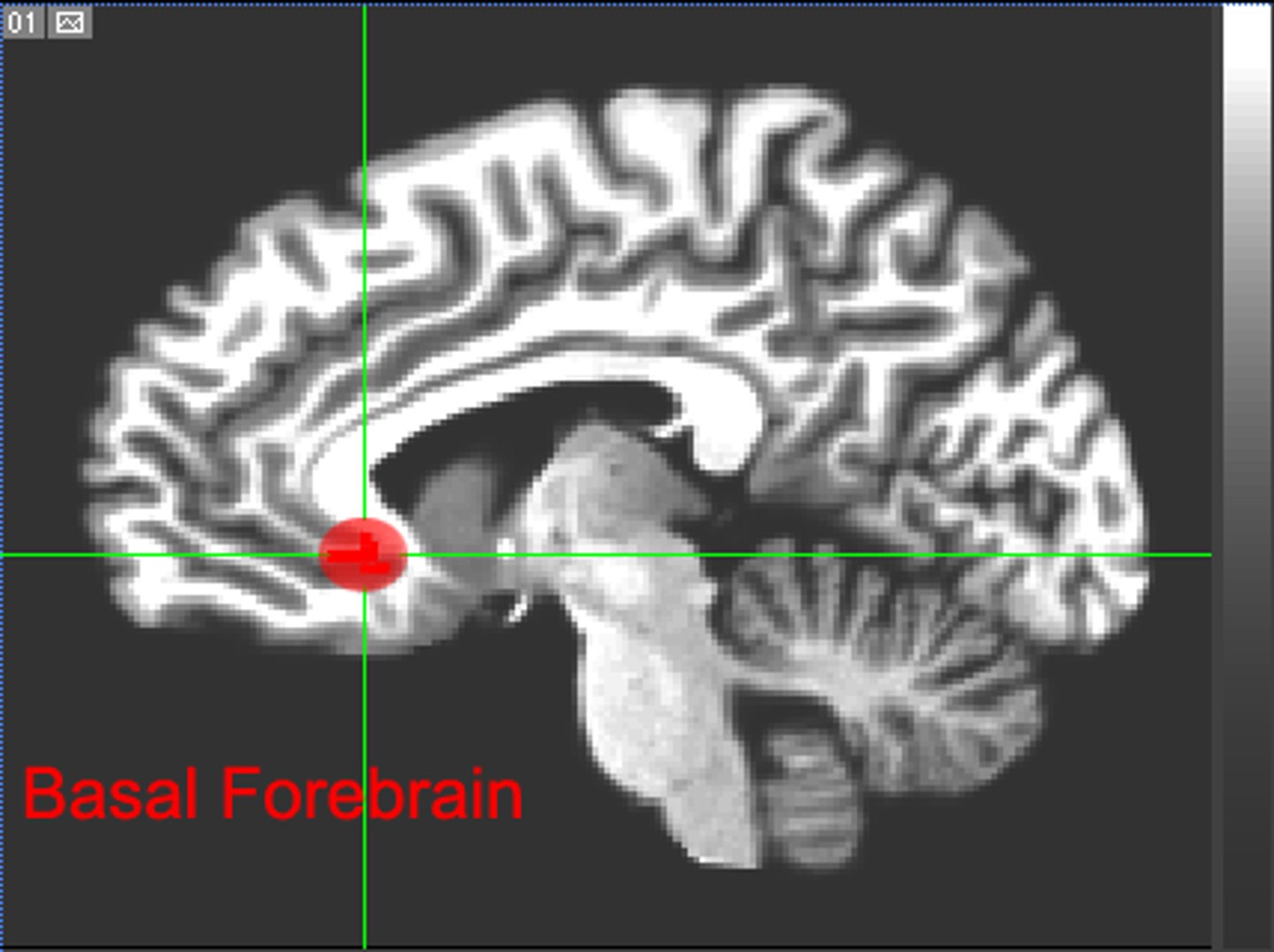
•Cholinergic neurons of the basal forebrain (acetylcholine)
What area(s) of the brain is/are responsible for the function of the WAKEFULNESS from the Circadian Biologic Clock?
Active during wakefulness and project to all of the wakefulness arousal systems:
•They interact with both the sleep-active and the sleep-promoting systems and act as STABILIZERS between wakefulness-maintaining and sleep-promoting systems to prevent sudden and inappropriate transitions between the 2 systems (what malfunctions in Narcolepsy w/ Cataplexy)
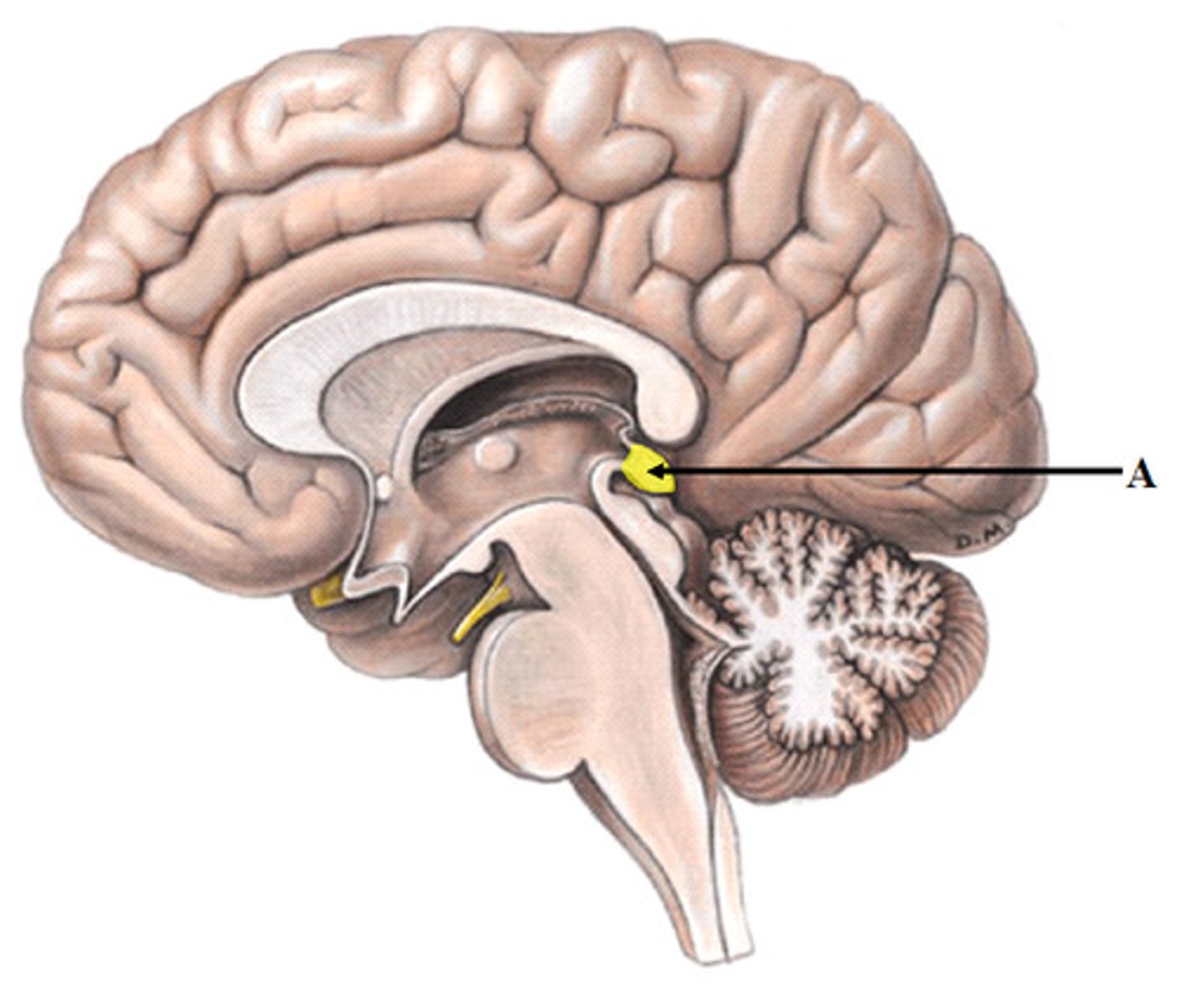
What is the function of the Hypocretin neurons in the posterolateral hypothalamus?
Suprachiasmatic nucleus (SCN) in Hypothalamus = clusters of thousands of cells that receive information about light exposure directly from the eyes by way of the retinal ganglion cells:
•The retinal ganglion cells transmit light signals via the retinohypothalamic tract to stimulate the SCN.
•The SCN projects to the pineal gland to produce or stop producing melatonin by way of a multi-synaptic pathway.
What area(s) of the brain is/are responsible for the function of the SLEEPINESS from the Circadian Biologic Clock?
Receives signals from the SCN and increases production of the hormone melatonin, which is a “night hormone" (lets body know it's "night time")
What is the function of the pineal gland in the Circadian Biologic Clock?
Synthesis is inhibited by light and stimulated by darkness (The nocturnal rise in melatonin increases between 8 and 10 pm and peaks between 2 and 4 am, then declines gradually over the morning)
Explain how Melatonin synthesis works
alerting signal; SCN clock
Melatonin acts via 2 specific melatonin receptors: MT1 attenuates the () and MT2 phase shifts the ()
•Dyschronization of the circadian clock --> Sleep erratically throughout the day because they are unable to match their circadian rhythms with the light-dark cycle.
•Most blind people maintain some ability to sense light and are able to modify their sleep/wake cycle
What happens if the SCN becomes damaged?
By taking small amounts of melatonin at the same time each day (peaks and valleys over time can help match the natural circadian rhythm)
How might those who lose their sight coordinate their wake-sleep cycle?
Communicates with the hypothalamus to control the transition between wake and sleep:
•Sleep-promoting cells within the hypothalamus and the brain stem produce GABA and galanin, which acts to reduce the activity of arousal centers in the hypothalamus and the brain stem
•Sends signals to relax muscles essential for posture and limb movement --> causes muscle atonia (so we don't act out our dreams)
What is the function of the brainstem in the Circadian Biologic Clock?
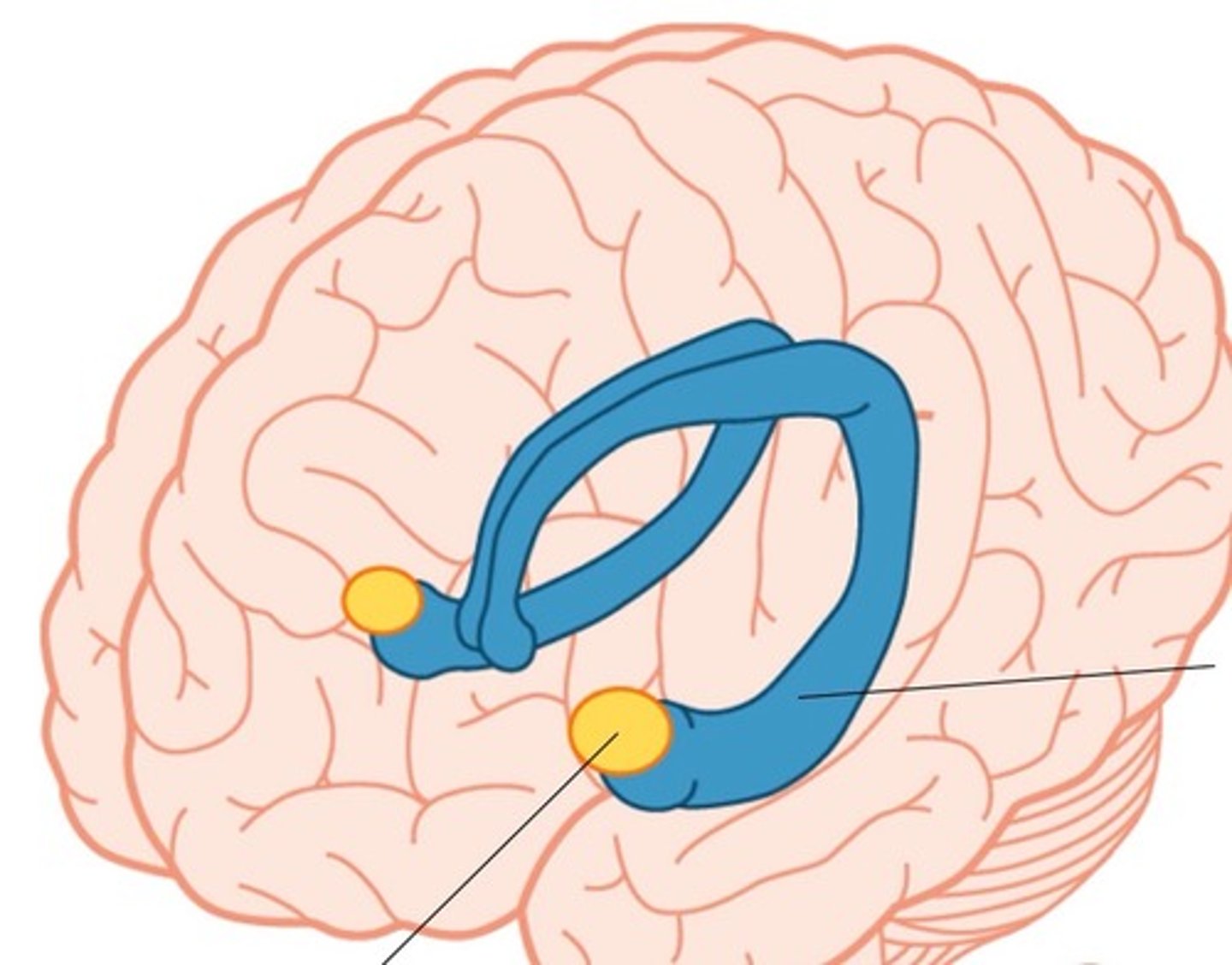
Acts as a relay for information from the senses to the cerebral cortex (the covering of the brain that interprets and processes information from short- to long-term memory):
-Most Sleep stages = Quiet Thalamus
-REM Sleep = Active Thalamus (sends cortex images, sounds, sensations for dreams)
What is the function of the thalamus in the Circadian Biologic Clock?
•Promotes sleep and wakefulness, while part of the midbrain acts as an arousal system.
•Release of adenosine (a chemical by-product of cellular energy consumption) from cells in the basal forebrain and other regions supports your sleep drive --> Caffeine counteracts sleepiness by blocking the actions of adenosine.
What is the function of the basal forebrain in the Circadian Biologic Clock?
More active during REM sleep (involved in processing emotions)
What is the function of the amygdala in the Circadian Biologic Clock?
zeitgebers ("time givers")
External stimuli that synchronize the circadian system are called [], with light being the most powerful.
Other include sleep-wake cycles, activity patterns, meal timing, and social schedules (work/leisure).
2–3
The hormone melatonin also plays a role in adjusting circadian timing.
Light and other zeitgebers entrain the master clock (SCN), which in turn synchronizes peripheral clocks.
Full synchronization to new conditions typically takes () days.
Type 2 Diabetes (b/c increases insulin resistance)
Given that the sleep cycles are highly connected to the endocrine system's functionality, what is often a first long-term complication that can appear from sleep disorders?
bidirectional
The relationship between the circadian system and these zeitgebers is (): circadian rhythms affect, and are affected by, environmental and behavioral cues.
An increase in body temperature is seen during the course of the day and a decrease is observed during the night
What effect does Body Temperature have on the Circadian Rhythm?
-Prolactin
-Testosterone
-GH
What hormones demonstrate circadian rhythms (max secretion at night)?
DIURNAL distribution (max levels in morning)
What kind of rhythm does Cortisol secretion exhibit?
4-6
NREM Sleep and REM Sleep occur in alternating cycles, each lasting approximately 90-100 minutes, with a total of () cycles
-Drowsiness or presleep (first or earliest stage of sleep)
-Transient and makes up 2-3% of total sleep time
-Non-restorative
Describe Stage NREM 1 (N1) Sleep
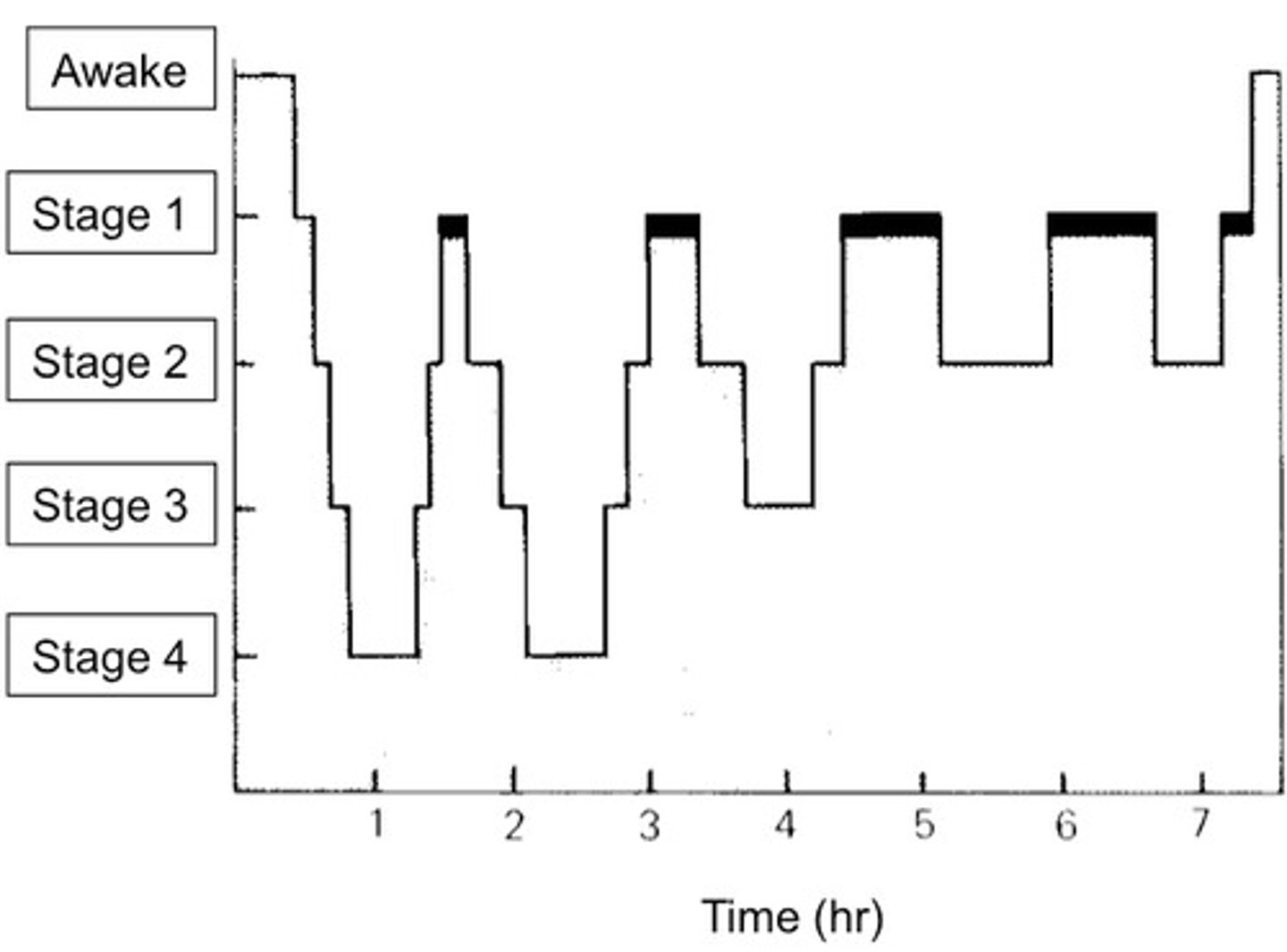
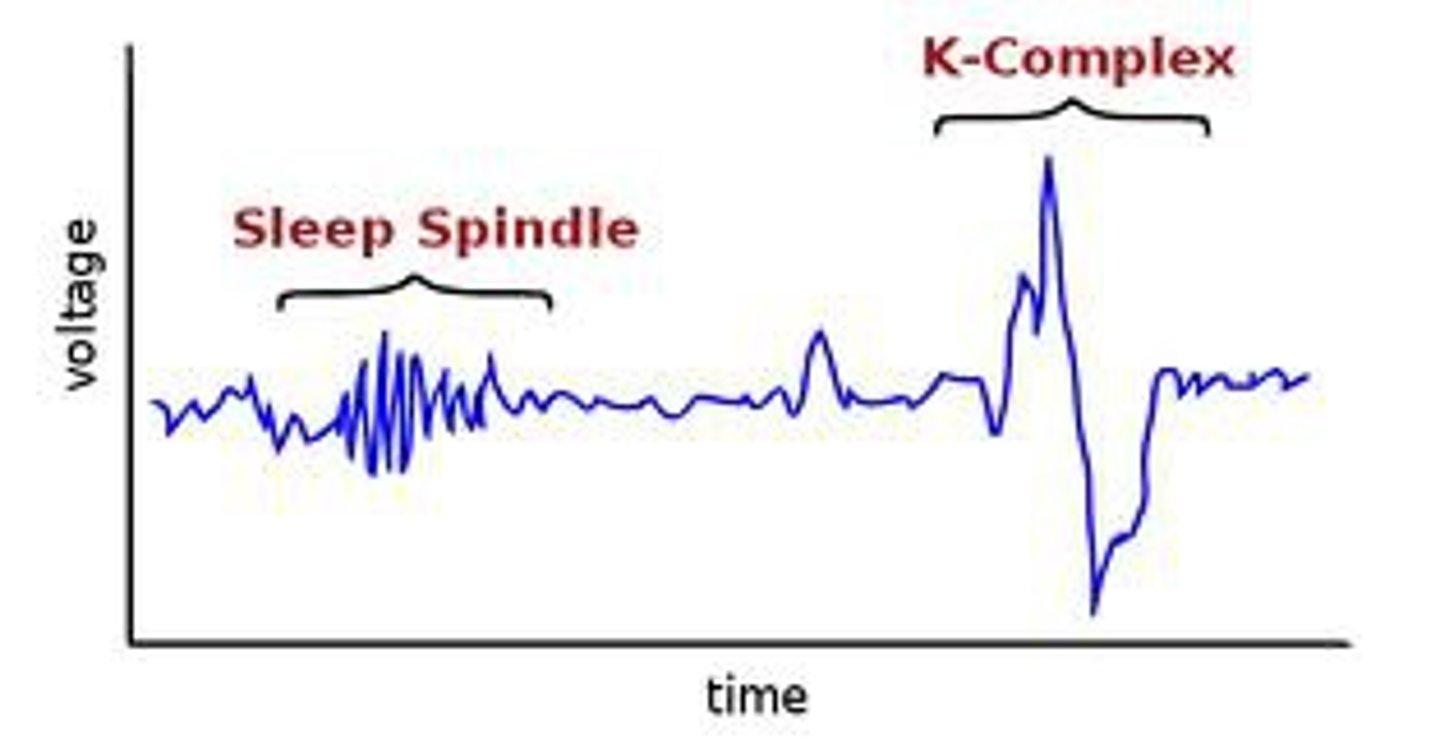
•Spend approximately 50% OF TOTAL SLEEP.
•EEG criterion = SLEEP SPINDLES and K COMPLEXES.
> Sleep spindles = frequency of 12-16 Hz (typically 14 Hz); occur in short bursts of waxing and waning spindle-like (fusiform) rhythmic activity
> K complexes = high amplitude biphasic, and transient and are often associated with sleep spindles.
Describe Stage NREM 2 (N2) Sleep
•AKA "slow wave sleep" or "delta sleep."
•Slow wave sleep (SWS) = deepest and MOST RESTORATIVE stage of sleep; constitutes approximately 22% OF TOTAL SLEEP.
Describe Stage NREM 3 (N3) Sleep
-Confusional arousals
-Night terrors (pavor nocturnus)
-Sleepwalking (somnambulism)
What are some slow sleep parasomnias that can occur during N3 Sleep (may be confused w/ seizures)?
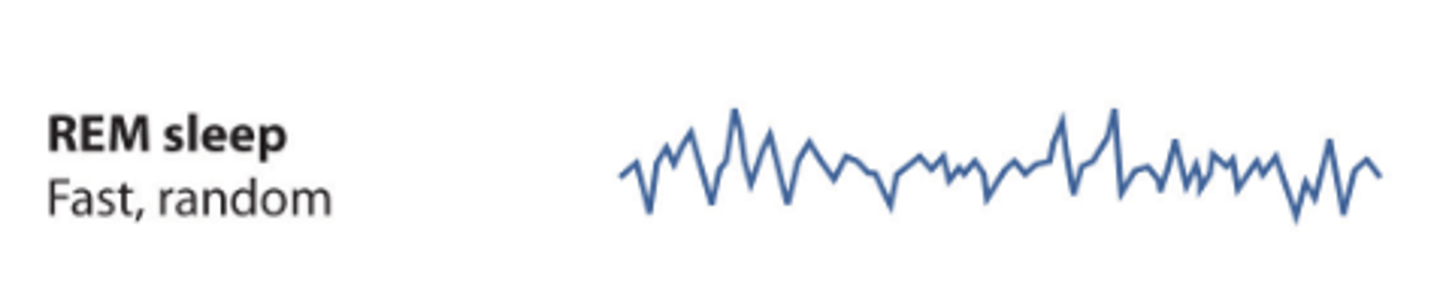
First stage identified due to the ability to do so without equipment:
(1) RAPID EYE MOVEMENT
(2) MUSCLE ATONIA
(3) EEG DYSYNCHONIZATION (compared to slow wave sleep).
Describe Stage REM Sleep
ACTIVITIES prior to bedtime
BED PARTNER history
CONSEQUENCES on waking functions, way of life
DRUG regimens
EXACERBATING or relieving factors (noises, lights, temperature, accessible stimulation)
FREQUENCY and duration of sleep
GENETIC factors or family history
HABITS
What questions should be asked when taking a Sleep Hx?
-Can suppress REM
-Cause Drowsiness
How might Anti-depressants alter sleep?
Cause Drowsiness
How might Pain medications and Antihistamines alter sleep?
Suppress the drive to sleep
How might Stimulants (includes caffeine) alter sleep?
Tests for Idiopathic Hypersomnia/Narcolepsy:
-The patient is given five chances to nap during the day. For each nap opportunity, they have up to 20 minutes to try to fall asleep.
-Each nap is scheduled every 2 hours (e.g., 9 AM, 11 AM, 1 PM, etc.).
-During each nap, how long it takes the person to fall asleep is measured — this is called sleep latency (Shorter latencies may indicate excessive sleepiness)
-If a patient enters REM sleep during one of these short naps, it’s called a SOREM (Sleep-Onset REM period), which is unusual and may suggest conditions like narcolepsy.
How does the Multiple Sleep Latency Test (MSLT) work? What does it test for?
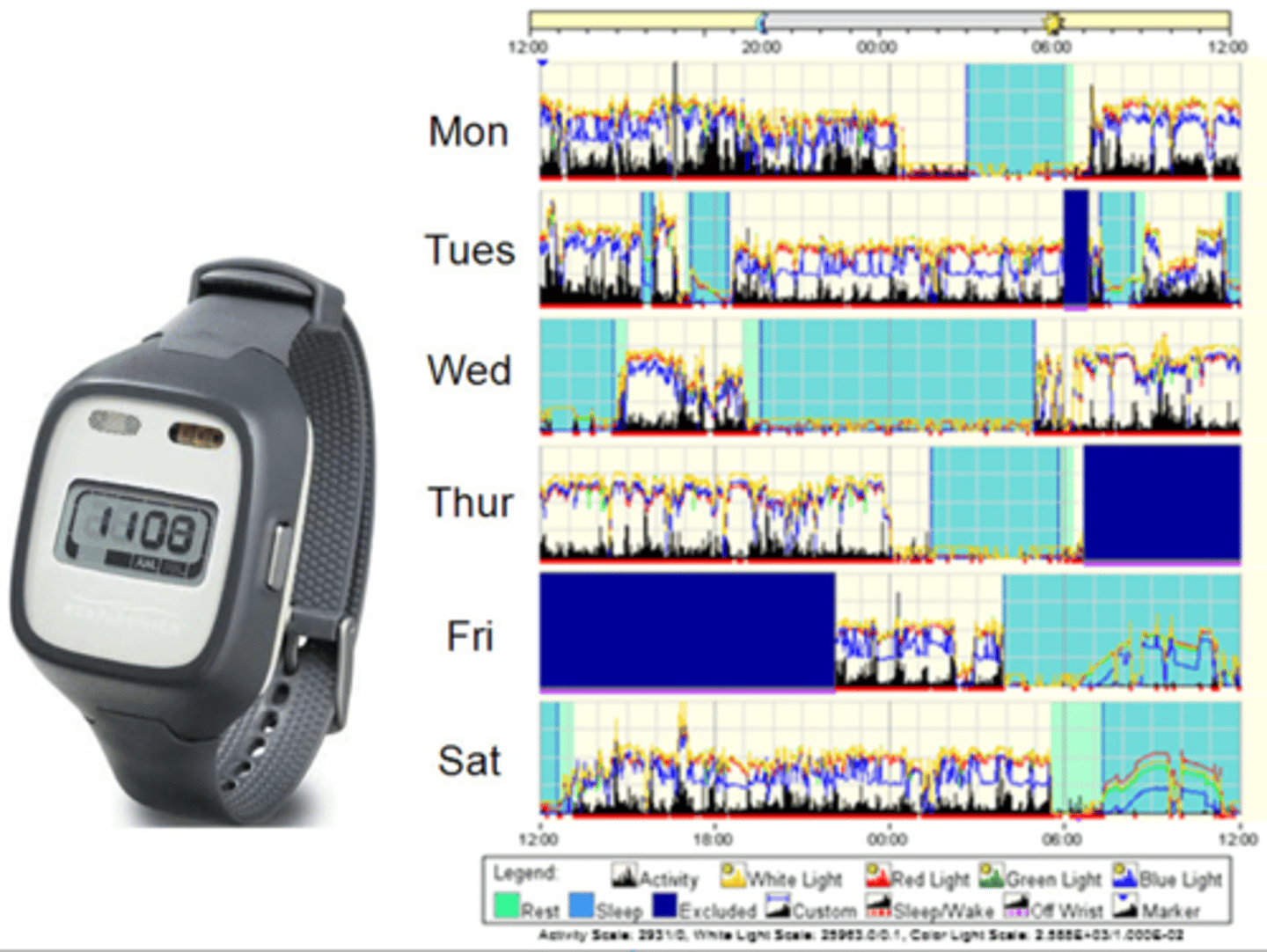
Activity monitor worn on wrist to count activity --> uses algorithm to approximate amount of pt's sleep
What is the purpose of an Actigraphy?
> WHIIRS (Women’s Health Initiative Insomnia Rating Scale) – Insomnia symptoms
> ISI (Insomnia Severity Index) – severity of insomnia symptoms
> STOP-BANG – OSA symptoms
> IRLS (International Restless Legs Scale) – RLS symptoms
> JHRLSS (Johns Hopkins Restless Legs Severity Scale) – RLS symptoms
> ESS (Epworth Sleepiness Scale) – daytime sleepiness
> PDSS (Pediatric Daytime Sleepiness Scale) – daytime sleepiness in pediatrics
> FSS (Fatigue Severity Scale) – fatigue symptoms
> MEQ (Morningness Eveningness Questionnaire) – sleep phase preference
What are some sleep scale questionnaires that can be used to evaluate for Sleep Disorders? What exactly do they evaluate?
Insomnia Disorder
Define Condition:
Number of symptoms that interfere with duration and/or the quality of sleep despite adequate opportunity for sleep (Acute < 3 mo & related to stress/changes in sleep schedule; Chronic > 3 mo to years + reduced QOL and Inc risk of Psych Illness)
-Sx:
◦Difficulty initiating sleep
◦Occurs at least 3 days a week
◦Causes significant distress
◦Frequent nocturnal awakenings
◦Early morning awakenings
◦Waking up feeling fatigued
-Path:
◦Doesn’t occur due to another disorder
◦Not due to medication or substances
◦Coexisting mental and medial disorders do not adequately explain the insomnia.
-Tx:
◦Sleep hygiene
◦CBTI
◦Pharmacology
> Benzodiazepines
>> Reduce sleep latency
>> Works as well as CBTI for short period of times – not supposed to be used for long term efficacy
> Non-benzo hypnotics
>> Zolpidem, eszopiclone, and zaleplon
>> Short term treatment
>> Less day time sleepiness
> Antidepressants = Trazodone, amitriptyline, doxepin
> Antihistamines = Hydroxyzine, diphenhydramine
-Prog:
> Chronic --> reduced QOL and Inc risk of Psych Illness
-Manualized 6-8 wk sessions
-Works on Sleep Hygiene
-Address cognitive distortions around sleep/habits + techniques to help w/ insomnia
How does Cognitive Behavioral Therapy for Insomnia (CBT-I) work?
Hypersomnolence Disorder
Define Condition:
Excessive sleepiness despite at least 7 hours of sleep with at least 1 of the following:
-Sx:
◦Recurrent periods of sleep within the same day
◦Prolonged, non restorative sleep > 9 hours; difficulty being fully awake after awakening
◦At least 3 times a week for at least 3 months
◦Causes distress or impairment in functioning
-Hx:
◦Viral infections
◦Head trauma
◦Genetic
-Path:
◦Persistent course unless treated onset, between ages 15-25
◦Doesn't occur in the course of another sleep-wake disorder
◦No due to substance or medication
◦Other disorders don't adequately explain
-Tx:
◦Life long therapy with stimulants or modafinil
◦Scheduled napping
-Prog: Persistent course unless treated
Narcolepsy
Define Condition:
Type of Hypersomnolence Disorder - Excessive daytime sleepiness and falling asleep at inappropriate times:
-Sx:
◦Recurrent episodes of need to sleep
◦Lapsing into sleep
◦Napping during the day
◦Hallucinations or sleep paralysis at the beginning or end of sleep episodes are common
-Dx:
◦Occurring at least 3 times per week for at least 3 months associated with at least 1 of the following:
> Cataplexy (SUDDEN MUSCLE WEAKNESS/PARALYSIS) - VERY RARE (and often not in younger pts)
> Hypocretin deficiency in CSF
> Reduced REM sleep latency on polysomnography
-Hx:
> More in MALES
-Path: Linked to a loss of hypothalamic neurons that produce hypocretin - may be Autoimmune
-Tx:
◦Sleep hygeine
◦Scheduled daytime naps
◦Avoidance of shift work
◦For excessive daytime sleepiness
> Stimulants
> Modafinil
◦For cataplexy
> Sodium oxalate
> TCAs
> SSRI
-Prog:
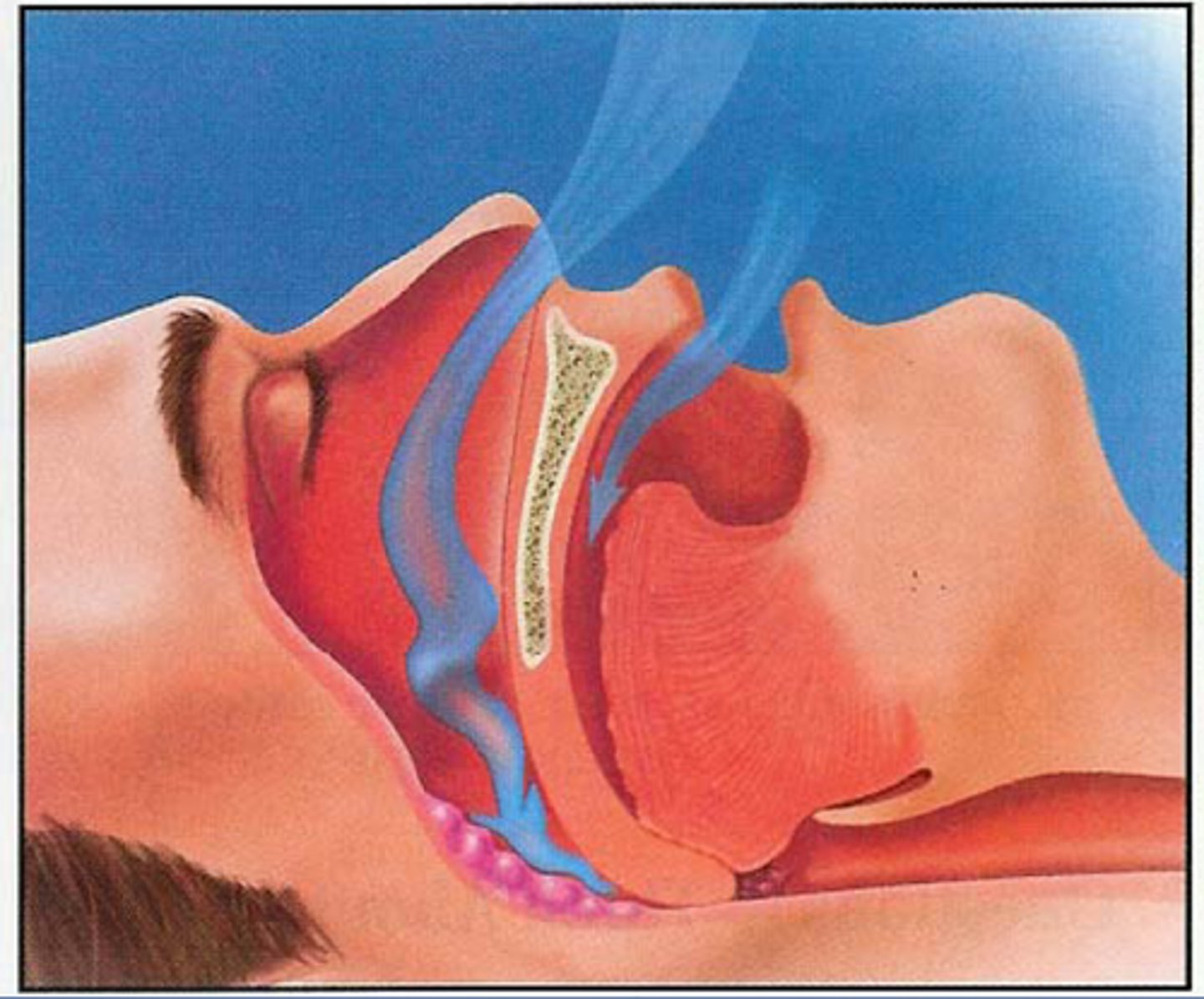
Obstructive Sleep Apnea Hypopnea (OSA) in ADULTS
Define Condition:
Apneic episodes characterized by cessation of breathing or hypopnea episodes of reduced airflow (>15/hour)
-Sx/PE:
◦Excessive daytime sleepiness
◦Sleep fragmentation
◦Snoring
◦Frequent awakenings with gasping or choking
◦Frequent Urination
◦Non-refreshing sleep
◦Morning headaches
◦HTN (Diastolic HTN)
-Hx:
> Obesity
> Inc Neck Circumference
> More in MALES (2:1 to 4:1), mainly OLDER Males (> 45)
> May have FHx
> Menopause if Female
> Craniofacial Abns
> Smoking, EtOH use
-Path/Prog: Lowers blood-oxygen levels + strain on the heart --> A/w cardiovascular problems and daytime sleepiness
-Tx:
> CPAP, BIPAP
> Wt. loss
> Exercise
> Surgery (Adenotonsillectomy, Uvulopalatopharyngoplasty Surgery (UPPP))
> Tursepatide (Tirzepatide = GLP-1 Agonist)
Obstructive Sleep Apnea Hypopnea (OSA) in CHILDREN
Define Condition:
Apneic episodes characterized by cessation of breathing or hypopnea episodes of reduced airflow (>15/hour)
-Sx/PE:
◦Excessive daytime sleepiness
◦Sleep fragmentation
◦Snoring
◦Frequent awakenings with gasping or choking
◦Frequent Urination
◦Non-refreshing sleep
◦Morning headaches
-Hx: Not as common, but some causes...
> Smaller Upper Airway (enlarged tonsils/adenoids)
> Obesity
> Craniofacial abns (Disorders or Genetic Conditions)
-Path/Prog: Lowers blood-oxygen levels + strain on the heart --> A/w cardiovascular problems and daytime sleepiness
-Tx:
> CPAP, BIPAP
> Wt. loss
> Exercise
> Surgery (Adenotonsillectomy, Uvulopalatopharyngoplasty Surgery (UPPP))
> Tursepatide (Tirzepatide = GLP-1 Agonist)
Central Sleep Apnea
Define Condition:
5+ apneas/hr of sleep
-Hx:
> Idiopathic, but RARE
> Cheyne-stokes Breathing (decreased EF, acute stroke)
> Opiate use
> More in MALES
-Tx:
◦Treatment of underlying conditions
◦ CPAP/BiPAP
◦ Supplemental O2
◦ Medications – acetazolamide, theophylline, sedative-hypnotics
Sleep-related Hypoventilation
Define Condition:
Seen on polysomnography - less respiration during sleep
-Hx:
> Medical/Neuro Disorders
> Med Use
> SUDs
-Sx/PE:
> Frequent arrivals
> Morning HAs
> Insomnia
> Excessive Daytime sleepiness
-Dx:
> Poly = Decreased Respiration
> Elevated CO2
-Tx:
> Treat underlying condition
> CPAP/ BiPAP
> Medication to stimulate/promote breathing (bronchodilations, Theophylline)
-Prog:
> Pulm HTN
> Cor Pulmonale
> Cardiac Arrhythmias
> Polycythemia
> Neurocognitive Dysfunction
> Resp Fail
Delayed sleep phase disorder
Define Condition:
Type of Circadian Rhythm Sleep Wake disorder - Chronic or recurrent delay in sleep-onset and awakening times with preserved quality and duration
-Tx:
◦ Timed bright light phototherapy
◦ Melatonin
◦ Chronotherapy ( delayed betimes by a few hours each night
Advanced sleep phase disorder
Define Condition:
Type of Circadian Rhythm Sleep Wake disorder - Normal duration and quality of sleep with sleep onset and awakening times earlier than desired
-Tx:
◦ Timed bright light phototherapy prior to bedtime
◦ Early morning melatonin nor recommended.
Shift-work disorder
Define Condition:
Type of Circadian Rhythm Sleep Wake disorder - Sleep deprivation and misalignment of the circadian rhythm secondary to nontraditional work hours
-Tx:
◦ Avoid risk factors
◦ Bright light phototherapy to facilitate rapid adaptation to night shift
◦ Modafinil may be helpful for patients with severe disease

Jet-lag disorder
Define Condition:
Type of Circadian Rhythm Sleep Wake disorder - Sleep disturbances associated with travel across multiple time-zones
-Tx:
◦ Disorder usually self-limiting
◦ Sleep disturbances generally resolve 2-3 after travel.
◦ Find a schedule “in the middle” --> adjust sleep schedule so there's a smaller shift in time change ==> actually allows for RESTORATIVE SLEEP time
Sleep Terrors
Define Condition:
Type of Parasomnia - sudden arousal from slow-wave sleep, accompanied by autonomic and behavioral manifestation of fear
-Hx: Seen in some children
-Path:
◦Disruption in sleep/wake schedule --> Insufficient sleep, underlying sleep disorder
◦Environmental stimulus (e.g., noises, lights)
-Sx/PE: Piercing scream or cry, accompanied by autonomic and behavioral manifestations of intense fear
-Tx:
◦ Treating underlying sleep disorder (if present)
◦ Sleep extension
◦ Scheduled awakenings

Sleepwalking
Define Condition:
Type of Parasomnia - series of complex behaviors during slow-wave sleep
-Hx: Seen in some children
-Path:
◦Disruption in sleep/wake schedule --> Insufficient sleep, underlying sleep disorder
◦Environmental stimulus (e.g., noises, lights)
-Tx:
◦ Treating underlying sleep disorder (if present)
◦ Sleep extension
◦ Scheduled awakenings

Nightmares
Define Condition:
Type of Parasomnia - Frightening dreams resulting in an awakening
-Hx:
◦ Genetics
◦ Parental reinforcement
-Path: Last 1/3 of night during REM
-Tx: Behavior therapy, Imagery rehearsal

REM Sleep Behavior Disorder
Define Condition:
Abnormal or disruptive behaviors emerging during REM sleep having the potential to cause injury or sleep disruption (Acting Out your Dreams)
-Sx:
> Talking, Laughing
> Shouting
> Gesturing
> Grabbing
> Flailing Arms
> Punching
> Kicking
> Sitting up/Leaping from bed
-Dx: Increased Motor function during REM sleep (acc to PSG)
-Hx/Path:
◦ Multiple System Atrophy - 70%
◦ Parkinson's Disease - 33%
◦ Dementia of Lewy Body - 40%

Restless Legs Syndrome
Define Condition:
Type of Sleep Related Movement Disorders - A neurological movement disorder characterized by:
◦ Unpleasant, tingling, creeping feelings or nervousness in legs during inactivity and sleep
◦ Experience an irresistible urge to move
◦ Sensations feel better with movement
-Hx
> More in adults, but in some teens
> FHx
> ADHD
-Tx:
◦ Ropinirole (Requip)
◦ Gabapentin (Neurontin)
◦ Old treatments: carbidopa-levodopa opioids, benzodiazepines, anticonvulsants
-Prog:
> Disturbed Sleep
> Negative Affect (Daytime)
Periodic Limb Movement Disorder (PLMD)
Define Condition:
Repetitive episodes of muscle movements:
◦ Clustering of jerking motions or upward flexing of the foot (4+ movements) every 20-40 seconds
◦ PSG findings: >15/hr in adults; >5/hr in children
-Hx:
> More in CHILDREN, in some adults
-Tx:
◦ Ropinirole (Requip)
◦ Gabapentin (Neurontin)
◦ Old treatments: carbidopa-levodopa opioids, benzodiazepines, anticonvulsants
-Prog:
> Disturbed sleep
> Daytime sleepiness