Clin Med Exam 6 - Cardiology
1/850
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
851 Terms
most common cause of death worldwide even before cancer
CAD
what maneuvers decrease venous return?
standing, valsalva
with what maneuvers will you best hear mitral valve prolapse?
standing and valsalvaw
what maneuvers increase venous return?
squatting, leg raise, lying down
with what maneuvers will you best hear aortic stenosis and regurgitation?
squatting, leg raise, lying down (increase venous return)
when do you best hear HOCM?
standing and valsalva
inspiration makes what.murmurs sound louder?
right side (tricuspid and pulmonic)
expiration makes what murmurs sound louder?
left side (mitral and aortic)
ACE inhibitors, CHF/pulmonary edema can cause what symptom?
cough
pulmonary hypertension due to severe left sided HF can cause what symptom?
hemoptysis
CAD, severe valvular disease with aortic stenosis, HOCM, vasovagal, cardiac arrhythmia, orthostatic hypotension, can cause what neuro symptom?
dizziness or syncope
HOCM
hypertrophic obstructive cardiomyopathy
endocarditis might present with what non-cardiac symptoms?
fever and chills
rheumatic fever cardiac symptoms
tachy, cardiomegaly, new murmur, pericardial friction rub, muffled heart sounds, chest pain (from carditis)
peripartum cardiomyopathy signs/symptoms
new onset of SOB, DOE, edema
what drugs can increase systemic blood pressure?
OTC cough medications, decongestants, NSAIDs, stimulants, oral contraceptives
what cardiac condition might splinter hemorrhages, osler nodes, and janeway lesions suggest?
endocarditis
Levine's sign
clenched fist against chest
sitting upright, leaning forward unable to fly flat due to chest pain might indicate?
pericarditis
abnormal JVP
>5cm
S1
the first heart sound, heard when the atrioventricular (mitral and tricuspid) valves close - "lub"
S2
second heart sound, heard when the semilunar valves (pulmonary and aortic) valves close - "dub"
S3
an abnormal heart sound detected early in diastole as resistance is met to blood entering either ventricle; most often due to volume overload associated with heart failure
ventricular gallop → early diastolic passive ventricular filling (systolic HF)
S4
atrial gallop → late active ventricular filling as the atrium contracts against stiff ventricle (diastolic dysfunction)
a pericardial friction rub on exam is indicative of?
acute pericarditis
rales (crackles) indicating fluid in the alveoli are seen in what heart conditions?
CHF/pulmonary edema
pericardium
Double-layered membrane surrounding the heart.
epicardium
outer layer of the heart
what makes up the majority of the heart's mass?
myocardium
what layer of the heart lines the chambers, valves, vessels?
endocardium
describe the flow of blood through the heart
Superior and inferior vena cava --> R atrium --> tricuspid valve --> R ventricle --> pulmonary valve --> pulmonary artery --> lungs --> pulmonary vein --> L atrium --> mitral valve --> L ventricle --> aortic valve --> aorta --> systemic circulation
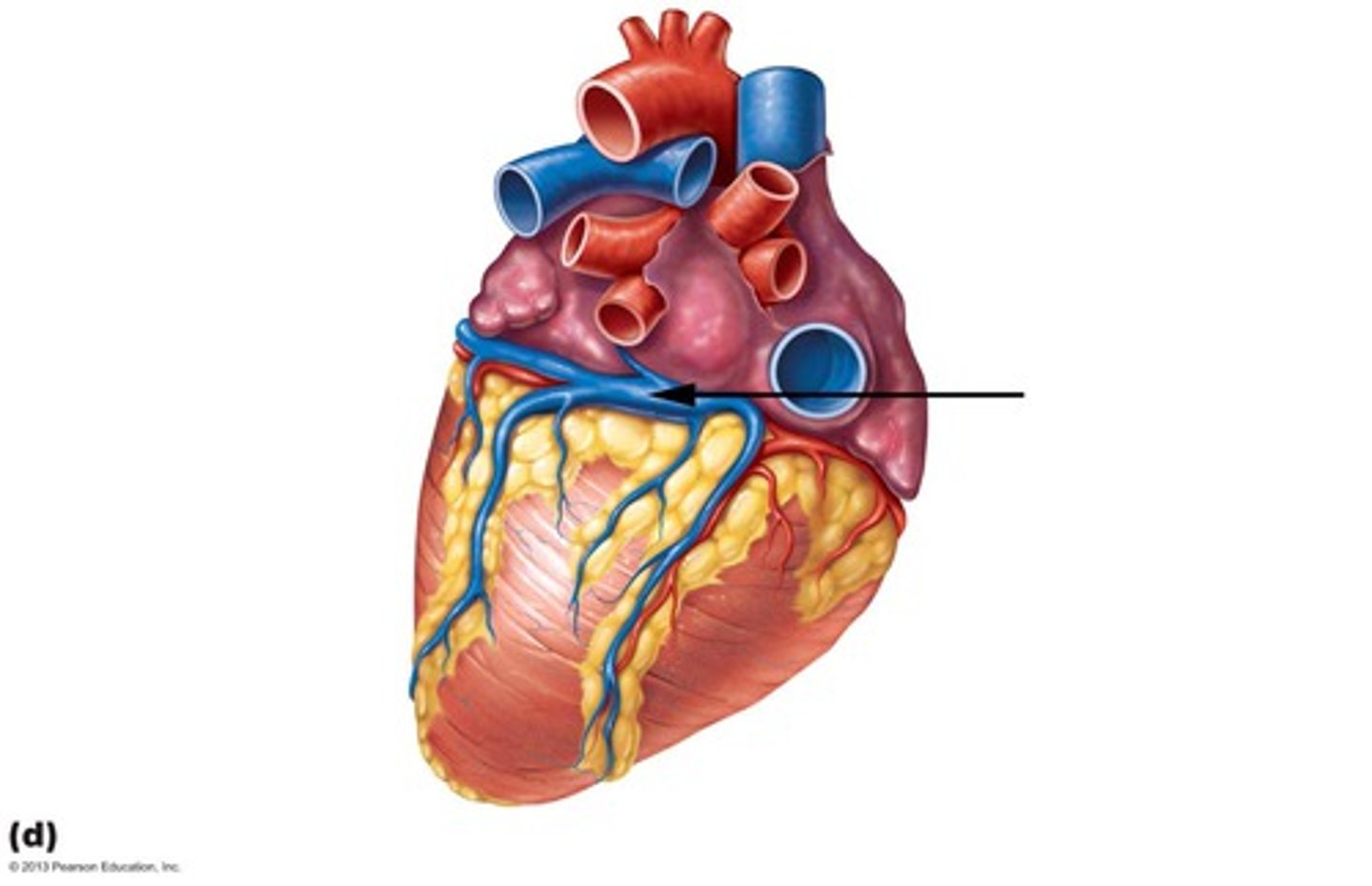
what supplies the myocardium?
coronary arteries
When do the coronary arteries fill with blood?
during ventricular diastole
Why don't the coronary arteries fill during systole?
because the pressure in the coronary arteries is higher than in the aorta during systole, so blood doesn't flow through them
What collects deoxygenated blood from the myocardium?
the coronary sinus vein
Where does the coronary sinus drain the deoxygenated blood?
the right atrium
Where is the coronary sinus located?
in the sulcus between the left atrium and left ventricle on the posterior surface of the heart
electrical system of the heart
SA node --> AV node --> bundle of His --> bundle branches --> Purkinje fibers
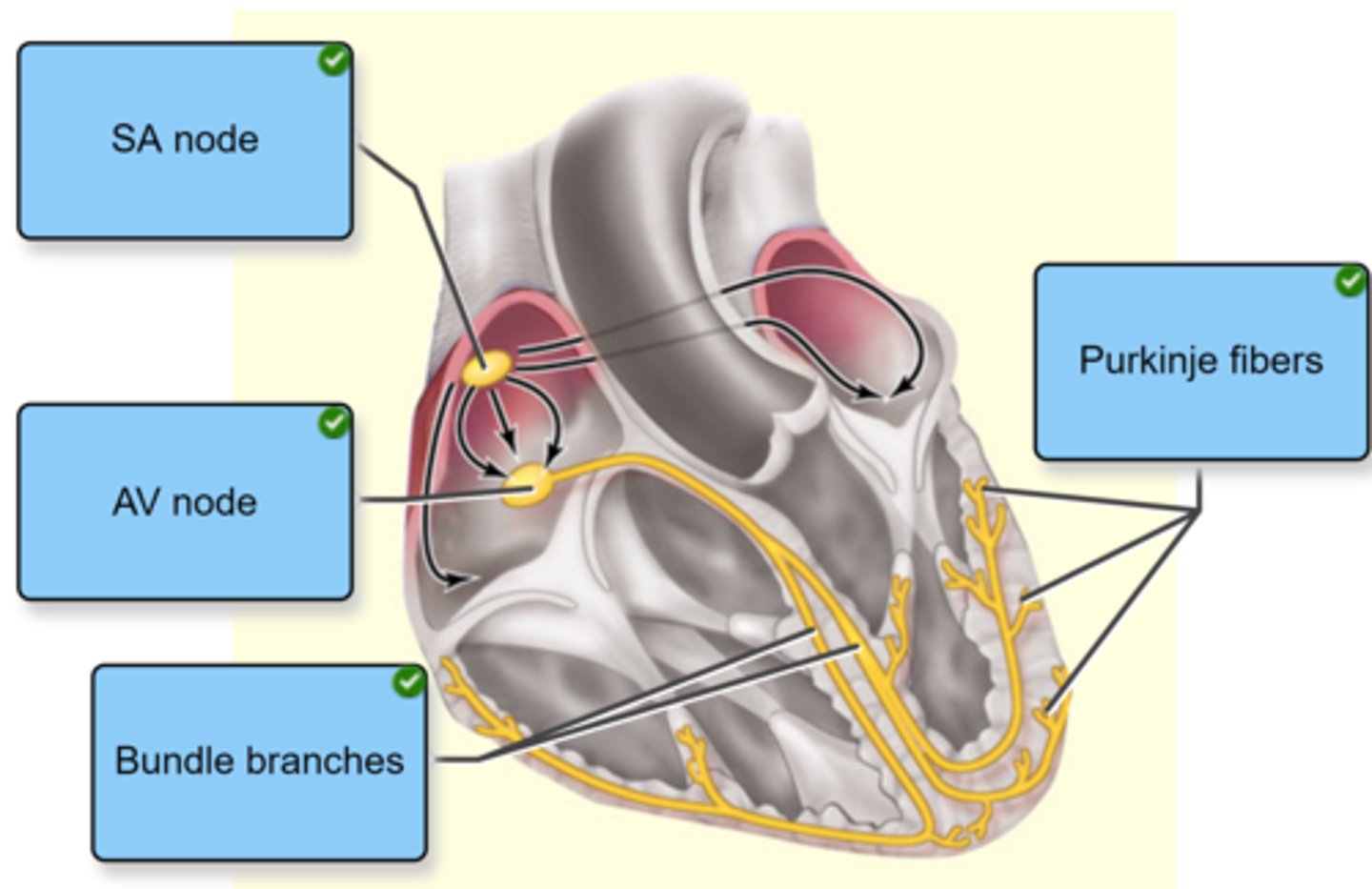
where is the SA node located? what does it set the sinus rhythm to?
right atrium
60-100 bpm
what is Bachmann's bundle?
a portion of the cardiac conduction system found in the left atria.
It is connected to the SA node and allows for simultaneous contraction of the atrias.
where is the internodal pathway and what does it do?
Located in the right atrium
Receives action potential from SA node and depolarizes the right atrium together with the SA node
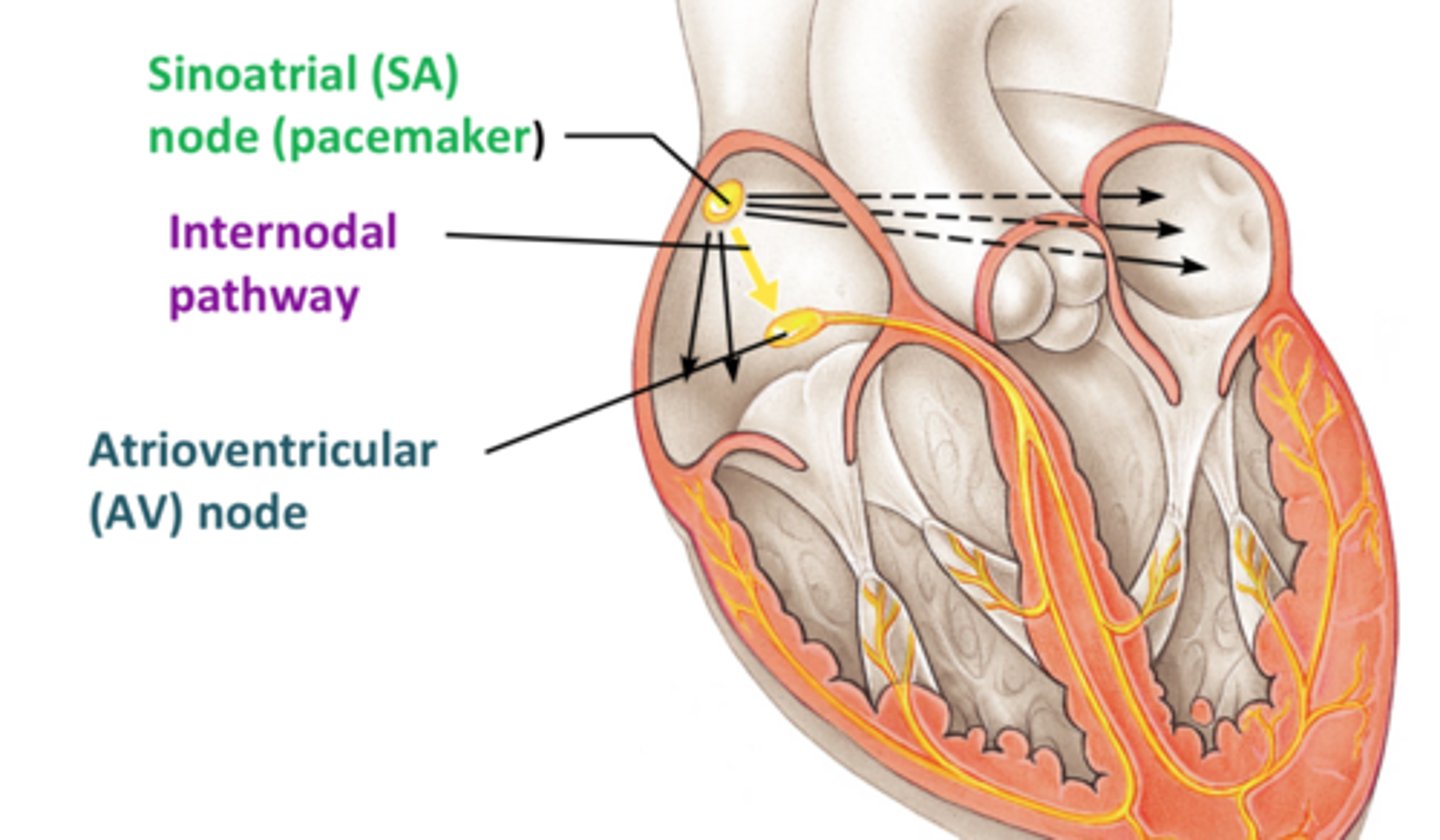
what does the AV node do?
located between the atria and ventricles --> slows electrical conduction from atria to ventricles to allow for ventricular filling before ventricles contract
Allows for depolarization to come from the atria down to the ventricles
what does the PR interval represent?
the time required for the impulse to travel from the atria through the AV node (AV node delay for ventricular filling)
carries electrical signals from the AV node to the Purkinje fibers in the ventricles
Bundle of His
Located in the subendocardial surface of the ventricle walls (part of the endocardium)
Receive electrical signals from the Bundle of His to the ventricles to contract
Purkinje fibers
what does it mean that pacemaker cells have automaticity?
they have the intrinsic ability to spontaneously depolarize and trigger action potential for ventricular cells to contract the heart's muscle (myocardium)
what rate can the AV node maintain should the SA node fail?
40-60 bpm
what rate can the Bundle of His and Purkinje fibers maintain should the SA and AV node fail?
20-40 bpm
what are ventricular cells vs pacemaker cells?
Ventricular cells: contractile cells (myocytes) that responds to the electrical signal generated by the pacemaker cells and cause forceful contraction
Pacemaker cells: noncontractile, specialized cells that spontaneously generate electrical impulses to initiate the heartbeat → contraction → pumping of blood
where are ventricular cells found?
in the myocardium of the heart
ventricular vs pacemaker cell action potential and depolarization
ventricular: fast response action potential with rapid depolarization phase
pacemaker: slow response action potential with gradual depolarization phase
What is the resting membrane potential of ventricular cells?
about -90 mV due to high permeability to potassium ions at rest
Do pacemaker cells have a stable resting membrane potential? how do they depolarize?
No, they have a pacemaker potential that slowly depolarizes due to If (funny) channels
What causes the slow depolarization in pacemaker cells?
If (funny) channels
What causes the rapid depolarization (Phase 0) in ventricular cells?
a large influx of sodium ions through voltage-gated Na+ channels
What ion is responsible for depolarization in pacemaker cells?
calcium influx through slow Ca2+ channels
What ion is responsible for repolarization in both ventricular and pacemaker cells?
Potassium (K+) efflux (leaving the cell)
What gives pacemaker cells automaticity?
The spontaneous depolarization caused by If (funny) currents
Why do ventricular cells have a long refractory period?
To prevent tetany and allow diastolic filling (relaxation)
Why do pacemaker cells have a shorter refractory period?
To maintain regular rhythmic firing of the SA node (60-100 bpm)
What occurs during Phase 1 of the ventricular action potential?
initial repolarization as Na+ channels close and K+ begins to leave the cell via fast K+ channels
What causes the plateau phase (Phase 2) in ventricular cells?
Ca2+ influx through slow Ca2+ channels and decreased K+ efflux
What occurs during Phase 3 of the ventricular action potential?
Rapid repolarization as Ca2+ channels close and K+ permeability increases (slow K+ channels open)
What is Phase 4 in ventricular action potentials?
Resting membrane potential (about -90 mV), maintained by K+ permeability.
Do pacemaker cells have a stable resting membrane potential?
no, there is just slow depolarization
Which channels are responsible for the pacemaker potential in Phase 4?
If (funny) channels
When do If channels open in pacemaker cells? when do they close?
(If) channels are open at about -60 mV until membrane hits threshold -40 mV to action potential, then they close
At what membrane potential do voltage-gated Ca2+ channels open in pacemaker cells?
At -40 mV (the threshold)
What is Phase 0 of the pacemaker action potential characterized by?
Opening of voltage-gated Ca2+ channels and rapid calcium influx
what causes depolarization of pacemaker cells?
opening of Ca2+ channels when threshold is reached
what occurs during Phase 3 in pacemaker cells?
repolarization due to potassium (K+) efflux through voltage-gated K+ channels
ectopic pacemaker cells
excitable group of cells that causes a premature heart beat outside the normally functioning SA node of the heart
can cause irregular heart beats/arrhythmias
threshold pacemaker vs ventricular
pacemaker: -40mV
ventricular: -70mV
primary depolarization ion pacemaker vs ventricular
pacemaker: Ca++
ventricular: Na+
membrane potential pacemaker vs ventricular
pacemaker: unstable -60mV (oscillates)
ventricular: stable, -90mV
what is the most influential ion in setting the resting membrane potential of cardiac cells and why?
potassium
due to cardiac cells being highly permeable to K+ at rest
RMP is primarily maintained by the ___________ gradient across the cell membrane
potassium
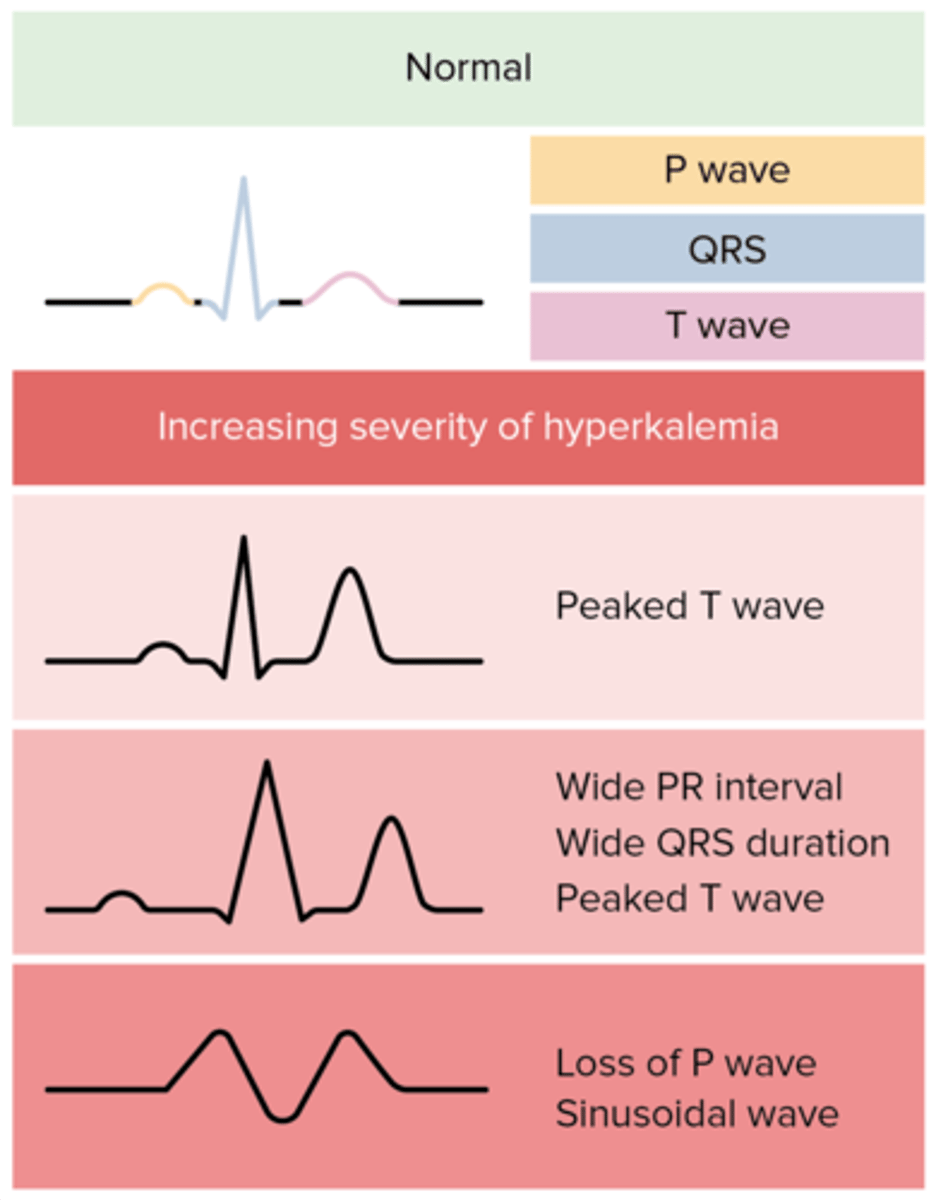
what will mild hyperkalemia show on EKG?
Peaked T waves due to faster repolarization of the ventricle (most prominent in precordial leads)
how does mild hyperkalemia affect the EKG and why?
Hyperkalemia makes the resting membrane potential less negative (depolarized a bit) --> more K+ in cell
Voltage-gated K⁺ channels are sensitive to voltage — and when the cell is less negative, these open earlier and more easily.
more K⁺ channels activate earlier, speeding up Phase 3 repolarization.
Result → peaked T waves (faster repolarization).
how does moderate hyperkalemia affect the EKG?
prolonged PR interval (slowed AV conduction)
widened QRS complex due to slowed ventricular conduction
this is due to inactivated Na+ channels as a result of higher RMP because of higher extracellular K+
how does moderate hyperkalemia result in bradycardia?
With both AV node and ventricular conduction slowing down, and SA node activity sometimes suppressed, the overall heart rate slows
what is seen on EKG in severe hyperkalemia and why?
Loss of P waves due to atrial depolarization is suppressed (Na+ channels are closed due to higher RMP, no Na⁺ influx = no depolarization = no P wave)
Sine wave pattern (fusion of QRS and T waves, pre-terminal rhythm that can lead to deadly ventricular arrhythmias or asystole → cardiac arrest)
severe hyperkalemia
>7.5
sine wave EKG
Normally, the QRS complex (ventricular depolarization) and T wave (ventricular repolarization) are separate, distinct parts of the EKG.
In severe hyperkalemia:
The QRS becomes so wide and distorted due to extremely slow conduction.
The T wave becomes tall and merges with the QRS.
what happens to the RMP in hypokalemia?
increase in K+ efflux making the RMP more negative (hyperpolarization) - depolarization more difficult as the cells are further from threshold
what happens the RMP in hyperkalemia?
decrease in K+ efflux making the RMP less negative (depolarization of the cell)
- cells are closer to the threshold for depolarization but may fail to fully repolarize
describe what you will see on EKG as potassium levels rise? (end with cardiac arrest)
1. peaked T waves
2. PR interval prolongation and flat and wide p waves
paroxysmal atrial fibrillation
< 7 days
AF that terminates spontaneously or
with intervention within 7 days of onset
persistent atrial fibrillation
< 1 year
AF that fails to self-terminate within 7
days but does not exceed 12 months
long standing persistent atrial fibrillation
> 1 year
AF that has lasted for more than 12
months
Individuals with long standing atrial fibrillation
where a joint decision by the patient and
clinician has been made to no longer pursue a
rhythm control strategy.
permanent (chronic) atrial fibrillation
Wenkebach
Nickname for second degree AV block type I
Progressive prolongation of the PR Interval
culminating in a non-conducted P wave
The PR interval is longest before the dropped beat
and shortest immediately after the dropped beat.
2° AVB
Mobitz I
(Wenkebach)
PRI> 200ms (five small squares)
Severe if PR interval > 300ms
1° AVB
Intermittent non-conducted P waves without
progressive prolongation of the PR interval.
The PR interval in the conducted beats remains
constant.
The RR interval is an exact multiple of the
preceding RR interval
2° AVB
Mobitz II
(High Grade)
Complete absence of AV conduction - none of the
supraventricular impulses are conducted to the
ventricles.
Perfusion sometimes maintained by a junctional or
ventricular escape rhythm.
P waves often seen "marching through"
3° AVB
(Complete)
intervention for 3° AVB
pacemaker
advantages of VVI pacemaker setting
useful for AF and high grade AV block
what is the AAI pacemaker setting able to detect?
ST changes
with which pacemaker setting is AV synchronicity lost?
VVI