120 quiz 4 ch 8
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
In what ways does blood carry oxygen?
Oxygen dissolved in plasma
Oxygen combined with hemoglobin (Hb transports most of the O2)
What equation expresses mL of oxygen dissolved in 100mL of plasma?
PO2 × 0.003 = mL/dL dissolved oxygen
Approximately 0.003 mL of O2 will dissolve in 100 mL of blood for every 1 torr of PO2. Thus, PaO2 of 100 = ____mL
0.3 mL
If PaO2 = 100 mmHg and Hb concentration = 15 g/dL, Hb carries ____ mL/dL
20
Normal cardiac output (Q) of 5 L/min:
O2 delivery to all body tissues = 1000 mL O2/min
O2 consumption by tissues = ____ mL/min
250 mL/min
O2 delivery is 4x body’s resting requirement; in other words, tissues consume about ___% of the O2 delivered to them
25%
Oxyhemoglobin (HbO2)
Hb combined with oxygen
Deoxyhemoglobin
Hb not bound with oxygen
Cooperative binding
Each molecule of oxygen bound to Hb makes the next molecule bind more quickly
Most oxygen that diffuses into pulmonary capillary blood rapidly moves into ____s and chemically attaches to ____.
RBCs, hemoglobin
approximately how many Hb molecules does each RBC contain?
280 million Hb molecules
Normal adult hemoglobin (Hb A) consists of:
Four heme groups
pigmented, iron-containing nonprotein portions of hemoglobin molecule
Four amino acid chains (polypeptide chains) that collectively constitute globin (protein)
Hemoglobin saturation normal values:
Normal SaO2 = _____ %
Occurs at PaO2 of ____ mmHg
97.5%
100 mmHg
Hemoglobin saturation normal values:
Normal SvO2 = ____%
Occurs at PvO2 of ____ mmHg
75%
40 mmHg
% saturation is NOT equal to O2 or Hb concentration.
This means that an SaO2 of 100% does not necessarily mean the O2 content is ____
normal
When hemoglobin is 100% saturated with O2, each gram of hemoglobin (g% Hb) can carry ____ mL of O2
1.34 mL of O2
What is the normal Hb level range?
12 to 15 g/dL
At 15 g/dL and 100% saturation, Hb carries ____ mL of oxygen
20.1 mL
Mixed venous blood at 75% saturation carries 0.75 × 20.1 (mL O2 at 100%) = ____ mL/dL
15.1 mL/dL
At 100% saturation Hb carries 20.1 mL oxygen
At 75% saturation mixed venous blood carries 15.1 mL oxygen
This makes the arterial-venous content difference = ~ ____ mL/dL
5 mL/dL
Each g% Hb can carry 1.34 mL of oxygen. Thus if Hb level is 15 g%, and if Hb is fully saturated, approximately ____ vol% of O2 will be bound to Hb
20.1 vol% of O2
Found by:
1.34 mL O2 × 15 g% Hb = 20.1 vol% of O2
At normal PaO2 of 100 mmHg, however, Hb saturation (SaO2) is only ~ 97% due to the following three normal physiologic shunts:
Thebesian venous drainage into left atrium
bronchial venous drainage into pulmonary veins
alveoli that are under-ventilated
Thus, amount of arterial oxygen in preceding equation must be adjusted to 97%:
20.1 vol% O2 × 0.97 = 19.5 vol% O2
To determine total amount of oxygen in 100 mL of blood, the following must be added together:
dissolved oxygen in plasma
oxygen bound to hemoglobin
What is the equation for total oxygen content of arterial blood (CaO2)?
CaO2 = (PaO2 × 0.003) + (SaO2 × 1.34 x Hb)
CaO2 = oxygen content of arterial blood, mL/dL
PaO2 = partial pressure of oxygen
0.003 = dissolved O2 factor
SaO2 = percentage Hb fully saturated with O2, %
1.34 = volume of O2 bound to Hb at 100% saturation
Hb = concentration of hemoglobin
Normal CaO2 (O2 content of arterial blood)?
about 20 mL/dL
What is the equation for total oxygen content of mixed venous blood (CvO2)?
CvO2 = (PvO x 0.003) + (SvO2 × 1.34 x Hb)
Normal CvO2 (O2 content of mixed venous blood)?
about 15 mL/dL
Normal C(a-v)O2 (arterial-venous O2 content difference)? (range)
Range is 3.5 to 5 mL/dL
What is the equation for total oxygen content of pulmonary capillary blood (CcO2)?
CcO2 = (PAO2 × 0.003) + (1.34 x Hb)
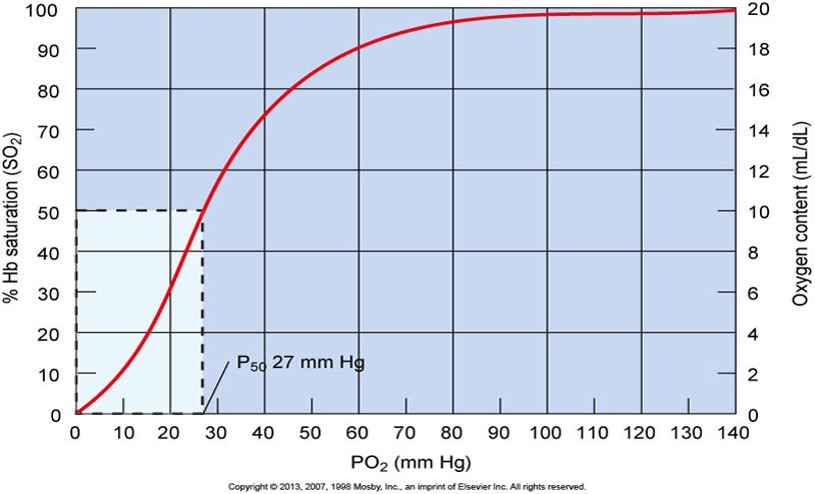
What does the Oxyhemoglobin Dissociation Curve graphically illustrate?
The percentage of Hb chemically bound to oxygen at each oxygen pressure PO2
What is the clinical significance of the flat portion of the HbO2 dissociation curve?
PO2 can fall from 60 to 100 torr and Hb will still be 90% saturated with O2.
excellent safety zone
As Hb moves through AC system, significant partial pressure difference continues to exist between alveolar gas and blood, even after most O2 has transferred. Why?
It enhances diffusion of O2
What is the effect of increasing PO2 beyond 100 torr?
doing so adds very little O2 to blood
dissolved O2 only (PO2 × 0.003)
What is the clinical significance of the steep portion of the HbO2 dissociation curve?
Reduction of PO2 below 60 torr causes rapid decrease in the amount of O2 bound to Hb.
however, diffusion of oxygen from Hb to tissue cells in enhanced
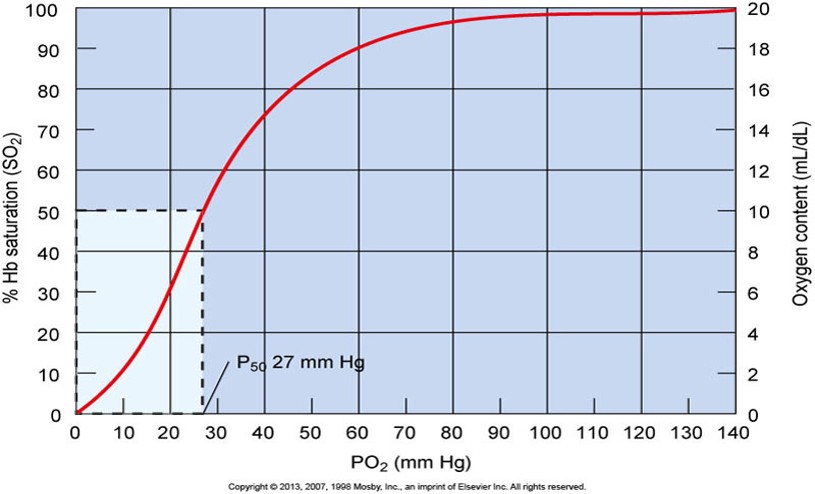
The flat portion of the HbO2 equilibrium curve shows that large changes in PO2 between 60 and 100 mmHg lead to what?
small changes in SO2 and CaO2
The steep portion of the HbO2 equilibrium curve shows that small changes in PO2 between 20 and 60 mmHg lead to what?
large changes in SO2 and CaO2
P50 is the point of reference on the HbO2 dissociation curve.
It is ~ = ____ torr
What does it represent?
27 torr
It represents partial pressure at which hemoglobin is 50 percent saturated with oxygen
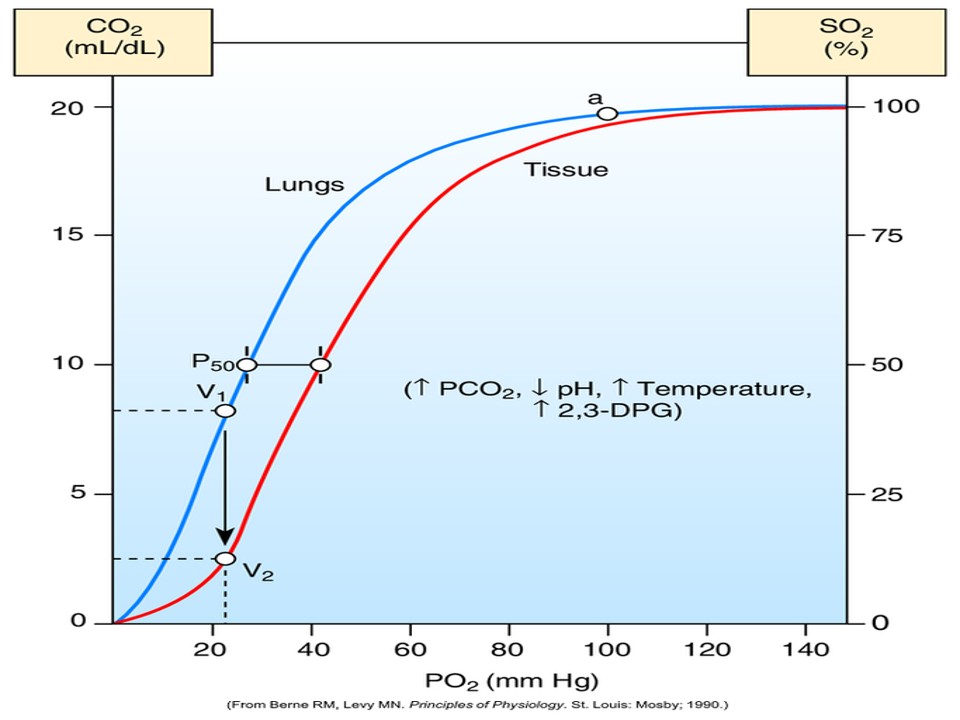
What factors affect the HbO2 dissociation curve?
pH
Temperature
CO2
2,3-bisphosphoglycerate (BPG)
When the curve shifts to the right, P50 _____
increases
Factors that shift HbO2 curve to the RIGHT:
↓ pH,
↑ PCO2, ↑ Temperature, ↑ DPG
A shift to the RIGHT means that Hb affinity for oxygen has decreased. What does this mean?
Hb releases additional O2 into the plasma, which incrases the pressure gradient for O2 diffusion into the tissues
When curve shifts to the left, P50 _____
decreases
Factors that shift HbO2 curve to the LEFT:
↑ pH,
↓ PCO2, ↓ Temperature, ↓ BPG
A shift to the LEFT means that Hb affinity for oxygen has increased. What does this mean?
Hb releases less O2 into plasma, so less O2 is available to tissues.
O2 and CO2 pressure gradients in the lungs are _____ in the systemic tissues.
reversed
At lungs, curve shifts left
At tissue level, curve shifts right
Total oxygen delivery (DO2)
What is it and what is it dependent on?
Total amount of oxygen delivered or transported to peripheral tissues
Dependent on:
Body’s ability to oxygenate blood
Hemoglobin concentration
Cardiac output
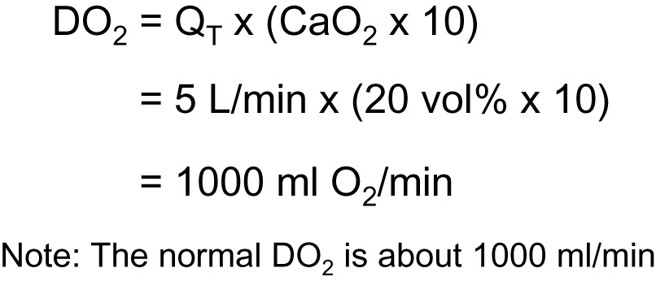
What is the equation for total oxygen delivery (DO2)?
DO2 = QT x (CaO2 × 10)
QT = cardiact output (L/min)
CaO2 = oxygen content (vol%)
What is the normal DO2?
about 1000 mL/min
DO2 decreases in response to:
Low blood oxygenation
low PaO2
low SaO2
low Hb concentration
low cardiac output
DO2 increases in response to:
Increased blood oxygenation
increased PaO2
increased SaO2
increased Hb concentration
increased cardiac output
What is the normal value of C(a-v)O2?
Normally, CaO2 is ~ 20 vol% and CvO2 is 15 vol%
thus, normal C(a-v)O2 is ~5 vol%
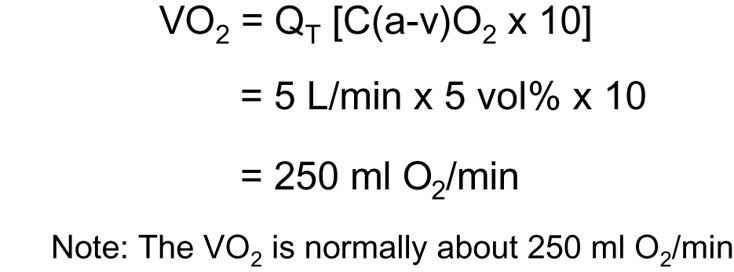
What is oxygen consumption (VO2)?
Equation?
Amount of oxygen extracted by peripheral tissues during period of one minute
VO2 = QT [C(a-v)O2 × 10]
What is oxygen consumption (VO2) normally?
about 250 mL O2/min
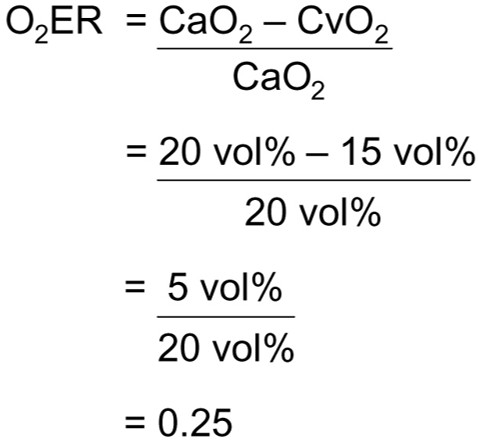
What is oxygen extraction ration (O2ER)?
Equation?
Amount of oxygen extracted by perippheral tissues divided by amount of oxygen delivered to peripheral cells
O2ER = C(a-v)O2 / CaO2
The oxygen extraction ratio (O2ER) is also called the ____.
Oxygen utilization coefficient
What is the normal value of O2ER?
In considering normla CaO2 of 20 vol% and normal CvO2 of 15 vol%,
O2ER = ~25%
Changes in the mixed venous saturation, or SvO2, can be used to detect changes in:
C(a-v)O2
VO2
O2ER
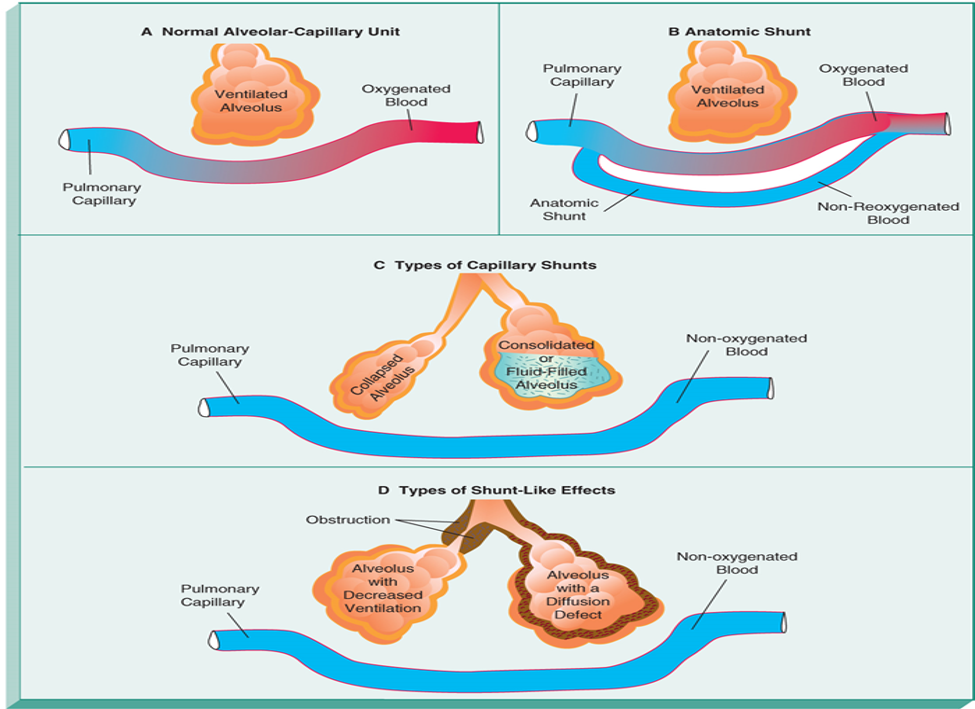
Pulmonary shunting
Portion of cardiac output that moves from right side to left side of heart without being exposed to PAO2 (oxygenation via alveolar oxygen)
Clinically, pulmonary shunting can be subdivided into:
Absolute shunt (true shunt)
Relative shunt (shunt-like effects)
Absolute shunts can be grouped under two major categories:
Anatomic shunts
Capillary shunts
Anatomic vs capillary shunts
Anatomic
exist when blood flows from right side of heart to left side without coming in contact with alveolus for gas exchange
Capillary
caused by alveolar collapse or atelectasis, alveolar fluid accumulation, alveolar consolidation
In healthy lung, normal anatomic shunt is approximately ___% of cardiac output
3%
Normal shunting is caused by nonoxygenated blood completely bypassing alveoli and entering:
pulmonary vascular system by means of bronchial venous drainage
left atrium by way of thebesian veins
Common causes of absolute shunting (conditions)
Congenital heart disease
Intrapulmonary fistula
Vascular lung tumors
Relative shunt, or shunt-like effect, exists when pulmonary capillary perfusion is in excess of _____
alveolar ventilation
What are common causes of relative shunting?
hypoventilation
ventilation/perfusion mismatches
chronic emphysema, bronchitis, asthma
alveolar-capillary diffusion defects
alveolar fibrosis or alveolar edema
The end result of pulmonary shunting is venous admixture. What is this?
Mixing of shunted, non-reoxygenated blood with reoxygenated blood distal to alveoli
Downstream in pulmonary venous system
When venous admixture occurs, shunted, non-reoxygenated blood gains oxygen molecules while, simultaneously, reoxygenated blood loses oxygen molecules.
Process continues until:
PO2 throughout all plasma of newly mixed blood is in equilibrium
All Hb molecules carry the same number of oxygen molecules
Shunt equation and information needed
Pb, PaO2, PaCO2, PvO2, Hb, PAO2, FIO2
Steps for solving shunt equation
Calculate PAO2
Calculate CcO2
Calculate CaO2
Calculate CvO2
Plug into shunt equation
Interpreting pulmonary shunting percentages
<10% - normal status
10-20% - indicated intrapulmonary abnormality
20-30% - significant intrapulmonary diseases
>30% - potentially life-threatening
hypoxemia
abnormally low arterial oxygen tension
frequently assoiciated with hypoxia
Although presence of hypoxemia strongly suggests tissue hypoxia, does not necessary mean _____ existence of tissue hypoxia
absolute
Hypoxia
low or inadequate oxygen for aerobic cellular metabolism
hypoxia is characterized by:
tachycardia, hypertension, peripheral vasoconstriction, dizziness, and mental confusion
What are the four main types of hypoxia?
hypoxic hypoxia
anemic hypoxia
circulatory hypoxia
histotoxic hypoxia
hypoxic hypoxia and causes
Inadequate oxygen at the tissue cells caused by low arterial oxygen tension (PaO2)
Common causes:
Low PaO2 caused by:
hypoventilation, high altitude
Diffusion impairment
interstitial fibrosis, interstitial lung disease, pulmonary edema, pneumoconiosis
Ventilation-perfusion mismatch
Pulmonary shunting
anemic hypoxia and causes
PaO2 is normal, but the oxygen-carring capacity of hemoglobin is inadequate
Common causes:
decreased Hb concentration
anemia, hemorrhage
abnormal hemoglobin
carboxyhemoglobin
methemoglobin
circulatory hypoxia and causes
blood flow to the tissue cells is inadequate; thus, oxygen is not adequate to meet tissue needs
Common causes:
slow or stagnant (pooling) peripheral blood flow
arterial venous shunts
histotoxic hypoxia and causes
Impaired ability of the tissue cells to metabolize oxygen
Cause:
cyanide poisoning
cyanosis
Blue-gray or purplish discoloration seen on mucous membranes, fingertips, and toes
May appear whenever blood contains at least 5 g% of deoxyHb
Peripheral vs Central cyanosis
peripheral
Low SvO2 (SaO2 may be normal), low blood flow states - tissues extract more O2, affects skin and nail beds
central
Low SaO2, more profound hypoxemia than peripheral, affects mucous membranes
Anemia vs polycythemia
Anemia
low # of RBCs, so Hb levels are lower than normal
Polycythemia
high # of RBCs, so Hb levels are higher than normal
Carboxyhemoglobin (HbCO) - CO inhalation
Hb has ____x greater affinity for CO than for O2
210x
Treating CO inhalation - competitive binding
High FiO2 - decreases half-life of HbCO
Hyperbaric oxygen therapy
Methemoglobin (metHb) characteristics & cause
Hb with Fe++ oxidized to Fe+++
Cannot bind with oxygen
Caused by nitrate poisoning or toxic reactions to oxidant drugs.
Normal <1% total Hb, value is on ABG