BIOL 4160 : Cardiac Physiology Part 2 (Exam 3)
1/183
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
184 Terms
In skeletal muscle and cardiac muscle, what does the muscle action potential directly elicit?
excitation contraction coupling
What direct effect does excitation contraction coupling have in skeletal and cardiac muscle?
results in an increase in calcium in the cytoplasm
Because cardiac muscle is striated, how is it similar to skeletal muscle (in terms of the process of contraction)?
same cross bridge cycle so they experience the same inhibition to prevent cross bridge cycling
In skeletal muscle, what 2 things does the quick action and subsequently long contraction allow for?
summation and tetanus
In the heart, why is summation not considered beneficial?
it does not assist in the function of the heart as a pump; if your heart has a long sustained contraction, you will die
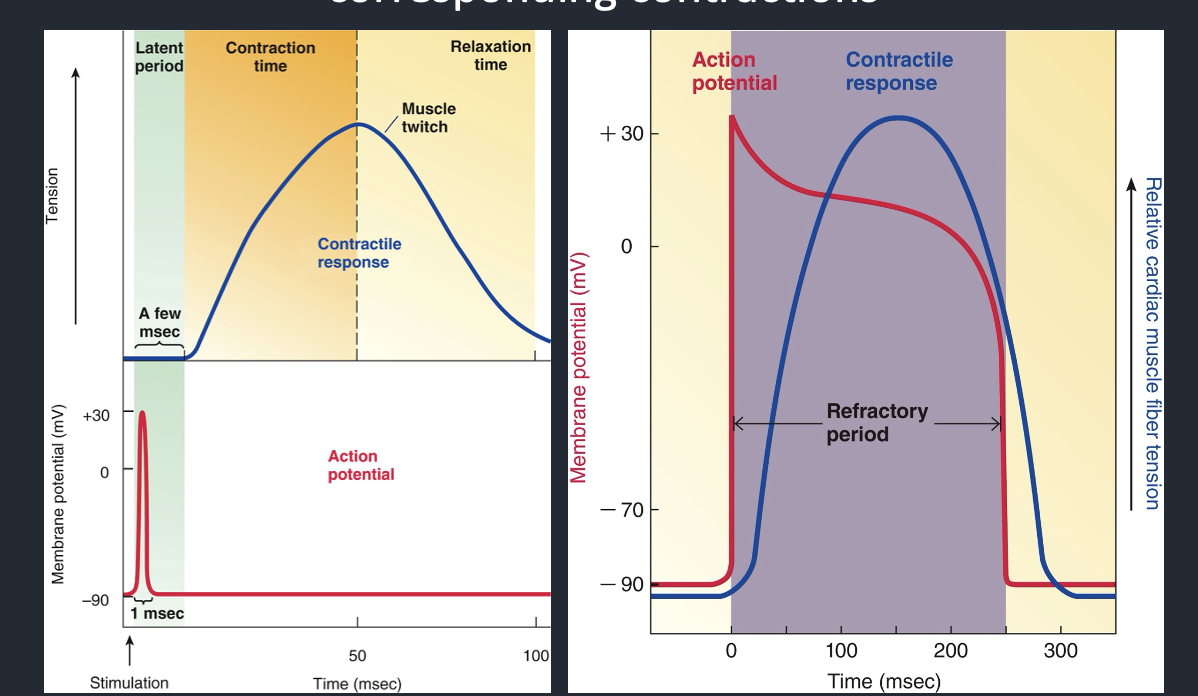
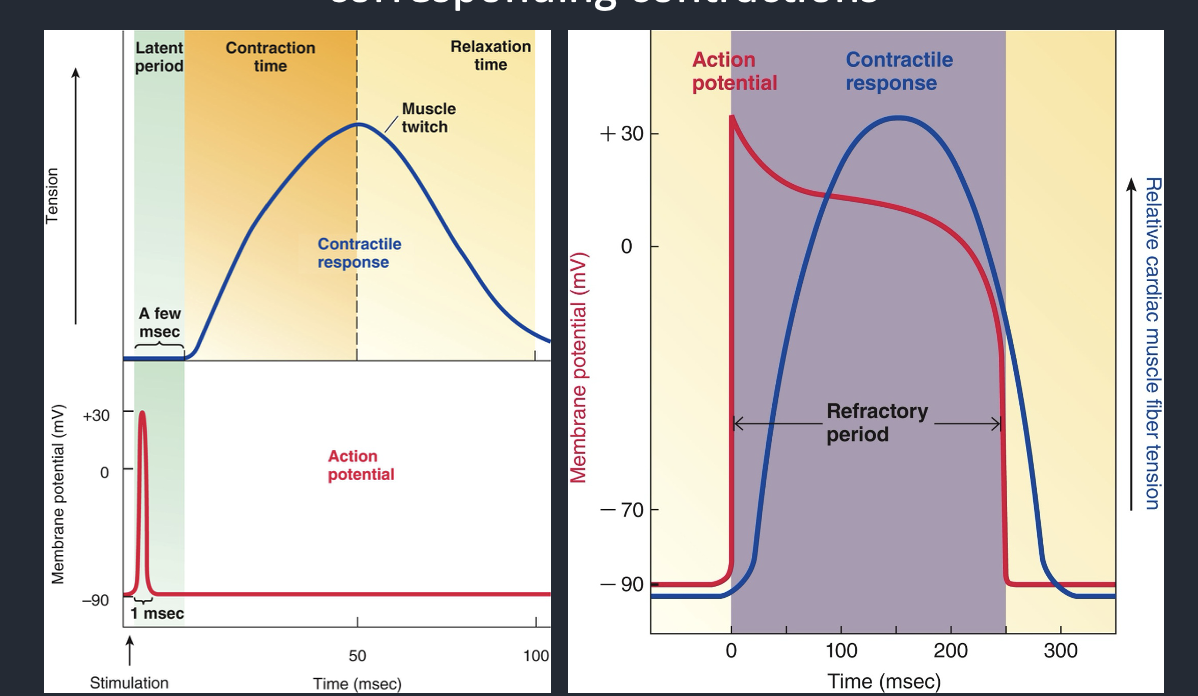
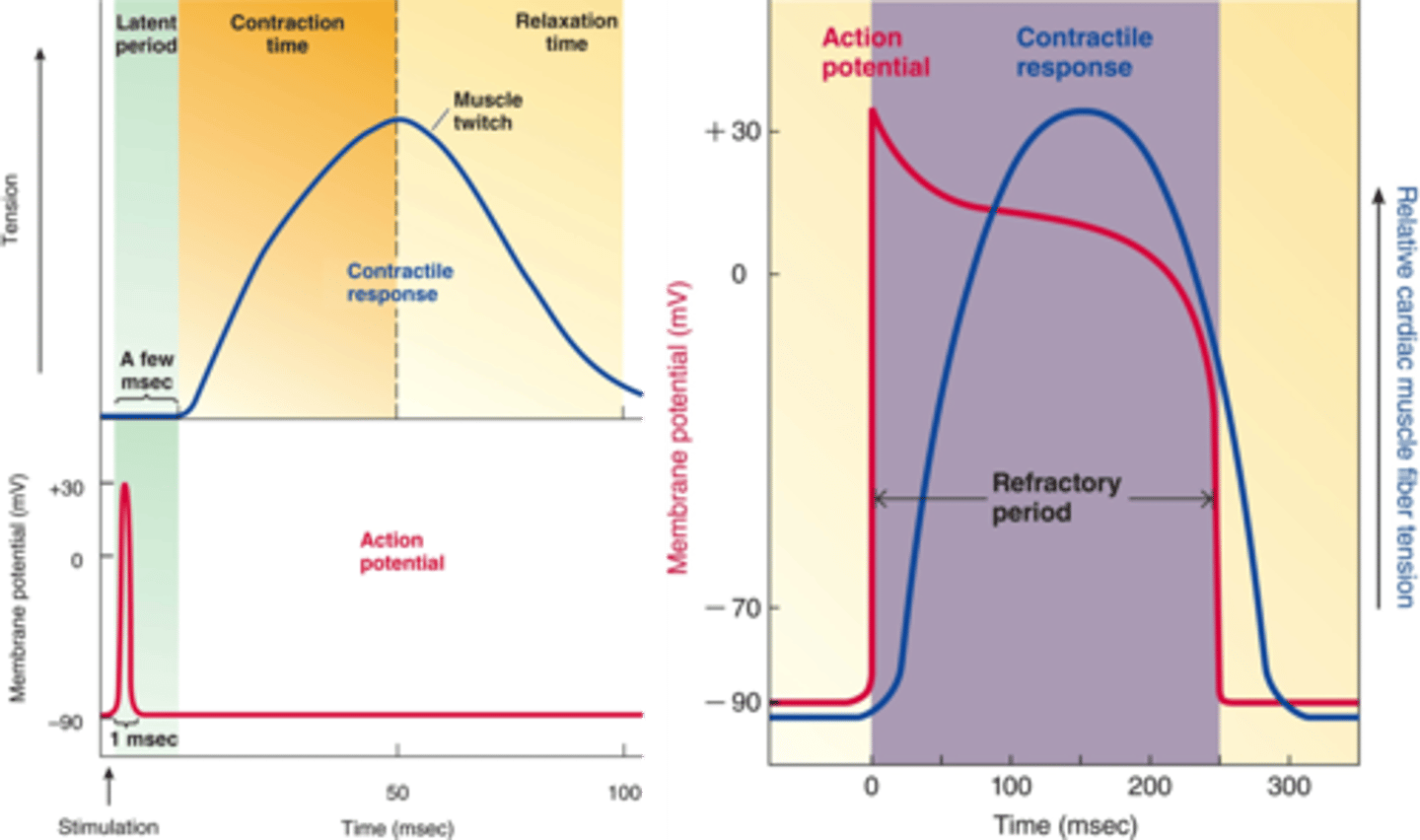
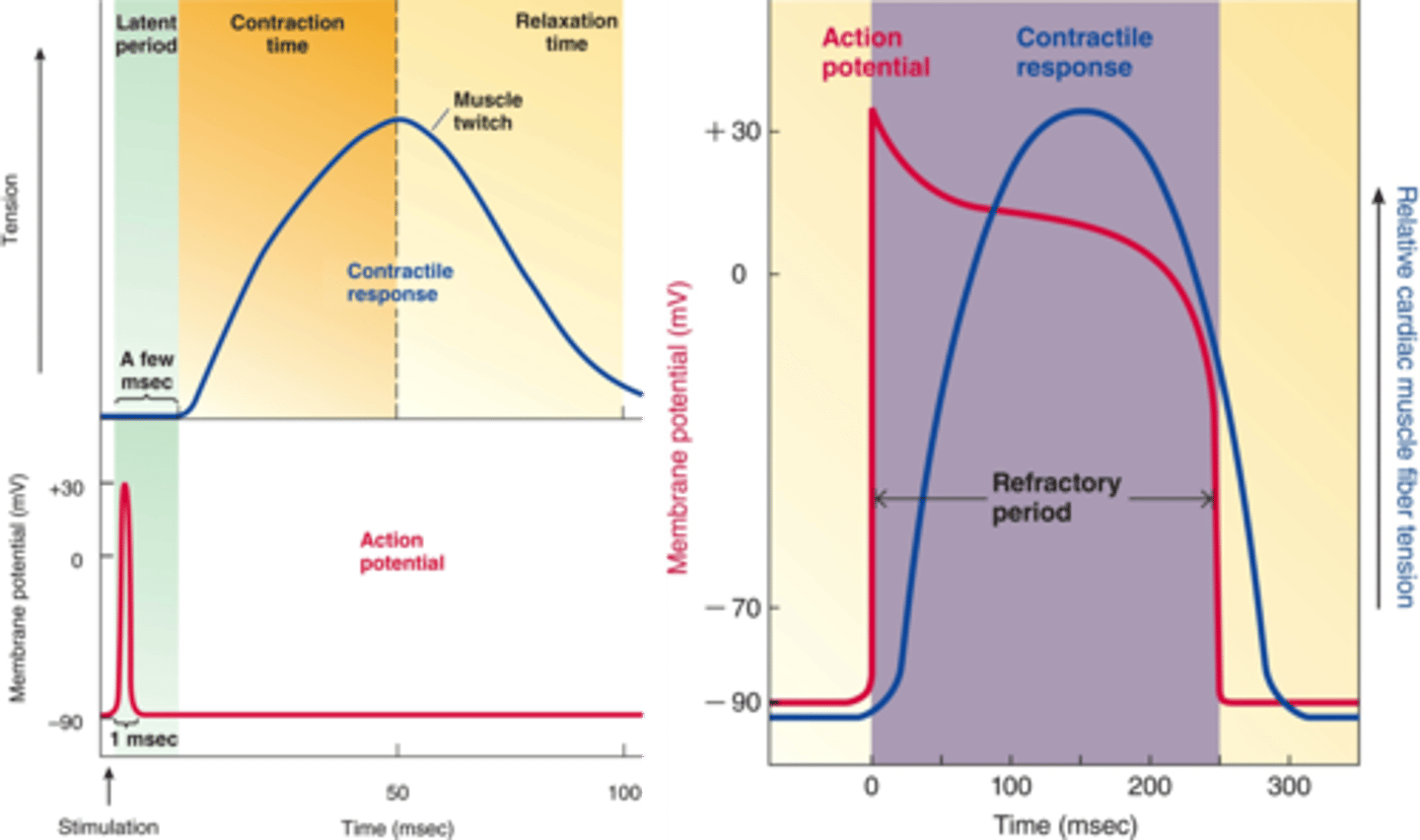
Cardiac vs Skeletal Action Potenital (Contractile Response)
In skeletal muscle,
the action potential is ___ (falls within the latent period)
then the corresponding contraction is ___ (multiple APs can be fired during corresponding contraction-- summation and tetanus)
In cardiac muscle
the action potential's ____ period lasts nearly as long as the ____ (both long), so the muscle cannot fire an ___ until the ____ is finished
In skeletal muscle,
the action potential is quick (falls within the latent period)
then the corresponding contraction is long (multiple APs can be fired during corresponding contraction-- summation and tetanus)
In cardiac muscle
the action potential's refractory period lasts nearly as long as the contraction (both long), so the muscle cannot fire an AP until the contraction is finished
The action potential of a skeletal muscle fiber falls within the ___ period of a muscle twitch.
The action potential of a skeletal muscle fiber falls within the latent period of a muscle twitch.
Can multiple action potentials be fired in skeletal muscle? If so, how?
Yes
Because each AP is brief and contraction is long, repeated neural stimulation can trigger multiple muscle action potentials.
This allows new APs to arrive before the muscle relaxes, leading to summation and stronger contractions.
How does the action potential of cardiac muscle differ from the action potential of skeletal muscle with regards to the duration of the contractile response?
In skeletal muscle,
the action potential is quick (falls within the latent period)
then the corresponding contraction is long (multiple APs can be fired during corresponding contraction-- summation and tetanus)
In cardiac muscle
the action potential's refractory period lasts the length of the contraction (both long), so the muscle cannot fire an AP until the contraction is finished
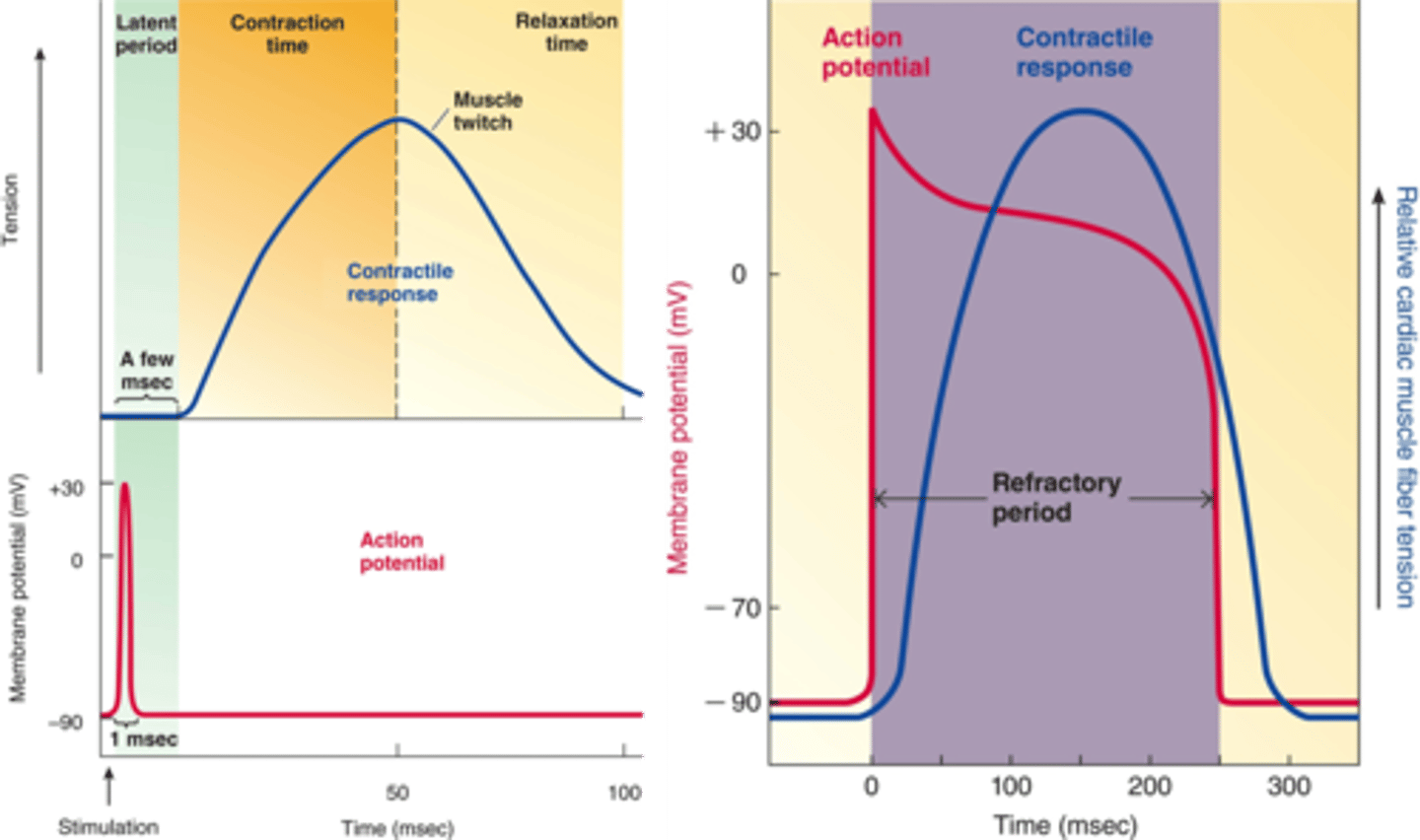
What does the large difference between the timing of the muscle AP and subsequent muscle contraction in skeletal muscle allow for?
- This allows us to have summation or a tetanic contraction
- The rate or timing of stimulation can allow us to modify the strength of the skeletal muscle contraction (summation = stronger contraction)
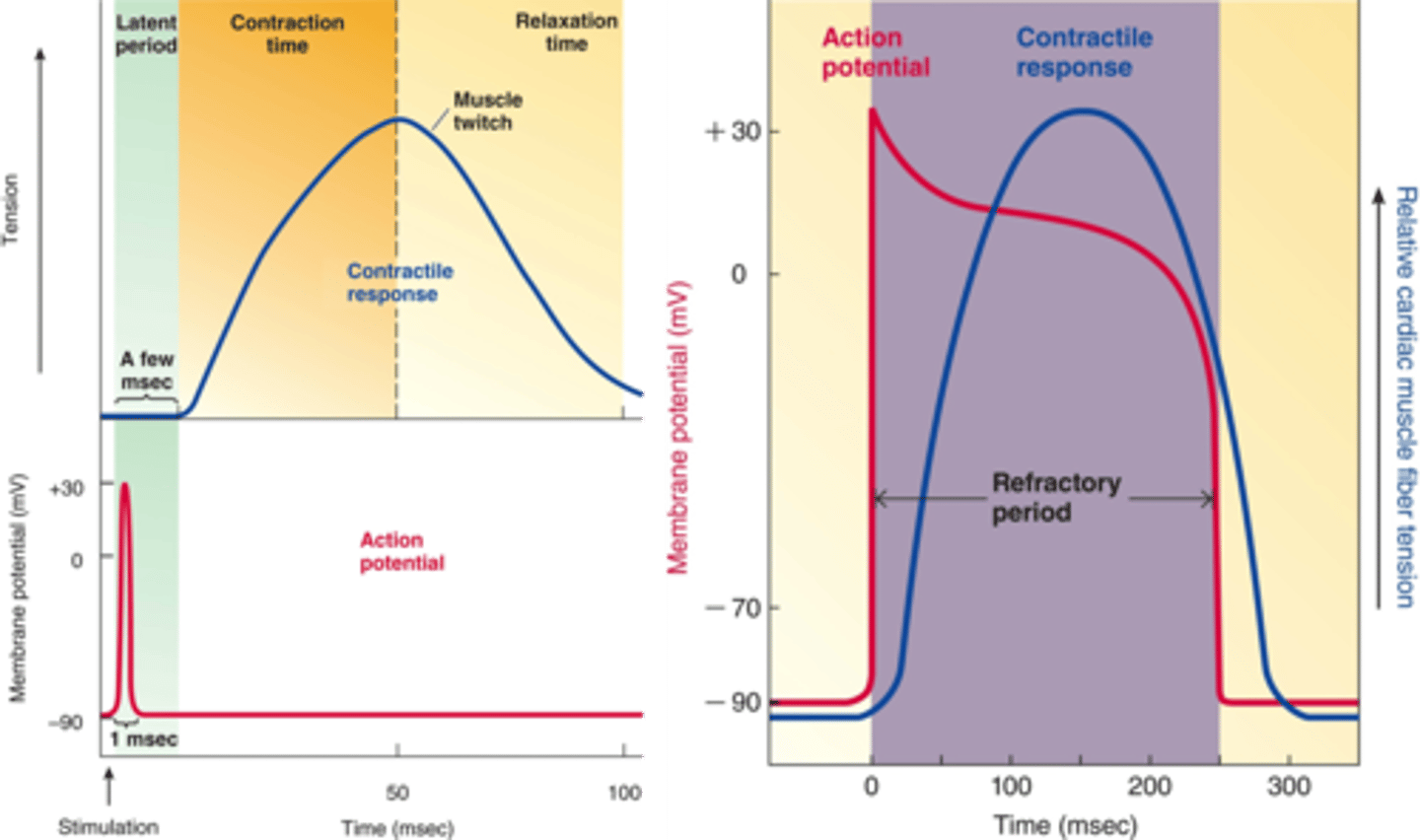
In cardiac muscle, about how long is the fast response action potential?
It is almost as long as the corresponding contraction
The Refractory period of the AP lasts almost to the end of the contraction that corresponds to the single excitation
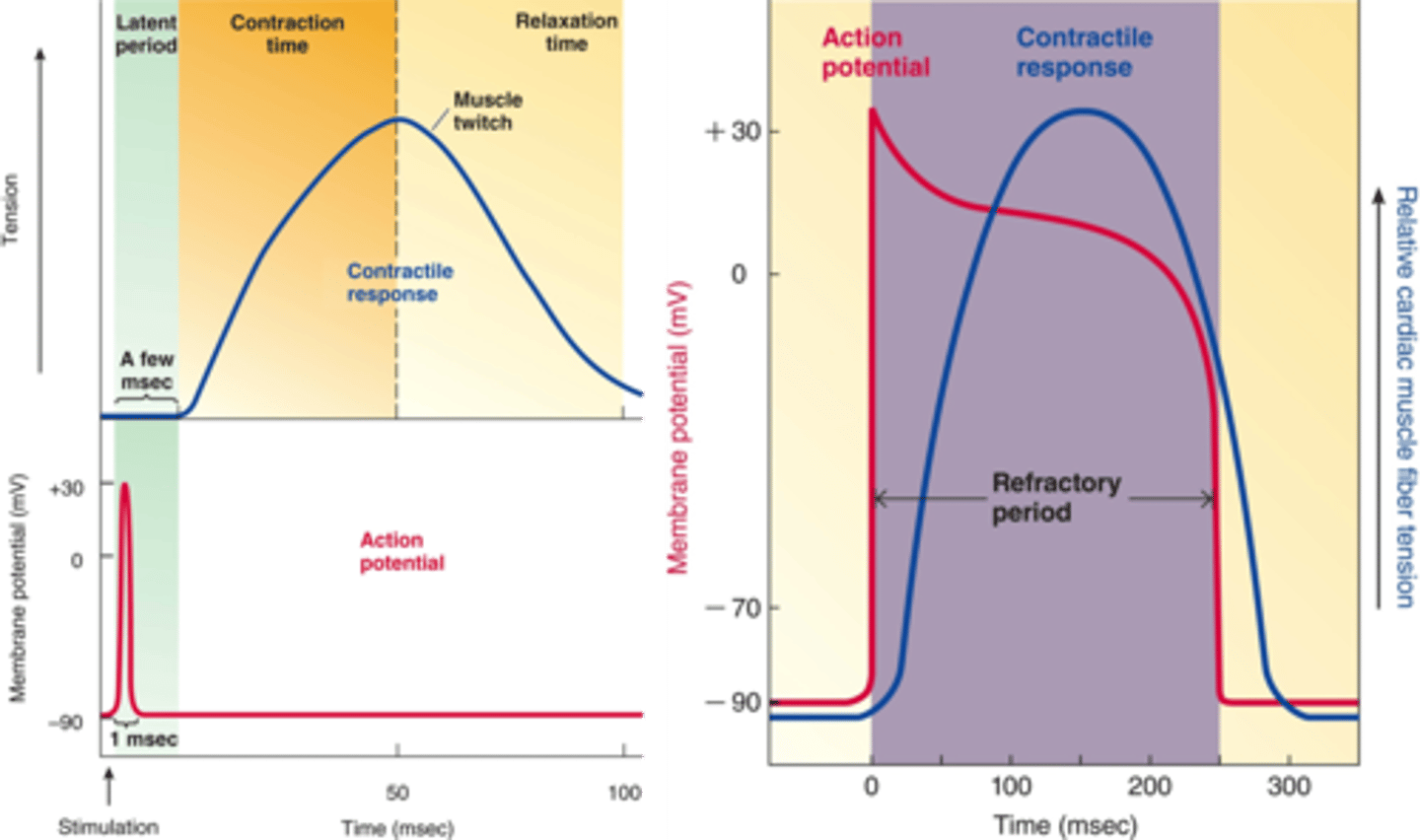
Why is the fast response action potential in cardiac muscle (refractory period) lasting almost as long as the corresponding contraction physiologically significant?
- Important physiologically because of the prolonged refractory, there is a less of a chance for something like summation to occur
- In order for the heart to be an efficient pump, it must contract and relax
- Summation would not be an effective way to modify the strength of cardiac contraction - too long of time between the filling period of the heart
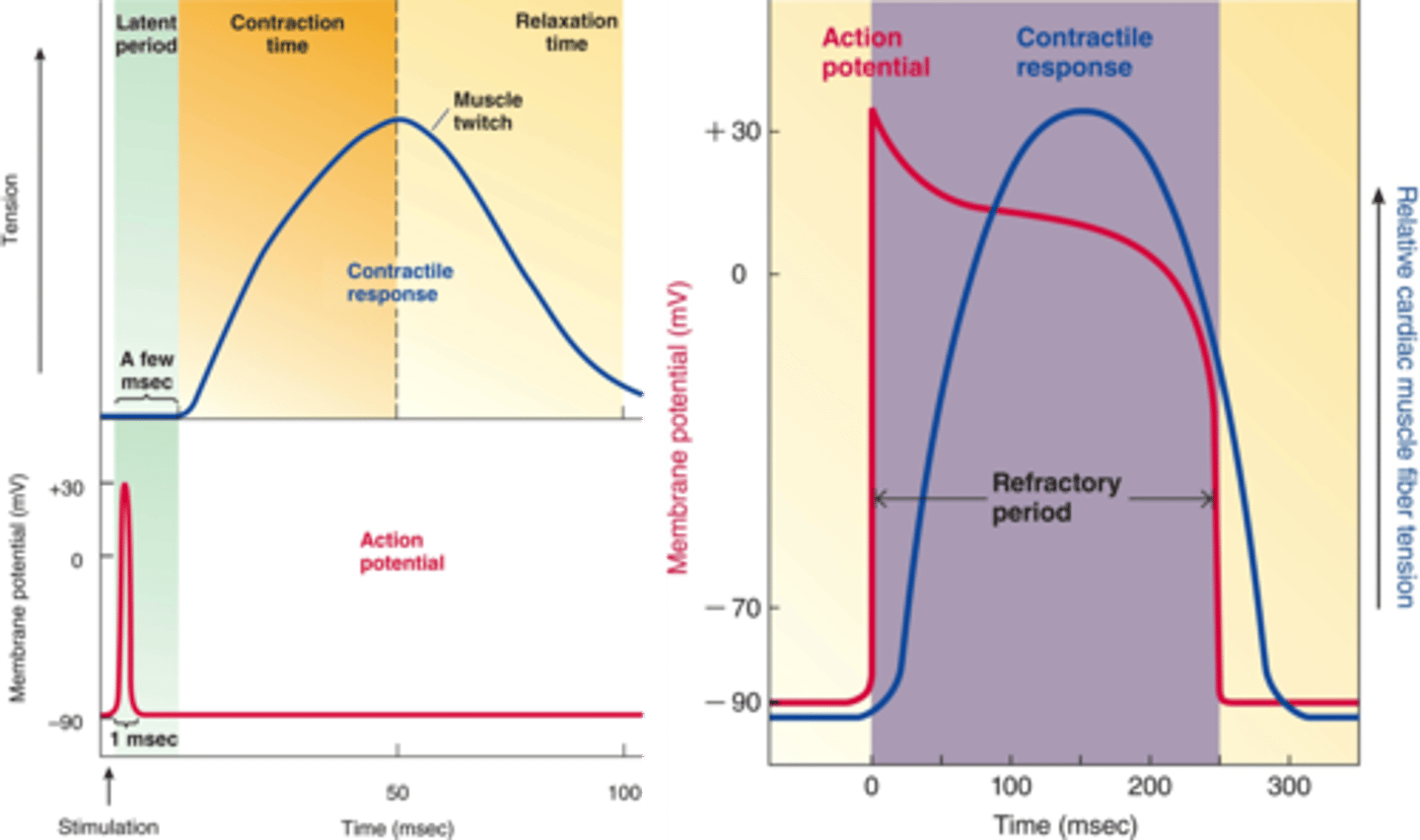
Why wouldn’t summation be an efficient way to increase contraction strength in cardiac muscle?
Because the prolonged refractory period prevents summation
allowing the heart to fully relax and refill between beats, which is essential for effective pumping.
Why is there less chance for summation to occur in cardiac muscle?
Because cardiac muscle has a prolonged refractory period after each action potential, which prevents another action potential from occurring too soon.
This ensures the muscle fully relaxes before the next contraction, reducing the chance of summation.
How can we regulate cardiac contraction strength (if frequency of stimulation or motor unit recruitment is disregarded)?
By varying the concentration of cytoplasmic Ca²⁺.
This affects how many actin–myosin cross-bridges form — more active cross-bridges create a greater overall force of contraction
Which channel is responsible for the shoulder in the fast response cardiac action potential?
L-type voltage gated calcium is responsible for shoulder
What is responsible for the long refractory period in cardiac muscle AP
(2 reasons)
The long refractory period in cardiac muscle is mainly due to:
Sustained calcium influx via L-type calcium channels during the plateau phase keeps the cell depolarized.
Fast sodium channels remain inactivated during this time and can’t reopen until the membrane repolarizes.
T/F: myocardial cells have t-tubules
True
____ is an extension of the plasma membrane that transverses a myocardial cell; important for excitation-contraction coupling
t-tubule
What initiates the cardiac fast action potential and the specific ion channels responsible for each phase:
(1st step of myocardial excitation-contraction coupling)
____ voltage-gated ____ channels are responsible for the upshoot of the AP
____ voltage gated ____ channels are responsible for a brief re-polarization
____ voltage-gated ___ channels are responsible for the shoulder
____ voltage-gated _____ is responsible for re-polarization
Fast voltage-gated sodium channels are responsible for the upshoot of the AP
T-type voltage-gated potassium channels are responsible for a brief re-polarization
L-type voltage-gated calcium channels are responsible for the shoulder (plateau)
Delayed rectifier voltage-gated potassium channels are responsible for re-polarization
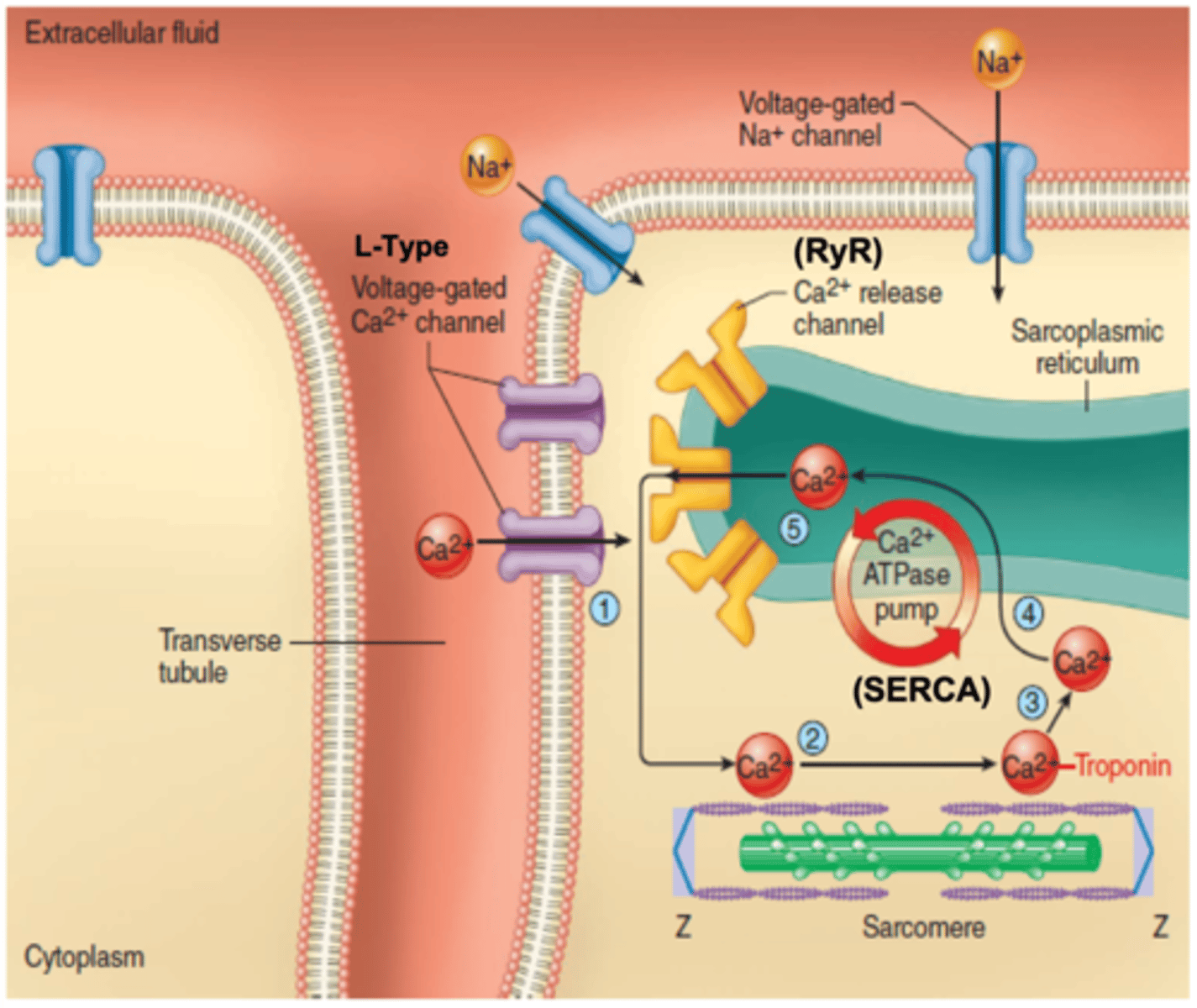
Explain the step by step process of excitation-contraction coupling in myocardial cells. Start at the initiation of the action potential
(end with relaxation)
An AP causes rapid depolarization of the sarcolemma (caused by Na+ influx via fast voltage gated Na+ channels)
Depolarization spreads into the T-tubules, where it opens L-type voltage-gated Ca²⁺ channels.
A small amount of Ca²⁺ enters the cell from the extracellular fluid.
This Ca²⁺ binds to RyRs on the SR, triggering calcium-induced calcium release (CICR).
A large amount of Ca²⁺ is released from the SR into the cytoplasm.
Ca²⁺ binds to TnC, causing a conformational change in TnI, which shifts tropomyosin and exposes cross-bridge binding sites.
As a result, myosin heads can attach to actin, leading to cross-bridge cycling and muscle contraction.
Relaxation begins when Ca²⁺ is pumped back into the SR by SERCA and out of the cell by the sodium-calcium exchanger.
(As cytoplasmic Ca²⁺ levels fall, troponin and tropomyosin return to resting positions, blocking myosin-binding sites and ending contraction.)
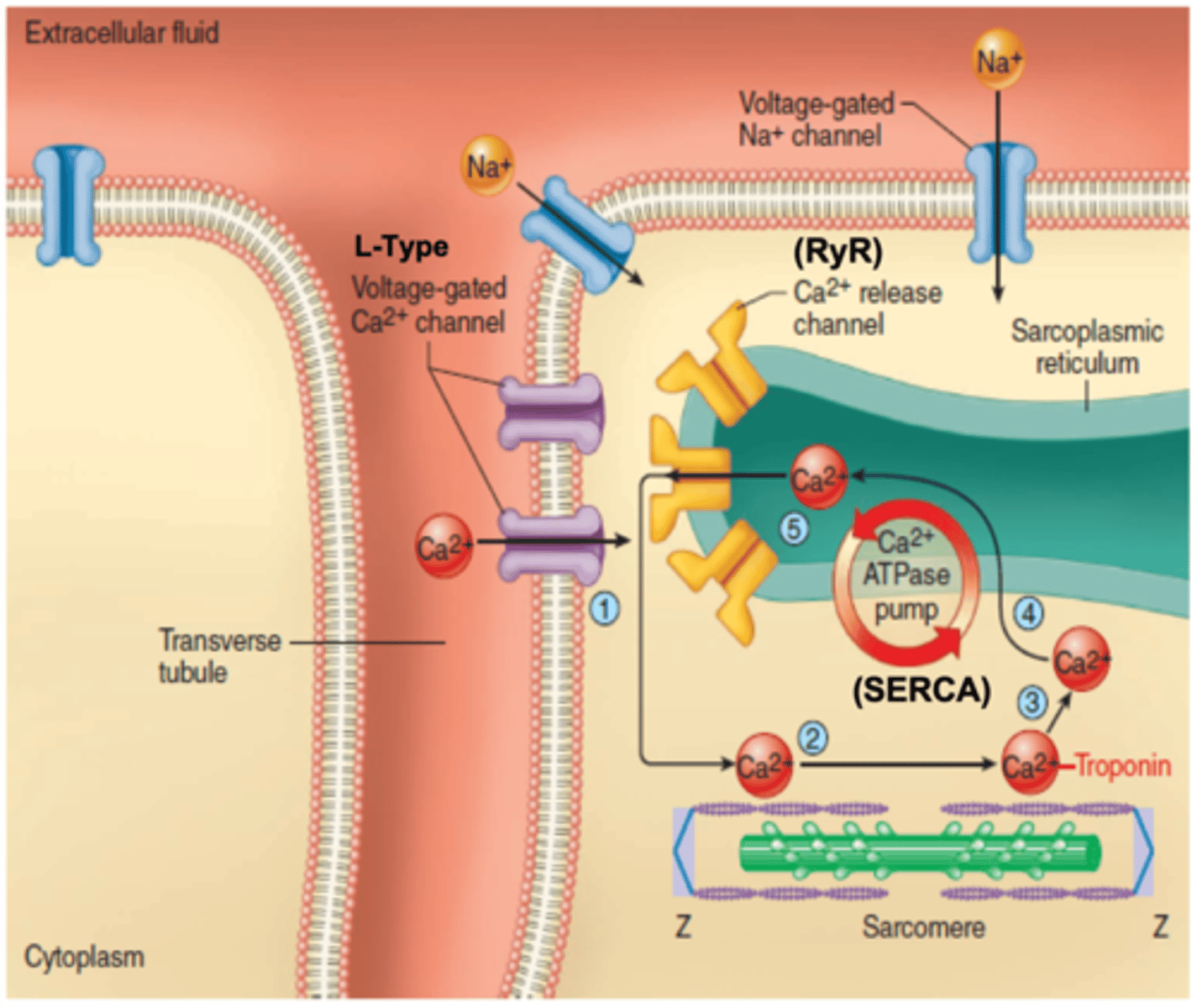
What percentage of calcium involved in excitation-contraction coupling comes from the extracellular fluid? The sarcoplasmic reticulum?
10%; 90%
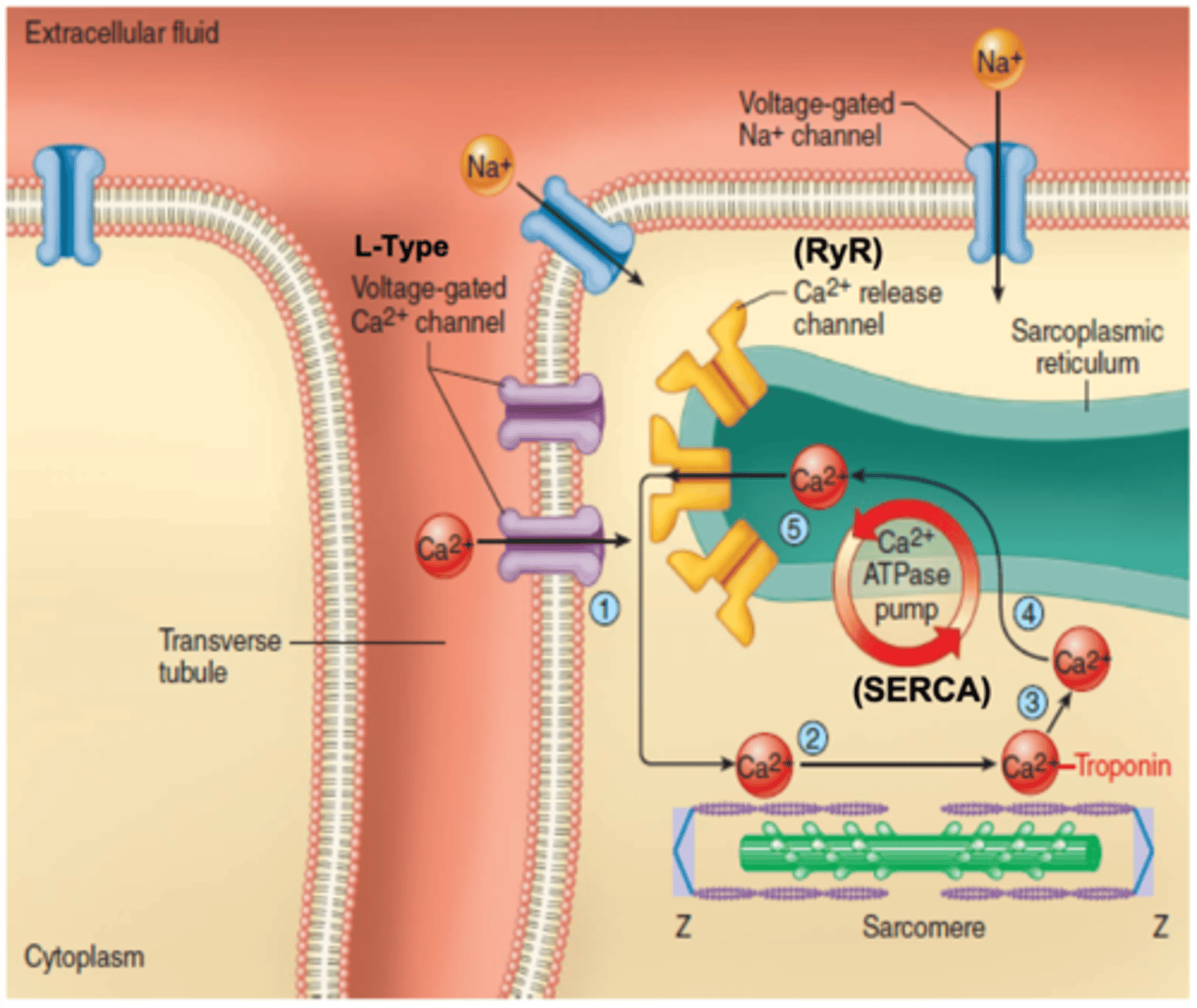
Does the L-type voltage-gated calcium channel provide enough calcium for contraction? Why is it physiologically significant?
The small amount of Ca²⁺ that enters through L-type voltage-gated channels (~10%) is not sufficient on its own for contraction, but it is absolutely essential because it triggers the release of the remaining 90% of Ca²⁺ from the SR.
Without it, no contraction can occur
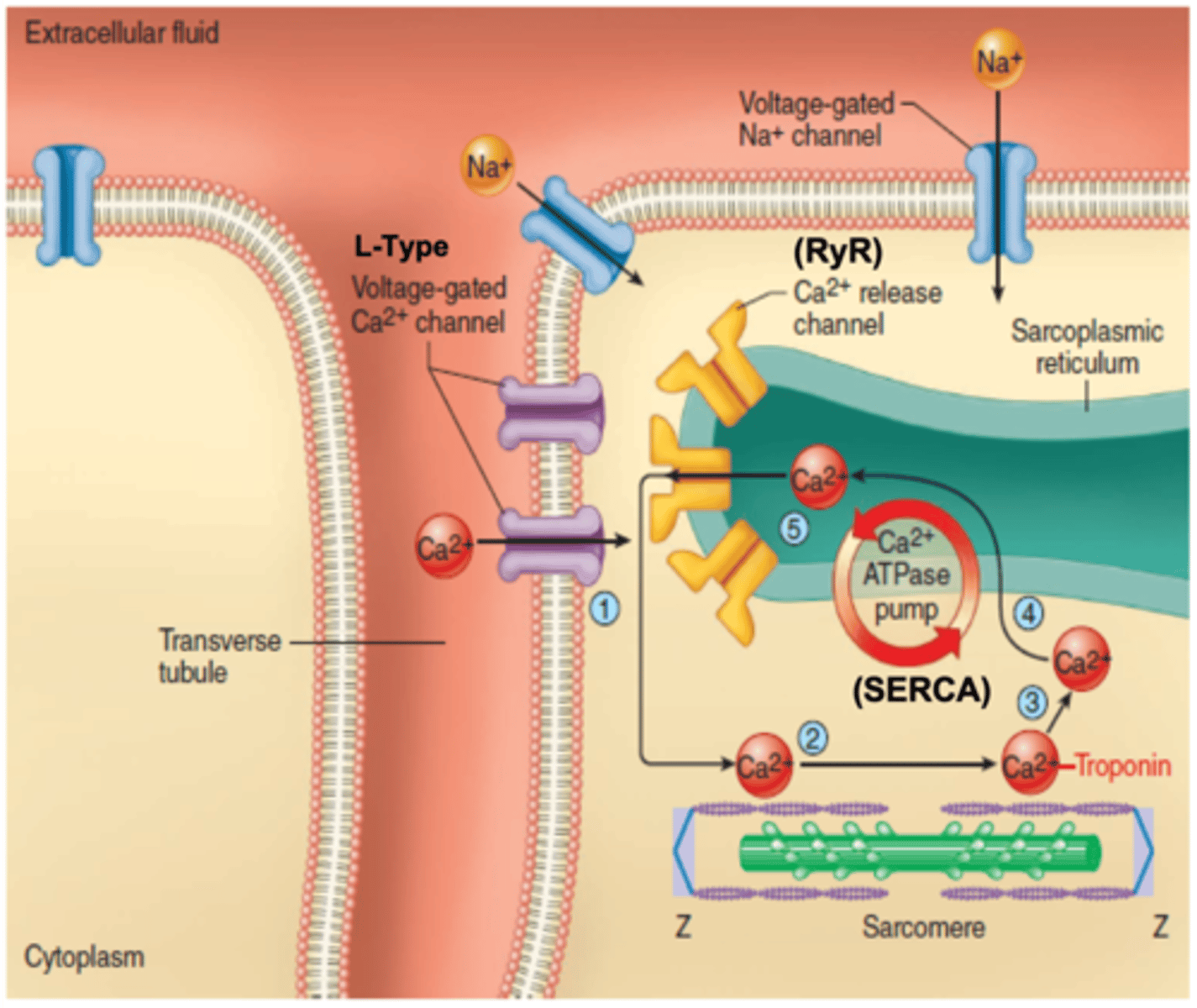
What type of transporter are SERCA pumps?
Does it utilize anything?
primary active transporters (utilize ATP)
What is the function of SERCA pumps in myocardial cells?
Pump calcium ions from the cytoplasm back into the SR lumen
functions to keep cytoplasmic Ca2+ low during resting position
When are SERCA pumps most active in myocardial cells?
(unsure)
SERCA pumps in myocardial cells are most active during diastole, the period of cardiac relaxation
When they are actively pumping Ca2+ from the cytoplasm back into the SR.
___ depicts the temporal relationship between individual events of a cardiac cycle.
Wigger's Diagram
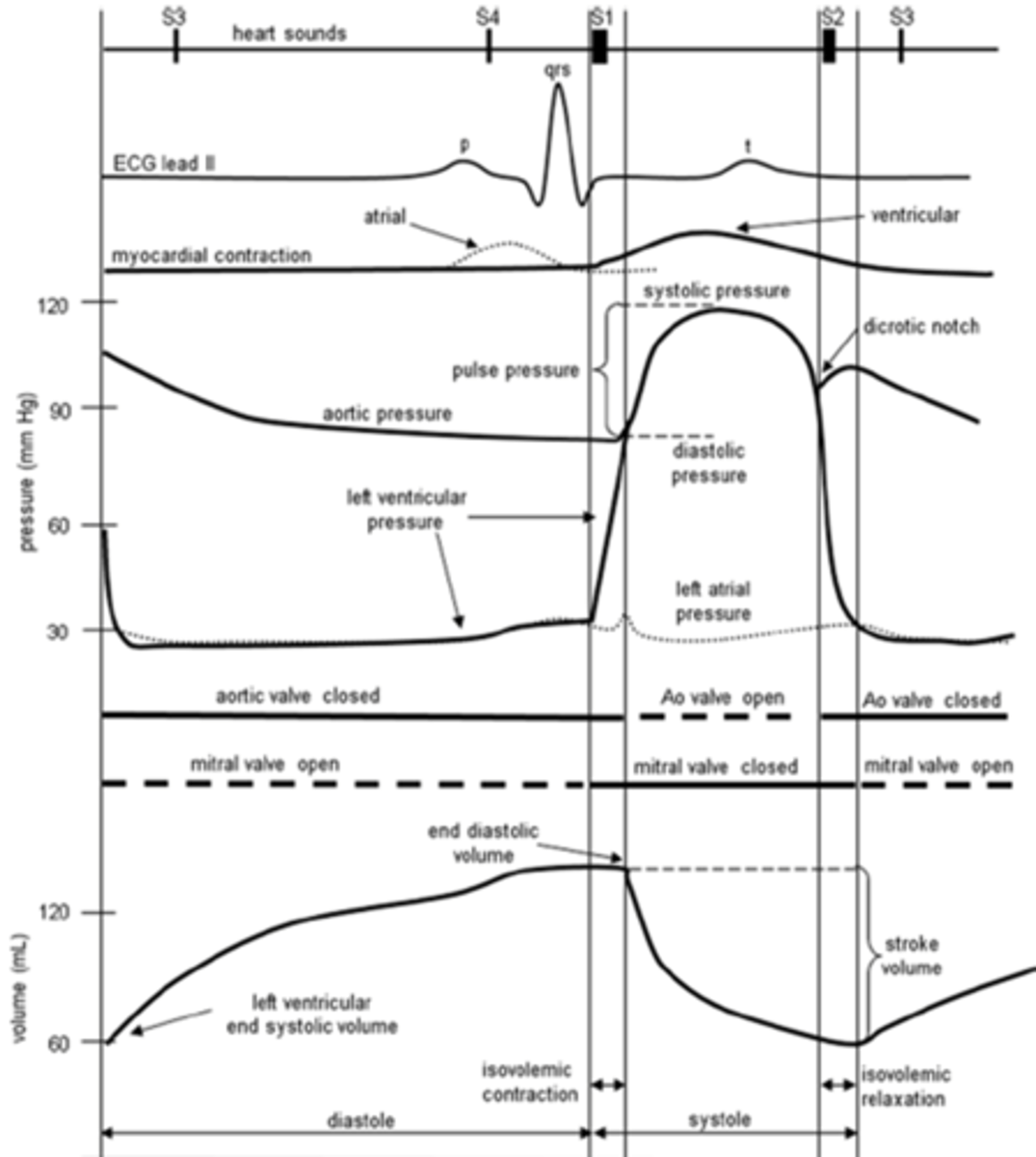
define Wigger's Diagram
a graph that depicts the temporal relationship between individual events of a cardiac cycle.
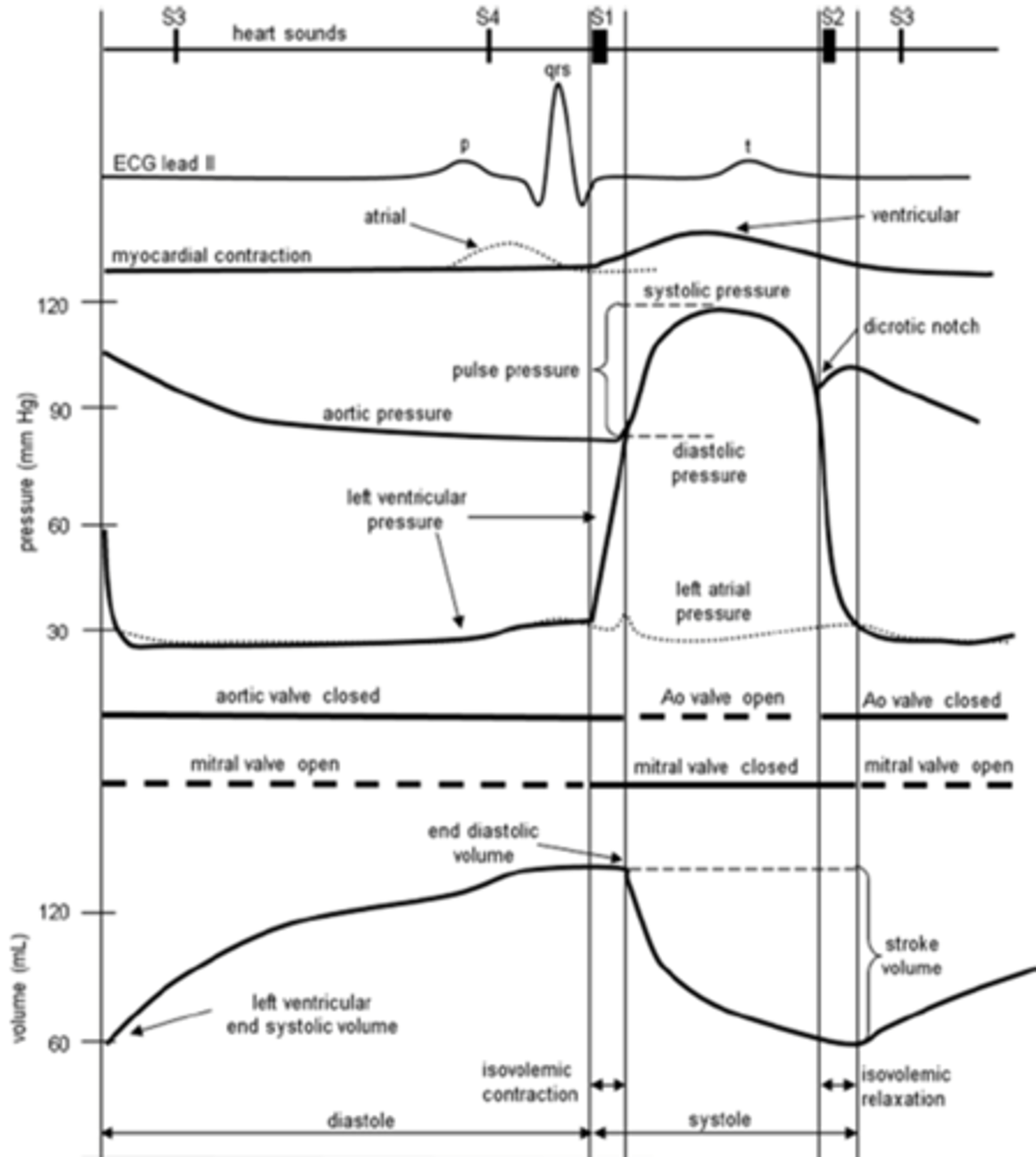
A Wigger's diagram depicts the ___ relationship between individual events of a cardiac cycle.
temporal
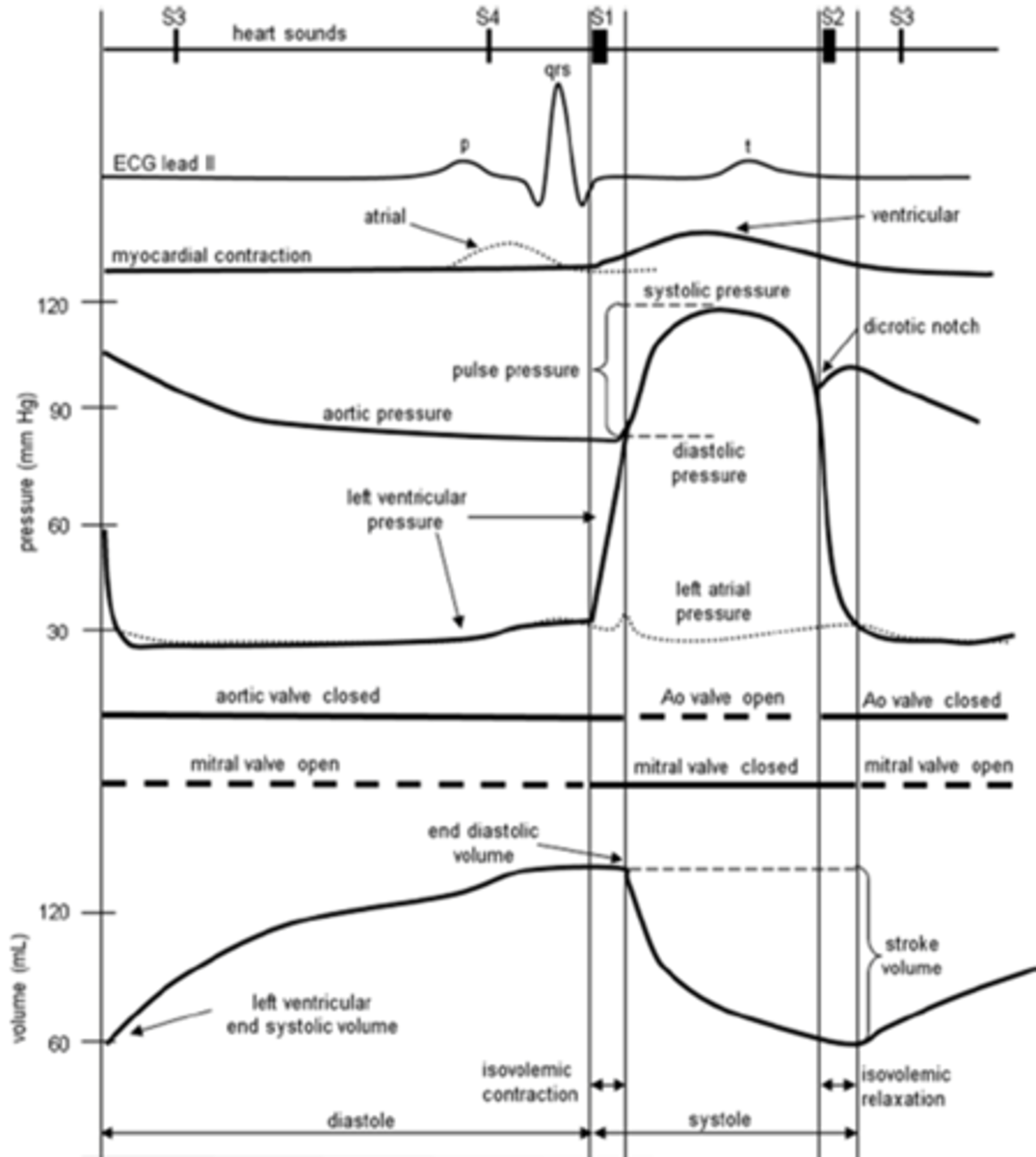
A Wigger's diagram depicts the temporal relationship between individual events of a ___.
cardiac cycle
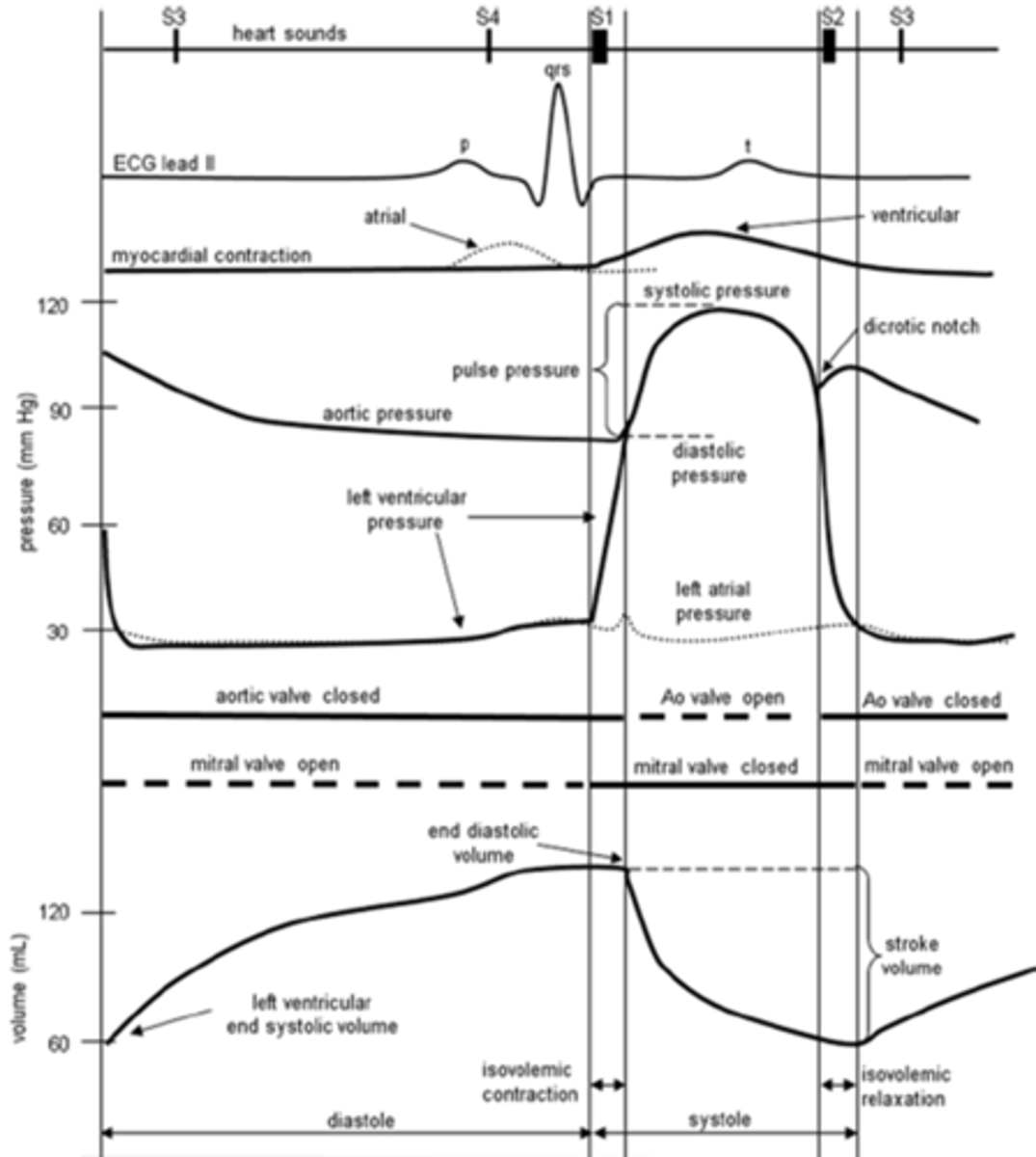
___ is the series of events in a single heartbeat
cardiac cycle
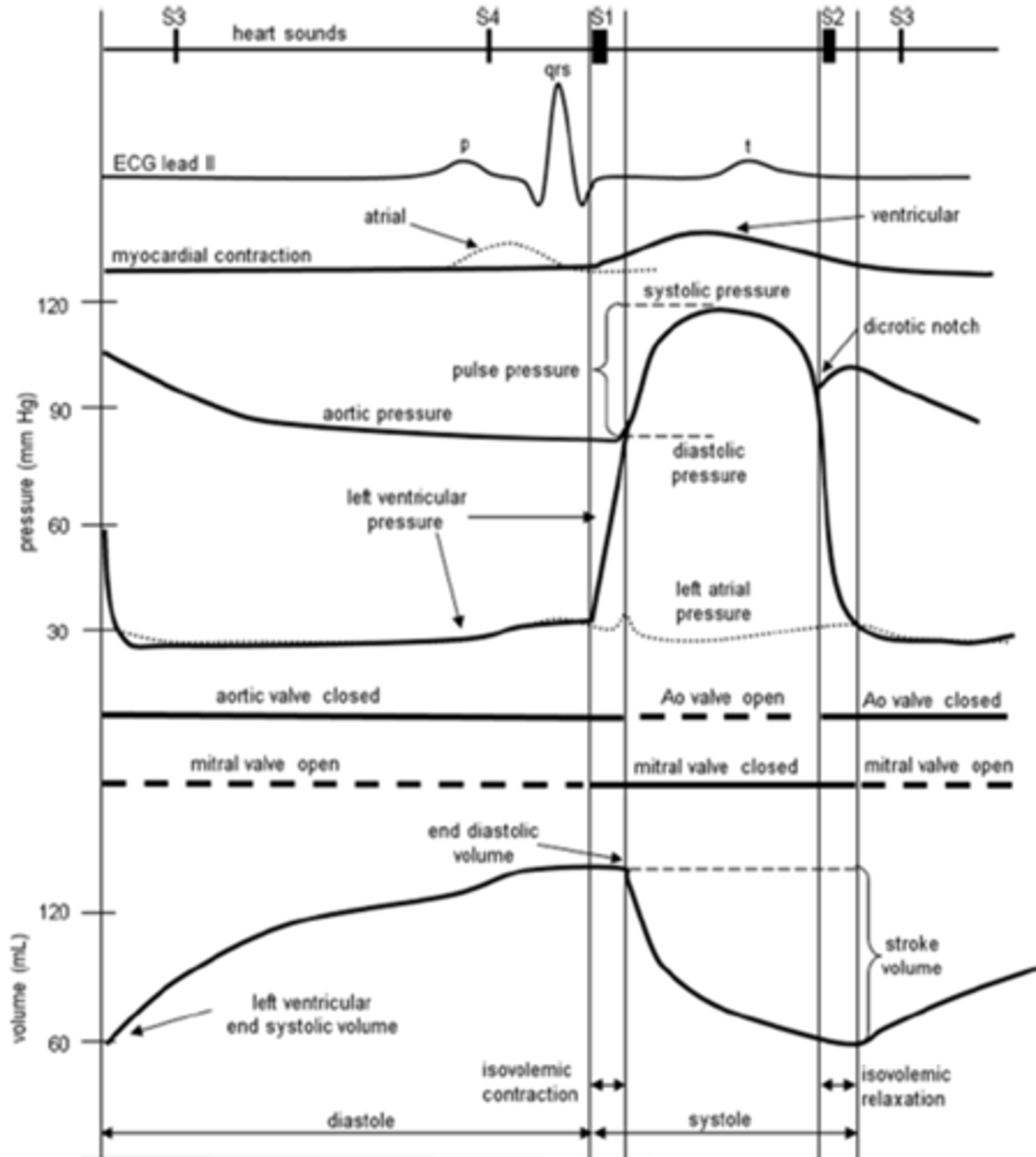
Which 4 things are included in a Wigger's diagram?
- ECG (mV; non-invasive clinical measurement that gives us markers of certain events in the cardiac cycle)
- Pressures (mmHg) in the ventricles, atria, and aorta
- Volumes (mL) in the ventricle
- Heart sound
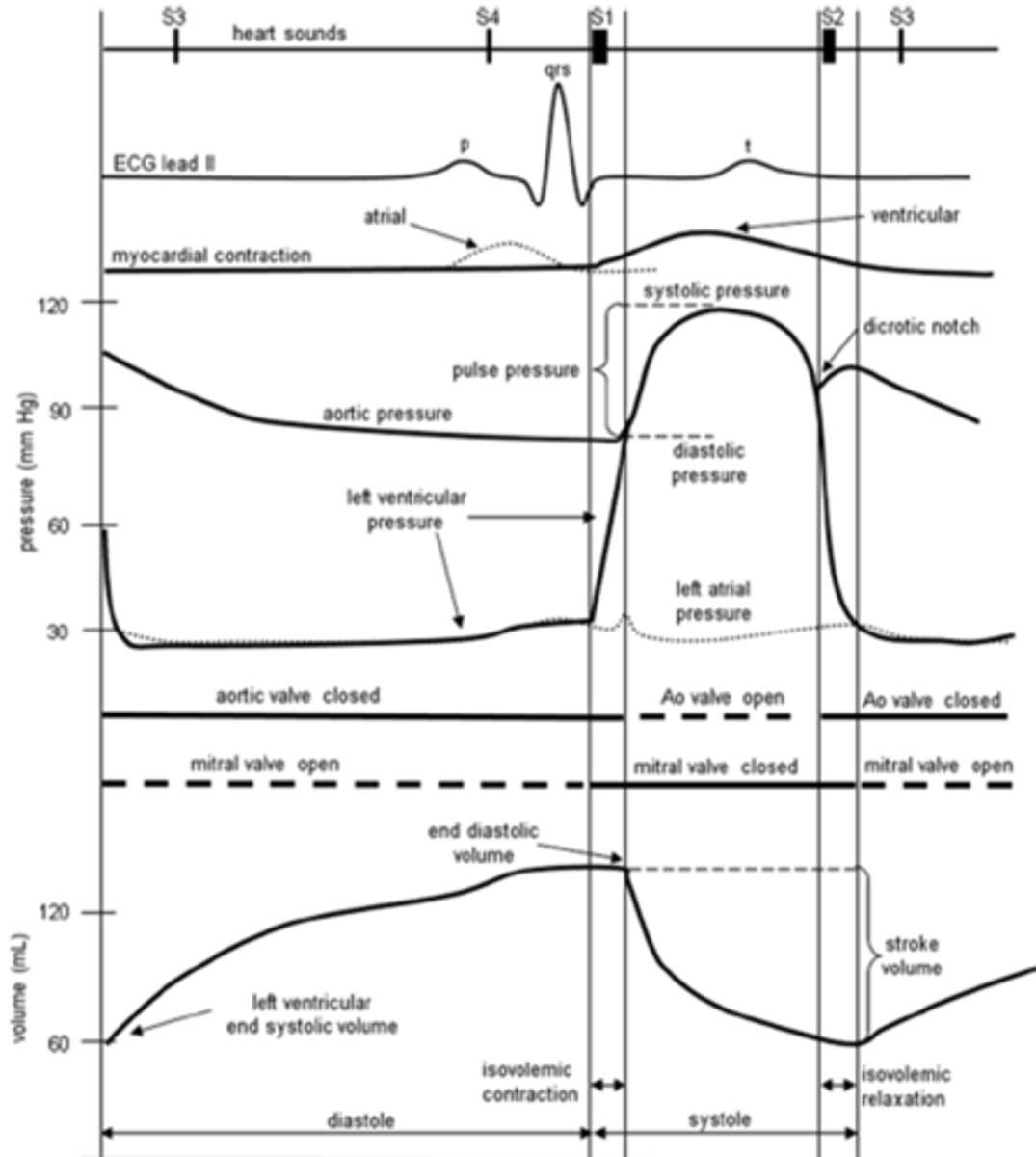
Starting midway through ventricular diastole, what is the state of the ventricles and atria?
(mention pressure)
Both the ventricles and atria are relaxed and passively filling (in a phase of passive ventricular filling; ventricular pressure is slightly lower than atrial pressure)
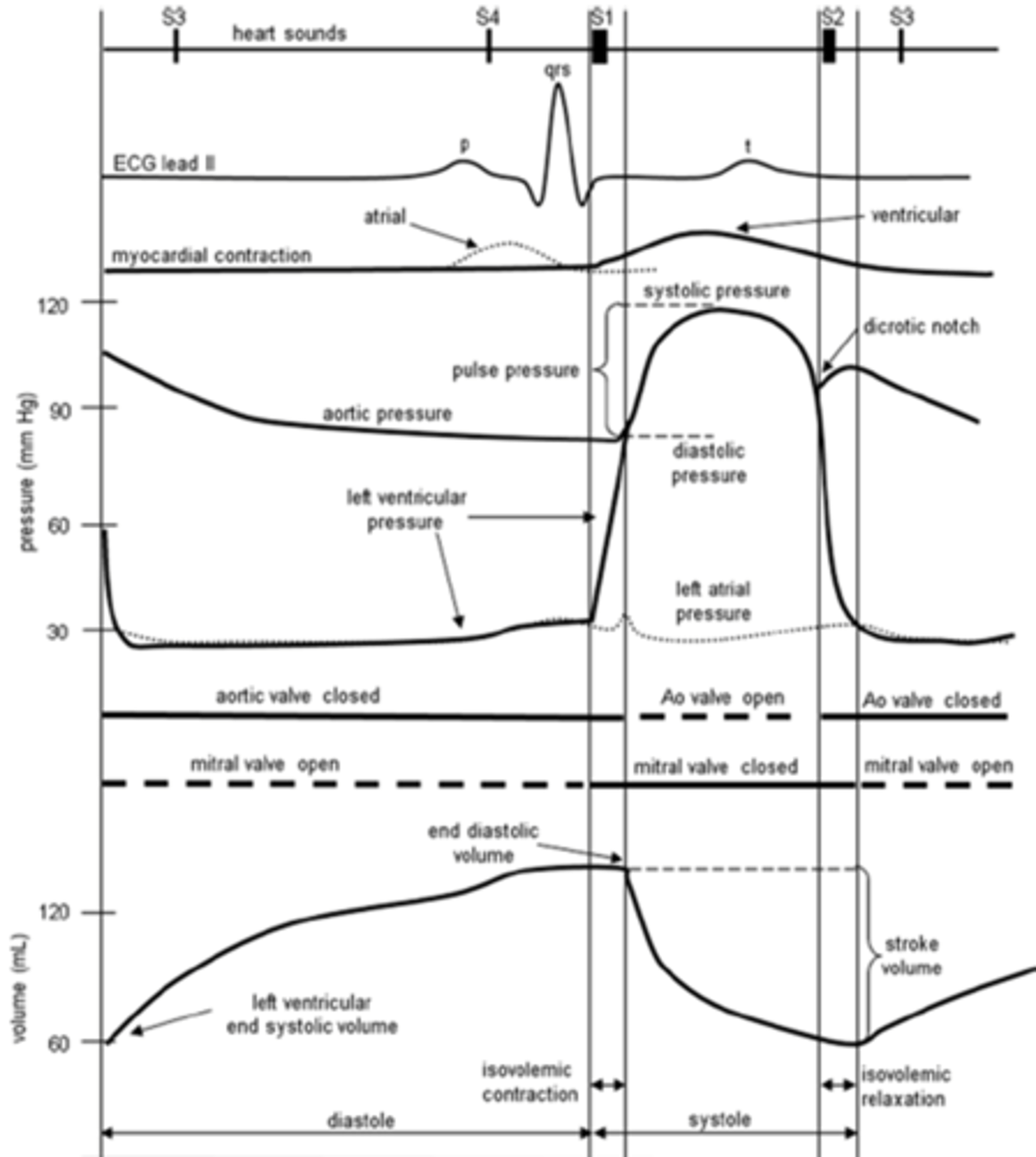
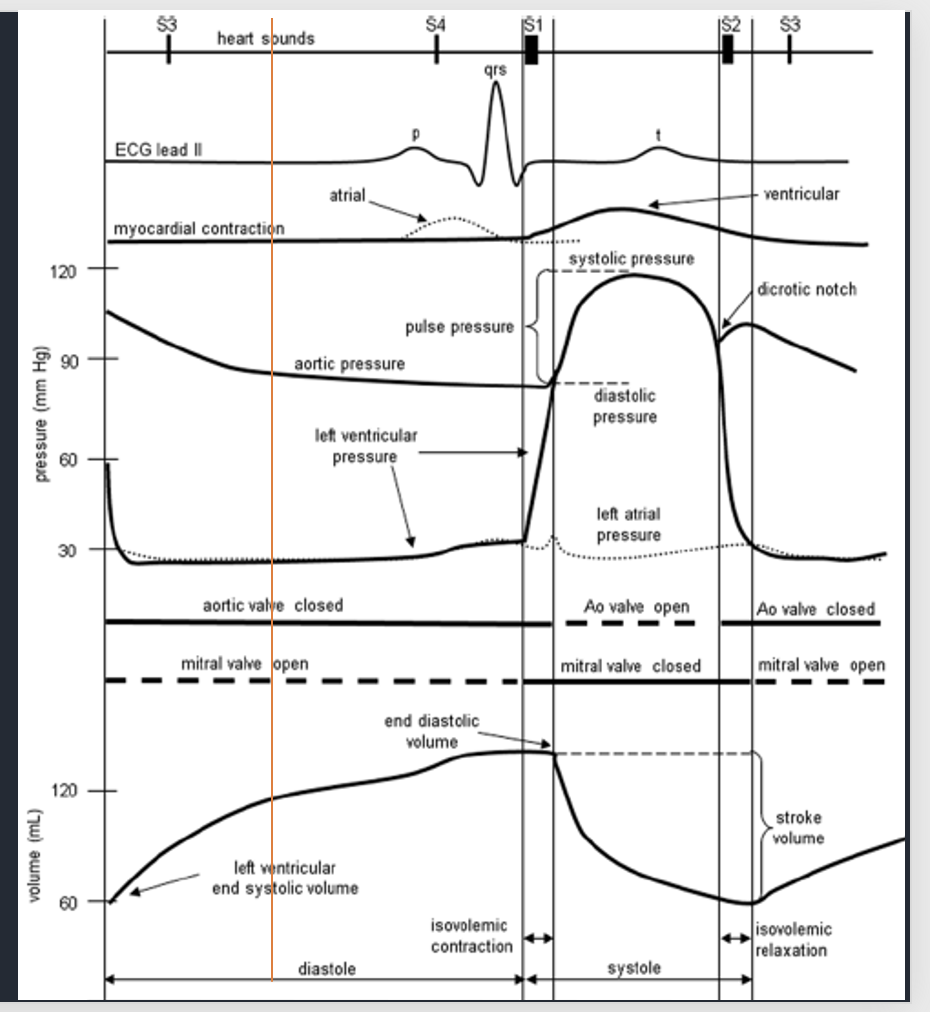
Starting midway through ventricular diastole (red line), what is the state of the ventricles and atria?
Ventricles are ____, atria are ___
In a phase of passive ___ ___
Ventricular pressure is slightly ___ than atrial pressure
Ventricles are relaxed, atria are relaxed
In a phase of passive ventricular filling
Ventricular pressure is slightly lower than atrial pressure
What does the P-wave in an ECG represent?
(aka what electrical events causes P wave)
atrial depolarization
What does the P wave (atrial depolarization) directly result in?
atrial contraction
___ drives active ventricular filling.
Atrial contraction
What does atrial contraction (which is a result of atrial depolarization = p-wave) result in?
active ventricular filling
The P wave on an ECG represents ____ ___, which precedes and causes ___ ___.
This contraction contributes to the final phase of ___ ____ called ____ ____.
The P wave on an ECG represents atrial depolarization, which precedes and causes atrial contraction. This contraction contributes to the final phase of ventricular filling called active filling.
What mechanical event marks the beginning of active filling?
atrial contraction
What is the physiological purpose of atrial contraction?
Pushes last 20% of blood into the ventricles
What is AV nodal delay?
What is the physiological significance of the AV nodal delay?
The AV nodal delay is the brief pause in electrical signal transmission between the atria and ventricles
This delay ensures that the atria fully contract and empty their blood into the ventricles before the ventricles begin to contract, optimizing ventricular filling and maximizing
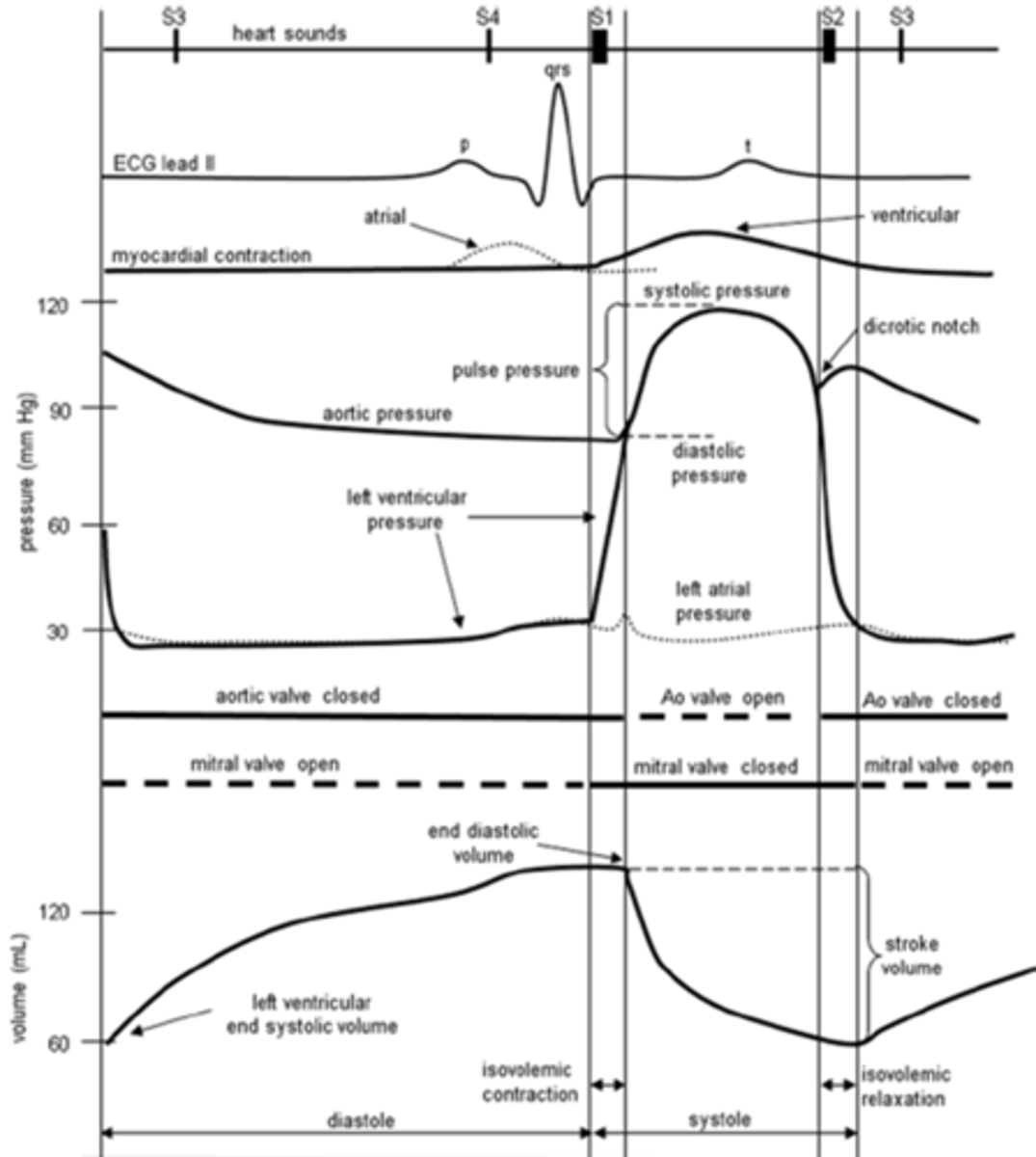
What would occur without AV nodal delay
end-diastolic volume (EDV) would drop by ~20%, reducing the heart's efficiency by about 20%.
What does the P-R interval represent on the ECG?
AV nodal delay
What marks the AV nodal delay on an ECG?
P-R interval
What marks atrial depolarization on an ECG?
P wave
Systole is the phase of cardiac muscle __________, which causes chamber pressure to __________.
Diastole is the phase of cardiac muscle __________, which causes chamber pressure to __________.
Systole is the phase of cardiac muscle contraction, which causes chamber pressure to increase.
Diastole is the phase of cardiac muscle relaxation, which causes chamber pressure to decrease.
During atrial contraction, what is true of the pressure gradient between the atria and the ventricles? where does blood flow
atrial pressure is higher than ventricular pressure (blood flows down its pressure gradient into the ventricles)
What does the QRS complex in an ECG represent?
ventricular depolarization
What does ventricular depolarization (QRS complex) directly result in?
ventricular contraction
What happens to the pressure in the ventricles as they contract?
increase in pressure
When the pressure increases in the ventricles after they contract, what does this directly result in?
ventricular pressure surpasses that of the Atria, which pushes closed the AV valve
What is the first heart sound a marker of?
AV valve closure
What mechanical event marks the beginning of isovolumetric ventricular contraction?
AV valve closure (first heart sound)
What can be measured as soon as the AV valves are shut?
end diastolic volume (largest volume present in the ventricles in any cardiac cycle)
What occurs during isovolumetric contraction?
ventricular pressure increases (but volume does not); occurs until it surpasses the pressure of the aorta
What causes the opening of the semilunar valves?
When ventricular pressure surpasses that of the aorta
What marks the beginning of ejection?
opening of the semilunar valves (ventricular pressure higher than pressure in the aorta; driving blood to leave the ventricles)
In the lab, what is a marker of ventricular ejection?
pulse (arterial pulse)
What does the t-wave represent?
ventricular repolarization
When does the t-wave occur with regards to the contraction of the heart?
t-wave (ventricular repolarization) occurs just before the ventricles relax
T/F: Ventricular repolarization causes the ventricles to relax.
False; no true cause and effect mechanism; however, from a temporal standpoint, the t-wave marks ventricular repolarization (but it occurs at the same time that ventricles relax)
What causes the semilunar valves to close?
when pressure in the ventricles drops below the aorta
What is the dicrotic notch?
pressure blip in the aorta that marks the closure of the semilunar valves and the second heart sound
What does the dicrotic notch marks?
semilunar valve closure (which causes the second heart sound)
What starts the beginning of isovolumetric ventricular relaxation?
closure of semilunar valves (can be seen at dicrotic notch, which aligns with the second heart sound)
During isovolumetric relaxation, how are the volume and pressure changing?
No change in ventricular volume, however, there is a decrease in ventricular pressure
Where can the end-systolic volume be measured?
the volume at the end of ejection (when the semilunar valves close)
What causes the opening of the AV valves?
when ventricular pressure drops below atrial pressure during isovolumetric relaxation (pressure gradient causes the opening of AV valves and the start of passive filling)
What causes first heart sound?
closure of AV valves
What causes the second heart sound?
closure of semilunar valves
What phase does the first heart sound mark the beginning of?
isovolumetric contraction
What electrical event is the QRS complex?
(skip)
ventricular depolarization
What mechanical event directly follows the QRS complex?
(skip)
ventricular contraction
What is true of the events of the cardiac cycle on the right side of the heart compared to the left side of the heart?
The same events are going on in the right side of the heart, but they are occuring at a lower pressure (pressure gradients are still there to allow these processes to happen though)
What can the functionality of the heart be expressed in terms of?
(slide 19)
cardiac output (CO)
___ is the volume of blood pumped by each ventricle per minute (L/min)
cardiac ouput
Cardiac output is the ___ of blood pumped by each ___ per ___
the volume of blood pumped by each ventricle per minute (L/min)
What is cardiac output?
The volume of blood pumped by each ventricle per minute (L/min)
What are the units of measurement for cardiac output?
L/min
What does it mean to say that the heart function as a demand pump?
The heart is going to pump the volume of blood per unit time that is going to satisfy the metabolic demand that is currently present in the tissues (at a given level of metabolism, there is a certain amount of nutrients utilized and a certain amount of waste products produced; the cardiac function driving the flow rate of blood must be sufficient to replace nutrients used and get rid of waste products)
What does increased metabolism in the tissues require?
an increased volume of blood per unit of time (increased cardiac output); as metabolism changes, the delivery of blood must match (otherwise, we wouldn't have the maintenance of nutrients or removal of waste products)
T/F: The rate of blood flowing through circulation is kept constant.
False; Not something that is homeostatically regulated (going to change as the demands of the body change)
How can we measure the true functionality of the heart?
cardiac output (volume of blood pumped by a ventricle per unit of time)
What are the units for cardiac output (CO)?
measured in liters of blood per minute (L/min); liters of blood passing a given point per unit of time
Which two things is cardiac output dependent upon?
heart rate (HR) and stroke volume (SV)
(independent variables)
In what ways can we manipulate cardiac output?
manipulate heart rate or stroke volume (because CO is a function of heart rate and stroke volume)
Why is cardiac output altered?
in order to match blood flow rate to tissue with metabolic demand
another word for the delivery of blood to a tissue
perfusion
Cardiac output is regulated to match blood ___ (perfusion) with ____ demand of the tissues
CO is regulated to match blood flow rate (perfusion) with metabolic demand of the tissues
What is the rate of resting cardiac output?
5 L/min
What can cardiac output increase up to (from the resting rate)?
Aka what is the maximum cardiac output that can be reached
Can increase to rates of 20 to 25 L/min
Approximately what volume of blood does one have in their body?
5 L
Why is cardiac cycle considered to be very efficient in humans?
- You have approximately 5 liters of blood in your body
- Efficient process
- Each ventricle pumps your entire blood volume per minute
CO is regulated to match ___ with ___ of the tissues.
blood flow rate (perfusion); metabolic demand
What is the resting cardiac output?
5 L/min
What capacity does the cardiac output have to increase to meet metabolic demand of active tissues?
4-6 fold
What is the cardiac reserve?
the difference between cardiac output at rest and the maximum cardiac output (which can reach flow rates of 20-25 L/min)
___ is defined as the difference between cardiac output at rest and the maximum cardiac output.
cardiac reserve
The maximum cardiac output can reach flow rates of about ___ L/min.
20-25 L/min