Systems Path Heart
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
what happens when heart can't meet demands (MC) or increased tissue command occurs results in cognition "backing up" in pulmonary and systemic circulation
heart failure (CHF)
heart failure symptoms
dyspnea, fatigue, orthopnea, tachycardia
how does CHF occur?
increased tissue congestion and complications due to compensations
who gets CHF?
older individuals or those that have had MI (and other risks)
causes of CHF
history of MI, HTN, CAD
Systolic dysfunction (CHF) results in
weak contraction
diastolic dysfunction (CHF) results in
failed relaxation
valvular dysfunction (CHF) results in
failure to effectively seal
forward failure (CHF) results in
insufficient output
backward failure (CHF) results in
congestion
forward failure is almost always accompanied by what?
backward failure (impacts virtually every organ)
The greater the stretch, the stronger is the heart's contraction.
Result is increased output
Cost is increased O2 and tension
frank-starling law
which neurohumoral mechanism increases HR and contractility?
NE
which neurohumoral mechanism causes diuresis and vasodilation?
ANP
structural changes associated with compensated heart failure
cardiac hypertrophy
cost is increased O2 consumption
what type of cardiac hypertrophy is pathologic resulting in increased pressure (HTN/valve stenosis)
concentric hypertrophy
what type of cardiac hypertrophy is physiologic and causes increased volume, bradycardia, and increased capillary density
eccentric hypertrophy

causes of left sided heart failure
HTN, CAD, valve disorders, cardiomyopathies
effects of left-sided heart failure
left ventricle hypertrophies, gradual decreased cardiac output (causing pulmonary edema), cough, dyspnea, rales, orthopnea, tachycardia
left ventricle decreased output and hypertrophy, increased pulmonary HTN
left-sided heart failure
how does left-sided heart failure occur?
prior damage to left side of heart from MI/cardiomyopathies
who gets left-sided heart failure?
those with previous complications
causes of left-sided heart failure
history of CAD, HTN, cardiomyopathies and MI
what is the MC cause of right-sided heart failure?
left sided heart failure
what is right ventricle pump failure, MC from left heart failure but also from lung pathologies?
right-sided heart failure
how does someone get right-sided heart failure?
increase pressure in pulmonary circulation -> hypertrophy
who gets right-sided heart failure?
those with hx of left heart failure or lung pathologies
when heart is overloaded by increased pressure
hypertensive heart disease
types of hypertensive heart diseases
systemic and pulmonary
left ventricle overworked by increased HTN
systemic hypertensive heart disease
complications associated with systemic hypertensive heart disease
CHF, arrhythmia, stroke, renal failure
how does systemic hypertensive heart disease occur?
hypertrophy of left ventricle not accompanied by increased blood supply
who gets systemic hypertensive heart disease?
those with history of HTN (African Americans)
possible causes of systemic hypertensive heart disease
stress, high sodium, low physical activity, atherosclerosis
right sided heart disease due to a lung pathology causing right ventricular hypertrophy
pulmonary hypertensive heart disease
acute pulmonary hypertensive heart disease is associated with what?
large PE (saddle embolism) which obstructs pulmonary a.
chronic pulmonary hypertensive heart disease is associated with what?
prolonged lung pathology
what accounts for 30% of all birth defects ranging from mild to severe/lethal?
congenital heart disease
risks associated with congenital heart disease
prematurity, trisomies, teratogens, material diabetes, fetal infection
left-to-right shunts
VSD, ASD, PDA
right-to-left shunts
tetralogy of fallout, transposition of great arteries
examples of obstructed flow causing CHD
valve stenosis, aortic coarctation
MC congenital heart defect (left-to-right shunt in ventricles)
ventricular septal defect
how does VSD occur?
increased pressure on R side of heart and pulmonary circulation
2nd MC congenital heart defect (left to right shunt in atria)
atrial septal defect
congenital malformation involving four distinct heart defects (right to left shunt)
tetralogy of fallot
the defects associated with tetralogy of fallot
VSD, pulmonary valve stenosis, overriding aorta, R ventricular hypertrophy
tetralogy of fallot is the MC congenital heart disease to cause ________
cyanosis
tetralogy of fallot is characterized by a ______ - shaped heart
boot

how does tetralogy of fallot occur?
4 malformations -> deoxygenated blood to be pumped into circulation -> cyanosis
swapped aorta and pulmonary trunk which is "incompatible with postnatal life" if no intervention is done = cyanosis + death
transposition of the great arteries
with transposition of the great arteries, the right ventricle is connected ->
aorta
with transposition of the great arteries, left ventricle is connected ->
pulmonary artery
how does transposition of the great arteries occur?
R ventricle pumps deoxygenated blood into systemic circulation
congenital narrowing of aorta
aortic coarctation
who is most likely to get an aortic coarctation?
males, turner syndrome
what type of aortic coarctation is associated with PDA and causes shunting of blood from pulmonary trunk to aorta
infantile (pre-ductal)
infantile aortic coarctation causes what?
cyanosis, hypoxia, R ventricular hypertrophy
what type of aortic coarctation is associated with the ligamentum arteriosum, MC asymptomatic, and causes increased BP in head/upper extremities but lower BP in lower extremities/kidneys
adult (post-ductal)
how does aortic coarctation occur?
narrowing restricts flow to lower extremities
group of conditions following ischemia
ischemic heart disease
ischemia to heart causes infarction after how long?
20-40 minutes
what is associated with 90% of IHD cases?
CAD
progression of IHD causes what?
fatty streaks, atheroma, luminal stenosis, thrombosis
acute cardiac syndromes (caused by sudden and significant ischemia)
angina pectoris, acute MI, sudden cardiac death, chronic IHD->CHF
(stable) cardiac chest pain that is a result of ischemia associated with a 70% occluded coronary artery with exertion substernal chest pain, back, jaw, left arm and shoulder pain which responds to rest and vasodilators
stable angina pectoris
how does stable angina pectoris occur?
slow growing atherosclerotic plaques causing stenosis
risk associated with developing angina pectoris (both types)
poor diet, ↓ exercise, dyslipidemia, smoking
(unstable) cardiac chest pain that is a result of ischemia associated with 90% occluded coronary artery with or without exertion, not improved by rest or vasodilating meds
unstable angina pectoris
how does unstable angina pectoris occur?
acute plaque disruption with significant and acute clotting of vessel
what is associated with angina pectoris in females?
nausea, dizziness, back pain, "discomfort" in lower chest/epigastric region, dyspnea and fatigue
myocardial cell death due to ischemia
myocardial infarction (MI)
how does someone get a MI?
acute plaque disruption with significant/acute clotting of vessel
artery MC involved in a MI
left anterior descending
risk associated with myocardial necrosis
HTN, smokin, CHF, diabetes, males age 40-60, postmenopausal females, sickle cell disease, amyloidosis
symptoms of MI
"crushing" pain, intense pressure, thready pulse, dyspnea, nausea, sweaty
cardiac markers
troponin, CK-MB, myoglobin
progressive heart failure, secondary to ischemic damage due to past MI or long-term CAD
chronic ischemic heart disease
sudden sustained arrhythmia leading to pump failure and death
sudden cardiac death (SCD)
MC cause of SCD
ischemic injury (CAD)
how does someone get SCD?
interruption of normal heart rhythm leading to systole or v-fib
who/why does someone get SCD?
Hx. of MI leading to fibrosis of heart, cardiomyopathies
chest wall trauma induced arrhythmia which causes SCD and is 50% lethal
commotion cordis
who does commotio cords occur in?
younger male athletes with underdeveloped chest
valvular heart diseases
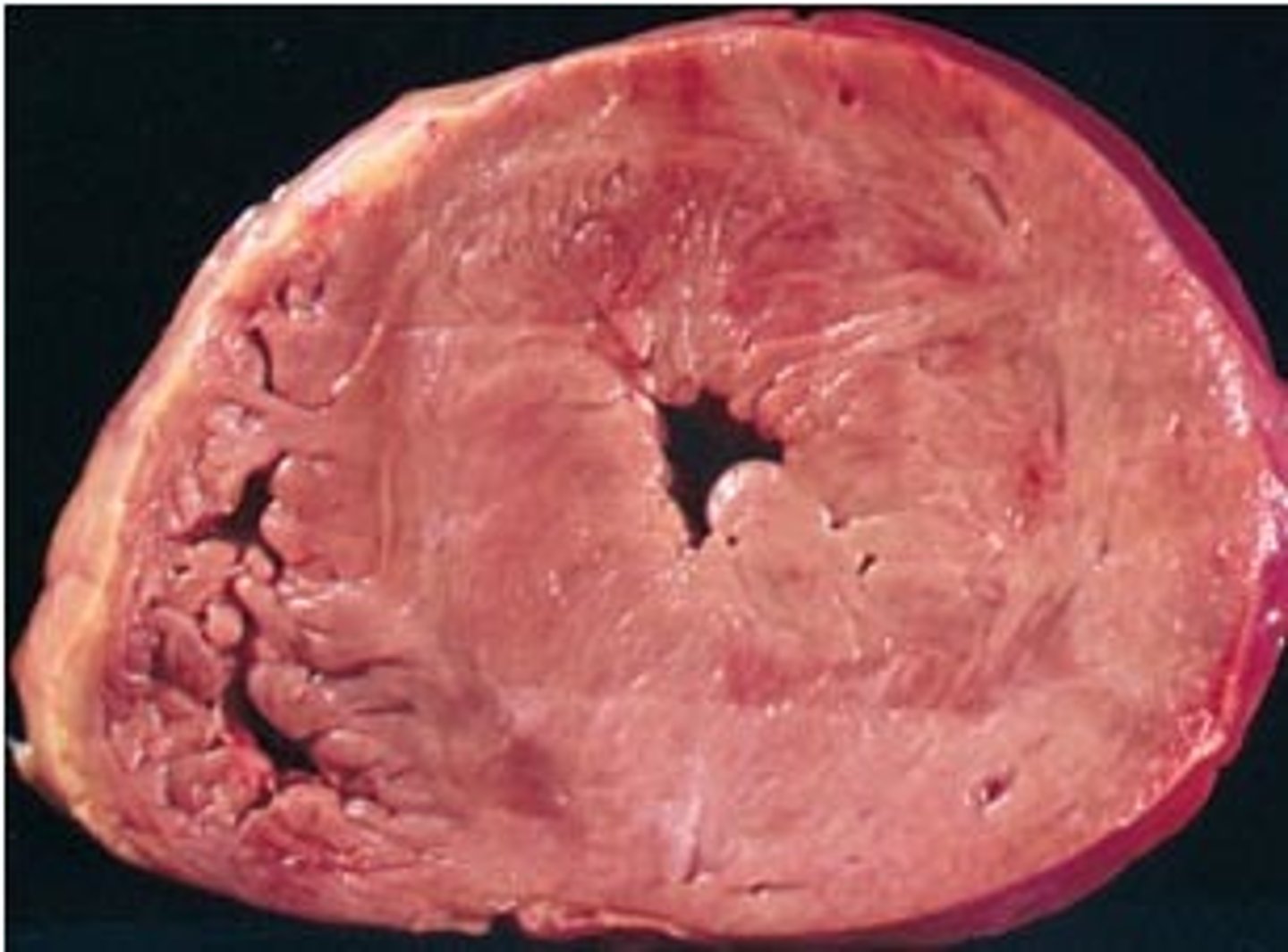
stenosis, insufficiency, murmur
narrowing of heart valve, failure to open (calcification or fibrosis)
stenosis
failure of heart valve to close
insufficiency (aka regurgitation or incompetence)
turbulent flow through diseased valve
murmur
turbulence causing palpable vibration in heart
thrill
Mc cause of aortic valve stenosis
calcific aortic stenosis
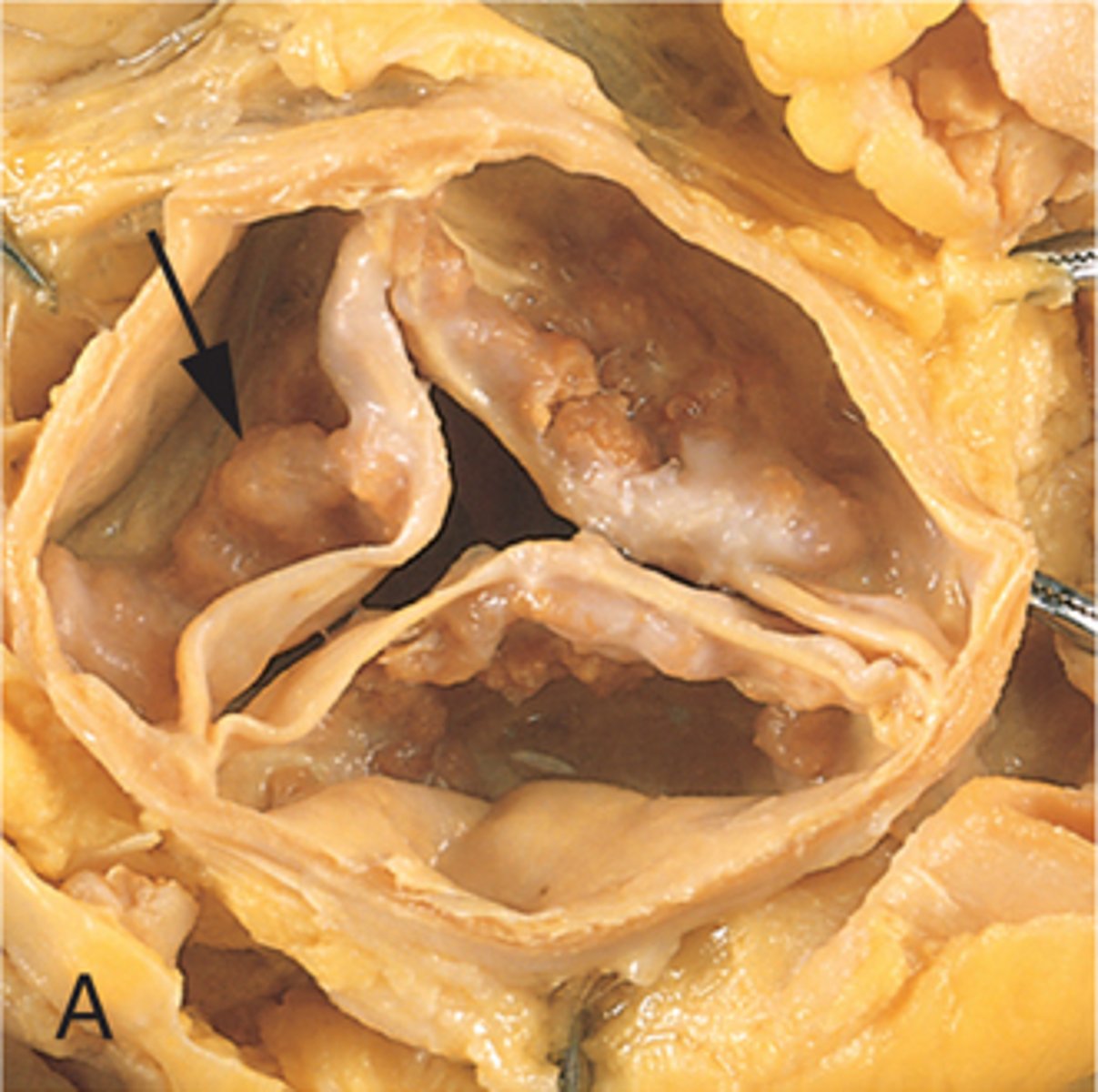
symptoms of the early stages of calcific aortic stenosis
asymptomatic, murmur, decreased cardiac output
symptoms of late stages of calcific aortic stenosis
left ventricular hypertrophy, Ca+-> severe stenosis
who is most likely to get calcific aortic stenosis ?
70-80 or younger with bicuspid aortic valve
risks associated with calcific aortic stenosis
HTN, infection/inflammation, increased cholesterol, bicuspid aortic valve
inflammatory valve disease 2-3 weeks after group A beta hemolytic strep infection NOT active bacterial infection
rheumatic valve disease
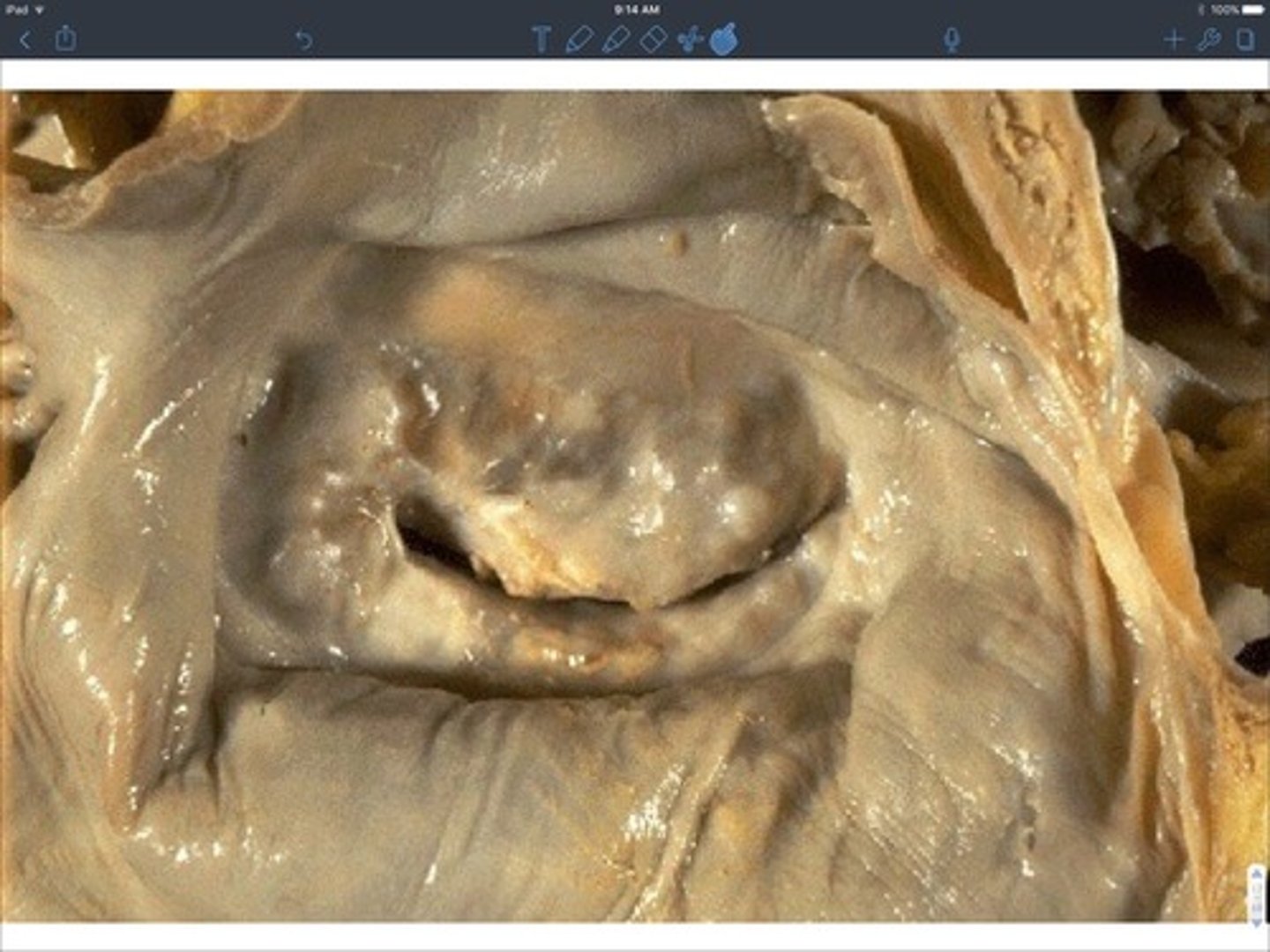
how does rheumatic valve disease occur?
immune cross reactivity due to molecular mimicry causing left side valve damage (mitral) and potential valve fusion
who is most likely to get rheumatic valve disease?
5-15 + untreated strep throat
why would someone get rheumatic valve disease?
untreated group A beta hemolytic strep
symptoms of rheumatic valve disease
fever, carditis (children), migratory polyarthritis (adults), Sydenham's chorea, skin rash
skin rash associated with rheumatic fever
erythema marginatum
