NURS 2001 Reading Guides 1-6 Exam 1
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
138 Terms
wellness
an integrated method of functioning oriented toward maximizing the potential of the individual
illness
separate short or long events that may challenge a person’s desire for health
when the person who moves toward illness and premature death develops signs and symptoms of disease or disabilities
When does treatment occur?
a systematic problem-solving approach to identifying and treating human responses to actual or potential health difficulties, serves as a framework for providing individualized care not only to individuals but also to families and communities
What is the nursing process?
assessment, diagnosis, outcome, planning, implementation, and evaluation
What are the 6 steps of the nursing process?
subjective data
based on patient experiences and perceptions
objective data
measurable, observe patients general appearance; assess vital signs; listen to heart, lungs, and abdomen; and assess peripheral circulation
is driven by patient, family, and community needs
is based on the nursing process, evidence-based thinking, and the scientific method
requires specific knowledge, skills, and experience
is guided by professional standards and codes of ethics
nurses are required ti contemplate analysis, develop alternatives and implement the best interventions
critical thinking is essential to resolving difficulties
How do nurses use critical thinking as part of the nursing process?
based on critical thinking, includes gathering and clustering data to draw inferences and propose diagnoses or hypotheses
What is diagnostic reasoning in nursing?
the nurse forms hypotheses, prioritizes them, generates solutions, and then takes actions.
the goal of this process is to direct you in implementing it in a way that will improve your patient’s care
What is the clinical judgement model?
emergency and urgent assessment
involves a life-threatening or unstable situation, such as a patient who has experienced a critical traumatic injury
use ABCDE to determine level of urgency
A (airway), B (breathing), C (circulation), D (disability), E (exposure)
comprehensive assessment
a complete health history and physical assessment
ex. physical similar to the one required for admission to school
focused assessment
based on patient’s health issues
ex. patient who preesnts to the clinic w/ a cough. health history focuses on duration of cough, associated symptoms such as wheezing or shortness of breath
life threatening issues always take priority
nurses prioritize on different ways
the ability to make decisions about the rank order in which nursing actions should be taken using nursing judgement
What does “priority setting” mean?
nonmaleficence (do no harm)
beneficence (promote good of client)
autonomy (clients right to make decisions)
confidentiality (respect right of client to maintain privacy)
justice (treat everyone fairly regardless of their ability to pay for treatment
What 5 ethical principles are nurses to use w/ in their nursing practice?
physical privacy
needed to make the client feel secure, don’t expose any more of the body than required at the time so client doesn’t feel vulnerable. curtain should be pulled, drape client w/ blankets, etc.
personal
maintain confidentiality and ensure client has been identified properly
if the nurse observes suspected abuse, they are required, by law, to report it
what is mandated reporting?
examples of therapeutic communication
ask openended questions, engage in active listening, staying away from medical terms, give positive reinforcement and reassurance w/ out passing judgement or disapproval
examples of non-therapeutic communication
giving personal opinions, giving approval and disapproval, using plural pronouns like “we”, giving false reassurances
Identify (state the team member’s name and title)
Situation (provide the circumstances that have required the communication to occur)
Background (provide the background data regarding the client assist the provider with familiarity)
Assessment (provide the most recent set of vital signs or other data relevant to the communication)
Recommendations (provide any suggestions that may be helpful to the situation)
Read back orders (repeat the orders that are given and clarify anything that is unclear)
What is ISBARR?
Inspection
Auscultation
Palpation
Percussion
What are the 4 techniques nurses use when assessing patients and what order are they performed in?
good light source, pen light, tape measure, pulse oximeter, tongue depressor
What tools are need for Inspection technique when assessing patients?
stethoscope and doppler
What tools are need for Auscultation technique when assessing patients?
no special tools but nurse should wear gloves
What tools are need for Palpation technique when assessing patients?
performed by advanced provider
need hands
What tools are need for Percussion technique when assessing patients?
electronic record
electronic communication tools for documenting progress, treatments, interventions, and client responses to care
physical record
when used, be sure to maintain integrity, properly date and time each entry followed by a full signature and title act the end. if error is made, draw single line through the entry and initial it
the client
Who has the right to see a patient record?
the client’s name, address, and phone number against the client’s medical record
the client’s age and date of birth
ask if the client has any illness or medical disability that could affect activities of daily living or social interactions
their contact person (an immediate family member, partner, or friend)
What is included on biographic data?
focusing on an ill or injured client’s reason for seeking medical care
What is a “chief complaint” or “presenting problem?”
document in chronological order the appearance of the manifestations connected with the reason for seeking care
begin w/ first event and continue until the present time
for each reported symptom, not the location, character of the symptom, severity of its appearance, its timing, and the setting it became noticeable
record the client’s answer to a question about their perception of the meaning of the illness injury
How should the history of present illness (HPI) be recorded?
after collecting data about the client’s biographic data, recognize if any of the social determinants (financial stability, education, social and communicty aspects, access to health care and neighborhood and environment) are active factors in their health status
if any of these factors play a role in the client’s health, follow that topic of conversation
How are social determinants of health used in the Health History?
childhood illness, injuries, chronic illness, hospitalizations, surgeries, immunizations, health maintenance examinations and screenings, allergies, current medications (medication reconciliation), and nutrition
What general topics are included in Health history?
general; specific
When taking a health history start with ______ questions, and then funnel down to more _______ questions.
do you have a family history of thyroid or diabetes?
to evaluate the client’s overall health and identify any unexpected manifestations
What is the purpose of Review of Systems? (ROS)
will help the rest of the interview go more smoothly
how can obtaining a thorough ROS help navigate your physical assessment?
if a client indicates manifestations in a specific body system are present or if they report painful symptoms, addressing that symptom becomes your priority
In what manner should a review of systems be conducted?
musculoskeletal, neurologic, hematologic, and endocrine
What are the 4 whole body systems that should be included in the ROS?
determines the client’s ability to care for themselves when they are not experiencing an acute illness
what is the purpose of a functional assessment?
self concept
healthy literacy
stress
activity and exercise
sleep
spirituality
substance abuse
What are the internal factors of a functional assessment?
occupational health
living environment
relationships
abuse
What are the external factors of a functional assessment?
alcohol use
do you ever drink alcohol in the morning?
have you ever felt guilty about drinking alcohol?
Tobacco/nicotine use:
do you vase?
do you or have you ever smoked or chewed tobacco?
Recreational Drug Use:
What type of substances have you consumed?
How often do you consume these substances?
Which substance abuse products would you ask about during a functional assessment?
be committed to preventing and managing their pain
share pertinent info w/ them about pain and pain relief
respect their reports of pain and respond appropriately to them'
consult w/ the appropriate pain management experts as needed
What are the responsibilities of the healthcare team when it comes to managing client pain?
ask for pain relief sooner rather than later
work w/ the healthcare team to develop a pain management plan
help the health care team evaluate their plan and the effectiveness of pain-relief interventions
share any info or concerns they might have about taking pain meds
What are the client responsibilities regarding pain management?
always believe the client
the client is entitle to adequate pain relief
pain is an urgent situation
base interventions on the client’s pain relief goals
use analgesics as prescribed
work w/ other health care team members
evaluate the effectiveness of interventions
prevent or minimize side and adverse effects of analgesia
educate the client and family about pain and pain management
The basic essentials for guiding pain management are:
relaxation
progressive muscle relaxation
distraction
cutaneous stimulation
thermal therapies
massge
transcutaneous electrical nerve stimulation
acupressure
guided imagery
hypnosis
biofeedback
music therapy
exercise
controlling the environment
other therapies
complementary therapies
What are some non pharmacological approaches to pain management?
complementary
used in addition to conventional treatment
alternative
used instead of conventional treatment
no later than 1 hour afterward
once the nurse has implemented an intervention for pain relief, when should the patient’s pain be reassessed?
nonopiods, opioids, and adjuvants
What 3 categories of meds are used to treat pain?
nonopiods
pain relieving medications that do not contain what has traditionally been called a narcotic component ex. aspirin, acetaminophen, NSAIDS
opioids
potent pharmacological analgesics once referred to as narcotics
adjuvants
medications that are primarily used to treat something other than pain, but that improve pain relief when used in combination w/ a pain medication
when it reaches a mild level
At what level should the patient notify you of pain?
Past medical history to include previous illnesses, and state of health
Last oral intake of liquids and food
Events leading to illness or injury
Allergies and type of reactions
Symptoms or chief complaint
Each prescribed medication, OTC medications, and herbal supplements
wHat is the PLEASE acronym?
C - have you ever felt the need to cut down on alcohol consumption?
A - Have you ever been annoyed at criticism regarding drinking?
G - Have you ever had guilty feelings related to drinking?
E - Have you ever taken a morning eye-opener?
What does the CAGE questionnaire stand for, for drinking?
pain
What is the 5 th vital sign?
acute pain
lasts 1 second up to 6 months, rapid in onset, varies intensity and duration, protective in nature
chronic pain
3 to 6 months, may be limited, intermittent, or persistent, lasts beyond the normal healing period, periods of remission or exacerbation are common
breakthrough
unpredictable episode of severe pain not controlled by current pain interventions
Legal obligation
pain management is standard care. not adhering to standards of care is a negligent act = malpractice
moral obligation
every patient has the right to pain management
clinical judgement model
represents the process of making clinical judgements
they incorporate critical thinking, clinical reasoning, and clinical judgement in order for nurses to make sound clinical decisions
What is the relationship b/t the nursing process and the clinical judgement model?
assigning a nursing activity or procedure to another person who has the training appropriate for that activity or procedure
What is delegation?
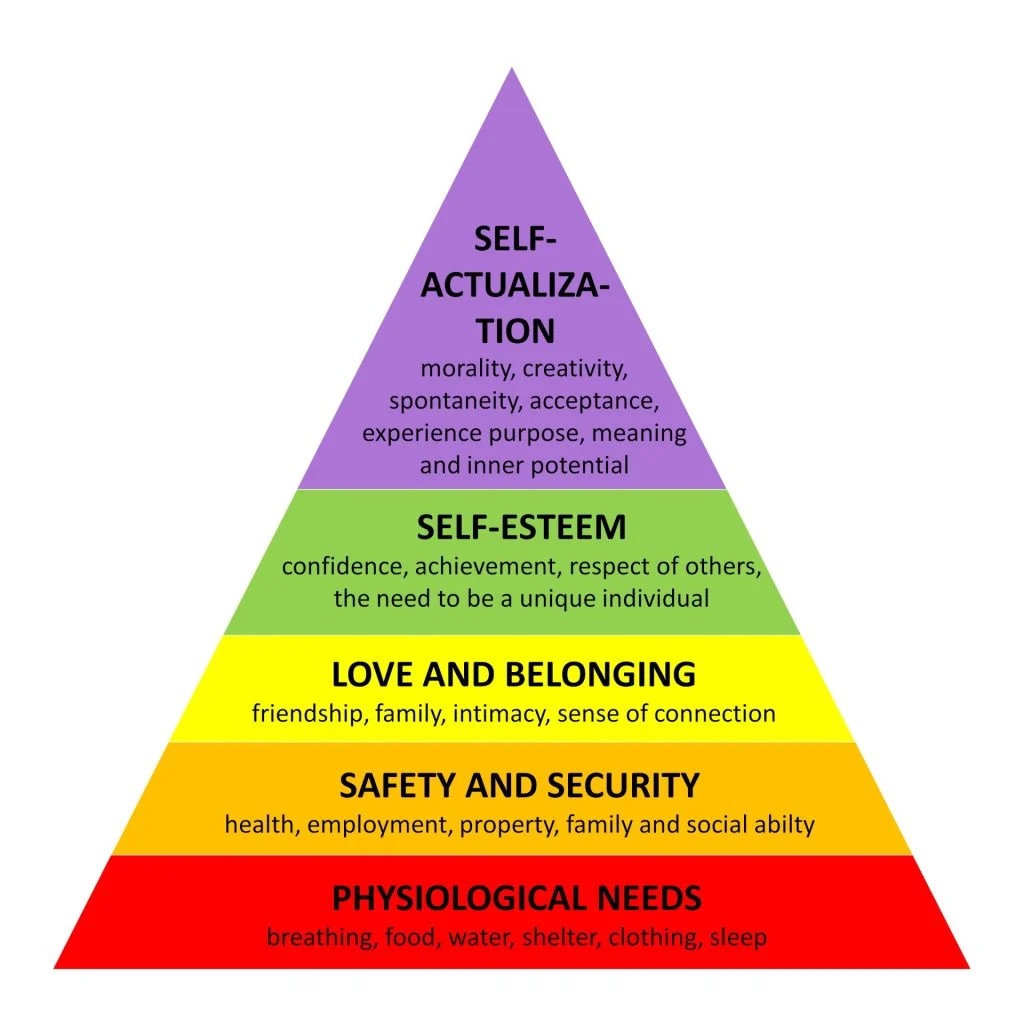
a theory that suggests there are five categories of needs that motivate human beings. the five categories are psychological, safety, love and belonging, esteem, and self-actualization
what is Maslow’s hierarchy of needs?
a systematic method that can be utilized in any health care setting to evaluate and treat the client. ABCDE is the acronym for airway, breathing, circulation, disability, exposure
What is the ABCDE approach?
priority is given to whatever finding poses the greatest or immediate risk to the client’s physical or psychological well-being
ex. if a nurse sees a wet area on the floor, the nurse or designee should dry the floor immediately to prevent clients from slipping and injuring themselves.
Explain the safety and risk reduction framework
interventions are selected that maintain client saefty while producing the least amount of restriction to the client; the nurse chooses interventions that are the least invasive
What is the least restrictive/least invasive priority setting framework?
priority is given to the client who has a reasonable chance of survival w/ immediate intervention. this framework is typically used in situations where resources are limited, such as with mass casualties and disaster triage
When would you use the survival potential and what are the categories w/ in it?
acute vs. chronic framework
a framework in which acute conditions are prioritized over chronic conditions
urgent vs. nonurgent framework
priority is given to the client who has urgent need over a client with a nonurgent need
Unstable vs stable framework
priority is given to the client who has an unstable condition versus the client with a stable condition
a sequence of factors needed for an infection to occur
how bacteria, viruses, fungi, parasites, and and prions move from place to place. these are contact, droplet, and airborne
What is the chain of infection?
infectious agent
something that contains bacteria, fungi, virus, parasite, prion
ex. Clostridium difficile, staphylococcus aureus, flora from GI tract
reservoir
the habitat of the infectious agent, a location where it can live, grow, and reproduce itself or replicate
ex. table, bed
portal of entry
any body orifice—for example, ears, nose, mouth, mouth, or skin—that provides a place for an infectious agent to replicate or for a toxin to act
mode of transmission
how bacteria, viruses, fungi, parasites, and prions move from place to place. these are contact, droplet, and airborne
susceptible host
required for the infectious agent to take hold and become a reservoir for infection
client w/ suppressed immune system
portal of exit
the route by which an infectious pathogen can leave the reservoir
wound drainage, GI tract
age
underlying disease HIV/AIDS
malignancy
transplants
medications: immunosuppressants, anti rejection medication, antineoplastics, antimicrobials, corticosteroids, gastric suppressants
surgical procedures
radiation therapy
indwelling devices: endotracheal tubes, urinary catheters, central venous catheters, arterial catheters, and implants such as pacemakers and artificial joints
What factors increase infection susceptibility?
infection prevention practices and these apply to all clients, whether or not they are known to have an infectious agent
What are standard precautions?
direct contact transmission
occurs when micro-organisms are directly moved from an infected person to another person, rather than through a contaminated object or person
indirect contact transmission
occurs when microorganisms are directly moved from the infected person to another person with having a contaminated object or person b/t these two
droplet transmission
occurs when droplets from the respiratory tract of a client travel through the air and into the mucosa of a host
airborne transmission
when small particles move into the airspace of another person
vehicle transmission
transmission of infectious agents to various individuals through a common source, such as contaminated food or water
vector-borne transmission
transmission of infectious agents through animals, such as insect or rodent
during medical asepsis
When should isolation precautions be used?
wet hands with water, apply enough soap to cover all hand surfaces, rub hands palm to palm, right palm over dorsum w/ interlaced fingers and vice versa, palm to palm with fingers interlaced, backs of fingers to opposing palms with fingers interlocked, rotational rubbing of thumb clasped in palm and vice versa, rotational rubbing, backwards and forwards with clasped fingers of hand in palm and vice versa, rinse hands with water, dry thoroughly with a single use towel, use towel to turn off faucet, and your hands are safe
How is hand hygiene properly performed?
when hands are not visibly soiled
When would you use hand sanitizer over soap and water?
Meant to protect the health care worker from contamination, blood, or body fluids. this equipment may include masks, eye protection, gown, gloves, and hair caps. equipment that should be put on (donned) prior to client interactions to prevent the spread of infectious organisms; can include gloves, gowns, masks, eye and face protection, and show covers.
What is the role of PPE?
natural defense of the body when injured, when foreign substances are present or when infectious agents attack.
in simple terms, explain the inflammatory response?
redness, swelling, heat, pain, loss of function
What are the signs and symptoms of inflammation?
infections that are acquired in a health care facility
What are healthcare associated infections?
bacteria that are resistant to one or more classes of existing antimicrobials
What are multidrug-resistant organisms (MRDOs)?
proper hand washing, wearing gloves, and using contact precautions
how can nurses prevent the spread of multi drug-resistant organisms?
interventions to eliminate or decrease the presence of micro-organisms that can cause infection.
What are the principles of aseptic technique