B3.1: Gas Exchange
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Respiratory System
provides O2 to body tissues, removes CO2, main organs are lungs
Gas Exchange
exchange of O2/CO2 btwn lungs (alveoli) and blood (capillaries)
Cell Respiration
production of ATP and CO2 w/ intake of O2 in mitochondria
Purpose of Gas Exchange
interchange of materials required for metabolism (O2/CO2)
-oxygen is required for aerobic respiration, to produce lots of ATP
-CO2, a waste product of aerobic respiration, needs to be removed from organism
Need for Ventilation System
in animals, O2/CO2 transported through blood
-gas exchange occurs in specialized ventilation organs (lungs/gills)
as organism becomes larger, distance from its center to exterior increases and their SA:V decreases
-therefore ventilation system becomes necessary to ensure efficient gas exchange and adequate gas supply to tissues
Gas Exchange Systems
distinct systems for gas exchange have evolved in different organisms depending on their environment and size
Small, Multicellular Organisms
diffusion across the surface is sufficient for organisms like flatworms (breathe through skin)
Insects
have separate respiratory and circulatory systems, use tracheal systems that push gases throughout body
Aquatic Organisms
like fish, have gills (heavily folded) to extract the dissolved oxygen from water
Mammals
have lungs, which are used to transfer gases from blood and atmosphere
Concentration Gradients
ventilation systems need to maintain [] gradient for gas exchange to occur
-[O2] is lower in cells bc it is constantly being consumed for aerobic respiration
-[CO2] is higher because it is being released as waste
Goal of Ventilation Systems
to provide fresh gases to cells from the atmosphere/water and remove waste products
-they are structured to have a very large SA, so that gas exchange can be maximized
-they are also connected to circulatory system via dense network of capillaries for continuous blood flow
so that [O2] can stay high and [CO2] can remain low in tissues
Lung Structure (5)
1. air enters through nose, goes from nose/mouth --> pharynx
2. then goes down the glottis to the trachea
3. trachea divides into two bronchi
4. Divides into many bronchioles
5. Bronchioles end w/ alveoli
Air in Nose
filtered, warmed, humidified
-travels to pharynx
Glottis
top of trachea
Trachea
ciliated and lined with mucus to trap/expel foreign matter
Bronchi
two short branches located at the lower end of the trachea that carry air into the lungs
Lobes of Lungs
right lung has 3 lobes, left as only two to allow room for heart
Bronchioles
lines w/ smooth muscles that regulate air flow
Alveoli
cluster of air sacs, site of gas exchange w/ blood
Alveolus Structure (5)
1. surrounded by epithelium (outermost layer of cells)
2. only one cell thick to increase diffusion
3. located near extensive capillary network to increase gas exchange w/ blood
4. spherical in shape to increase SA
5. internal surface has fluid (just outside alveoli, btwn it and capillaries) bc dissolved gases diffuse easier/faster
Properties of Ventilation Surfaces (4)
1. have large SA
2. retain moisture - easier for gases to diffuse across membranes in dissolved form (alveoli lined w/ water)
3. adequately permeable for absorption
4. lined by single layer epithelium to optimize efficiency
Inhalation/Exhalation
inhalation brings O2 rich air into alveoli
-O2 diffuses, alveoli --> capillaries (bc of concentration gradient)
-CO2 diffuses, capillaries --> alveoli
exhalation expels CO2 rich air out of alveoli
*more O2 in atmosphere than lungs, more O2 in lungs than blood, therefore diffusion occurs w/ concentration gradient (and vice versa for CO2)*
Type 1 Pneumocytes (Alveolar Cells)
responsible for gas exchange btwn alveolus and blood
-extremely thin to reduce diffusion distance
-connected by occluding junctions, prevents leakage
-mature cells are amitotic, does not divide
Occluding Junctions
very tight junction, nothing gets through
Type II Pneumocytes (Alveolar Cells)
responsible for secretion of pulmonary surfactant
-cuboidal in shape
-contains many secretory vesicle that discharge surfactant components
*alveolar epithelium is an example of a tissue where more than one cell type is present, bc different adaptation are required for overall function*
Pulmonary Surfactant
liquid that lines alveoli to allow easier gas exchange
-same liquid create surface tension (propensity for cohesion) which would cause alveoli to collapse during exhalation and resist inflation
however the surfactant reduces this surface tension
-creates a barrier btwn liquid and air, made during 28th week of pregnancy
Ventilation
Process of moving air in and out of lungs for gas exchange
-breathing, or contraction of respiratory muscles, changes volume of thoracic cavity
-change in volume creates a pressure differential btwn chest and atmosphere during which air moves towards equilibrium
Lungs
located in thoracic cavity or thorax
-walls are formed by ribs and sternum
-attached to external and internal intercostal muscles
-floor is formed by diaphragm
Ventilation Process
internal and external intercostal muscles, as well as diaphragm and abdominal muscles are antagonistic muscles
-during inspiration, external intercostal muscles and diaphragm contract
-during expiration, internal intercostal muscles and abdominal muscles contract
Inspiration
external intercostal muscles contract, lifting ribs and sternum
-diaphragm contracts, flattening the floor
volume of thoracic cavity increases, increase volume of lungs and decreases pressure
-negative pressure draws air from atmosphere into lungs
Expiration
Internal intercostal muscles contract, lowering ribs and sternum
-abdominal muscles contract, relax diaphragm, raising the floor
volume of thoracic cavity decreases, decreases volume of lungs and increases pressure
-air flows out of lungs into atmosphere
Feedback Control of Ventilation
[CO2] in blood has a greater impact than [O2]
CO2 from cells (released during respiration) diffuses into interstitial fluid (liquid btwn cells), then plasma (liquid of blood), then RBCs
CO2 reacts w/ H2O to form H2CO3 (carbonic acid) which becomes bicarbonate (HCO3-) and H+, which is acidic and lower pH
-hemoglobin binds most of CO2 to stabilize pH
basically increase CO2 leads to decrease pH (more acidic), which increase ventilation
Respiratory Acidosis
occurs when CO2 accumulates and pH drops, requiring faster breathing to remove excess CO2
Chemoreceptors
Specialized sensory receptors that detect chemical changes in blood (O2, CO2, pH)
-either peripheral or central
Peripheral Chemoreceptors
in carotid bodies and aortic bodies, basically detect pH of blood
Carotid Bodies
cluster of chemoreceptors found in arteries
Central Chemoreceptors
in medulla oblongata, primarily detect changes in CO2 and pH of cerebrospinal fluid
Medullary Respiratory Centers
consist of medulla oblongata and pons
-medulla sets the basic rhythm for breathing
-pons fine-tunes breathing rate and depth
Negative Feedback (6)
1. increase in CO2 or decrease in pH
2. chemoreceptors detect changes
3. signals are sent to medulla oblongata
4. increase impulses (decrease when CO2 is low) via phrenic nerve to diaphragm and intercostal muscles
5. increase breathing rate and depth to remove CO2 (opposite occurs when CO2 is low)
6. CO2 levels drop, pH returns to normal
Lung Capacity
volumes of air associated w/ different respiratory phases
Total Lung Capacity
volume of lungs after maximum inhalation (about 6L)
Tidal Volume
volume of air exchanged during normal breathing (about 500mL/breath)
Vital Capacity
volume of air exchanged during maximum inhalation and exhalation (about 4L)
Inspiratory Reserves
volume of air inspired w/ max effort after a normal inhalation
Expiratory Reserves
volume of air expired w/ max effort after a normal exhalation
As Physical Activity Increases...
so does O2 consumption and CO2 production due to increased cell respiration
-once increased CO2 detected in blood, brain increases ventilation
increase ventilation = more breaths
increase tidal volume = greater volume per breath
-both increase the intake of O2 which allows undisrupted gas exchange as needed by body
Ways to Measure Ventilation (4)
1. Observation - Counting number of breaths
2. chest belt attached to pressure meter, recording rise and fall of chest
3. Spirometer
4. Balloon (simple alternative)
Spirometer
measures volume and speed of breaths, presents data on digital display
Balloon
used to measure a single breath, air released underwater to measure volume displaced
Hemoglobin (Hb)
globular protein in RBC, responsible for O2/CO2 transport
-consists of 4 polypeptide chains each w/ a heme prosthetic group that contains and iron ion (Fe2+)
-each Fe2+ binds to an O2 molecule, for a total of 4
Oxygen Dissociation Curve
sigmoidal graph that depicts the relationship btwn [O2] (referred to as partial pressure, pO2) and hemoglobin saturation
slightest change in pO2 causes hemoglobin to load/unload O2 in significantly different amounts due to cooperative bonding
Cooperative Bonding
phenomenon in which binding of one O2 increases Hb's affinity for O2 bc O2 binding causes a conformation change
Changes Hb from Tense (T) state (low O2 affinity) to Relaxed (R) state (high O2 affinity)
-ensures rapid O2 loading in lungs and efficient O2 unloading in tissues where O2 levels are lower
*such behavior creates sigmoidal shape on curve, displaying increasing O2 affinity as more O2 binds*
Tense State vs Relaxed State
each time O2 binds to Hb, Hb becomes more relaxed, making it easier for O2 to bind in lungs
but in tissues, Hb arrives relaxed (saturated) w/ O2, and as it unloads O2, it becomes tense, making it easier to unload O2
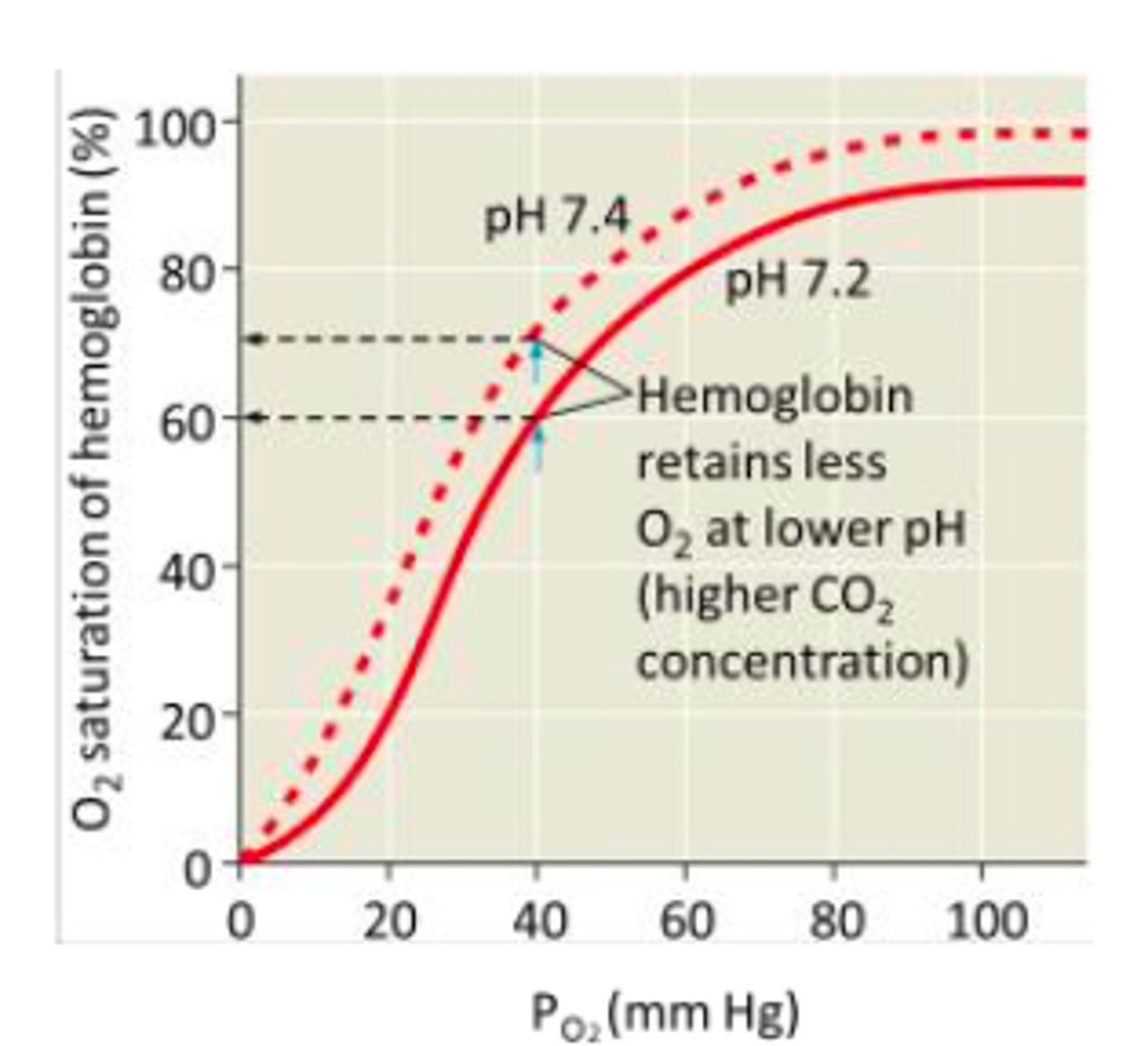
Bohr Shift
phenomenon in which increase [CO2] or decrease pH reduces Hb's affinity for O2, causing increased O2 dissociation
-oxygen dissociation curve shifts to the right, which means that at the same pO2, HB releases more O2 to tissues
Basically the increased H+ (from more CO2 making blood acidic) protonates Hb and causes a conformational change that promotes O2 release
-decreases Hb's affinity for O2 (in presence of CO2)
-enhances O2 delivery to tissues in high metabolic activity areas
Bohr Shift Diagram
Less saturated Hb at higher pO2 bc more CO2 = more acidic = higher metabolic activity so needs more O2 for respiration
-therefore O2 leaves Hb faster, allowing for more O2 for respiration
Allosteric Binding of CO2
CO2 binds at a different site from the O2-binding site which affects Hb's structure and function
when CO2 binds to amino groups in Hb, carbaminohemoglobin (HbCO2) forms
-this stabilizes the Tense (T) state and promotes O2 unloading bc T state decreases Hb's affinity for O2
*ensures that O2 is released where it is need most, as in actively respiring tissues that produce high levels of CO2*
Adult Hemoglobin (HbA)
optimized for O2 loading at lungs and efficient unloading at tissues
-composed of two alpha and two beta chains
has higher binding of 2,3-Bisphosphoglycerate (2,3-BPG) which reduces O2 affinity, promoting its unloading
-stabilizes Tense State
-shifts oxygen dissociation curve right, enables more efficient O2 unloading at active tissues, therefore unloads O2 at tissues w/ lower pO2
2,3-bisphosphoglycerate
Compound that lowers hemoglobin's affinity to oxygen, thereby freeing up oxygen for use by tissues
Fetal Hemoglobin (HbF)
optimized for O2 transfer across placenta, allowing fetus to obtain sufficient O2 from maternal blood
-composed of 2 alpha and 2 gamma chains, instead of beta
binds to O2 more tightly allowing O2 to be extracted from HbA (which comes from mother, basically allows O2 transfer from mom Hb to Fetal Hb)
-does not bind to 2,3-BPG which allows higher O2 affinity, shifting oxygen dissociation curve to the left
around 6 months old, HbF becomes HbA via gene expression on CHR 11