Ch6: Respiratory System
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
Thoracic cavity
Location of the lungs and heart
Nares
Entry point for air in the respiratory tract located in the nose
AKA nostrils
Vibrissae
AKA nasal hairs
Filters air within nasal cavity
Nasal cavity
Area just behind the nostrils
Removes dirt and particulate matter from the air by filtering with mucous membranes and vibrissae
Warms and humidifies air
Pharynx
Resides behind the nasal cavity and the back of the mouth
Common pathway for air and food
Larynx
Below the pharynx
Pathway for air only
Contains vocal cords
Glottis
Opening of the larynx
Epiglottis
A flap of cartilage that covers the glottis during swallowing so that food doesn't go into the trachea
Trachea
what is it
what does it contain
Below the larynx
the windpipe
Composed of about 20 rings of cartilage
Lined with ciliated epithelial cells
Bronchi
Trachea divides into these cartaliginous tubes
Lined with ciliated epithelial cells
Bronchioles
what is it
what does it contain
In the lungs
Bronchi divide into these
Not cartaliginous
Alveoli
Tiny balloon-like structures in the lungs
Site of gas exchange
Surfactant
Coats each alveolus to relieve surface tension and prevent alveolus from collapsing on itself
Bronchioles and alveoli (purpose)
Allow for exceptionally large surface area for gas exchange (100 meters squared)
Chest wall
Forms the outside of the thoracic cavity
Pleurae
Membranous sacs that surround each lung
Form closed sacs against which the lungs expand
Visceral pleura
Surface of pleura adjacent to the lung
visceral= closer to the lung
Parietal pleura
Surface of pleura that is far away from the lung
Diaphragm
what is it
what controls it
Thin, muscular structure that divides the thoracic cavity from the abdominal cavity
Under somatic control
Chest wall, back and neck muscles
May contribute to breathing, especially when breathing is labored
Intrapleural space
Space within the pleura
External intercostal muscles
where are they
what are they used for
how are they used
One of the layers of muscles between the ribs that plays a role in INHALATION
Contract to expand the thoracic cavity alongside the diaphragm which also contracts
Relax to contract the thoracic cavity
Where exactly:
They run from the lower edge of one rib to the upper edge of the rib below
Fibers run downward and forward (like putting your hands in your jacket pockets 🧥)
🫁 What they do:
Help pull the ribs upward and outward during inhalation (breathing in)
This expands the chest cavity, allowing air to enter the lungs
Let me know if you want a diagram!
Intrathoracic volume
Volume of the chest cavity
Inhalation
what is inhilation
what happens to the intrathoracic vlume
what happens to the pressure and volume of the intrapleural space
describe what happens next in the process of inhalation and what is the primary mechanism referred to as
-When air enters the lungs
-it increases
-it increases in volume but decreases in pressure
-The gas in the lungs is initially at atmospheric pressure, which is now higher than the pressure in the intrapleural space.
The lungs will therefore expand into the intrapleural space, and the pressure in the lungs will drop.
Air will then be sucked in from a higher-pressure environment—the outside world.
This mechanism is referred to as negative-pressure breathing because the driving force is the lower (relatively negative) pressure in the intrapleural space compared with the lungs.
Negative-pressure breathing
Driving force for inhalation is the negative pressure in the intrapleural space compared to the lungs. When the diaphragm contracts, increase in volume lowers pressure, so air goes from high to low pressure
Exhalation
what is it by definition
how does it differ from inhalation
how it operate
When air is pushed out of the lungs
Does not have to be an active process because muscles recoil
literally exact opposite process:
As the diaphragm and external intercostals relax, the chest cavity decreases in volume.
What will happen to pressure in the intrapleural space? It will go up, again explained by Boyle’s law.
Now pressure in the intrapleural space is higher than in the lungs, which is still at atmospheric pressure.
Thus, air will be pushed out, resulting in exhalation. During active tasks, we can speed this process up by using the internal intercostal muscles and abdominal muscles, which oppose the external intercostals and pull the rib cage down.
This actively decreases the volume of the thoracic cavity. Finally, recall that surfactant prevents the complete collapse of the alveoli during exhalation by reducing surface tension at the alveolar surface.
Internal intercostal muscles
Layer of muscles beneath the ribs
Oppose the external intercostals and pull the rib cage down
Decrease volume of thoracic cavity to help with exhalation
Abdominal muscles
Can help with exhalation if needed
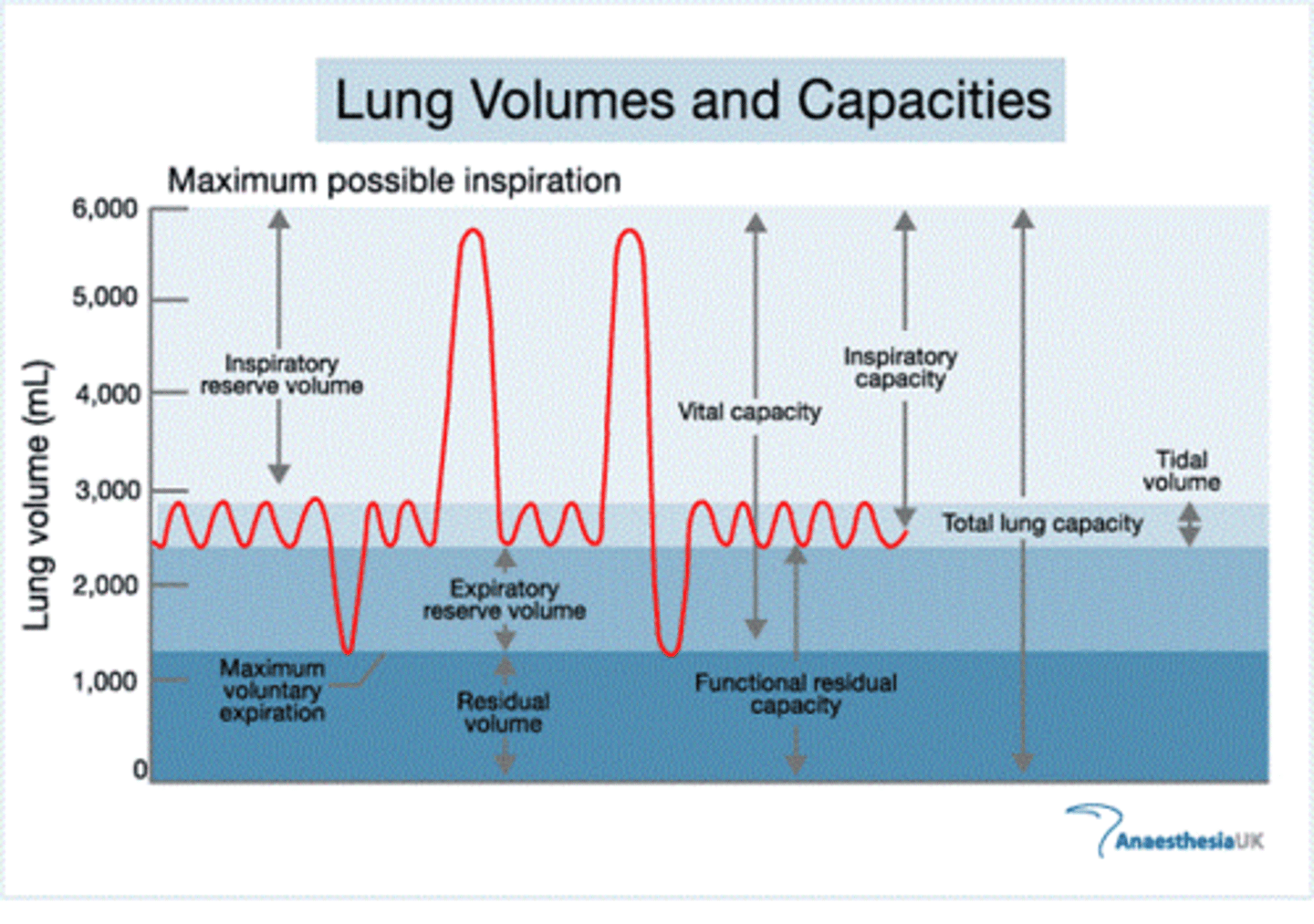
Spirometer
what does it do]
what are its limitations
Helps assess lung capacities and volumes
Cannot measure residual volume- amount of air remaining in the lungs are exhalation
Total lung capacity (TLC)
The maximum volume of air in the lungs when one inhales completely
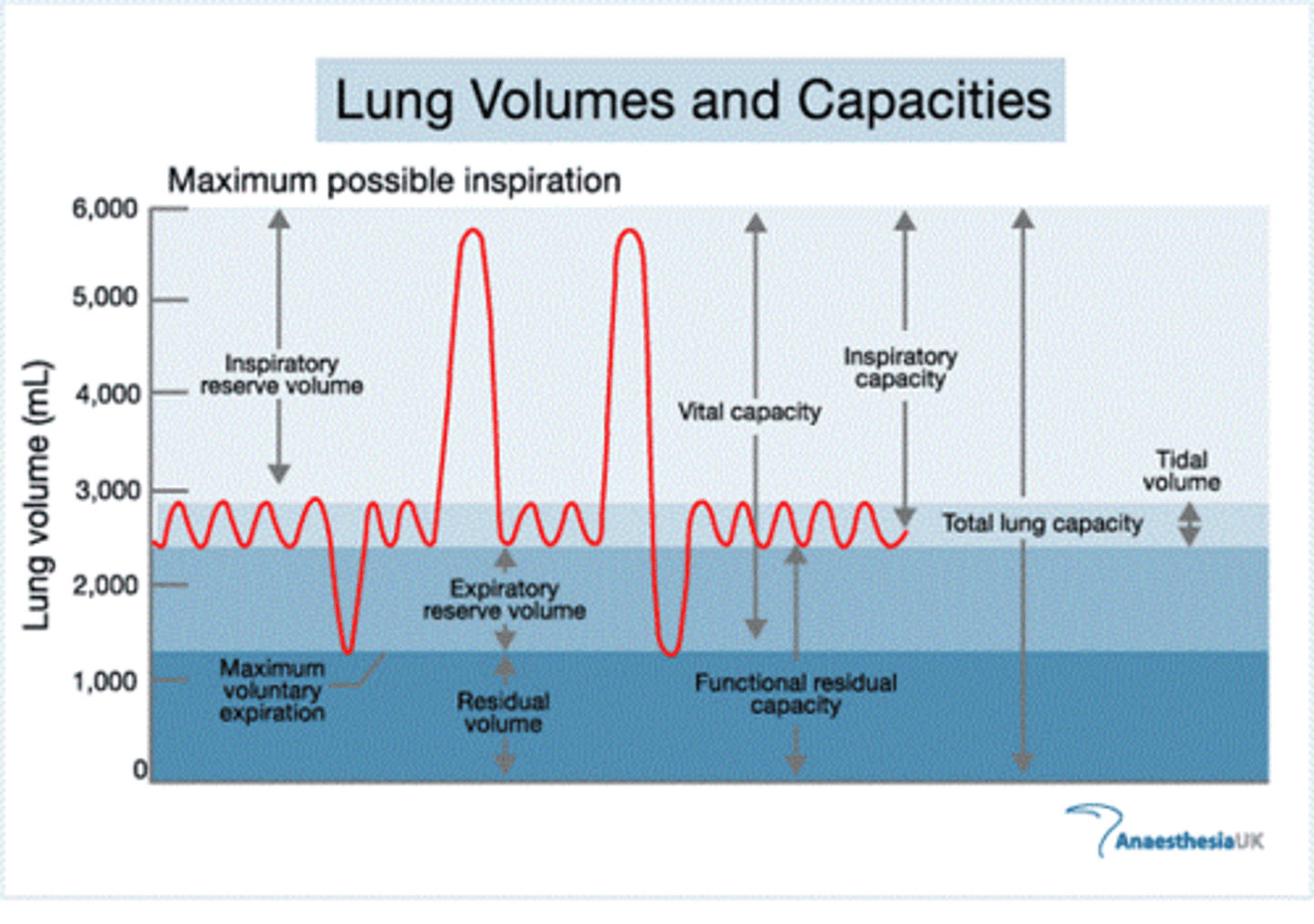
Residual volume (RV)
The minimum volume of air in the lungs when one exhales completely
Cannot be measured by a spirometer
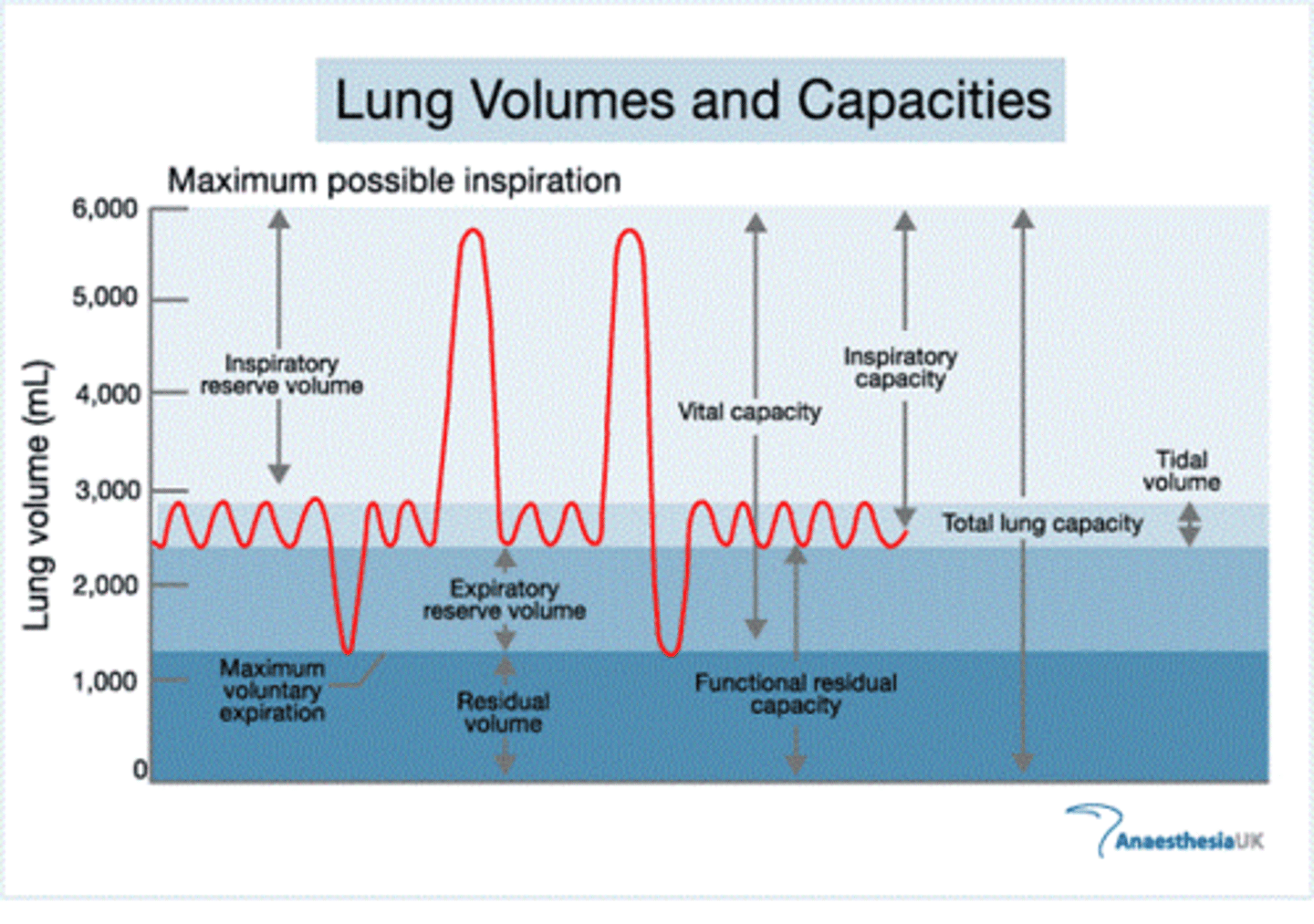
Vital capacity (VC) and equation
The difference between the minimum and maximum volume of air in the lungs
Total Lung Capacity - Residual Volume
(TLC - RV)
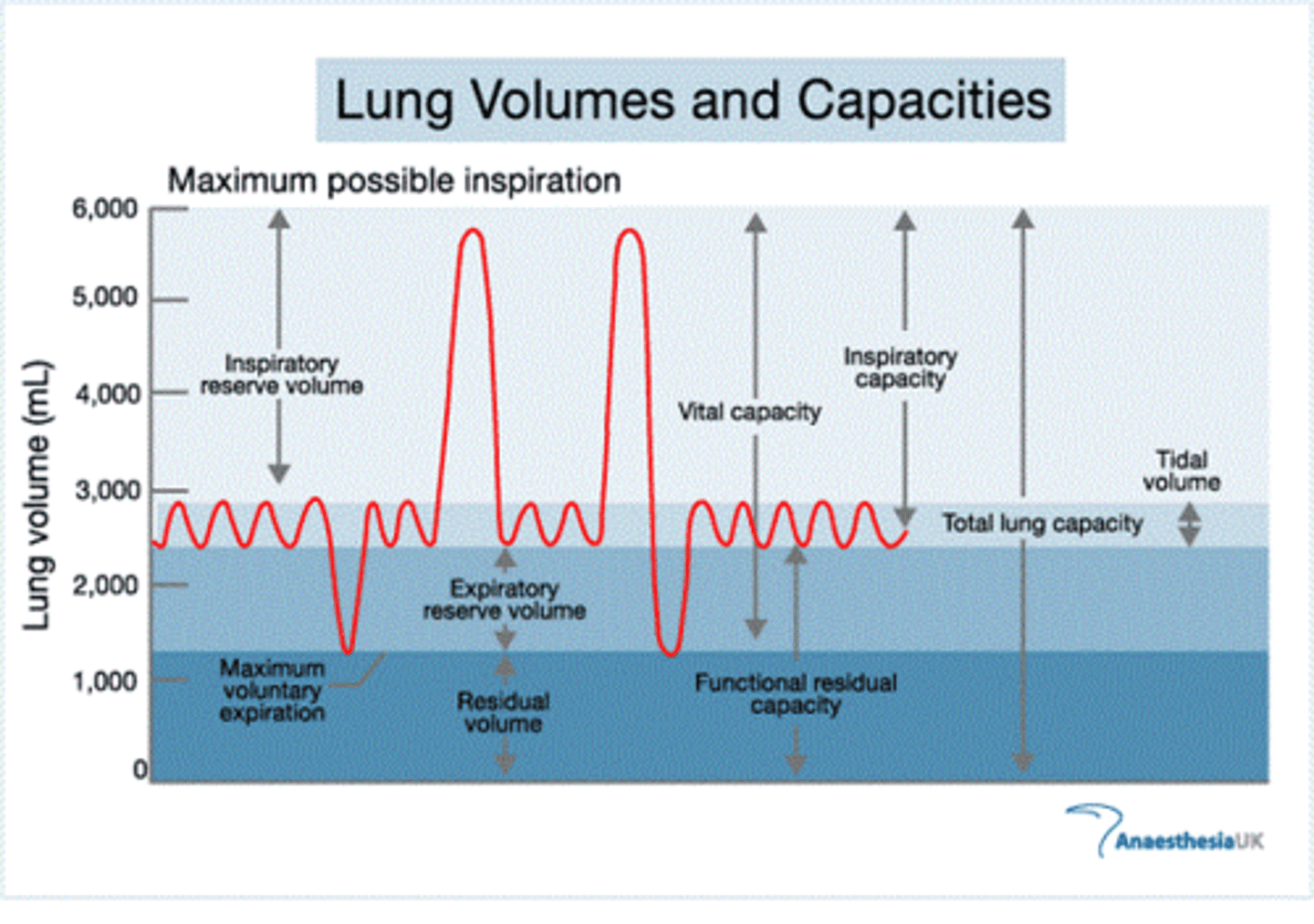
Tidal volume (TV)
The volume of air inhaled or exhaled in a normal breath
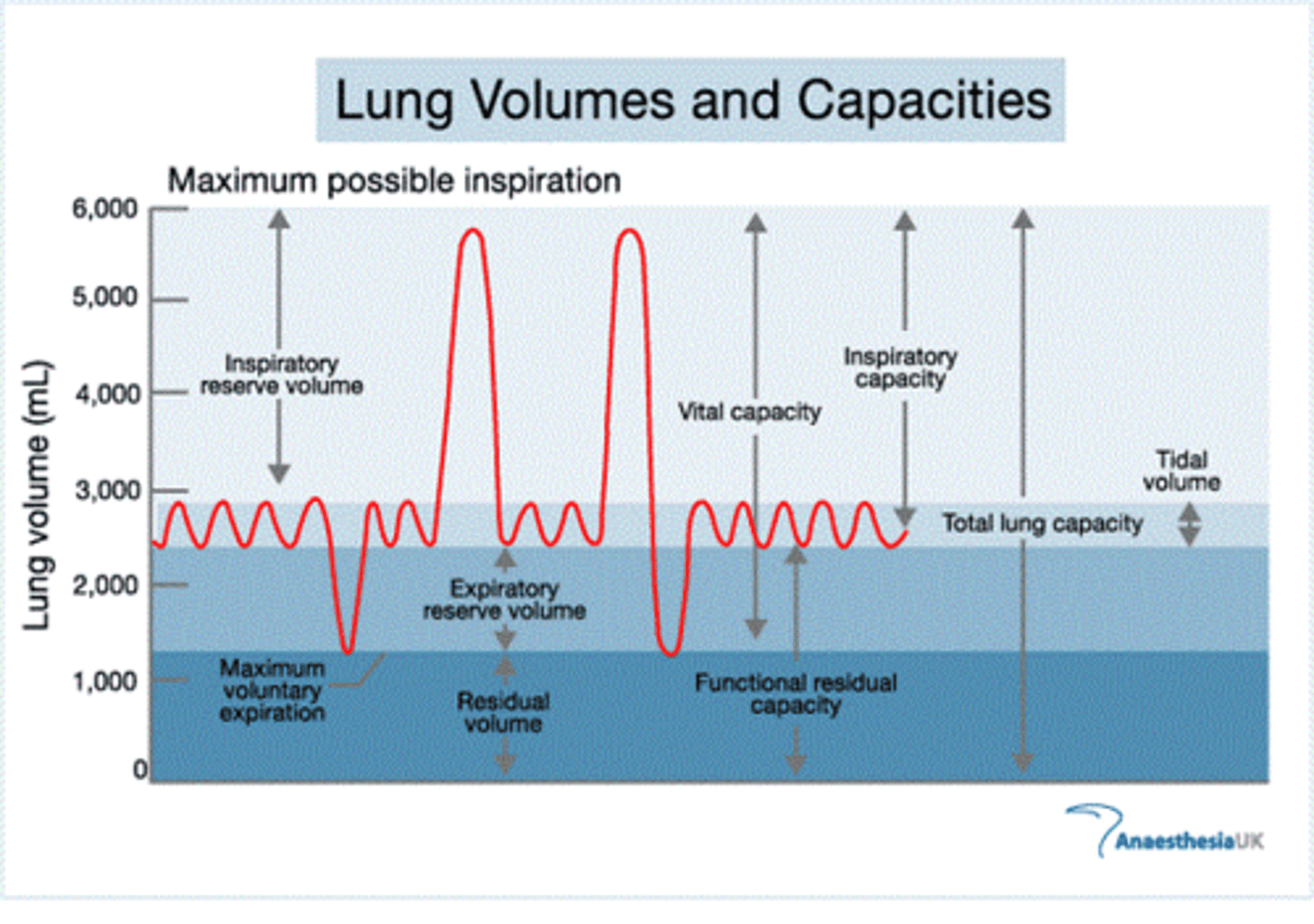
Expiratory reserve volume (ERV)
The volume of additional air that can be forcibly exhaled after a normal exhalation
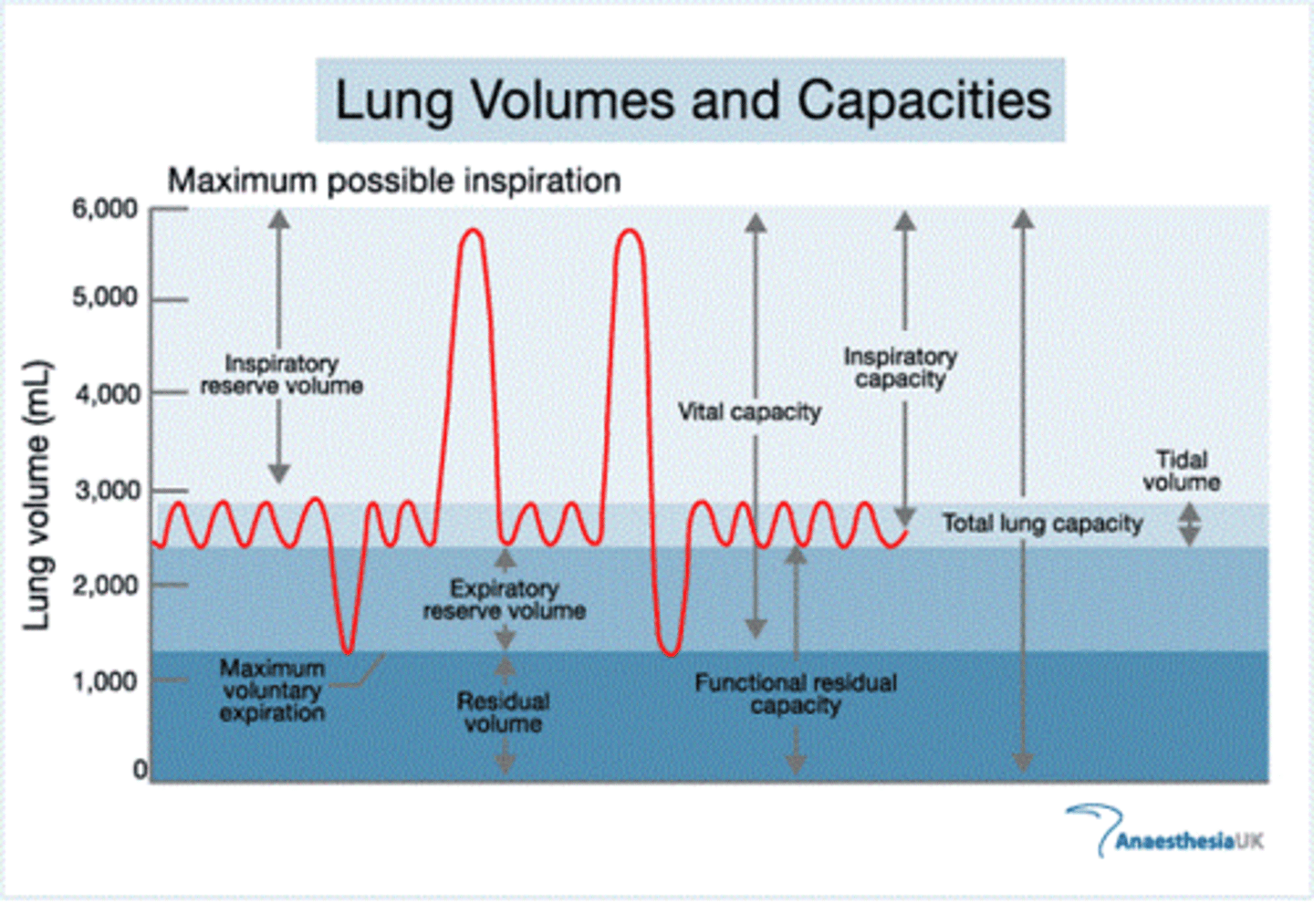
Inspiratory reserve volume (IRV)
The volume of additional air that can be forcibly inhaled after a normal inhalation
Medulla oblongata
what does it do
what structure does it contain
Structure in the hindbrain that regulates ventilation
Ventilation center
what is it/ what does it do
what structure is contained here
Collection of neurons in the medulla oblongata that fire rhythmically to cause regular contraction of respiratory muscles
chemoceptor
Chemoreceptors in ventilation center
Ventilation center neurons use these to detect carbon dioxide concentration and act accordingly
Hypercarbia or hypercapnia
what is it
what does it cause
Too much CO2 in the blood
Causes respiratory rate to increase so more CO2 will be exhaled
Respiratory rate
Rate at which one breathes
Hypoxia
Low oxygen concentration in the blood
Ventilation center neurons respond to this as well but only when oxygen is very low in the blood
Cerebrum
The structure through which we can control our breathing
Overridden by medulla oblongata when we breathe too little for a time
Hypoventilation
what is it
what does it cause in terms of concentration and pH
Too little breathing
Causes CO2 concentration in blood to increase, causing pH to go down
Hyperventilation
review bicarbonate buffer system and make a separate flashcard
Too much breathing
Causes CO2 concentration to decrease, making the bicarbonate buffer system shift to the left to compensate, causing alkalemia
Pulmonary arteries
alveloi are surrounded by capillaries
capillaries bring deoxygenated blood from the pulmonary arterier
the pulmonary arteries emerge from the right ventricle of the heart
Pulmonary veins
Bring newly oxygenated blood to the left atrium of the heart
Identify and describe the driving force for gas exchange in the aveoli
How would our respiratory systems adjust if we moved to higher altitudes where less oxygen is available?
The driving force for gas exchange is the pressure differential of the gases.
When it initially arrives at the alveoli, blood has a relatively low partial pressure of oxygen and a relatively high partial pressure of carbon dioxide, facilitating transfer of each down its respective concentration gradient.
O2 in the alveoli flows down its partial pressure gradient from the alveoli into the pulmonary capillaries, where it can bind to hemoglobin for transport. Meanwhile, CO2 flows down its partial pressure gradient from the capillaries into the alveoli for expiration. no energy needed for this gas transfer at the alveoli.
2.First, we would breathe more rapidly to try to avoid hypoxia; second, the binding dynamics of hemoglobin to oxygen would be altered to facilitate the unloading of oxygen at the tissues.
the natural response of hemoglobin to the decreased carbon dioxide concentration in the environment would actually be to decrease the unloading of oxygen to tissues, so other mechanisms can counteract and override this phenomenon to allow adequate delivery of oxygen.
In the short term, the body can make more red blood cells to ensure the adequate delivery of oxygen. In the long term, the body could develop more blood vessels (vascularization), which would facilitate the distribution of oxygen to tissues.
Thermoregulation
what is it
through what mechanisms does it occur
describe the mechanisms
other mechanisms of heat regulation
the regulation of body temperature
vasodilation and vasoconstriction
As capillaries expand, more blood can pass through these vessels, and a larger amount of thermal energy can be dissipated. As capillaries contract, less blood can pass through them, conserving thermal energy
While these capillary beds provide a mechanism for thermoregulation, humans predominantly regulate temperature using capillaries and sweat glands in the skin, or rapid muscle contraction (shivering). The respiratory system can also transfer heat to the environment through evaporation of water in mucous secretions. Other animals, such as dogs, take advantage of this cooling mechanism by panting.
Vasodilation
Expansion of capillaries in the nasal cavity and trachea to dissipate thermal energy
Vasoconstriction
Contraction of capillaries in the nasal cavity and trachea to conserve thermal energy
how does the respiratory system fight off pathogens
The nasal cavity also contains an enzyme called lysozyme. Also found in tears and saliva, lysozyme is able to attack the peptidoglycan walls of gram-positive bacteria.
The internal airways are lined with mucus, which traps particulate matter and larger invaders. Underlying cilia then propel the mucus up the respiratory tract to the oral cavity, where it can be expelled or swallowed; this mechanism is called the mucociliary escalator.
Macrophages can engulf and digest pathogens and signal to the rest of the immune system that there is an invader. Mucosal surfaces also contain IgA antibodies that help to protect against pathogens that contact the mucous membranes.
Finally, mast cells also populate the lungs. These cells have preformed antibodies on their surfaces. When the right substance attaches to the antibody, the mast cell releases inflammatory chemicals into the surrounding area to promote an immune response. Unfortunately, these antibodies are often reactive to substances such as pollen and molds, so mast cells also provide the inflammatory chemicals that mediate allergic reactions.
Mucociliary escalator
Internal airways are lined with mucus which traps particulate matter and larger invaders
Underlying cilia propel the mucus up the respiratory tract to the oral cavity, where it is expelled or swallowed
Macrophages
Seen in the lungs, especially alvoeli. Engulf and digest pathogens and signal to the rest of the immune system that there is an invader
IgA antibodies
Contained on mucosal surfaces
Help protect against pathogens that contact mucous membranes
Mast cells
can also be seen in lungs. Release inflammatory chemicals to promote an immune response upon contact with an antigen
Can Cause allergic reactions
what does the bicarbonate buffer system do
what is the equation
plays a role in pH balance in blood -
CO2 (g) + H2O (l) <-> H2CO3 (aq) <-> HCO3- (aq) + H+ (aq)
Physiological pH
7.35-7.45
what happens when ph is too low
pH of blood is too low and H+ concentration is high- acidemia
acid-sensing chemoreceptors just outside the blood-brain barrier send signals to the brain to increase the respiratory rate.
Further, an increasing hydrogen ion concentration will cause a shift in the bicarbonate buffer system, generating additional carbon dioxide.
Just because the reaction is going rightward doesn’t mean CO₂ is being “burned off.” It means there's a lot of CO₂ available — and it's driving the reaction to the right, producing more H⁺.
So:
If CO₂ levels are high, the equation shifts right → more H⁺ → lower pH (acidosis).
The body sees the end result: high H⁺ (low pH).
It assumes the cause is high CO₂ (and often it is — like in hypoventilation).
So it increases respiration to remove CO₂, which shifts the equation left and consumes H⁺, raising the pH.
Effects of acidemia
CO2 concentration increases due to excess of H+
Ventilation center senses this and increases respiratory rate to blow off more CO2
Decreased CO2 pushes bicarbonate buffer equation to left until H+ concentration is normal again
As the respiratory rate increases, more carbon dioxide is blown off. This will also push the buffer equation to the left, but notice the difference: the shift to the left in the previous paragraph was caused by an increase in hydrogen ion concentration, which elevated the concentration of carbon dioxide. Here, the removal of carbon dioxide causes a shift to the left that allows the hydrogen ion concentration to drop back to normal.
what happens when pH is too high
pH of blood is too high- alkalemia
then the body will seek to increase acidity.
If the respiratory rate is slowed, then more carbon dioxide will be retained, shifting the buffer equation to the right and producing more hydrogen ions and bicarbonate ions. This results in a lower pH.
Condition | Blood pH | H⁺ Levels | Effect on Respiratory Rate | Why? |
|---|---|---|---|---|
Acidemia | ↓ pH (< 7.35) | ↑ H⁺ (too acidic) | ↑ Increased (hyperventilation) | To blow off CO₂, shift buffer left, and lower H⁺ |
Alkalemia | ↑ pH (> 7.45) | ↓ H⁺ (too basic) | ↓ Decreased (hypoventilation) | To retain CO₂, shift buffer right, and raise H⁺ |
Effects of alkalemia
Respiratory rate is slowed to increase CO2 concentration and shift bicarbonate buffer equation to right to decrease pH
If H+ is an acid and HCO⁻3 is a base, then why doesn't increasing both of them maintain a constant pH?
The reason is because H+ is a strong acid, while HCO⁻3 is a weak base. (buffer system!)
Difference between lung response and kidney response to pH imbalances
Lung response is faster
Kidney response is slower, more long-term