L16 - small animal ectoparasites
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Canine Demodicosis
• Hosts: dog;
• Location: hair follicles, sebaceous glands, corneum layer of the skin;
• Significance for human health: none.
• Demodex canis: locates in hair follicles & sebaceous glands;
• Demodex injai: longer body, locates in the hair follicles and sebaceous glands and is generally associated with greasy/oily skin and coat;

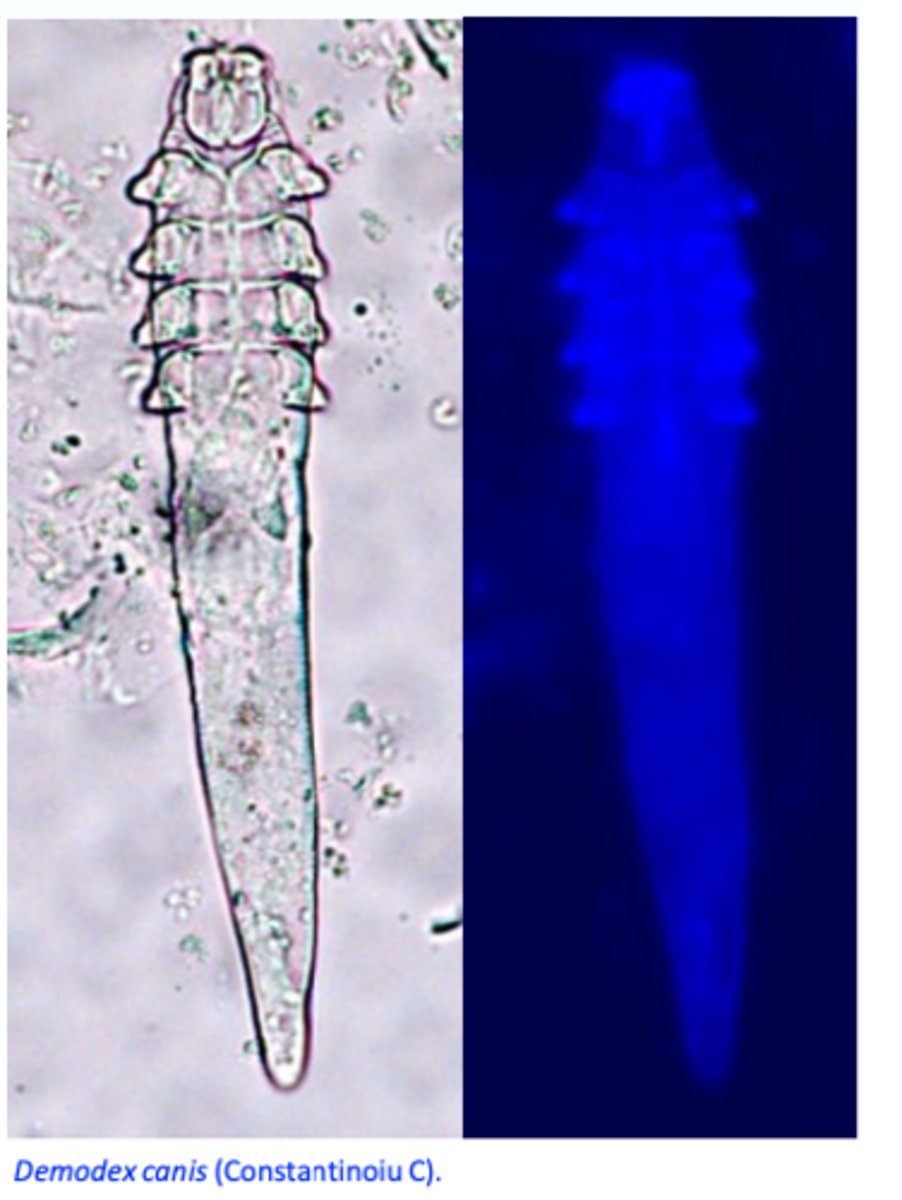
Demodex canis
Morphology: adult stage
Body: elongated;
Four short, stumpy pairs of legs, located at the front of the body;
Opistosoma is striated;
Demodex canis
Morphology
immature stages and eggs
• Immature stages: smaller, elongated body, very short legs;
• Eggs: spindle-shaped, asymmetrical, 81 μm long.
• The ratio between adults and immature stages/eggs is an important indicator for the success of the therapy!!
Demodex canis: Life cycle
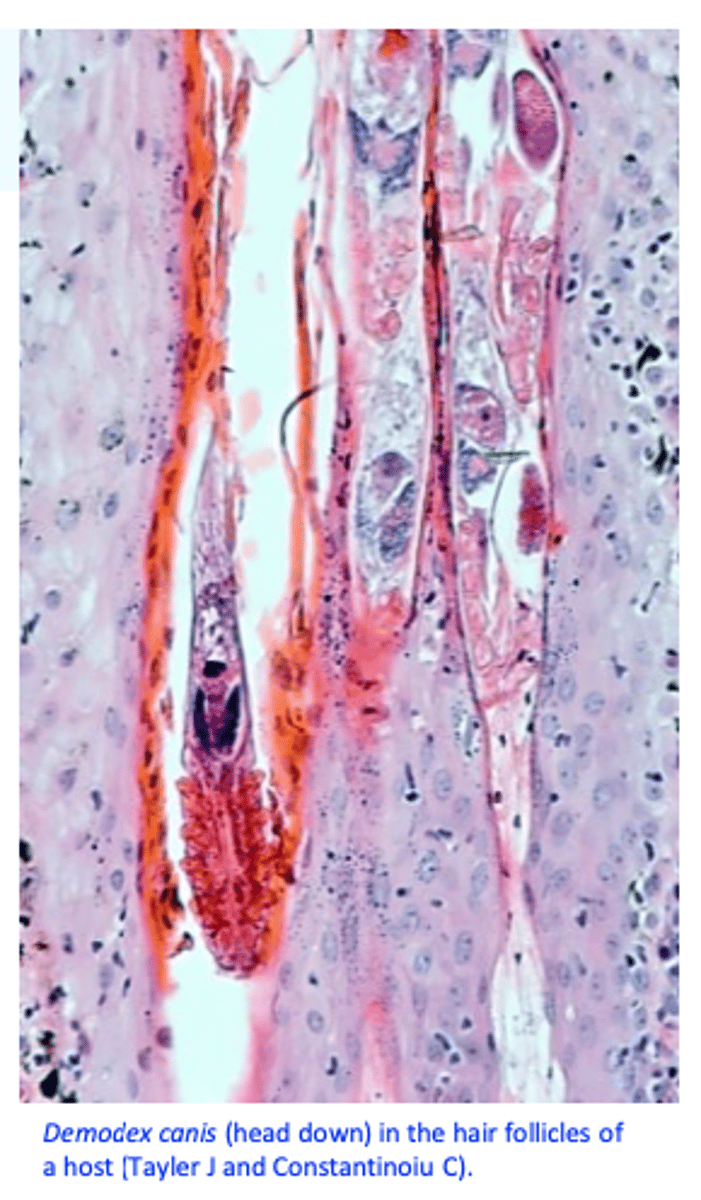
Demodex canis lives as a commensal, embedded head down in hair follicles, sebaceous glands and Meibomiam glands of the skin;
Females lay 20-24 eggs in the hair follicle which give rise to hexapod larvae => octopod nymphs => adults;
• The life cycle lasts 18-24 days;

Demodex canis: Epidemiology
Most dogs have Demodex canis in their skin but as a commensal;
Pups usually acquire the mites from mother by direct contact
• A single bitch may produce multiple litters affected with Demodicosis;
Demodicosis is NOT CONTAGIOUS;
Demodicosis is more common in purebred dogs;

Demodex canis: Pathogenesis
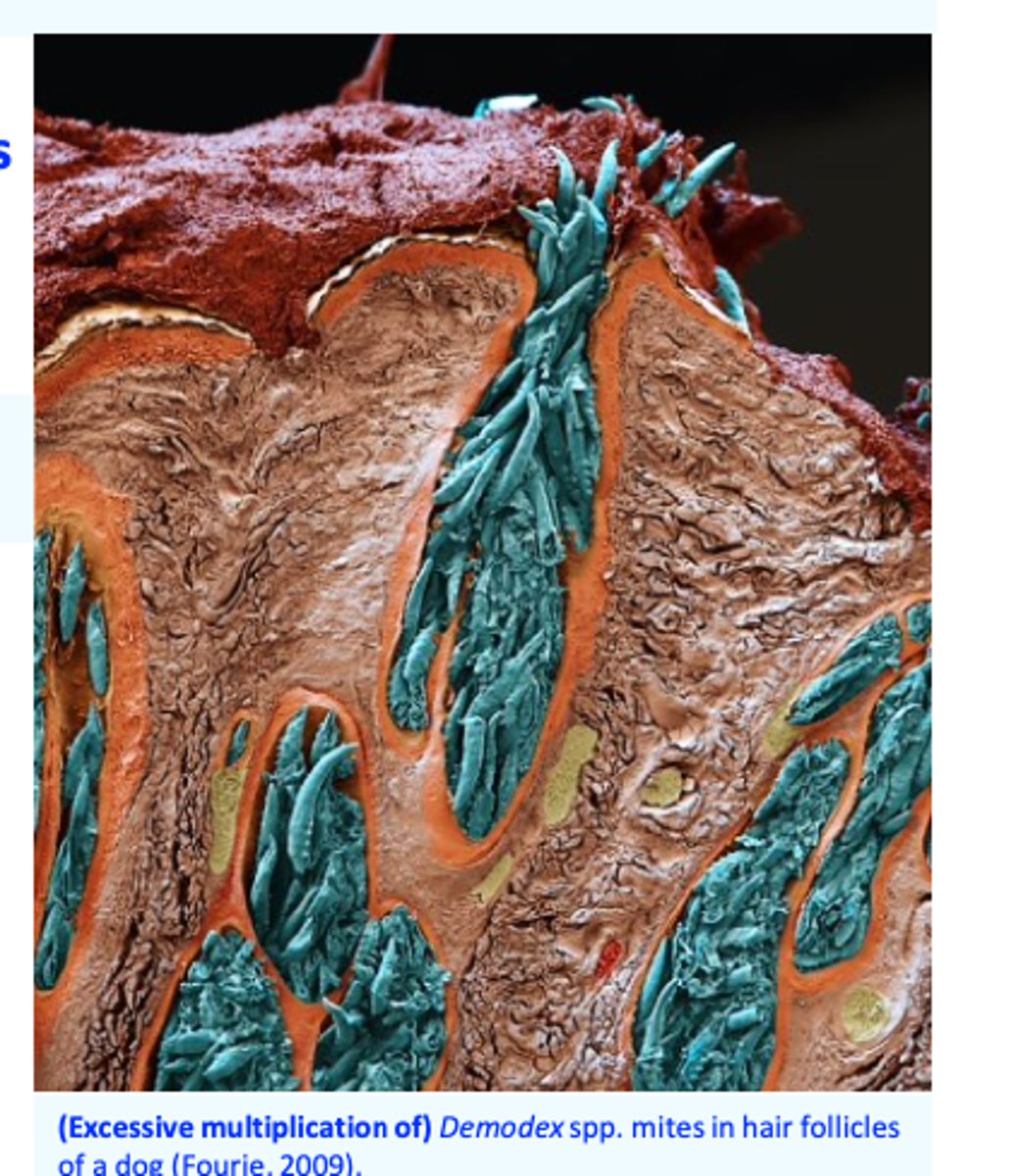
Demodicosis is the results of excessive multiplication of the mites and
development of huge populations in the skin of the dogs (clinical signs depend on the degree of mite proliferation);
Demodex canis is present in the skin of most dogs but only some develop severe clinical signs, why/how?
Altered immune response
1) A hereditary, Demodex canis-specific T cell defect and/or
2) Immunosuppression induced by other conditions
Demodex canis: Pathogenesis
1)
2)
1) Genetic basis of the disease based on:
Disease more common in purebred dogs;
There is breed predisposition;
A single bitch may produce multiple litters affected with Demodicosis (autosomal recessive inheritance suspected) => breeding of the dogs affected by (juvenile onset generalized) demodicosis is not recommended;
2) Factors that may cause immunosuppression and allow the proliferation of Demodex canis:
Hypothyroidism, hyperadrenocorticism, neoplasms, corticosteroid treatments, stress, endoparasites (Leishmania spp.), poor nutrition, chemotherapy, etc.
Many immunosuppressed dogs never develop demodicosis????!!!

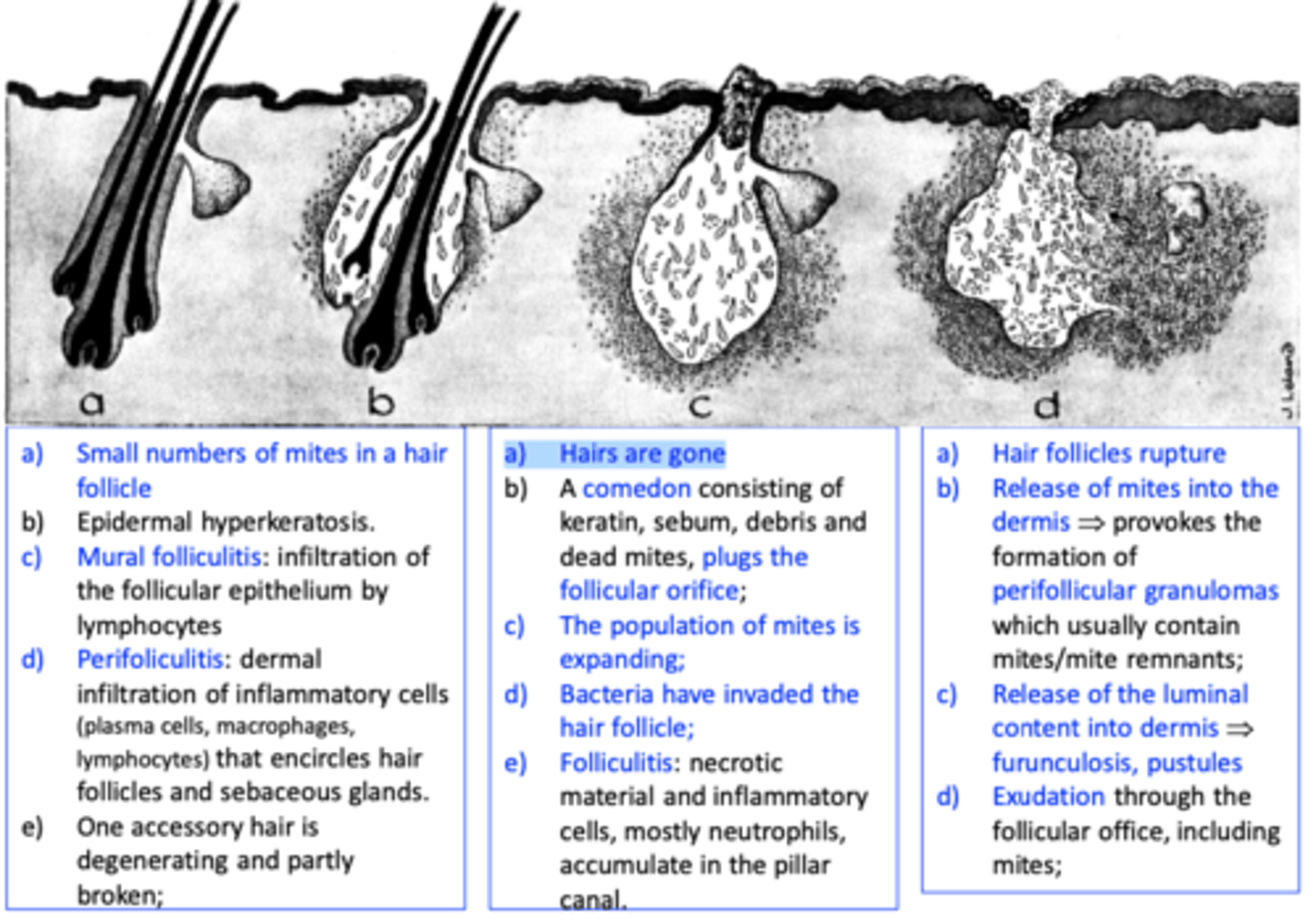
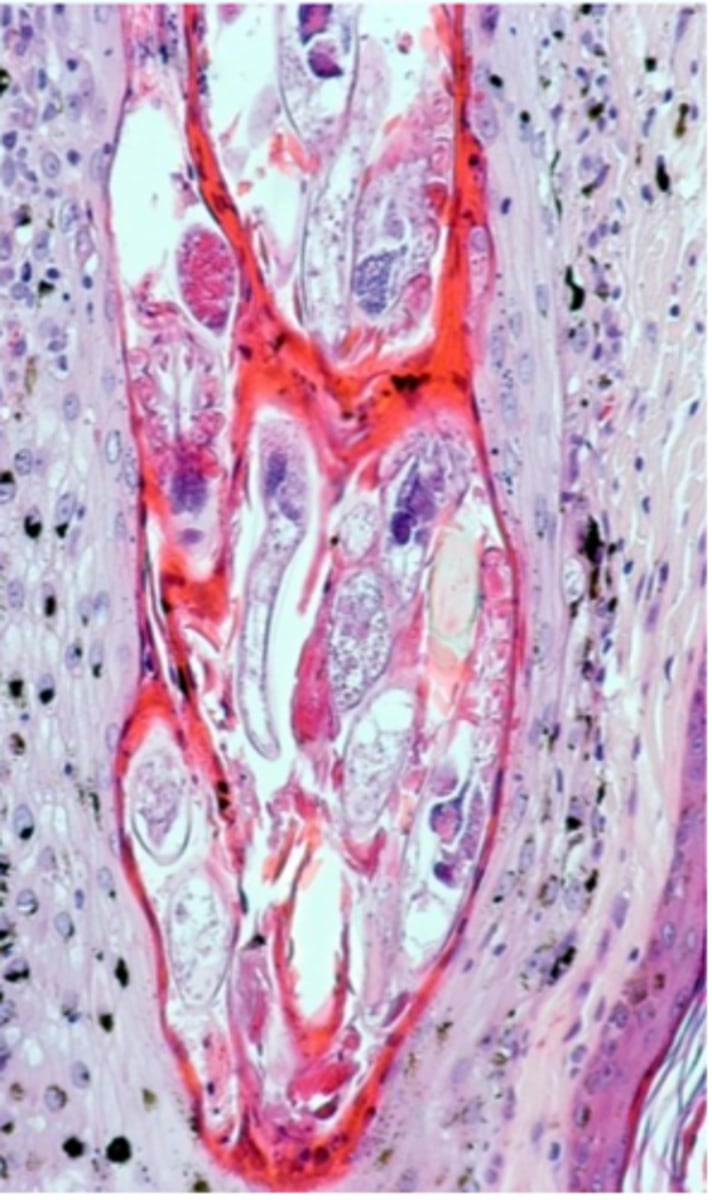
Demodex canis: Histopathology
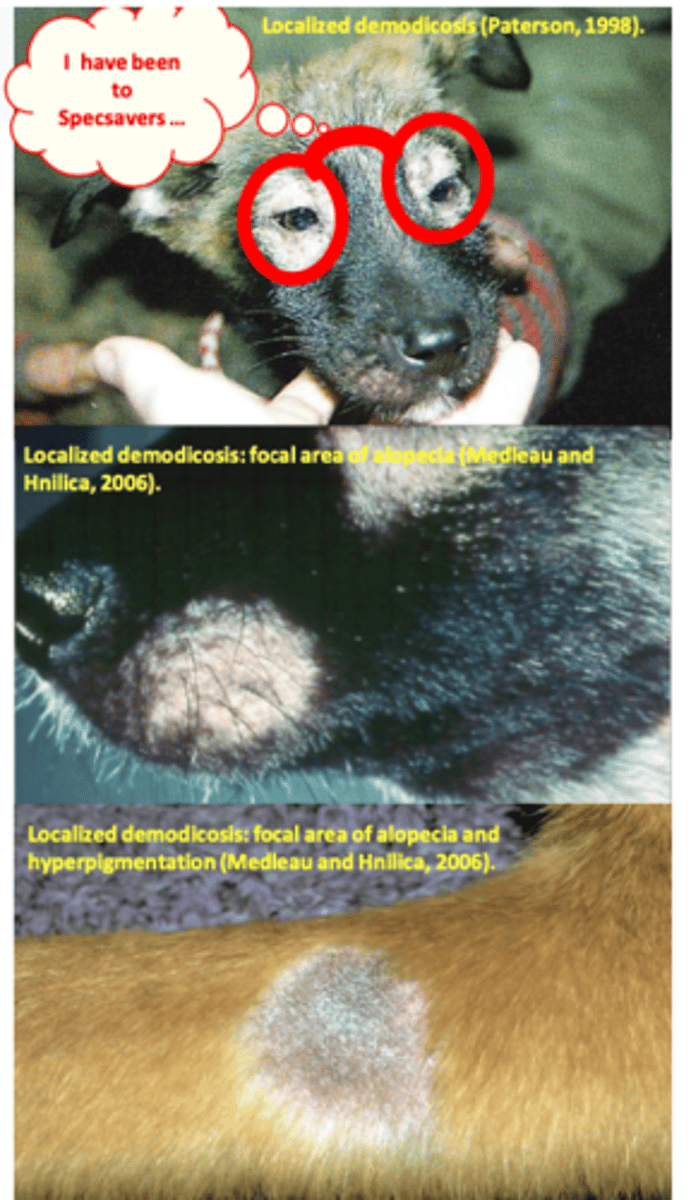
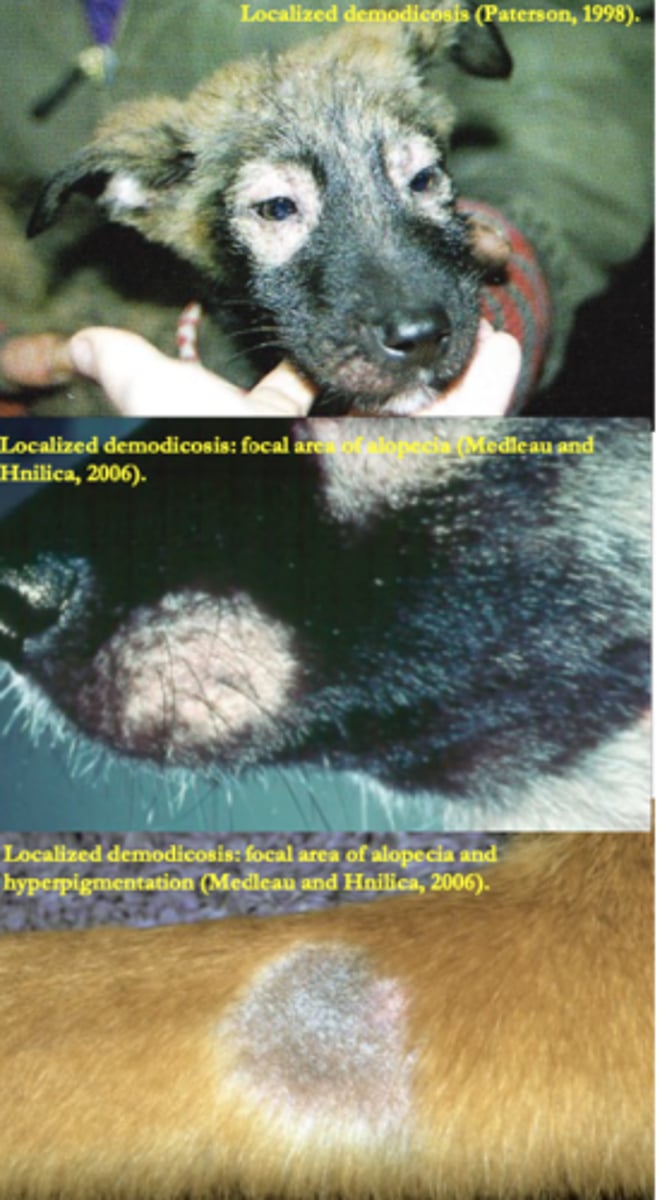
Deodex canis: localised demodicosis
Less than six lesions or only one body region affected;
Most cases occur in young dogs (3-6 months old);
Lesions are most common on head and the forelegs;• Circumscribederythema,(focal)alopecia,fine
scales, hyperpigmentation, usually no pruritus;
Good prognosis:
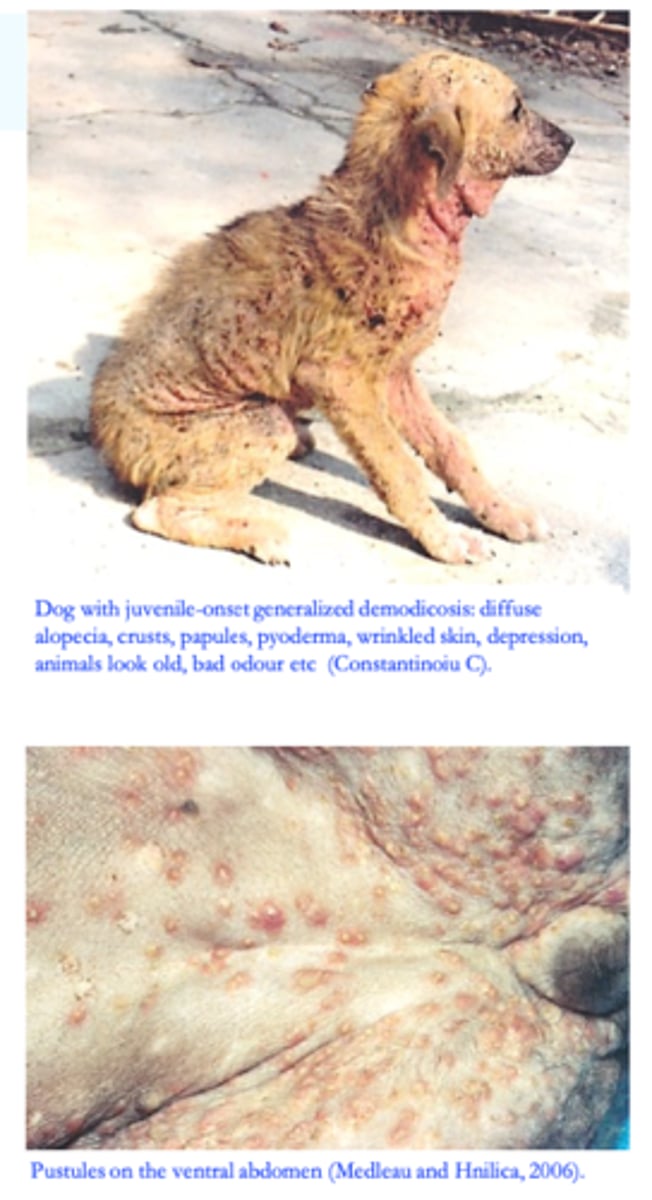
Deodex canis: 2) Generalized demodicosis
•More than 6 focal lesions, involvement of two or more body regions or involvement of two or more feet;
• Very serious skin disease that might be life threatening;
• Treatment used to be lengthy and expensive → treatment failures were common;
Juvenile-onset demodcosis: onset in young dogs, usually between 3 and 18-24 months;
a)b) Adult-onset demodicosis: onset in dogs older
than 18-24 months of age;

Deodex canis:
Juvenile-onset generalized demodicosis
• Onset in young dogs, usually between 3 and 18- 24 months;
Inherited disease (multiple genes involved) => affected animals and their parents or siblings should not breed;
Temporary immune alteration seems to play an important role;
Risk factors

Deodex canis:
B) Adult-onset generalized demodicosis
• Onset in dogs older than 18-24 months of age that are immunocompromised because of an underlying condition such as:
Hyperadrenocorticism (endogenous or iatrogenic);
Hypothyroidism;
Immunosuppressive drug therapy;
Diabetes mellitus;
Neoplasms;
Stress: oestrus, pregnancy, surgery;
Adult-onset generalized demodicosis is not inherited.

Generalized demodicosis
I. Squamous form
Alopecia: patchy, regional, multifocal, or diffuse;
Erythema, silvery grayish scaling, comedones, hyperpigmation;
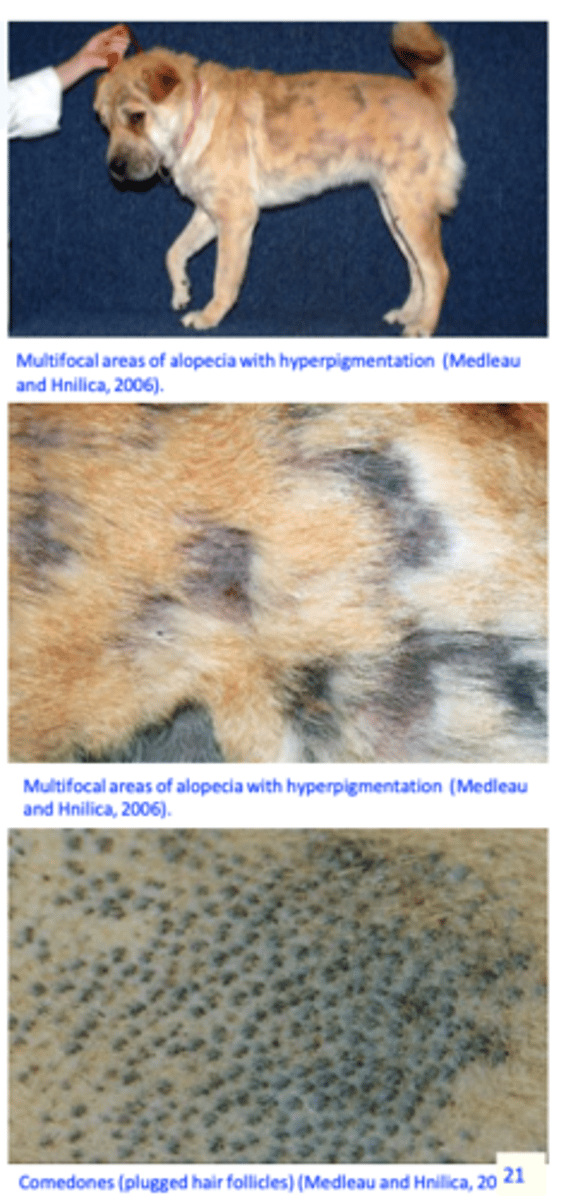
Generalized demodicosis
II. Pustular form
Secondary bacterial infection => papules & pustules, furuncles, pruritus (the short form of D. canis is more often associated with pruritus);
Crusts, hyperpigmentation, affected skin may become eroded or ulcerated from secondary superficial or deep pyoderma;
Peripheral lymphadenopathy, pain, fever, anorexia, lethargy, depression, debilitation;
Affected dogs may have an offensive odour (due to oxidation/effects of bacteria on the skin lipids);
The animals will look older, skin is wrinkled;
Lesions can be anywhere on the body, including the feet;
Generalized demodicosis
III. Pododemodicosis
Interdigital erythema, alopecia, pruritus, pain, hyperpigmentation, lichenification, scaling, swelling, crusts, pustules, ulcers etc;

Generalized demodicosis
IV. Otodemodicosis
Pruritus (shaking the head, excoriations at the base of the ear), erythema, pale coloured ceruminous discharge, bacterial complications (=> pruritus);

Deodex canis: Diagnosis
I. Clinical signs & history
II. Microscopic examinations of the skin scrapings
• Deep scrapings until capillary
bleeding;
Finding more than one mite clinical demodicosis;
For each scraping record the area, the number of mites, the ratio between live and dead adults and the ratio between immature and mature mites => the data are used to monitor the efficacy of the therapy;
IV. Trichography
V. Exudative sampling:
VI. Acetate tape preparations:
VII. Oticswabs
VIII. Skin bioposies

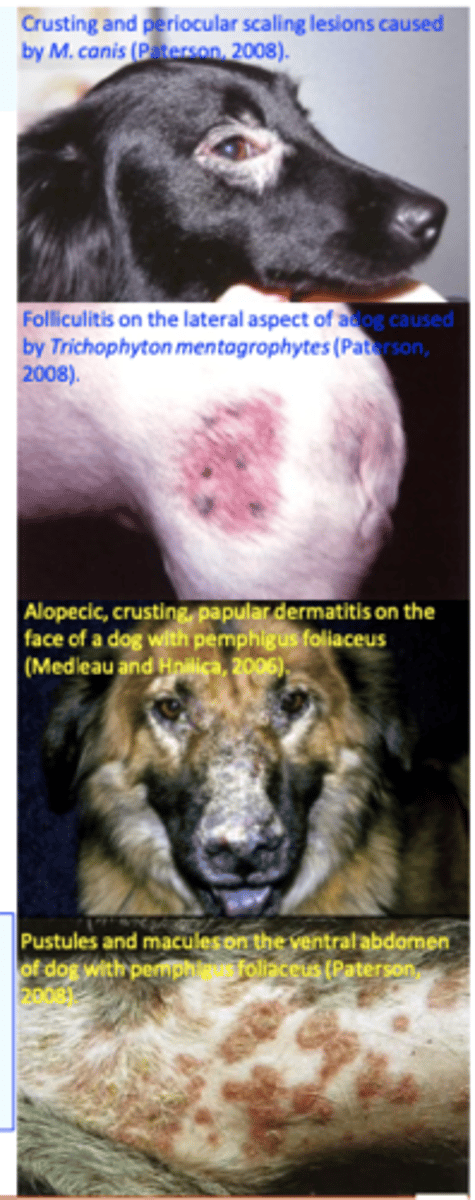
Deodex canis: Differential diagnosis
Other causes of folliculitis and furunculosis
Hypersensitivity (atopy, flea bite, food etc);
• Dermatomyositis
• Hyperadrenocorticism
Clinical signs of generalized demodicosis may be variable => it is advisable to perform skin scrapings in dogs with unidentified skin diseases, pyoderma, seborrhea, alopecia, exfoliative dermatitis etc;
Deodex canis: Treatment
Localized demodicosis
a) Acaricidal treatment might not be necessary
b) If you decide to treat:
• Do not use glucocorticosteroids!!
why not use glucocorticoids?
will weaken immune system
Generalised demodicosis: treatment is (used to be?) challenging
Need to identify/treat the underlying conditions;
Treatments used to be expensive and long => owner compliance;
The success rate used to be lower in dogs with adult-onset demodicosis than in dogs with juvenile-onset demodicosis;
Treatment failures used to occur:
Side effects of some drugs/therapeutical schemes;
Relapses used to occur anytime (3 years) after cure.

Generalised demodicosis: principles of therapy
1) Identify the underlying condition and correct/treat it (adult onset demodicosis);
2) Acaricidal therapy
- Formamidines (Amitraz), macrocyclic lactones (Ivermectin, Moxidectin, Milbemycin, Doramectin) and isoxazolines (Afoxolaner, Fluralaner, Sarolaner, Lotilaner);
3) Treat the concurrent bacterial skin infection
4) Monitor the efficacy of the therapy
• Switch to another acaricide in unresponsive dogs.
Acaricidal therapy - formamidines
3. Isoxazolines: approved, very effective
• Afoxolaner
• Sarolaner
• Fluralaner
• Lotilaner
Clinical efficacy increases with increasing the concentration and reducing the treatment intervals => should be used only in dogs not responding to conventional treatment severe/fatal toxicoses might occur (antidotes: Atipamezole and Yohimbine);
Concurrent use of amitraz dips and macrocyclic lactones should be avoided/used cautiously.

Acaricidal therapy
2. Macrocyclic lactones (MLs)
Depending on the compound, MLs are licensed for prevention and control of a wide range of parasites
Often used extralabel (and at doses greatly higher than those recommended by manufacturers) for the control of some parasites
A significant proportion of collies and other herding dogs breeds harbour a mutation in the MDR1 (ABCB1) gene that makes them extremely susceptible to toxicity from MLs => MLs in extralabel dosage/formulation should not be used/used with extreme cautios in ML sensitive dogs (Collie and other herding dog breeds);
Acaricidal therapy
Isoxazolines
• Afoxolaner(NexGard,NexGard
Spectra)
• Fluralaner (Bravecto)
Lotilaner
Single treatment (orally or spot-on): highly effective: remission rate 100% 84 days after a single treatment;
Sarolaner - 2 monthly treatments are highly effective: remission rate 100% 44 days after the first treatment
Generalized demodicosis: Monitor the efficacy of the therapy
Treatment efficacy is monitored monthly by clinical examination and skin scrapings;
• Treatment should be changed in dogs that show no clinical improvement or do not show reduction in mite counts after 1-2 month treatments
Time to cease the therapy
-> No clinical signs and two negative scrapings one month apart
Dogs with generalized demodicosis and their parents should not breed
Feline Demodicosis
Demodex cati
Demodex gatoi

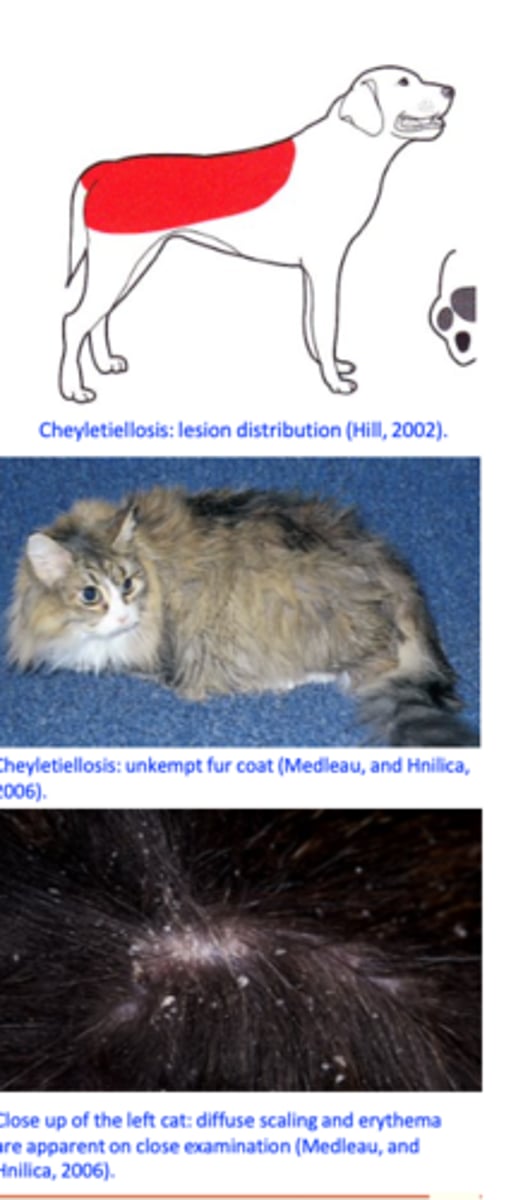
Cheyletiellosis (Walking dandruff)
• Cat: Cheyletiella blakei
• Dog: Cheyletiella yasguri
• Rabbits: Cheyletiella parasitivorax
• Also reported from foxes and accidentally from humans;
• Feeding: tissue fluids/lymph

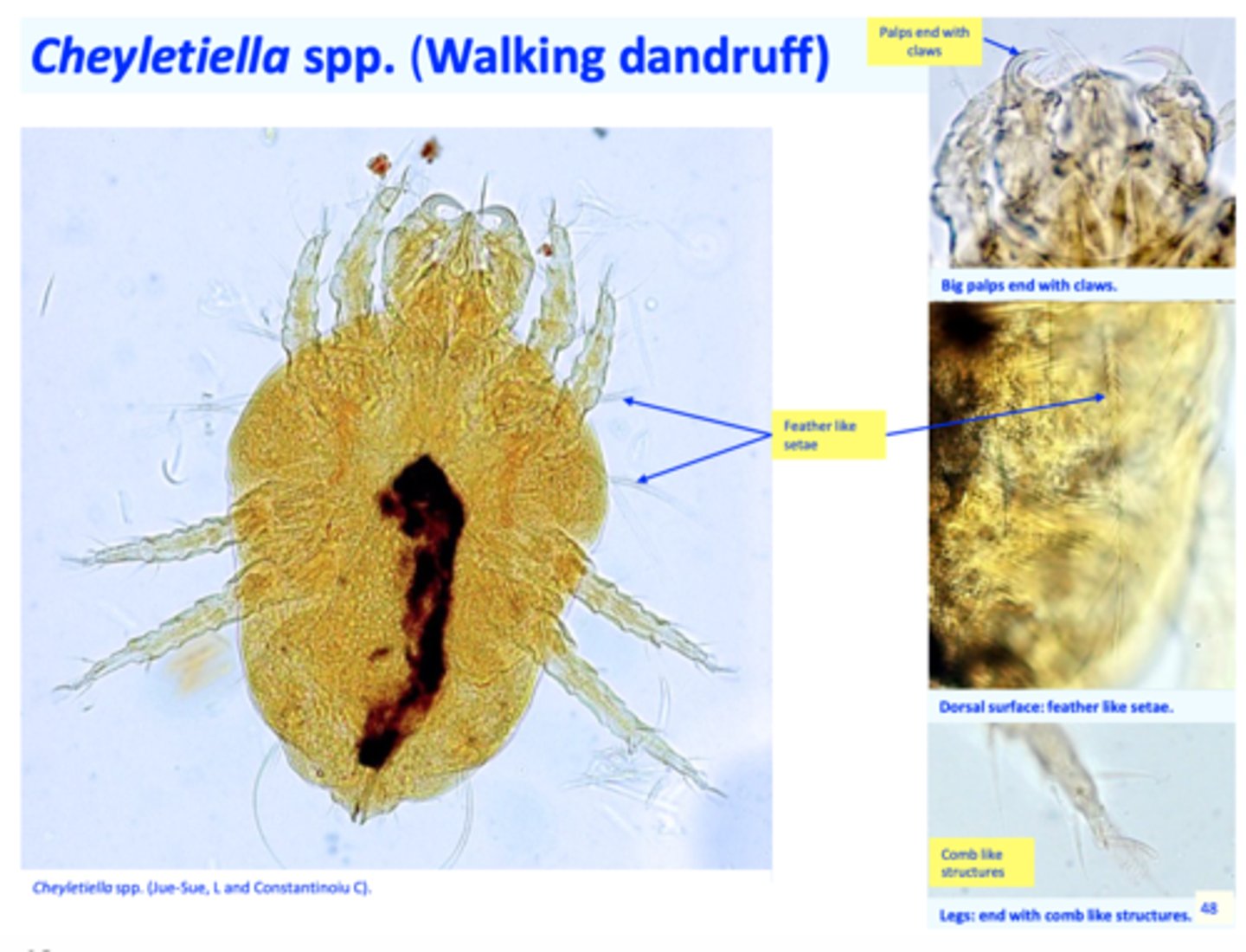
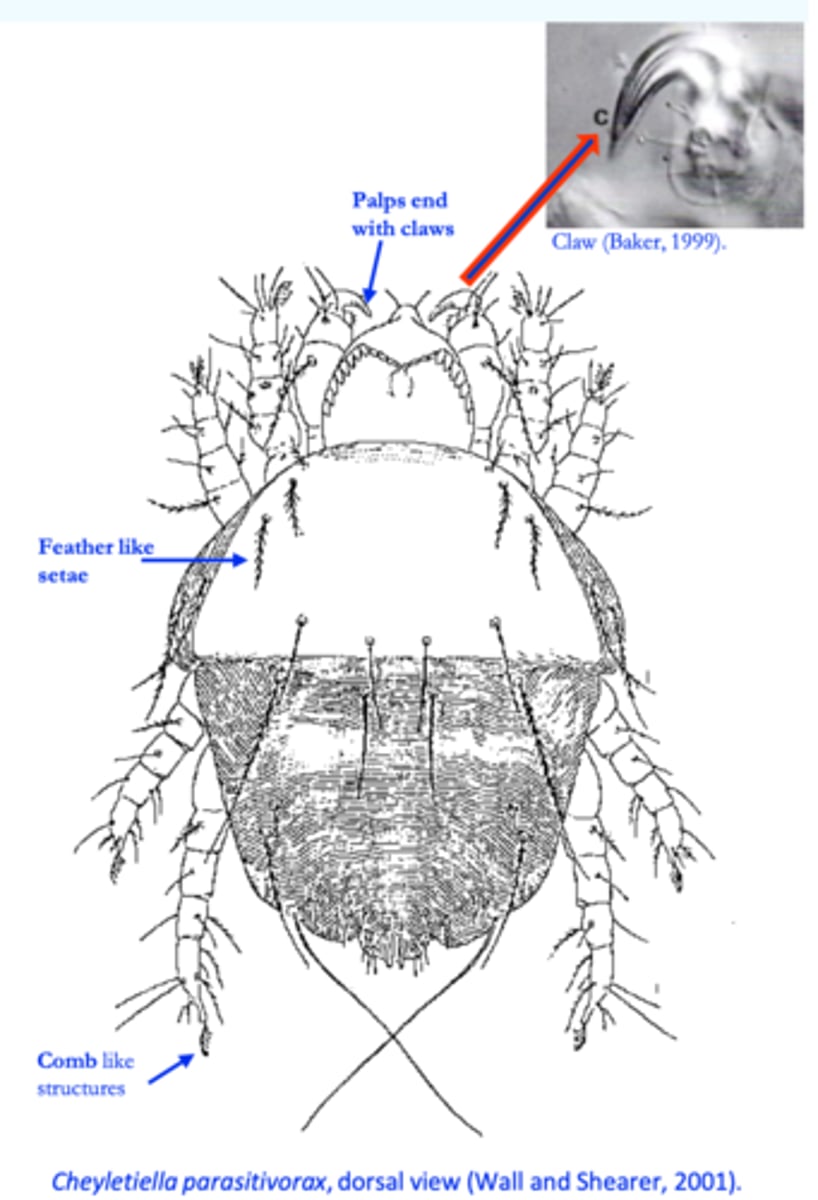
Cheyletiella spp. (Walking dandruff)
Gnathosoma: big, palps end with claws;
Legs: end with comb like structures;
Dorsal surface: feather like setae.
Cheyletiella spp. (Walking dandruff)
Life cycle
• The parasites spend their entire life on the host;
• Eggs are attached to the hairs of the host
• The life cycle comprises egg, larva, two nymphal stages and adults
Cheyletiella spp. (Walking dandruff) Epidemiology
• All breeds might be affected;• More common in Cockerel and cats with long hair;
• Animals from all ages might become infested:
• Infestations are more severe in young animals;
• Some animals, usually adults, do not show clinical signs => asymptomatic carriers;
• Parasites are easily transferred from one host to another host (direct contact and indirect: brushes, combs etc) => highly contagious => common in animals from kennels, pet shops or that visit kennels, groomers etc => in multiple-pet households more than one animal is generally affected;

Cheyletiella spp. (Walking dandruff)
Pathogenesis
Pruritus because of the mechanical activity and hypersensitivity => the severity of clinical signs might not be proportional to the number of mites;
Scaling seems to be the result of a host defence mechanism => epidermal cell turnover increases in response to injury to the epidermis;
Cheyletiella spp.
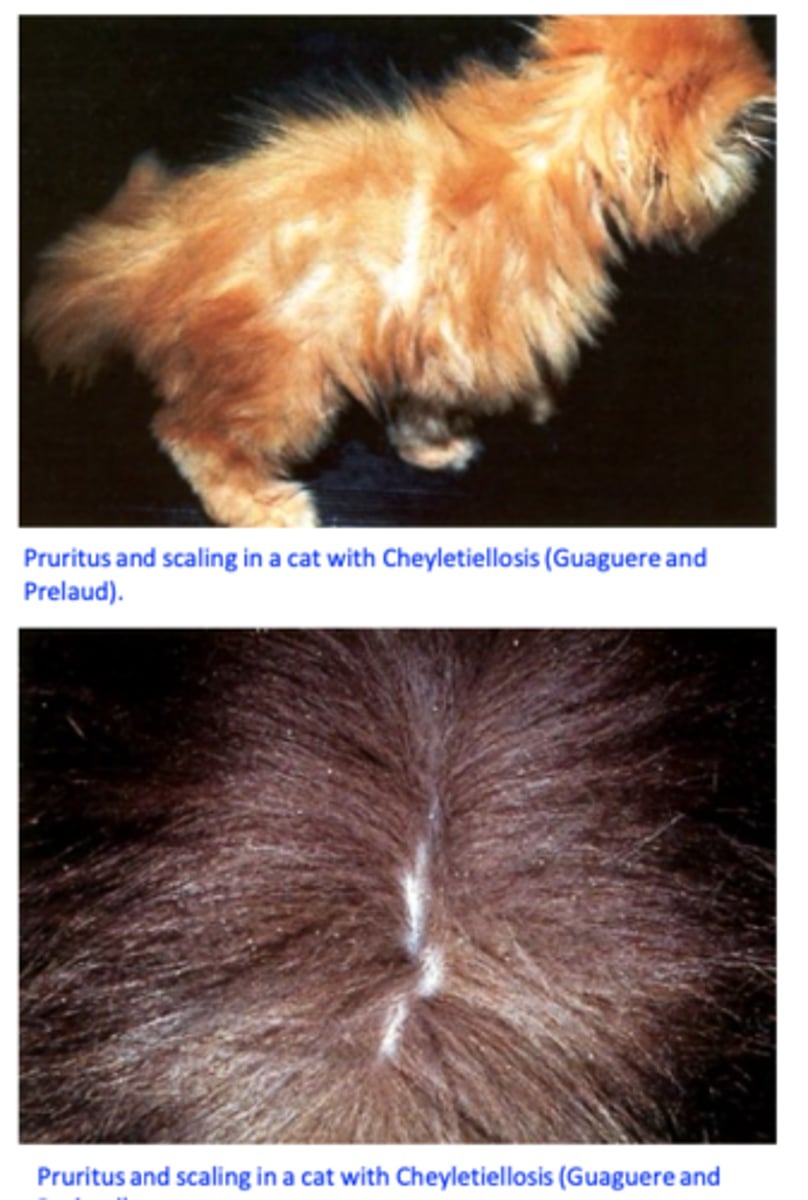
Clinical signs
• Lesionsoccurmainlyoverthedorsum;
Excessive scaling (i.e., dandruff, scurf) => gives the hair coat a
powdery or mealy appearance;
Pruritus: may be mild to severe;
Alopecia, erythema, papules, crusts;
Cat: miliary dermatitis.
Cheyletiella spp.: Diagnosis
Clinical signs
History
Detection of Cheyletiella mites or eggs might be difficult:
- Direct examination of the surface of the skin with magnifying glasses
- Superficial skin scrapings;
- Acetate tape impressions
- Combing (flea comb) or brushing of the hair
Sometimes the infestations are diagnosed because of the dermatitis caused by Cheyletiella spp. to the owners!!!

Cheyletiella
Differential diagnosis
• Ectoparasites: lice, fleas, Demodex spp., Sarcoptes scabiei;
• Hypersensitivities: food, atopy;
Cheyletiella spp.: Treatment
Cheyletiella spp. are generally sensitive to many acaricidal compounds
All affected and in-contact animals (dogs, cats, rabbits) should be treated
Continue treatments for 2-4 weeks after resolution of clinical signs and pruritus and until no mites or eggs can be found;
The environment should be cleaned and treated with an acaricide
Fipronil (spray & spot on) applied every 30 days for 2-3 treatments
Selamectin, spot-on, three times at 1-month intervals
Moxidectin & imidacloprid (Advocate), two monthly treatments, 100% efficacy in dogs
Trombiculosis
(Chigger/harvest mites)
Neotrombicula/Trombicula spp.(many species)
Hosts: dog, cat, humans etc.

Ivermectin
not registered for dogs, extralabel use!!!
➢ should be considered only if approved treatments fail!!
➢ can cause severe neurological adverse effects: lethargy, ataxia, tremours, mydriais and death;
➢ Collie dogs, their crosses and other herding breeds are most commonly
affected
Doramectin
• Not approved for use in dogs but used extra label for the treatment of Demodicosis;