Pathophysiology Midterm: Chapter 23 (Concepts of Care for Patients With Noninfectious Upper Respiratory Conditions)
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
Obstructive Sleep Apnea (OSA)
- A sleep-related breathing disorder with apneic periods that last 10 seconds or more.
- defined by partial or complete collapse of the airway, interrupting ventilation and resulting in hypoxia and lack of sleep
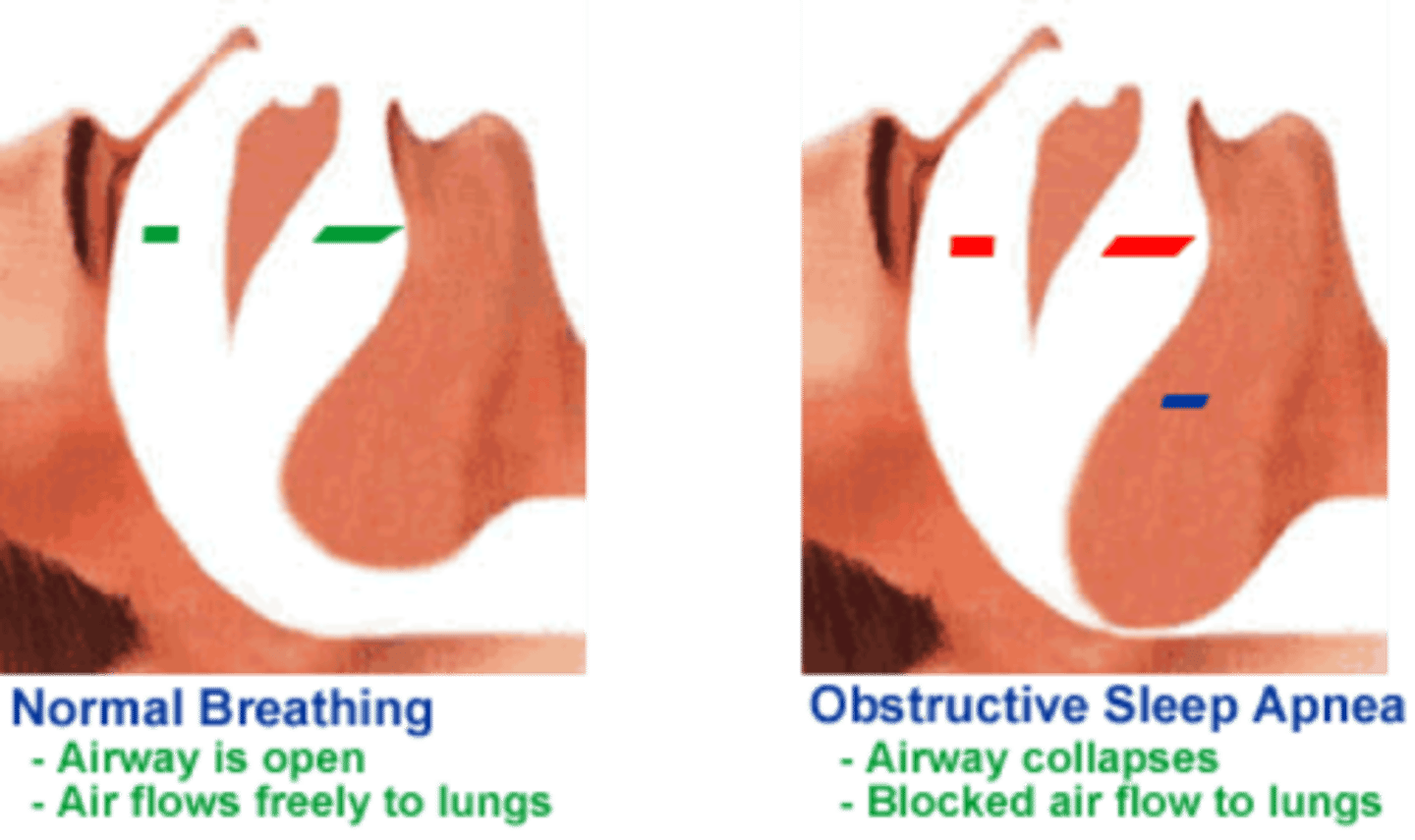
What does OSA result from?
Partial or total airway obstruction recurring during sleep with apneic episodes that last 10 seconds or longe
What is OSA characterized by?
Intermittent hypoxia (low levels of oxygen in the tissue, affecting gas exchange)
Symptoms of OSA
Fatigue, daytime sleepiness, headaches, waking with gasping or choking sensation, difficulty concentrating, irritability, depression, and memory problems
What can OSA increase the risk of?
hypertension and other cardiovascular disorders, insulin resistance, stroke, and cognitive impairment such as dementia
What is the most common cause of OSA?
- upper airway obstruction by the soft palate or tongue.
- During sleep the head and neck muscles relax, allowing the tongue, soft palate, and neck structures to be displaced.
- As a result, the upper airway is obstructed, but neural control of chest movement is unimpaired.
Structural Risk Factors for OSA
Soft tissue and craniofacial dimensions, and obesity, which are attributed to genomic variation, though more research is needed to better understand genetic data and OSA
Risk factors for OSA
Age, male sex, obesity, or enlarged tonsils, uvula, or adenoid tissue
Interprofessional Collaborative Care for OSA: Assessment (History)
- Ask about sensations of daytime sleepiness or falling asleep while performing tasks such as using the computer, reading, or driving
- Ask patients whether they can recall ever being awakened by their own snoring and whether family members have noticed heavy snoring
- Also ask whether family members have ever observed the patient to have a disturbed breathing pattern while sleeping.
- Whether they have tried to induce a deeper sleep with over-the-counter sleep aids or increased evening alcohol consumption.
- Ask patients whether they are awakened often with "heartburn," stomach contents in the mouth, or a burning, choking sensation with coughing.
Common pattern of breathing for OSA
increasing spaced out breaths + apnea + chest and abdominal movements = gasps/snorts that wake pt up
Why do PTs w/ OSA also develop some degree of gastroesophageal reflux disease (GERD) at night?
strong abdominal and chest movements during an apnea episode, overeating, eating or drinking close to bedtime, and lying flat while sleepin
Interprofessional Collaborative Care for OSA: Physical Assessment / Signs and Symptoms (PHYSICAL)
- Assess patients' general appearance, including height and weight
- Examine the jaw, external neck, and chin. OSA is associated with a retracted lower jaw, smaller chin, and shorter neck.
- Examine the oral cavity and throat for size and shape of the pharynx, size and shape of the uvula, and tongue thickness and position, and determine whether other structures (e.g., tonsils, adenoids, pillars, soft palate) are swollen or enlarged.
When doing a physical cardiac assessment on a pt w/ OSA, what are we monitoring?
hypertension
BP. HR, O2
if not treat for high BP,= redo BP later on during exam
What do we ask when doing a Psychosocial Assessment for OSA pt?
- Irritability, personality changes, depression
-CNS - recall, concentration, perceived energy level, and the ability to stay on task when working or studying.
- Long-term untreated = + risk of mild cognitive impairment or dementia
Interprofessional Collaborative Care for OSA: Diagnostic Assessment
- A beginning assessment includes having the patient complete a questionnaire regarding perceived sleep quality and extent of daytime sleepiness
- Polysomnography: ECG, EEG, EMG (Sleep Study Test)
Polysomnography
- a sleep study testing for wakefulness and sleepiness
- electrodes are applied to measure electrocardiogram (ECG), electroencephalogram (EEG), pulse oximetry, electrooculography (EOM), and electromyography (EMG)
Nonsurgical Management for OSA
- Position-fixing devices may prevent subluxation of the tongue and reduce obstruction. Use of an oral appliance, called maxillomandibular advancement, can improve airflow by supporting the lower jaw in a more forward position.
- Noninvasive positive-pressure ventilation (NPPV) via continuous positive airway pressure (CPAP) to hold open the upper airways is the most commonly used form of nonsurgical management for OSA.

Surgical Management for OSA
- Implanted stimulators represent a minimally invasive surgery that can help patients with mild to moderate sleep apnea. This surgery involves placing an electrode in the neck that can stimulate the hypoglossal nerve (cranial nerve XII).
- Tracheostomy is a possible but uncommon type of surgery to manage OSA
- tonsillectomy, adenoidectomy, uvulectomy, or repair of a deviated septum.
-Uvulopalatopharyngoplasty (UPPP) is a collection of procedures that are more complex and intended to resolve OSA by remodeling the entire posterior oropharynx.
- Modified uvulopalatopharyngoplasty (modUPPP) is a more recent reconstructive approach with a variety of procedures that may be performed using conventional, robotic-assisted, or laser surgery techniques.
Post Op Care for Surgical Management of OSA
- Maintain a patent airway
- Relieving pain
- Preventing complications
Education points for pt that just underwent surgery for OSA?
oropharynx checks for bleeding, swelling, or indications of infection.
examine throat with a mirror twice daily and assess its internal size (often by comparing it to coin sizes)
infection? = call PCP
Evaluation for Treatment of OSA
less sleep apnea episodes
better gas exchange = better sleep
less day time sleepy // + daytime energy
chill surgery recovery
Epistaxis
Nosebleed, common due to the many capillaries within the nose

Why do nosebleeds occur?
As a result of loss of tissue integrity from trauma to the nasal mucosa, hypertension, blood dyscrasia (e.g., leukemia), inflammation, tumor, decreased humidity, nose blowing, nose picking, chronic cocaine use, and procedures such as nasogastric (NG) suctioning.
Where in the nose do older adults tend to bleed from?
Posterior portion of the nose
When does a patient often report when bleeding occurs?
After sneezing or blowing the nose
What should be documented with epistaxis?
- Document the amount and color of the blood, and take vital signs.
- Ask about the number, duration, and causes of previous bleeding episodes and the patient's history of nasal or facial trauma or other bleeding or bruising issues,
- as well as current medications and family history of bleeding
Emergency Care for a Patient with Anterior Nosebleed
•Sit patient upright and leaning forward to prevent blood from entering the larynx and possible aspiration.
• Offer reassurance, and attempt to keep the patient quiet to reduce anxiety and blood pressure.
• Squish nose for 15-20 minutes, and apply ice or cool compresses to the nose and face if possible.
• If nasal packing is necessary, loosely pack both nares with gauze or nasal tampons.
• To prevent rebleeding from dislodging clots, instruct the patient not to blow the nose for 24 hours after the bleeding stops.
• Instruct the patient to seek medical assistance if these measures are ineffective or if the bleeding occurs frequently.
What can be done if the nosebleed doesn't respond to interventions (anterior nosebleed)?
The affected capillaries may be cauterized with silver nitrate or electrocautery, and the nose packed. Anterior packing controls bleeding from the anterior nasal cavity.
What can be done if the nosebleed doesn't respond to interventions (posterior nosebleed)?
- may be more severe and harder to control
- Posterior packing, epistaxis catheters (nasal pressure tubes), or gel tampons are placed through the nose within the posterior nasal region to stop the bleeding
What may be prescribed for a nosebleed patient?
humidity, oxygen, bed rest, and antibiotics may be prescribed. Opioid drugs may be prescribed for pain.
What may be assessed for a nosebleed patient?
Respiratory distress
O2 Sat - hypoxemia?
if on opioids - hourly check for gag/cough reflexes
What should be done for posterior bleeding that doesn't respond to packing or tubes?
Cauterizing or ligating the blood vessels or performing an embolization of the bleeding artery with interventional radiology.
Home remedies for aftercare of nose bleeds?
• Petroleum jelly to the nares for comfort.
• Saline nasal sprays = + moisture and prevent rebleeding.
• Avoid vigorous nose blowing, the use of aspirin or other NSAIDs, and strenuous activities such as heavy lifting for at least 1 month.