Hematology
1/146
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
147 Terms
What should you observe in general appearance during a physical exam?
Look for pallor, jaundice, cachexia (severe unintentional weight loss, muscle wasintg), or other abnormal general appearances
What nail abnormalities can indicate underlying disease?
Platonychia (flattened nails)
and
koilonychia (spoon-shaped nails)
How is anemia diagnosed?
By laboratory measurement: hemoglobin below the normal range for age and sex (Hb <12 g/dL in males, <11 g/dL in females)
Why do adult males normally have higher hemoglobin than females?
About 2 g/dL higher, due to hormonal and physiological differences
What factors affect the symptoms of anemia?
1. Speed of onset (rapid anemia causes more severe symptoms)
2. Severity of anemia
3. Age of the patient (younger patients tolerate anemia better)
4. Presence of cardiovascular disease (symptoms at higher Hb levels)
At what hemoglobin level does anemia become an emergency?
Hb <4 g/dL, may require urgent blood transfusion
What are some signs and symptoms of chronic severe anemia?
Fatigue, pallor, shortness of breath, tachycardia, dizziness, palpitations, headache, cold intolerance
What cardiovascular symptoms are seen in anemia?
-Exertional dyspnea or dyspnea at rest
-Palpitations
-Throbbing in head and ears
-Precipitation of angina, intermittent claudication, and vascular insufficiency
What genitourinary symptoms may occur in anemia?
Amenorrhea or menorrhagia, loss of libido
Why?
-Severe anemia can disrupt hormonal balance (especially sex hormones).
-Low oxygen delivery and iron deficiency can affect reproductive function and sexual drive
What gastrointestinal symptoms may be present in anemia?
Anorexia, nausea, flatulence, weight loss
What are the visible signs of anemia on physical examination?
1. Pallor of skin, mucous membranes, conjunctivae, and palmar creases
2. Tachycardia and collapsing pulse
3. Raised jugular venous pressure (JVP)
What cardiovascular signs may develop in chronic severe anemia?
1. Flow/haemic murmurs (e.g., midsystolic across aortic and pulmonary valves)
2. Cardiomegaly
3. Congestive heart failure
4. Ankle edema
What is the most common type of anemia worldwide?
Iron deficiency anemia
Why is menstrual history important in evaluating anemia?
Menorrhagia is a common cause of anemia in menstruating females
What aspects of dietary history are important in anemia evaluation?
Intake of iron and folate, especially in pregnancy, lactation, or periods of growth; assess for malnutrition from diarrhea or malabsorption
Why is drug history important in anemia evaluation?
Certain drugs can cause blood loss (aspirin, NSAIDs), hemolysis (e.g., antimalarials in G6PD deficiency), or bone marrow suppression
How can specific clinical findings suggest the cause of anemia?
1. Abdominal mass → possible caecal carcinoma
2. Jaundice → hemolytic anemia or portal hypertension
3. Neurological signs (neuropathy, dementia, subacute combined degeneration) → B12 deficiency
4. Pain crises/ulcers → sickle cell anemia
What is the morphological classification of anemia?
Based on red cell size, hemoglobin content, and red cell indices:
Microcytic hypochromic anemia: Low MCV, MCH, MCHC; examples: iron deficiency, sideroblastic anemia, thalassemia
What are common causes of macrocytic anemia?
Megaloblastic anemia due to folic acid or vitamin B12 deficiency
What defines a normocytic normochromic anemia?
RBCs have normal MCV, MCH, and MCHC
What are common causes of normocytic normochromic anemia?
Blood loss, hemolytic anemia, aplastic anemia
What is dimorphic anemia?
Presence of two populations of RBCs (microcytes and macrocytes) on peripheral smear
What causes dimorphic anemia?
Combined deficiencies, e.g., iron + folic acid or vitamin B12 deficiency
What is leucopenia?
A low total white blood cell (leukocyte) count in the peripheral blood
What is agranulocytosis?
Virtual absence of granulocytes (including neutrophils) in peripheral blood
Why is neutropenia clinically important?
Neutrophils are key phagocytic cells; low counts increase risk of severe infections and fatal sepsis
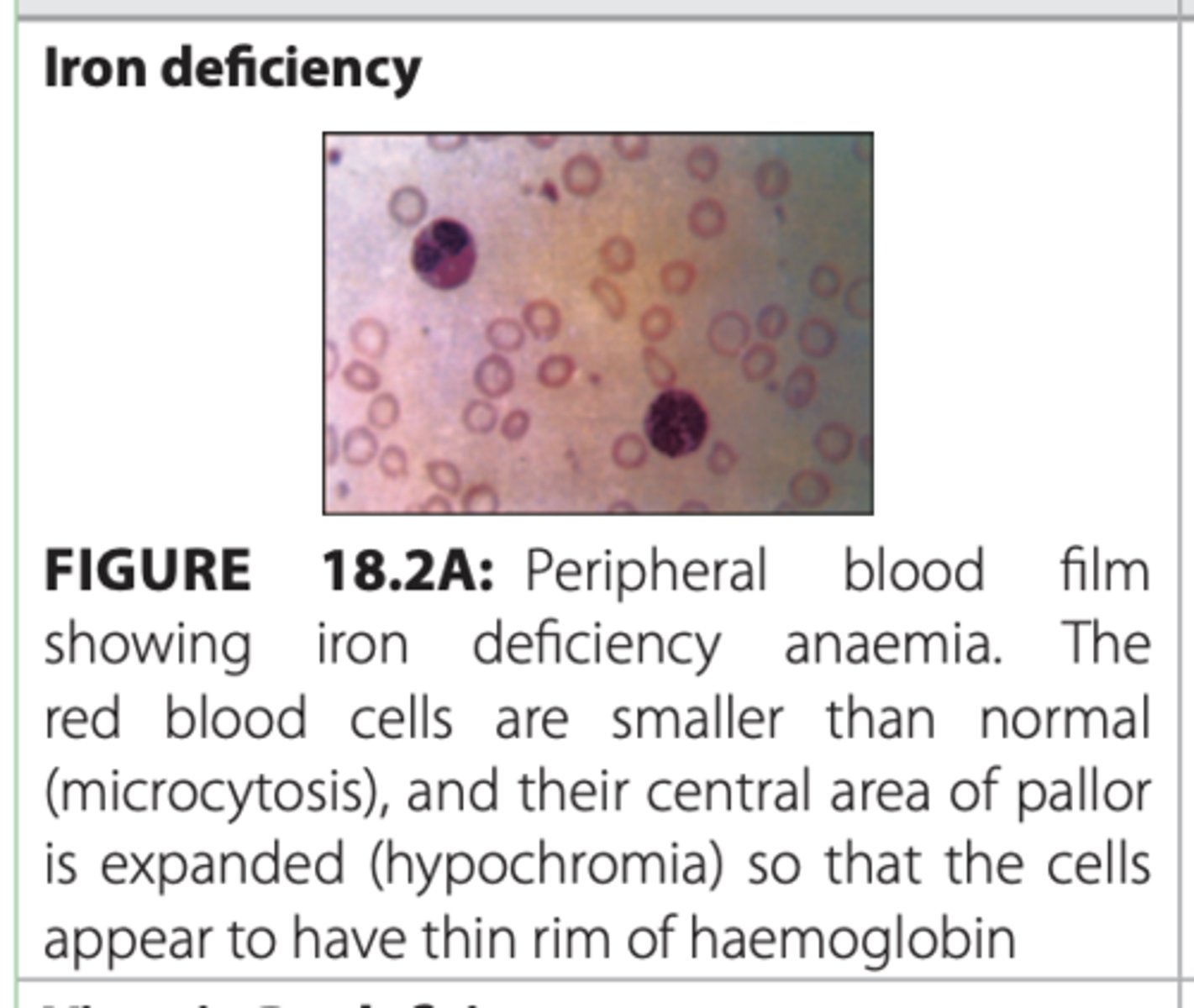
What are key features of iron deficiency anaemia?
-Glossitis with papillary atrophy (“bald tongue”)
-Angular stomatitis (cheilosis)
-Dysphagia (Plummer-Vinson/Peterson-Kelly syndrome)
-Koilonychia (spoon nails)
-Microcytic, hypochromic RBCs on peripheral smear
What would IDA look like on a peripheral blood film?
Causes of IDA?
1. Dietary deficiency (strict vegetarian diet)
2. Malabsorption, gastrectomy
3. Chronic blood loss (menstrual, GI tract, renal, pulmonary)
4. Increased demand (children, pregnancy, lactation)
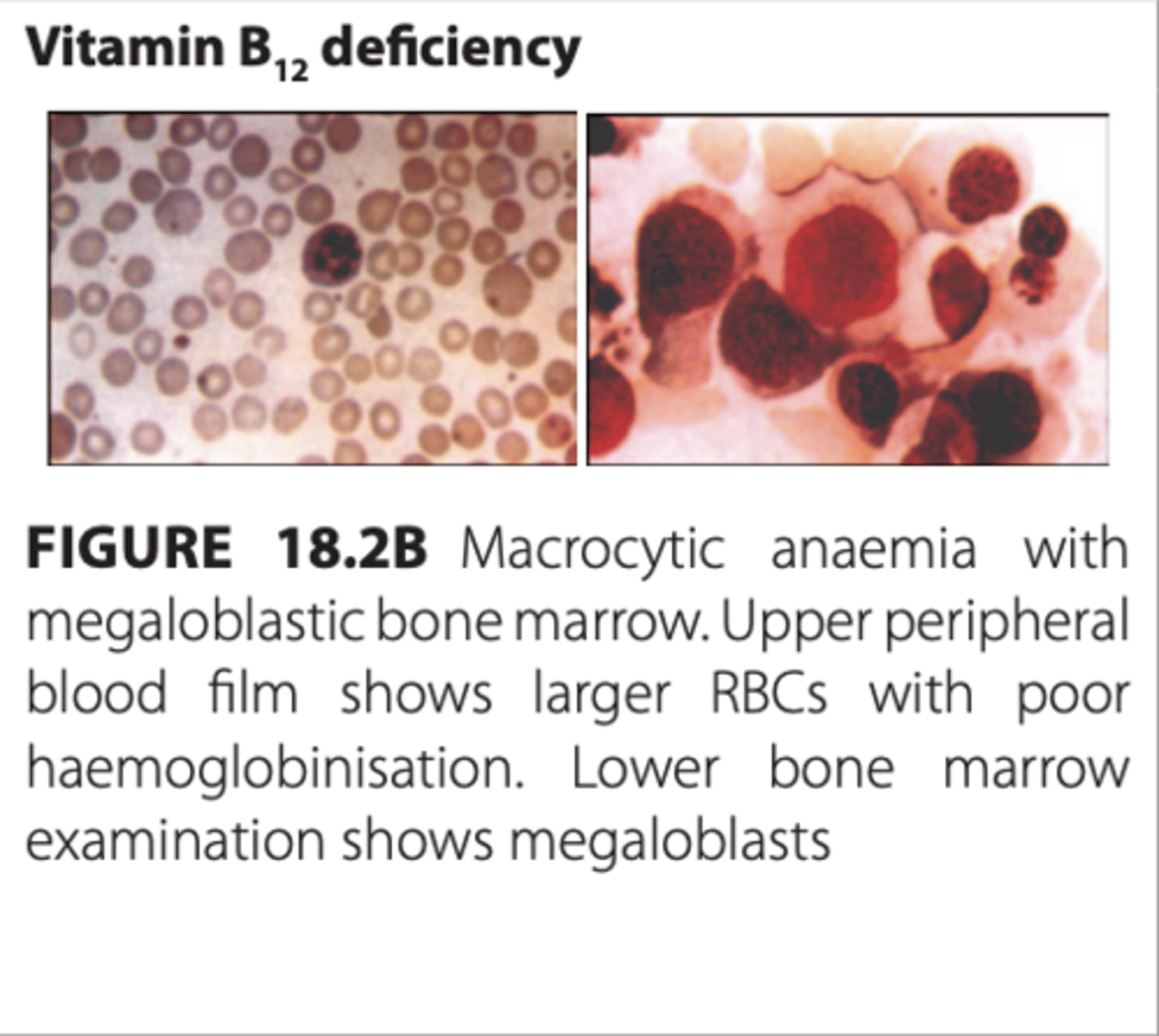
What are the features of vitamin B12 deficiency anaemia?
1. Mild jaundice, lemon-yellow skin, grey hair
2. Red, smooth, sore tongue
3. Tingling, paresthesias, abnormal gait
4. Neurological and mental changes (poor memory, depression, hallucinations)
5. Macrocytic RBCs; megaloblastic bone marrow
What would you expect Vitamin B12 deficiency to look like on a peripheral blood film?
Causes of Vitamin B12 deficiency?
1. Poor dietary intake (vegetarian)
2. Malabsorption (diarrhea)
3. Autoimmune gastritis → loss of intrinsic factor
4. Gastrectomy
What are the features of folic acid deficiency anaemia?
-Similar to B12 deficiency except no neurological features
-Macrocytic RBCs, megaloblastic bone marrow
Causes of folic acid deficiency anemia?
1. Increased demand (pregnancy)
2. Poor intake (low green vegetables)
3. Malabsorption
4. Infection
5. Haemolytic anaemia
What are the features of haemolytic anaemia?
-Symptoms/signs of anaemia
-Mild jaundice, dark urine/stool (hemoglobinuria)
-Abnormal facies (frontal bossing), skin ulcers (sickle cell)
-Hepatosplenomegaly
-Pigmented gallstones
What would you expect Haemolytic Anaemia to look like on a peripheral blood smear?
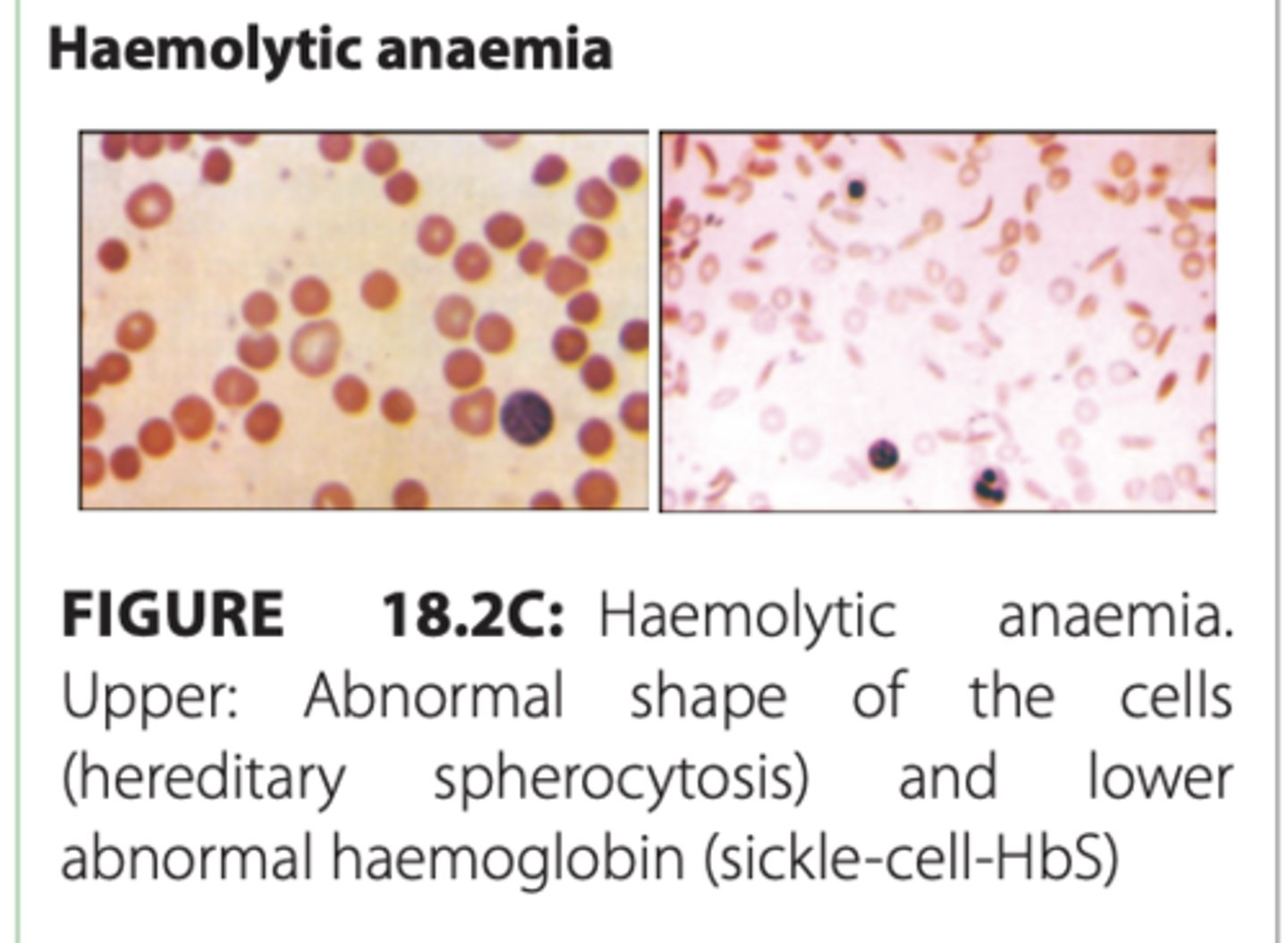
Causes of Haemolytic anemia?
-Congenital/hereditary (spherocytosis, thalassemia, G6PD deficiency)
-Drug-induced (analgesics, antimalarials, antibiotics)
-Autoimmune
Infection (e.g., malaria)
What are the features of hypoplastic or aplastic anaemia?
-Symptoms/signs of anaemia
-Neutropenia → infections, necrotic mouth/throat ulcers
-Thrombocytopenia → bleeding (skin, mucous membranes, epistaxis, haematuria, intracranial bleed)
-Bone marrow: mostly fat and fibrosis, very few hematopoietic cells
What would you expect hypoplastic or aplastic anemia to look like on a peripheral blood smear?
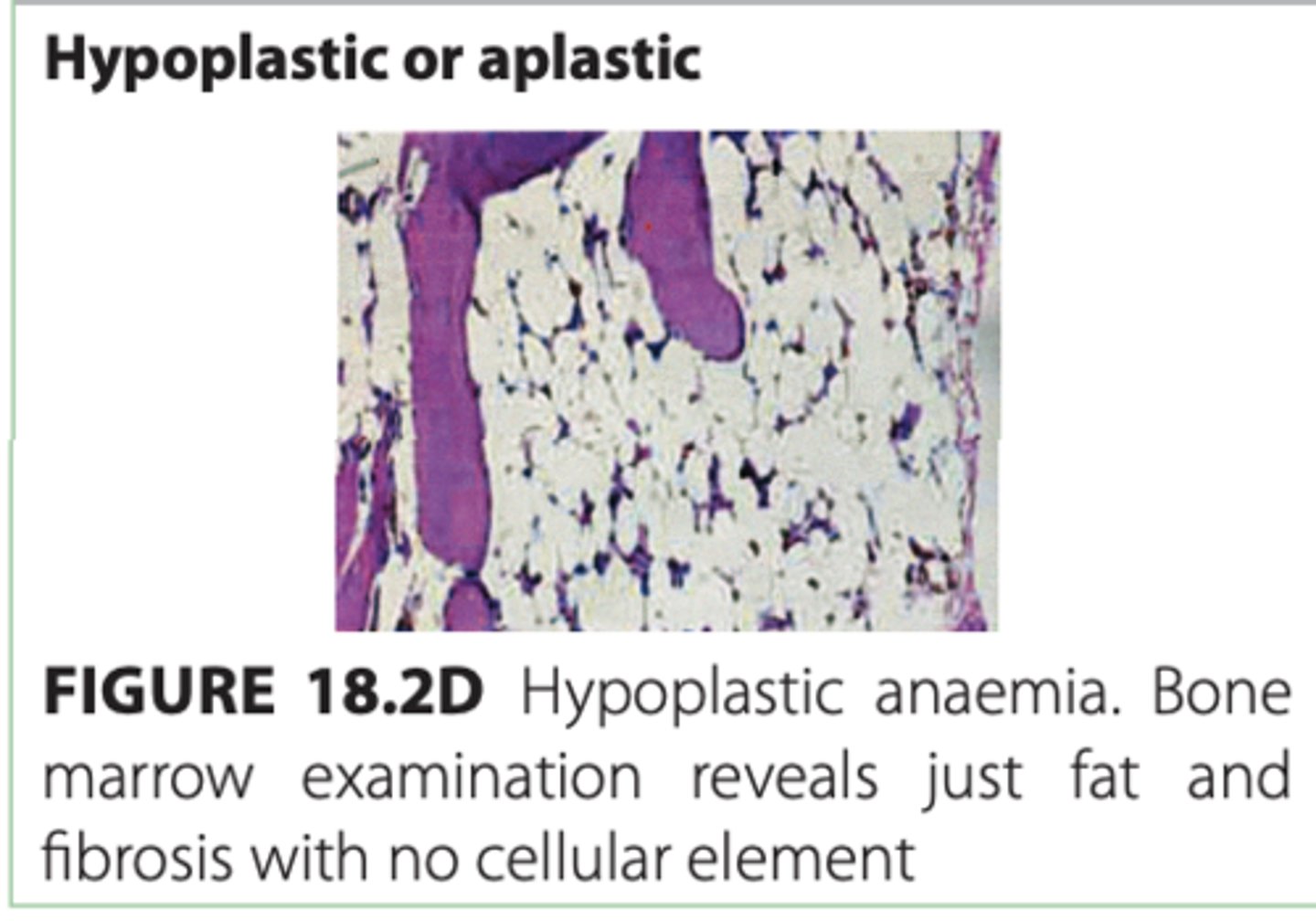
Causes of hypoplastic or aplastic anemia?
-Irradiation, drugs, chemicals
-Infection
-Autoimmune disease
What infections are neutropenic patients at highest risk for?
Neutropenia = a lower-than-normal number of neutrophils in the blood (neutrophils are a type of white blood cell that fight bacterial and fungal infections)
Bacterial infections; opportunistic infections like fungi and viruses (HSV, VZV) can occur too
What infections are lymphopenic patients more prone to?
Lymphopenic (or lymphocytopenia) = having an abnormally low number of lymphocytes in the blood
Viral and atypical infections (e.g., Pneumocystis jirovecii, Toxoplasma)
Common presenting symptoms of neutropenia?
Fever, sore throat, mouth ulceration, anal ulcers, skin infections; may progress to septic shock if untreated
What is the clinical course if neutropenia is untreated during infection?
Rapid progression to septicemia and shock within hours
Define leucocytosis
Total WBC >11,000/µL, often due to an increase in one WBC type (neutrophils, lymphocytes, eosinophils, basophils, monocytes)
What is neutrophilic leucocytosis?
Increase in neutrophils, usually a normal response to infection or injury
What is a Leukemoid reaction?
Leukemoid reaction = a marked, temporary increase in white blood cells (WBCs) that mimics leukemia, but is not cancer
What are common causes of a leukaemoid reaction?
-Severe infection
-Tuberculosis
-Malignant infiltration of bone marrow
-Occasionally, severe hemorrhage or hemolysis
What is leucoerythroblastic anaemia?
Presence of nucleated red cells and WBC precursors in peripheral blood, often due to marrow infiltration or severe anemia
Causes of leucoerythroblastic anaemia?
-Marrow infiltration (metastatic carcinoma, myelofibrosis, osteopetrosis)
-Myeloma
-Lymphoma
-Severe hemolytic or megaloblastic anemia
Define leukaemias (aka leukemia)
Malignant disorders of myeloid or lymphoid cells, characterized by proliferation or defective apoptosis, infiltrating blood, bone marrow, and tissues
Leukemias = cancers of the blood-forming cells in the bone marrow
How do acute vs chronic leukemias differ?
Acute: Immature cells, rapid progression, aggressive
Chronic: Mature/differentiated cells, slow progression, indolent
What is multiple myeloma?
Malignant proliferation of clonal plasma cells, producing a monoclonal paraprotein in serum
Multiple myeloma = a cancer of plasma cells (a type of white blood cell that normally makes antibodies)
Key lab finding in multiple myeloma?
Monoclonal dark-staining band on serum protein electrophoresis
Pathophysiology of bone disease in multiple myeloma?
Plasma cells secrete cytokines → osteoclast activation → lytic bone lesions, bone pain, fractures, hypercalcemia
Common complications of multiple myeloma?
-Anemia/pancytopenia (bone marrow involvement)
-Hypercalcemia
-Renal failure
-Bone lesions and fractures
-Soft tissue infiltration is rare
Age group commonly affected by multiple myeloma?
Older adults; may present as solitary plasmacytoma of bone or extramedullary plasmacytoma
What is Polycythaemia
Polycythaemia is a condition characterized by an increase in the concentration of red blood cells (RBCs) in the blood, which leads to increased hemoglobin and hematocrit (packed cell volume, PCV). This can make the blood thicker and increase the risk of clots
What are the two main types of polycythaemia?
1. Relative (apparent) – due to reduced plasma volume (dehydration, diuretics, alcohol)
2. True (absolute) – actual increase in RBC mass
What is polycythaemia rubra vera (PRV)?
A myeloproliferative disorder of the bone marrow causing true polycythaemia
What are secondary causes of true polycythaemia?
1. Chronic hypoxemia (COPD, congenital heart disease) → ↑ erythropoietin
2. Tumors causing inappropriate erythropoietin (renal, lung tumors)
Common early signs of polycythaemia?
-Red complexion / plethora
-Headache, tinnitus, feeling of fullness in the head
-Often noticed by friends/family
Symptoms specific to polycythaemia rubra vera?
-Pruritus (esp. after hot bath)
-Gout (high red cell turnover)
-Hepatosplenomegaly
-Thrombotic episodes due to high platelet count
-Paradoxical bleeding tendency
Complications of high hematocrit in polycythaemia?
Increased risk of:
-Heart attack
-Stroke
-Peripheral vascular disease
When hematocrit (the % of blood made up of red blood cells) is too high in polycythaemia, the blood becomes thicker, which can slow flow and cause clots
What type of lymphadenopathy is commonly seen in hematologic malignancies? (cancer of blood, bone marrow, or lymphatic system)
-Usually painless
-Often generalized
-Frequently associated with hepatosplenomegaly and other systemic manifestations
Describe lymph node involvement in lymphocytic leukemia.
-Diffusely enlarged
-Firm, discrete, painless
-Commonly involves cervical, axillary, and inguinal regions
Describe lymph nodes in Hodgkin’s lymphoma.
-Painless
-Discrete
-Rubbery consistency
What systemic “B symptoms” may accompany lymphadenopathy in hematologic malignancy?
-Weight loss
-Fever
-Night sweats (drenching)
What is Hodgkin's lymphoma?
A cancer of the lymphatic system (the nodes and immune tissue).
Usually shows up as a painless swelling of lymph nodes, often in the neck.
Key feature: presence of Reed-Sternberg cells (a specific type of abnormal cell seen on biopsy).
Can cause B symptoms: fever, night sweats, and unexplained weight loss.
Often starts in one group of lymph nodes and spreads in an orderly way
Treatment: usually chemotherapy and/or radiation
Describe lymph nodes in non-Hodgkin’s lymphoma.
-Firm
-Painless
-Often associated with systemic symptoms, extranodal involvement (bone, brain, skin)
-May cause compression symptoms (gut obstruction, ascites, SVC obstruction, spinal cord compression)
Difference between Non-Hodgkin's and Hodgkin's lymphoma
Hodgkin lymphoma is a cancer of the lymphatic system characterized by Reed-Sternberg cells, usually starts in one lymph node group and spreads in an orderly fashion, often causing painless lymph node swelling and B symptoms like fever, night sweats, and weight loss. Non-Hodgkin lymphoma also involves lymphocytes but does not have Reed-Sternberg cells, can start in multiple lymph nodes or extranodal sites and spread randomly, and its symptoms and aggressiveness vary depending on the subtype. Hodgkin lymphoma generally has a better prognosis and is highly treatable, while non-Hodgkin lymphoma’s outlook depends on the specific type and aggressiveness
Key distinguishing feature between Hodgkin and non-Hodgkin lymphomas on physical exam?
Hodgkin: rubbery, discrete nodes
Non-Hodgkin: firm nodes with systemic/extranodal involvement
What are the primary functions of the spleen?
-Clears bacteria and particulates from blood
-Generates immune responses to pathogens
-Reticuloendothelial activity: destroys RBCs and other formed elements
-Extramedullary erythropoiesis when bone marrow is insufficient
Why does splenomegaly occur in hematologic disorders?
-Enlargement occurs when the spleen’s normal functions are exaggerated:
-Excess clearance of blood cells (e.g., hemolytic anemias)
-Immune stimulation (e.g., infections, autoimmune diseases)
-Extramedullary hematopoiesis (e.g., myeloproliferative disorders)
What does hepatosplenomegaly indicate?
: Involvement of both liver and spleen suggests systemic hematologic or infiltrative disease, e.g., leukemia, lymphoma, storage disorders, myeloproliferative disorders
How does extramedullary erythropoiesis contribute to splenomegaly?
Extramedullary erythropoiesis (EME) is when the body makes red blood cells outside of the bone marrow, usually in organs like the liver and spleen
When the bone marrow cannot meet RBC demand, the spleen resumes its fetal hematopoietic function, producing RBCs and enlarging in the process
What are common symptoms of splenomegaly?
-Abdominal discomfort or dragging sensation from the mass
-Acute enlargement → pain due to stretching of the capsule
-Back pain and bloating from stomach compression
-Colicky pain radiating to left shoulder tip (splenic infarct/perisplenitis), seen in myeloproliferative disorders and sickle cell anemia
-Rupture (trauma or infiltrative disease) → intraperitoneal bleeding, shock, possibly painless
Is a palpable spleen always indicative of disease?
No. Spleen must enlarge 2–3× normal size to be palpable. In some tropical regions, asymptomatic splenomegaly is common in healthy individuals
What is the significance of spleen tip descent on deep inspiration?
Indicates palpable splenomegaly, helping differentiate from normal anatomy
In simple terms:
Normally, the spleen is tucked under the rib cage and usually can’t be felt.
During deep inspiration, the diaphragm moves down, sometimes allowing the spleen tip to be felt if it’s enlarged.
Significance: If you can feel the spleen tip, it suggests splenomegaly rather than just normal anatomy
Ask the patient to take a deep breath when palpating the left upper quadrant to help detect an enlarged spleen
What are the two main types of bleeding causes?
1. Local/structural defects – e.g., trauma, peptic ulcer, vascular malformations
2. Haemostatic failure – problems with vessel wall, platelets, or coagulation factors
What is primary haemostatic failure?
Bleeding due to vessel wall abnormalities or platelet defects (quantitative or qualitative). Examples: thrombocytopenia, thrombasthenia, von Willebrand disease
What is secondary haemostatic failure?
Bleeding due to coagulation factor deficiency (e.g., hemophilia) or excessive fibrinolysis (e.g., after tPA or streptokinase therapy)
How can the site of bleeding help differentiate causes?
-Muscle/joint bleeding (hemarthrosis): coagulation defect
-Purpura, epistaxis, GI bleed, menorrhagia: platelet disorder or primary hemostatic failure
-Recurrent bleeding at a single site: local structural abnormality (e.g., Osler-Weber-Rendu disease)
-Spontaneous bruising in elderly with normal labs: senile purpura
Why is the history of bleeding after minor stress important?
Recurrent bleeding after dental extraction, surgery, or childbirth suggests an underlying haemostatic defect rather than a local anatomical cause
What does the duration of bleeding history suggest?
Long-standing bleeding indicates a congenital disorder (e.g., hemophilia), whereas recent onset suggests an acquired disorder
What is the significance of precipitating factors in bleeding?
Spontaneous bleeding suggests a severe hemostatic defect, whereas bleeding only after trauma is usually milder or situational
Why is a surgical history important in bleeding evaluation?
Bleeding after procedures (dental extraction, tonsillectomy, circumcision) tests the hemostatic system:
-Immediate post-op bleeding: defective platelet plug formation
-Delayed bleeding (hours later): defect in coagulation/fibrin stabilization
How does family history contribute to diagnosis?
A history of excessive bleeding in relatives may indicate inherited bleeding or coagulation disorders. Lack of family history does not exclude congenital disease
Why assess for systemic illness in bleeding patients?
Bleeding from multiple sites without trauma or surgery may indicate systemic disorders:
-Liver or renal failure
-Paraproteinaemia
-Connective tissue disorders
How can drugs cause bleeding?
By:
1. Depressing bone marrow → thrombocytopenia
2. Interfering with coagulation factors (e.g., warfarin)
3. Inhibiting platelet function (e.g., NSAIDs)
Why is occupation relevant in bleeding assessment?
Exposure to chemicals or toxins can cause thrombocytopenia or other hemostatic defects
What are common presenting features of thrombosis (formation of a blood clot (thrombus) inside a blood vessel that blocks or slows blood flow)?
Arterial or venous thrombosis may present with:
-Swelling of one or both legs (DVT)
-Pain, warmth, and redness
-Dilated superficial veins
What is pancytopenia?
A combination of anemia, leukopenia, and thrombocytopenia
Causes of pancytopenia with hypocellular or acellular marrow?
Due to reduced production of blood cells from bone marrow suppression or infiltration (e.g., aplastic anemia, chemotherapy, marrow infiltration)
Causes of pancytopenia with hypercellular marrow?
Due to peripheral destruction or splenic sequestration of mature cells (e.g., hypersplenism, autoimmune hemolysis)
How do patients with pancytopenia present clinically?
Symptoms include:
1. Acute infections (from leukopenia)
2. Bleeding (from thrombocytopenia)
3. Signs and symptoms of anemia (fatigue, pallor, dyspnea)
Pallor on general inspection suggests what?
Anemia
Plethoric (reddish) facies indicates what condition?
Polycythaemia
Frontal bossing and "hair-on-end" appearance suggest?
Thalassaemia
Emaciated appearance in a hematologic patient suggests?
Chronic anemia, malnutrition, or malignancy
emaciated (very thin, wasted) appearance