L4: Bipolar disorders
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
What are mood disorders? - definition
mental health conditions in which the principle feature is prolonged, intense, pervasive affective disturbance
What are mood disorders? - 2 types
unipolar = includes only depressive episodes
bipolar = both manic and hypomanic and depressive episodes
Are depressive and manic episodes 2 ends of the same spectrum?
individually conceptualised as dichotomous ‘highs’ and ‘lows’ BUT
one can cycle rapidly between depressive and manic symptoms within the same episode (mixed episode)
Symptoms are Not the ‘opposite’ of each other
Bipolar I disorder: DSM5 diagnostic criteria
A - criteria have been met for at least one manic episode
B - presentation is not better explain by Schizophrenia- spectrum disorder
Bipolar II disorder: DSM5 diagnostic criteria
A - criteria have been met for at least 1 hypomanic episode, and at least one major depressive episode
B - there has never been a manic episode
C - presentation is not better explained by Schizophrenia disorder
D - symptoms of depression/unpredictability caused by mood alternation causes clinically significant distress/impairment in functioning
Key diagnostic differences between Bipolar I and II - bipolar one the person typically experiences:
full blown mania, with very marked functional impairment
Depressive symptoms which may - or may not - meet the threshold for MDD
Key diagnostic differences between Bipolar I and II - bipolar II the person typically experiences:
hypomania but symptoms are below the threshold for full blown mania, which less marked functional impairment
Depressive symptoms which meet criteria for major depression
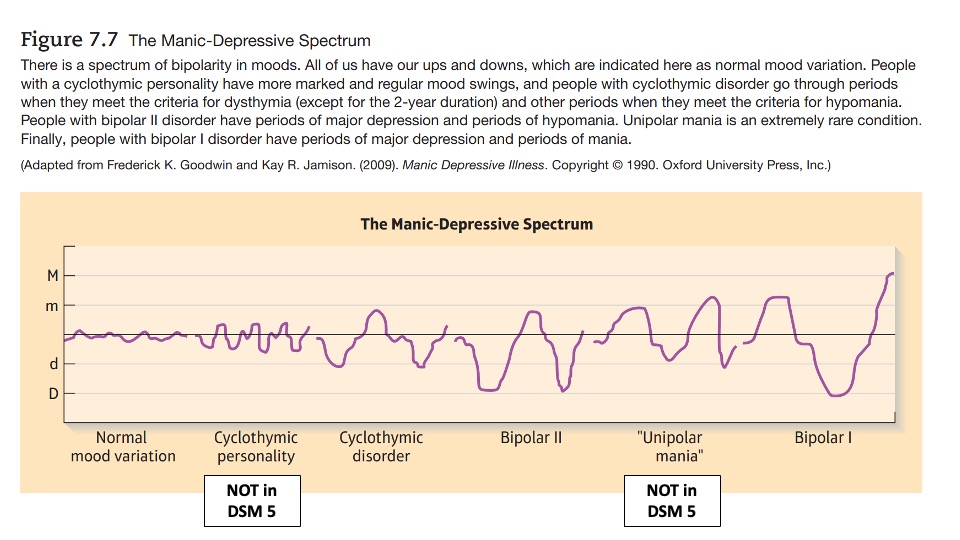
What other bipolar - type disorder exists ? - Cyclothymic disorder
cyclical mood changes less severe than seen in bipolar disorders
numerous periods of depressive then hypomanic symptoms for less than 2 years
No period of mood stability lasting longer than 2 months
Has never met the criteria for a full mania, hypomanic or depressive episode
Cause sig functional impairment
Image on the patterns of mood variation of the manic-depressive spectrum
Are depressive symptoms qualitatively or quantitively similar in MDD and bipolar II - in bipolar II depressive episodes are more
servere, and frequent, cause more role impairment
shorter
more frequently have psychotic features and psychomotor difficulties, substance use and mood lability as associated factors
Are depressive symptoms qualitatively or quantitively similar in MDD and bipolar II - in MDD depressive episodes are more
are accompanied by higher levels of anxiety, agitation, insomnia, physical symptoms and weight loss
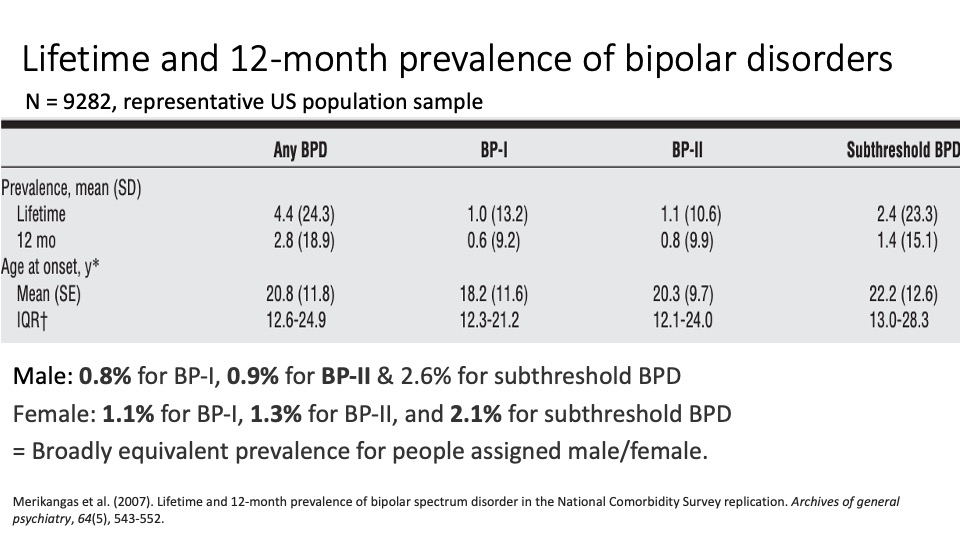
lifetime and 12 month prevalence of bipolar disorders
male - 0.8% for BP1, 0.9% for BP11 and 2.6% for sub threshold BP
Female - 1.1% for bp1, 1.3% for bp2 and 2.1% for sub threshold BPD
broadly equivalent for men and women
Global prevalence of bipolar disorders
Africa - 0.1-1.83%
Europe - 0.6-6.2%
Worldwide - 1% for b1 , and 1.5% for bipolar 2
Epidemiology of bipolar disorder
prevalence does not appear to vary with ethnicity
Evidence mixed on whether type 1 or 2 has greater prevalence: indication that 2 is more common
40% of people with MDD experience subclinical hypomanic symptoms, suggesting more heterogeneity in the MDD category than initially thought
if a person is untreated, episodes of bipolar -related mania can last 3-6 months
episodes of depression last 6-12 months
Age of onset - trimodal
onset has 3 peaks (trimodal), some argue that there is a peak In each life phase
Prodromal symptoms of bipolar disorder - Faedda et al (2015) - method
reviewed 25 papers with prospective and retrospective designs to look at what ‘comes before’ bipolar diagnosis’s
Prodromal symptoms of bipolar disorder - Faedda et al (2015) - Prodormal features were
mood lability
subliminal hypomania/deppresion
Other specified bipolar related disorders
Major depression, especially with hypomanic or psychotic symptoms
Prodromal symptoms of bipolar disorder - another review noted that
specific prodromal neurocognitive impairments in verbal memory, attention and executive functions but no decrement to general intelligence
Clinical course of bipolar disorder - Gignac et al (2015) - reviewed outcomes of 1st mania
syndromal recovery rates were 77% at 6 months and 84% at 1 year
recurrence was 26% with 6 months, 41% by 1 year and 60% by 4 years
younger age at first episode was associated with risk of recurrence after 1 year
Clinical course of bipolar - b2 - Vieta and Suppess (2008)
greater number of total mood episodes than B1
Shorter duration of mood episodes
More persistent depression
Less chance of psychosis or hospitalisation
Low rates of cross over to bipolar 1
clinical course of bipolar - Judd et al - followed cohort of people w B1 across 13 years
patients has symptoms for 48% of weeks
Depressive symtoms (32%) were common than manic/hypomanic symptoms (9%) or cycling/mixed symptoms (6%)
Minor depressive, and hypomanic symtoms combined were more frequent than major depressive and manic symptoms (30% vs 11)(
clinical course of bipolar - Judd et al - followed cohort of people w B1 across 13 years - conclusions
the longitudinal weekly symptomatic course of bipolar 1 disorder appear chronic. More time is spent depressed than manic, and subsyndromal symptoms predominate
Clinical course for bipolar II disorder - Judd et al, longitudinal study across 13 years
p’s had symptoms for 54% of weeks
Depressive symptoms (50%) were more common than manic/hypomanic symptoms (1%) or cycling/mixed symptoms (2%)
Minor depressive, and hypomanic symptoms combined were 3x more frequent than major depressive and manic symptoms (40% vs 13%)
Clinical course for bipolar II disorder - Judd et al, longitudinal study across 13 years - conclusion
the longitudinal weekly symptomatic course of B2 disorder is chronic and overwhelmingly dominated by depressive symptoms. As w bipolar I subsyndromal symptoms predominate
The brain in bipolar disorder - what is default mode network
default mode network: brain activity when a person is restfully awake
includes contemplation, remembering, thinking of others and planning for the future…. internal narrative
The brain in bipolar disorder - how is the Default Mode network involved
DMN activity inversely correlated with other networks such as attention and memory performance
DMN activity is different in bipolar disorder compared to controls : patterns of hypo and hyper connectivity
Pattern of interaction between network may themselves differ in bipolar…. need more research
The brain and b bipolar disorder: distinguishing between unipolar and bipolar depression - key structural differences:
Lower volume in anterior cingulate cortex for U
Lower volume in hippocampus and amygdala in B
Lower white matter integrity in B
The brain and b bipolar disorder: distinguishing between unipolar and bipolar depression - key functional differences: emotional stimuli
more activation in the amygdala in unipolar towards neg emotional stumili
Less activation in the amygdala in unipolar towards positive emotional stimuli
The brain and b bipolar disorder: distinguishing between unipolar and bipolar depression - key functional differences: DM network
failure to activate the default mode during cognitive tasks greater for bipolar
Stronger functional connectivity in bipolar for the default mode network
Stronger functional connectivity in bipolar in prefrontal cortex, anterior Cingular cortex, parietal and temporal regions and thalamus
Cogntion and bipolar disorder
impairments in attention, verbal learning and memory and executive functions
some experience cognitive decline across the course but others resume usual levels
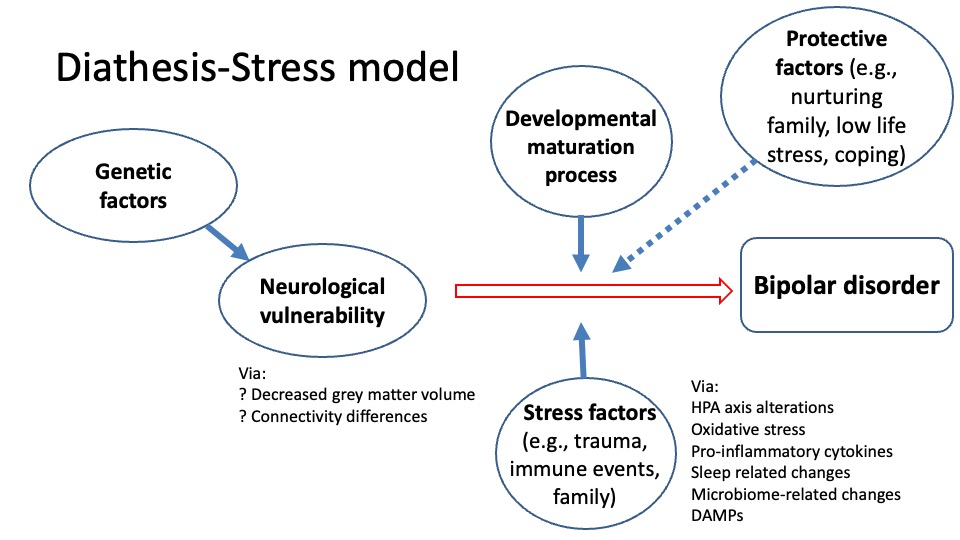
Genetics and bipolar disorder
MZ concordance rate of 40-70%
First degree relatives have 5-10% risk - 7 x higher than general population
relatives more likely to develop unipolar depression than bipolar, suggest genetic risk transcends mood disorders
Also shared genetic risk between diagnoses of bipolar and depression
risk is polygenic =
multiple single nucleotide polymophisms, which are highly prevalent in the general population and confer a small increased risk induvidually
Polygenic risk scores
Genetic variants (SNPs) affecting 100s loci are found more frequently in groups of people with a given condition
enables a statistical estimate of how a person’s variants affect their risk of developing it.
A polygenic risk score:
“ An individuals relative risk of a specific condition based on the collective influence of many genetic variants compared to someone without the variants (a control) “
Socioenvrionmental risk factors of bipolar disorder
childhood trauma and abuse (especially emotional)
childhood adversity and neglect
childbirth
substance misuse (especially opioids)
canabis and cocaine use (predict onset of mania)
some other medical conditions e.g. asthma,IBS(suggest shared autoimmune pathway)
bipolar and the immune system - fries et al (2019)
consider how evidence of epigenetic in bipolar disorder can be squared with its high heritability
suggest that findings of consistent immune-related epigenetic alterations in people with bipolar may demonstrate how immune dysfunction is transmitted across generations
Diathesis stress for bipolar
Treatment for bipolar disorder - different mood stabilisers used for
different mood phases of bipolar disorder. lithium is used in both phases
Treatment for bipolar disorder - treatment timings
pharmacological and psychological treatment in early illness is more effective than later stages in terms of response, relapse rate, time to recurrence, symptomatic relief, remission, psychosocial functioning and employment
The role of lithium in mood stabilisation
lithium carbonate is used to help with both hypomanic and manic and depressed phases as a long term treatment
unknown how it woks, we do know it reduced norepinephrine levels, increases serotonin synthesis and has some anti-inflammatory actions
Possible routes include changes to levels and properties of glutamate, GABA, dopamine and neurotrophic factors
Treating depressive episodes in bipolar disorder - SSRI’s should not be
prescribed on their own as they can worsen mania and hypomania, should be combined with olanzapne or another antipsychotic
Treating depressive episodes in bipolar disorder - SSRI’s should not be - however
balance of risk and benefit may shift for people with B2, who how no evidence of hypomania with low dose antidepressants: in this case, an SSRI on its own may be merited
Distinguishing MDD from Bipolar at first presentation with depressive symptoms - markers of bipolar can include
easier age at onset of illness
hyperhagia, hyperwsommnia, and psychosis
higher frequency of affective episodes
Comorbid substance use disorders, anxiety disorders, binge eating disorders and migranes
Family history of psychopathy
Distinguishing MDD from Bipolar at first presentation with depressive symptoms - markers of bipolar can include - if decide to administer antidepressants need to be careful of
insufficient response
amplification of anxiety, dysphoria and mood instability
Psychological treatment for bipolar disorder - normally trialed as adjunctive therapies (alongside meds)
a systematic review of 39 trails found that, in comparison to medication alone, psychological treatments reduce episodic recurrence. some therapies also stabilise depressive symptoms
sychological treatment for bipolar disorder - commonly used approaches
CBT
Psychoeducation
Family therapy
Similarities of bipolar and Schizophrenia
share polygenetic risk
Show cogntive, neurological and functional progression without effective treatment
Feature similar symptoms
Show prodromal symptoms, before initial onset and also before relapse