BME 260 Final Exam Bio
1/368
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
369 Terms
bone cells osteocyte
mature bone cells that make up the majority of the bone cell population
a single osteocyte occupies a
lacuna (a pocket surrounded by two different layers of bone matrix termed lamellae)
osteocytes do not
divide
narrow passageways, termed canaliculi, penetrate through the
lamellae, connecting lacunae providing a communication pathway between osteocytes
cytoplasmic extensions of osteocytes fill the canaliculi
osteocytes maintain the
protein/mineral content of surrounding bone matrix and play a role in bone repair
bone cells- osteoblast
produce new bone matrix in a process termed ossification or osteogenesis
the matrix that is produced by osteoblasts is not
crystalized by calcium or other minerals upon release
at this point, the bone matrix is termed osteoid
osteoblasts release a significant amount of
calcium, above its solubility limit, to help initiate calcium deposition within osteoid
osteoblasts differentiate into
osteocytes if they become completely surrounded by bone matrix
bone cells- osteoprogenitor cell
bone contains small numbers of these mesenchymal cells
osteoprogenitor cell differentiates into
osteoblasts
osteoprogenitor cell play an important role in
fracture healing responses
osteoprogenitor cells are found on
all exterior surfaces of bone (ex. facing the marrow cavity and the outer surface of a long bone)
bone cells- osteoclast
cells that absorb and remove bone matrix
very large cells that are multinucleated
osteoclasts are more
similar to macrophages than other bone cells
osteoclasts secrete these to dissolve the matrix and release the minerals found in the bone matrix
acids and proteolytic enzymes
this process is termed osteolysis (or resorption)
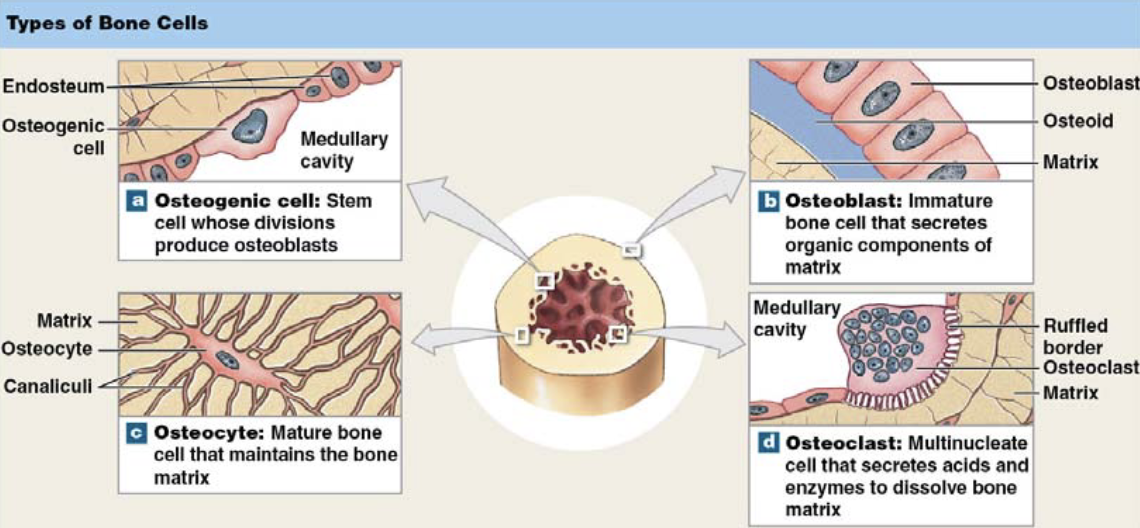
in living bone, osteoblasts and osteoclasts are both
active; the balance of these two processes determine if new bone is formed, old bone is removed or there is no net change
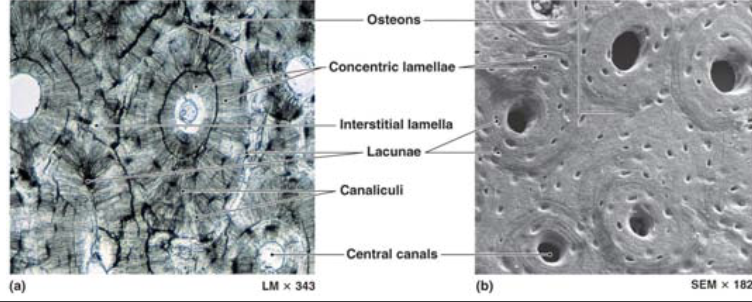
the functional unit of compact bone is the
osteon (or Haversian canal system)
osteocytes are arranged in
concentric circles surrounding a central canal, which contains blood vessels (normally a capillary and a small venule)
these lamellae form a bulls-eye like pattern
perforating canals (volkmann canals) are
the passageways for blood vessels to enter the bone
in spongy bone
the lamellae are not arranged in the osteon structure
thin trabecular divide and converge in a
seemingly “random” pattern
spongy bone is typically found where
stresses arise from multiple directions
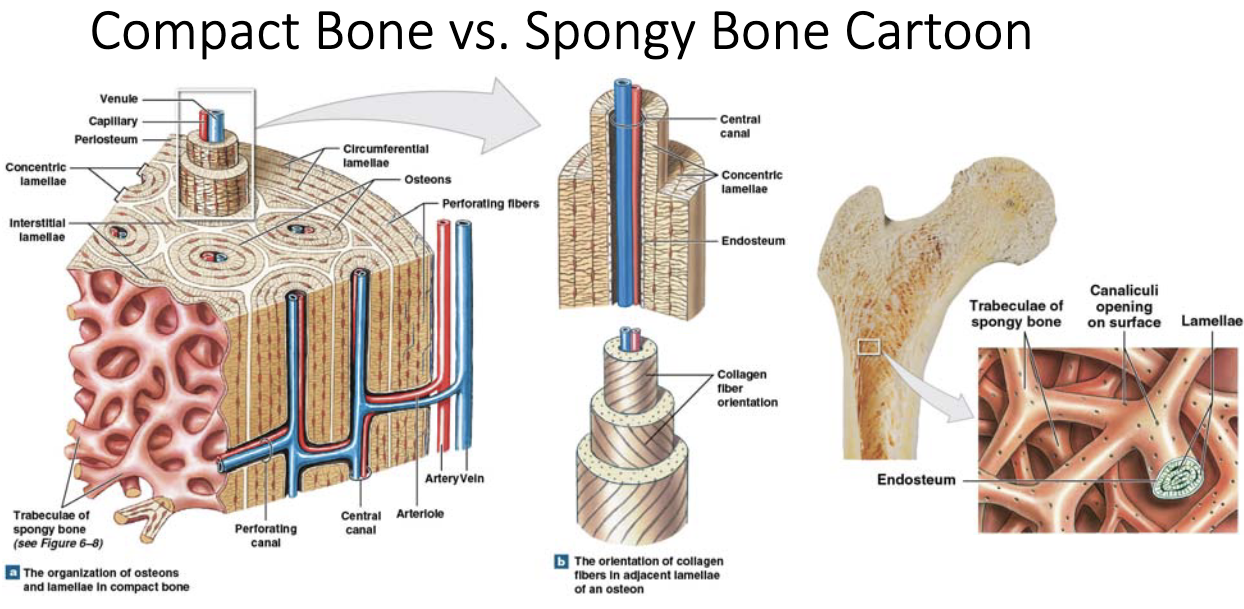
the role of spongy bone is to
reorient those stresses to a more uniform direction (compact bone handles the stresses in a more uniform direction)
red bone marrow is found between
trabeculae of long bones; some spongy bone may contain yellow bone marrow
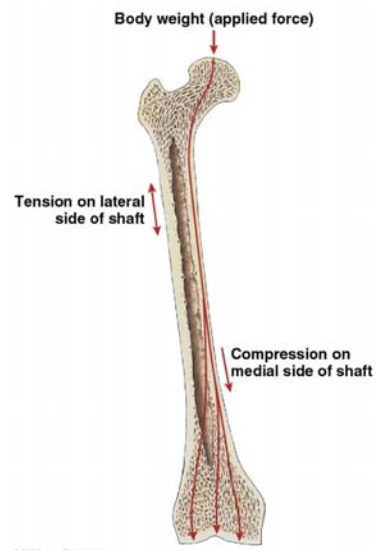
the epiphysis (which is composed of spongy bone)
transfer forces from many directions to the diaphysis
the compact bone must withstand both
tensile and compressive forces if the load is off-center
assuming a non-rigid body
wolff’s law tries to quantify the
loading condition on bone and the remodeling of the bone (ex. a tennis player will have different bone mechanical properties in their playing arm vs. their non playing arm)
axial skeleton
composed of 80 bones
skull
8 cranial bones + 14 facial bones
6 auditory bones + the hyoid bone
vertebral column
24 vertebrate +sacrum +coccyx
thoracic cage
24 ribs + sternum
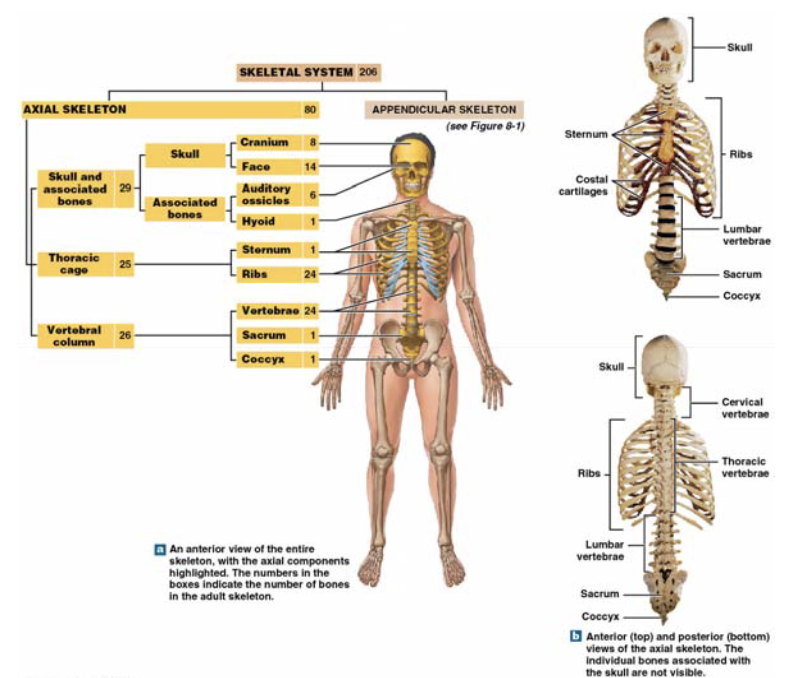
axial skeleton protects
the brain, spinal cord, and thoracic/abdominal organs
extensive surface for muscle attachment
helps with respiration
stabilize the appendicular skeleton
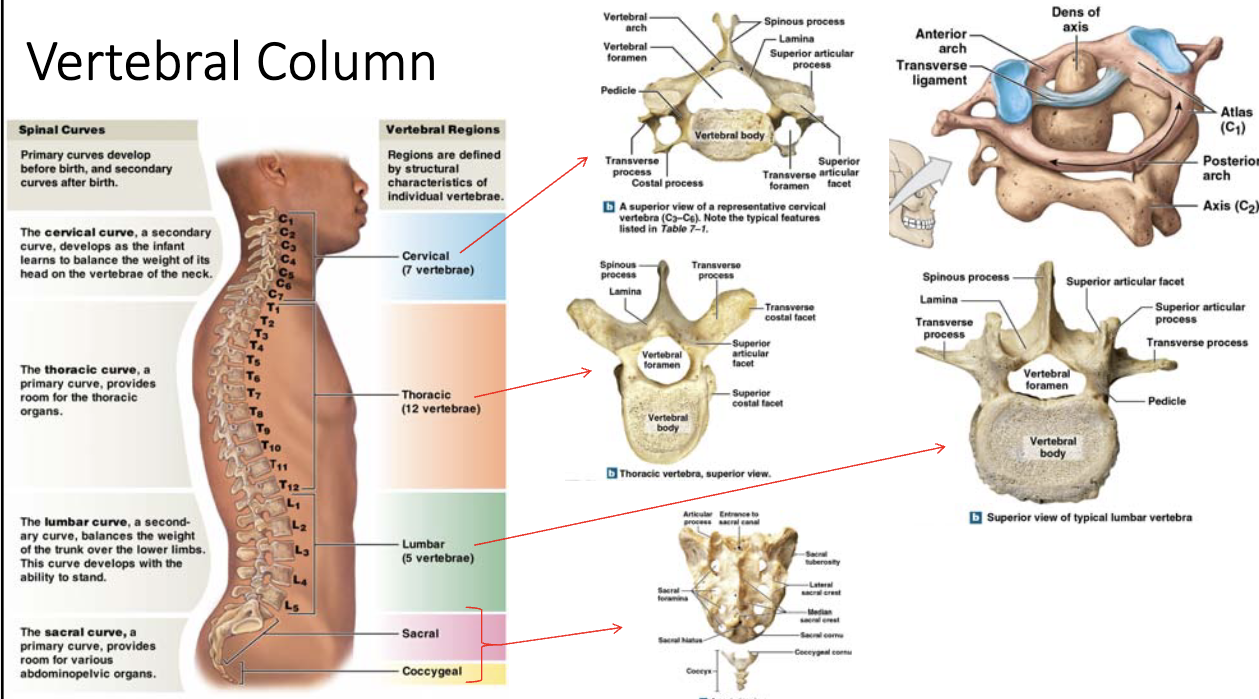
vertebrae
7 cervical vertebrae (compose the neck)
12 thoracic vertebrae (articulates with the ribs)
5 lumbar vertebrae (strength and articulates with the sacrum)
sacrum, composed of fused sacral vertebrae-begin to fuse after puberty
coccyx, composed of ~4 fused coccygeal vertebrae-begin to fuse around age of 25
cervical vertebrae
the atlas (C1) holds up the head and axis (C2) which provides a pivot for the head
lumbar vertebrae
largest of the vertebrae, withstand a significant portion of the weight
sacrum
protects reproductive, digestive, and urinary organs
coccyx
attachment site for multiple muscles/ligaments
appendicular skeleton
composed of 126 bones
pectoral girdle
2 clavicles + 2 scapula
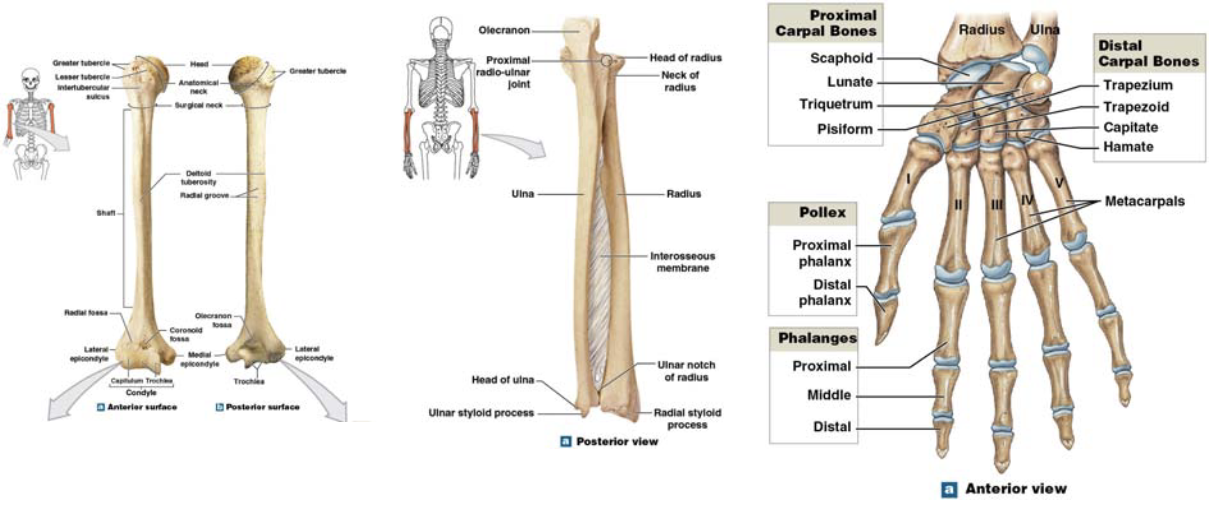
upper limbs
60; humerus, radius, ulna, carpal bones, metacarpal bones, phalanges
pelvic girdle
2 hip bones
lower limbs
60; femur, tibia, fibula, patella, tarsal bones, metatarsals bones, phalanges
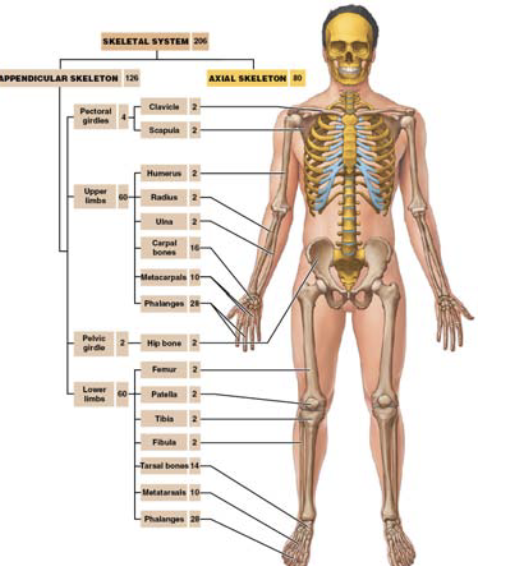
the appendicular skeleton allows you to
manipulate the/interact with the environment
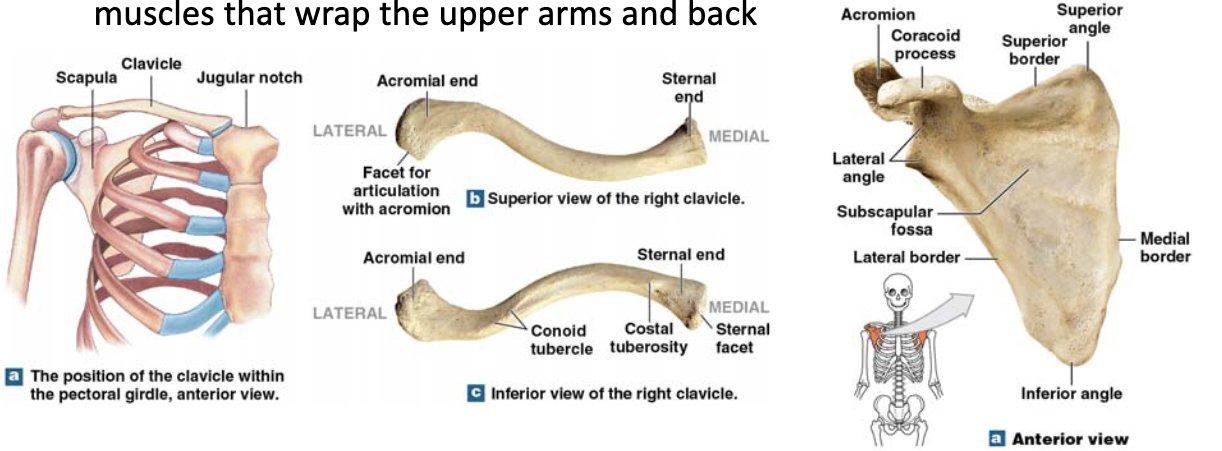
pectoral girdle helps
to anchor the arms to the axial skeleton, attachment site of muscle that wrap the upper arms and back
upper limb adapted for
manipulation/interaction with the environment
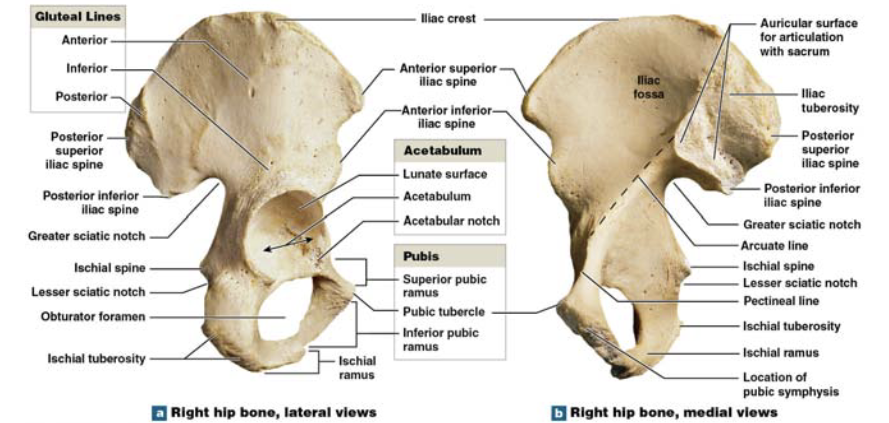
pelvic girdle attach to
lower limbs, involved in weight bearing
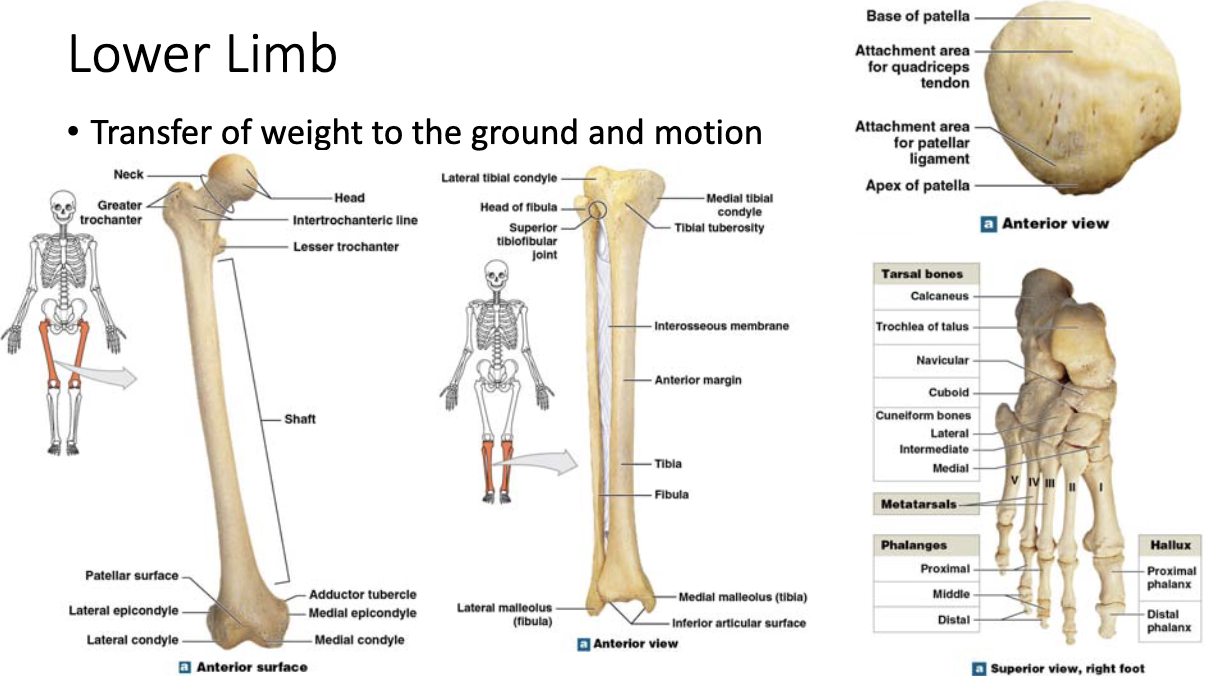
lower limb transfer
of weight to the ground and motion
movement can only occur at
joints (or articulations)
joints are the locations where
two (or more) bones meet
remember bones are relatively inflexible
the stricture of the joint determines
the type and amount of movement that may take place
the need for mobility at a joint is balanced by the strength of the joint
strong joints are typically
inflexible-the joints between the vertebrae
highly mobile joints tend to be
weak-the shoulder joint
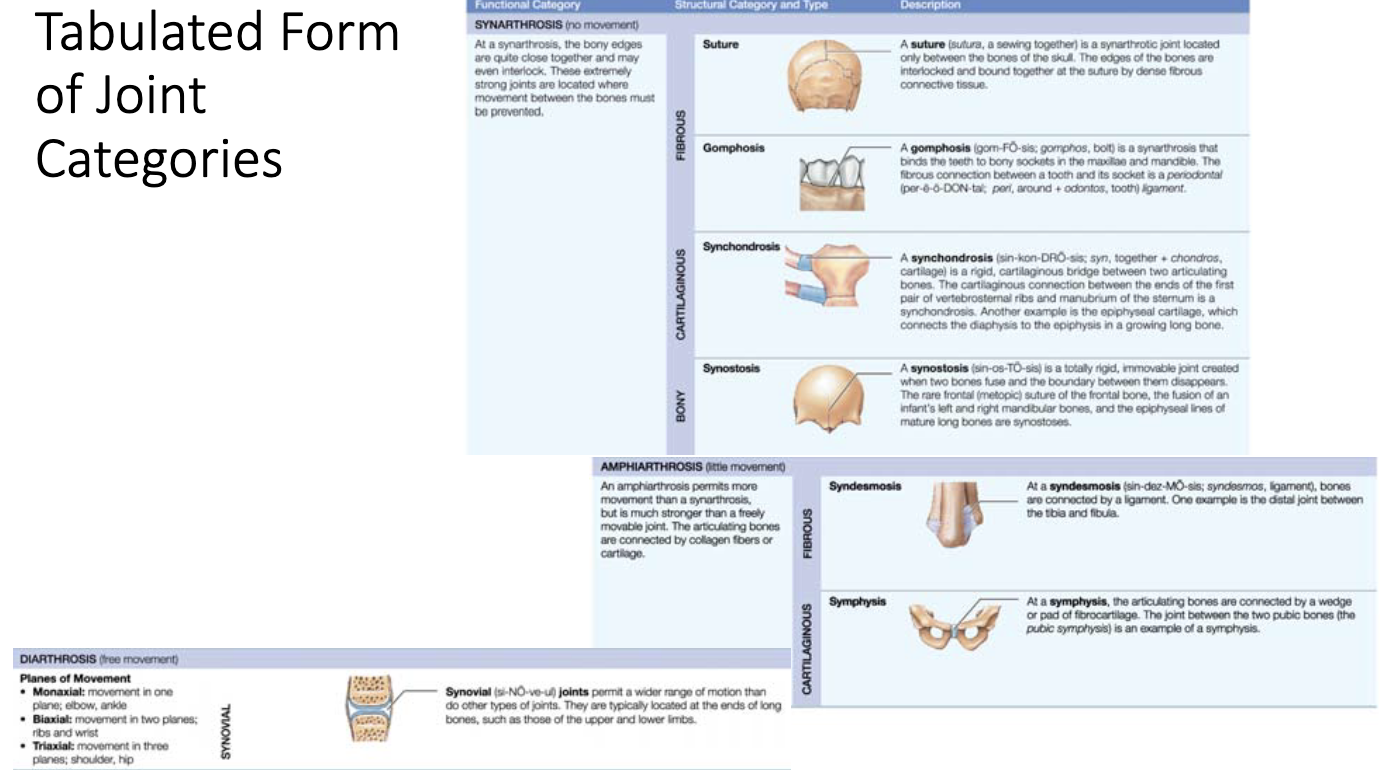
joint categories
synarthrosis, amphiarthrosis, diarthrosis
synarthrosis
immovable joint, typically fibrous or cartilaginous, bones may fuse over time
amphiarthrosis
slightly movable joint, can be fibrous or cartilaginous
diarthrosis
freely movable joint (synovial joint), these joints are sub-divided by range of motions that are allowed
the articulation between the superior and inferior articular processes of adjacent vertebrae are
gliding joints that permit small movements
small flexion movements and rotation movement are allowed at these joints
vertebrae are separated by small cushions of
fibrocartilage termed intervertebral discs
the exception to this are the vertebrae that compose the sacrum/coccyx and the join between the atlas and axis
intervertebral discs have
an outer layer of collagen fibers that attach to the vertebrae
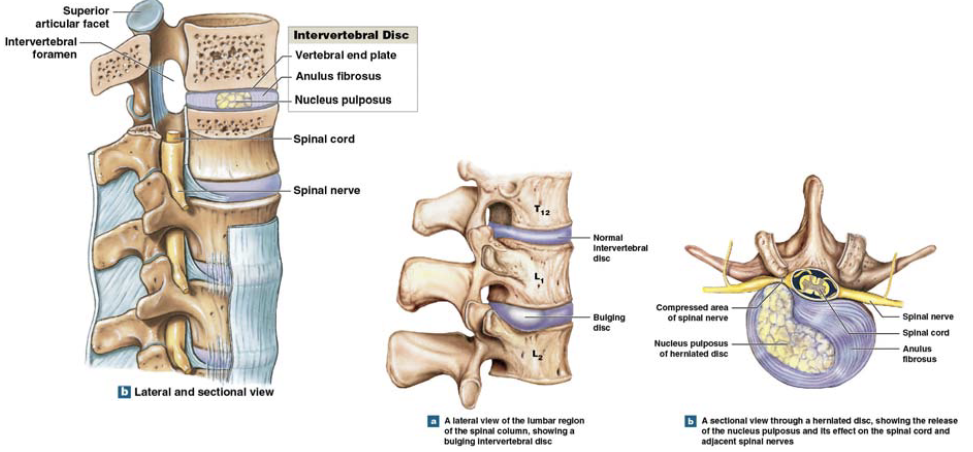
the intervertebral discs outer layer surrounds the
nucleus pulposus, which is a soft gelatinous core-shock absorber
articulations move the nucleus pulposus to allow for a gliding motion
synovial joints
freely moveable and contain a two-layered joint capsule (articular capsule) that surrounds the joint
synovial joints contain
a fibrous capsule to provide a mechanical strength to the capsule
a synovial membrane, which is an incomplete layer of epithelial cells to produce a synovial fluid
under normal conditions bones cannot come in contact with each other in a synovial joint
articular cartilage covers the articulating surfaces
this cartilage contains a large portion of water and is composed of many charged proteins (typically hyaluronan)
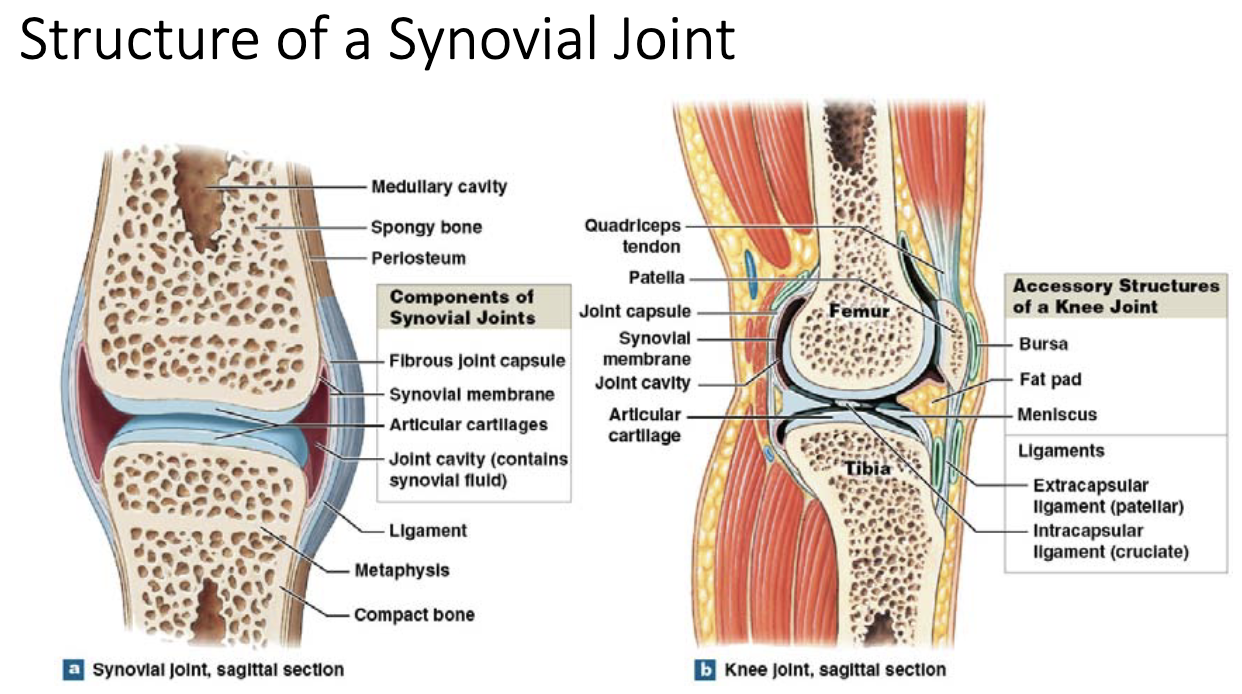
cartilage reduces the coefficient of friction between bones and it holds in place the lubricant; synovial fluid
cartilage-cartilage, cartilage-bone and bone-bone should never come into contact with each other
synovial fluid
a clear highly viscous fluid that is similar to interstitial fluid with the addition of proteoglycans and hyaluronan
relatively low amounts on all joints
functions of synovial fluid
lubrication, nutrient distribution, shock absorption
synovial fluid lubrication
cartilage is a sponge for synovial fluid; upon compression this fluid is squirted into the joint space and significantly reduces the friction coefficient
synovial fluid nutrient distribution
cartilage is avascular and the synovial fluid brings nutrients and removes waste from the joint space it is continually circulated through the joint space
synovial fluid shock absorption
synovial fluid cushions joints subjected to compression and due to the high viscosity can dampen sudden high-magnitude impacts (ec. walking)
supporting joint structures
meniscus, fat pads, ligaments, tendons, bursae
meniscus
pad of fibrocartilage located between opposing bones, may help to direct the flow of synovial fluid
fat pads
localized mass of adipose tissue that can protect the articular cartilage-packing material that fills space during articulations
ligaments
support, strengthen and reinforce joints (sprain is a tear of the collagen fibers within a ligament
tendons
not part of the joint, but may limit the motion of the joint as they pass over the joint space
bursae
small, fluid-filled sacs that contain synovial fluid, they form when tendons/ligaments rub against other tissues, can act as a shock absorber
gliding movements
two opposing surfaces slide over each other
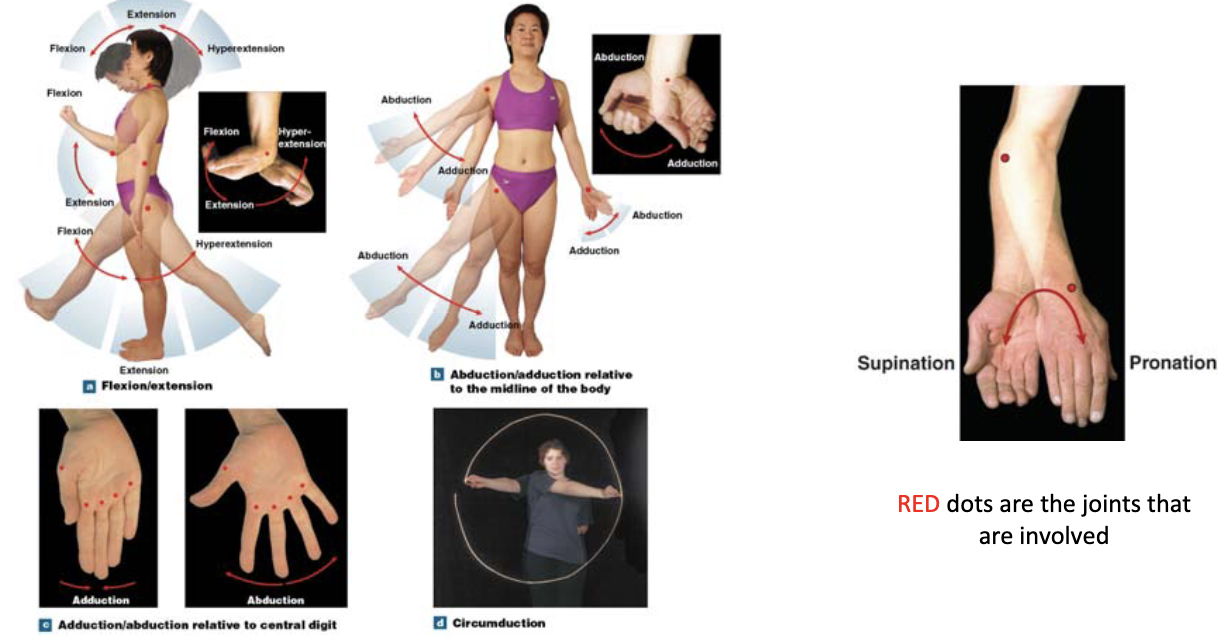
angular movements
flexion, extension, abduction, adduction, circumduction, pronation/supination
classification of synovial joints
gliding joint, hinge joint, saddle joint, pivot joint, ball and socket
gliding joint
flattened or slightly curved surfaces that slide across one another, but offer little movement
hinge joint
permit angular motion in a single plane
condylar joint
ellipsoid joints that have an oval articulation nested within a depressed surface, permits biaxial angular motion
saddle joint
concave bone articulating with a convex bone, permits biaxial angular motion
pivot joint
only permits rotation along one direction
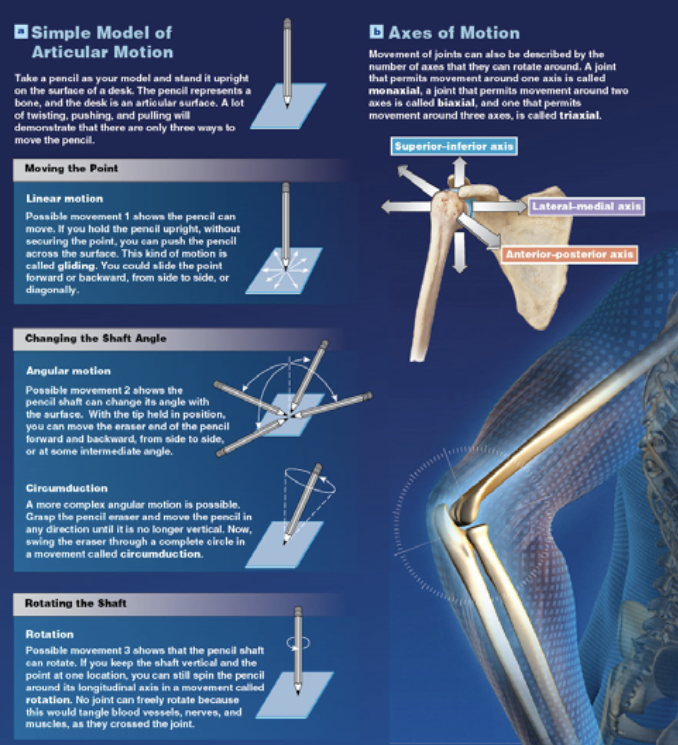
ball and socket joint
rounded head of one bone rests within a cup-like depression of a second bone, permits angular rotation circumduction
shoulder joint
permits the greatest range of motion of any joint and it is also the most frequently dislocated
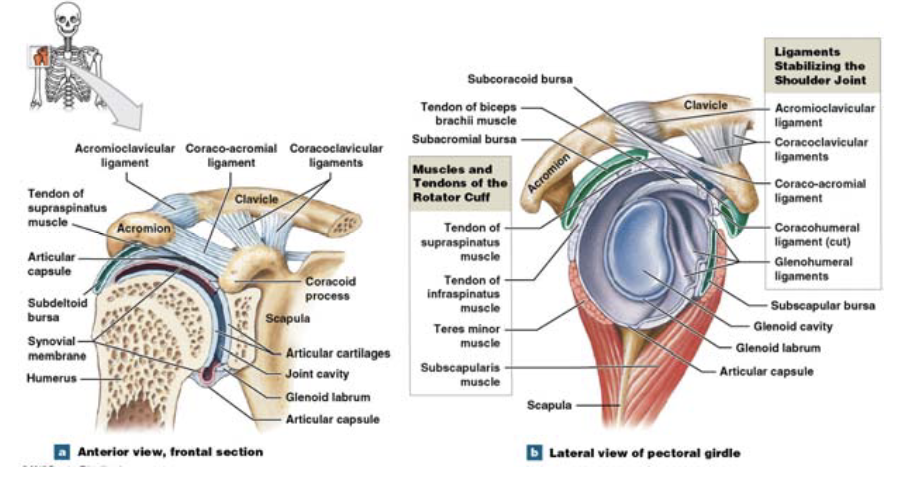
the bones of the pectoral girdle provide some stability, because they project over the joint
is it the skeletal muscles that provide the majority of the stability/strength to the joint
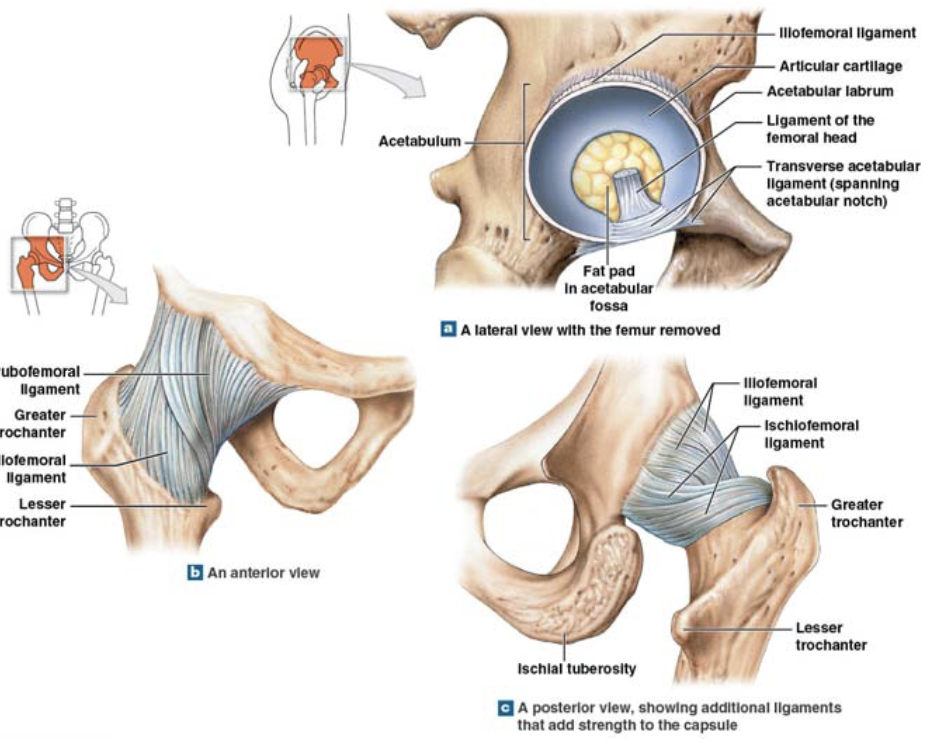
hip joint
relatively stable ball and socket joint that permits extension, flexion, adduction, abduction, circumduction and rotation
the articular capsule of the hip joint is extensive and strong, enclosing both the head and the neck of the femur
much of the strength and stability is provided by the surrounding muscles, which are typically much more extensive than the shoulder joint
also the pelvic girdle for the humeral head
many ligaments also wrap the hip joint
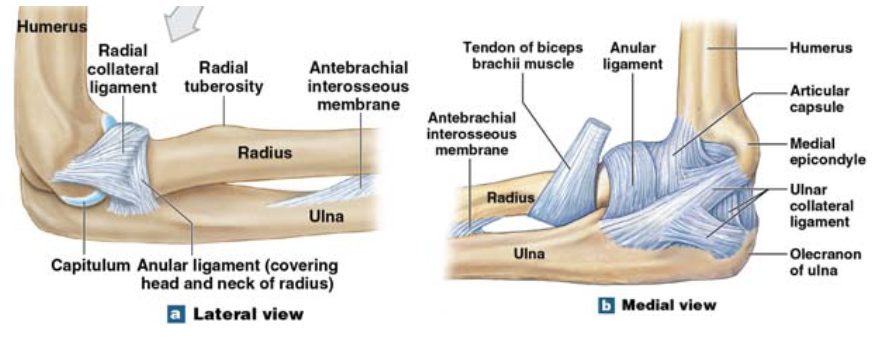
elbow joint
complex hinge joint, involving the articulation of three bones
humeroradial joint is a much smaller joint that helps to support the main joint (strongest)
this joint is very stable because the humerus interlocks with ulna, a thick capsule surrounds the entire joint and there is extensive ligaments that wrap around the joint
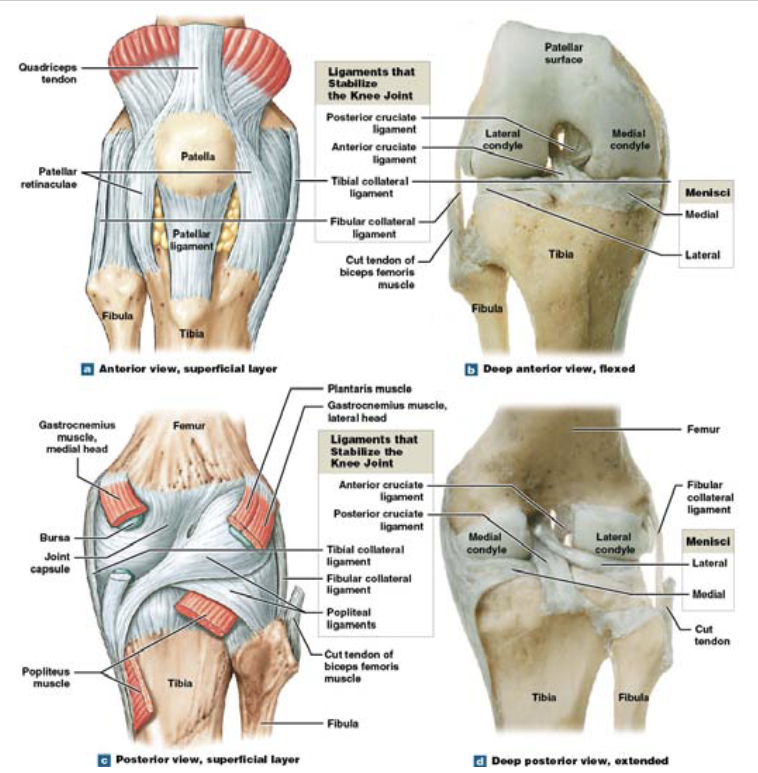
knee joint
most complicated
hinge joint
not stable and the contact points are always changing (femur-tibia, femur-tibia, patella-femur)
the articular capsule of the knee is thin and not complete, however extensive ligaments and tendons help to strengthen the joint
kinesiology
breaking down motor movements, determining the nature of each moevemtn
erect posture
human body does not have one single posture because we are a multisegmented organism
has many issues (not a static position, oscillations of the center of gravity is remarkable constant, very strong alignment with the line of gravity and particular anatomical features)
energy costs of erect posture
there appears to be a minimal demand for excess energy to maintain an erect posture as compared with basal energy demands
poor erect posture (either stand stiffly or relaxed) does not have an effect on other organ function
proprioceptors (sense of self) are responsible for most of the movements necessary for the maintenance of erect posture
changes to ones posture can be made with frequent repetition of specific exercises
walking
is a reflexive action;no conscious control is needed
example of translational motion of the body by angular motion of the legs
phases of walking
beginning of restraining phase of one leg overlaps the end of the propulsion phase of the other leg-period of double support (running does not have)
swinging phase like a pendulum, where gravity and momentum of the body provide much of the motion
supporting phase is like an inverted pendulum
motion during the supporting phase is provided by the propulsion of the other leg and the overall momentum of the body
running
there is no period of double support and there is a period of no support
jumping
the amount of energy needed to overcome inertia is intense
functions of blood (which is connective tissue)
transporting dissolved gases, nutrients, hormones and metabolic wastes, regulate pH and composition of interstitial fluid, restricting fluid loss at injury sites, defense against toxins and pathogens, stabilize body temperature
blood functions: regulate the pH and composition of interstitial fluid
diffusion between blood and fluid compartments dictates concentrations
blood functions: restricting fluid loss at injury site
clotting prevents the loss of fluid and cellular matter