OPT 323 Epidemiology Terms and Studies
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
101 Terms
What are the 2 assumptions of epidemiology?
diseases and risk factors DON'T occur at random
AND
disease is NOT randomly distributed throughout a population
What are the 3 main practical goals of epidemiology?
describe the burden of disease, disability, or death within a population
predict the probability that an individual within a defined population will develop a disease
compare the disease frequencies/”factors” within or between populations (or between exposed and unexposed groups)
What is epidemiology?
study of distribution and determinants of disease in a human population
What is the exposure?
entity = toxical chemical, micro-organism
OR
behaviour = where one works, socializes
OR
attribute = age, race, sex, genes
NOTE: these may be associated with an increased OR decreased occurence of disease
What is the outcome?
disease state, event, or behaviour that is under condition
What are 3 main shortcomings of epidemiology?
difficulty in measuring exposure = duration, some things are hard to measure
separating causal contributions of exposure from other exposures to remove confounds
difficulty assessing role of multiple small risks and how they interact
What is the main impractical goal of epidemiology?
does exposure A cause outcome B?
establishing causation is always our ultimate goal
What are Hill's 9 causal criteria?
temporality = exposure must be BEFORE outcome
strength of association
biological gradiant = dose-response
plausability and mechanism
constistency and replication
specificity
coherence
experimental evidence
analogy = alternate explanations
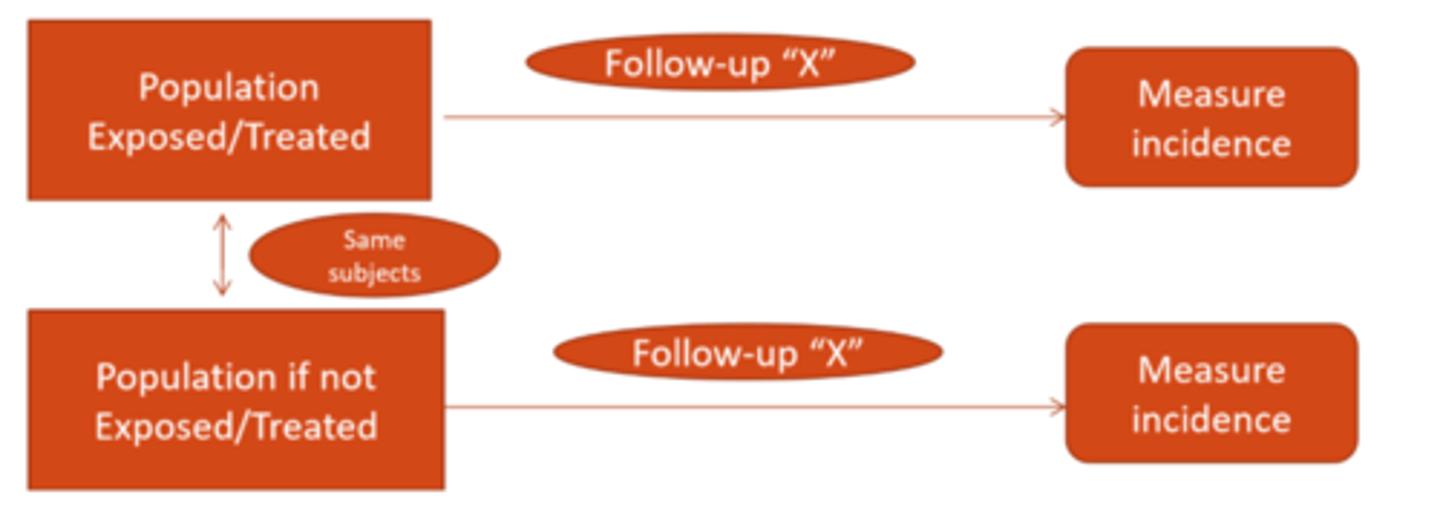
What is the ideal design for an epidemiological study?
counterfactual model = have 1 singular population and compare the measured incidence if exposed vs not
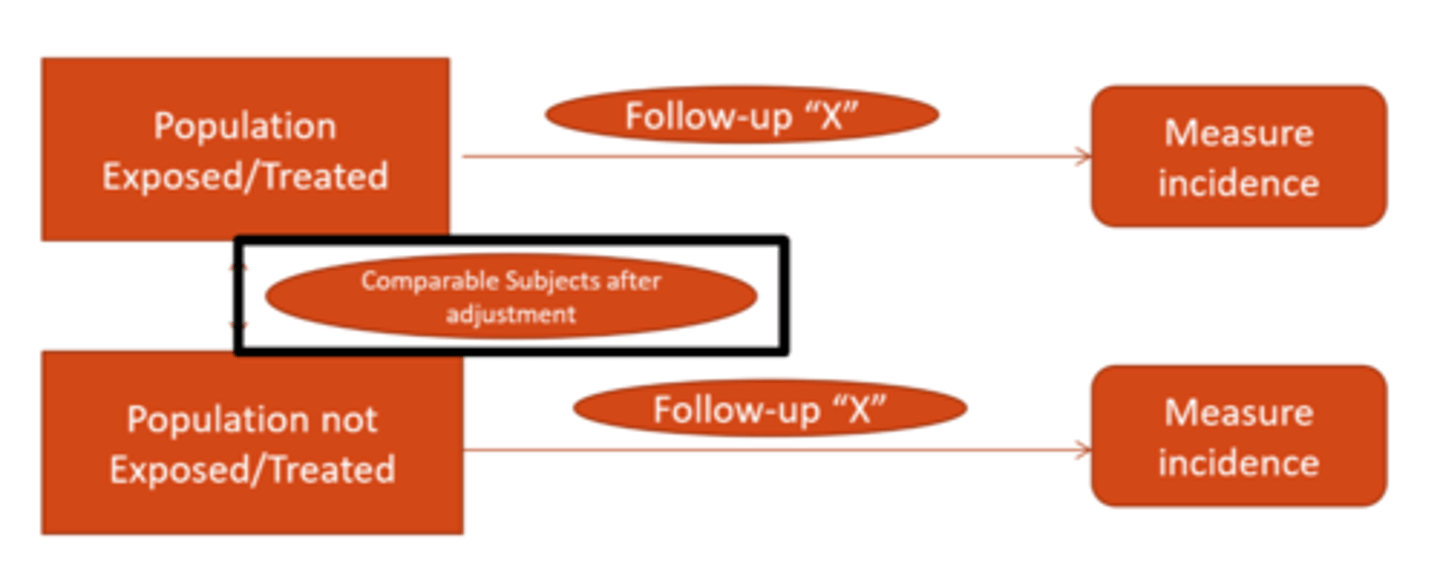
What is the real design for an epidemiological study?
have 2 populations (each as similar as possible), 1 exposed and 1 not, then measure incidence in both
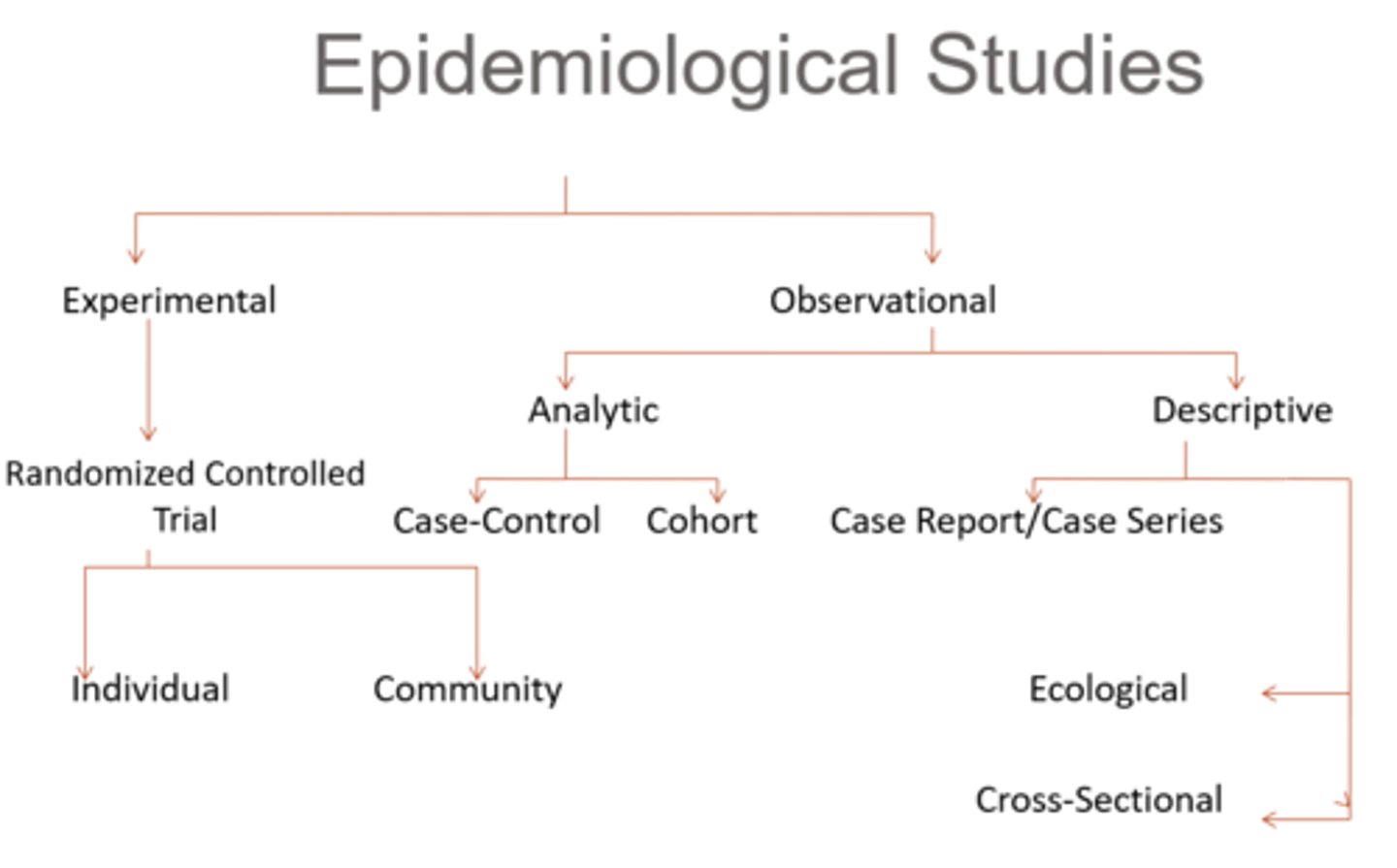
What is the difference between an experimental vs observational epidemiologic study?
experimental = exposure status assigned by researcher
observational = exposure status NOT assigned by researcher
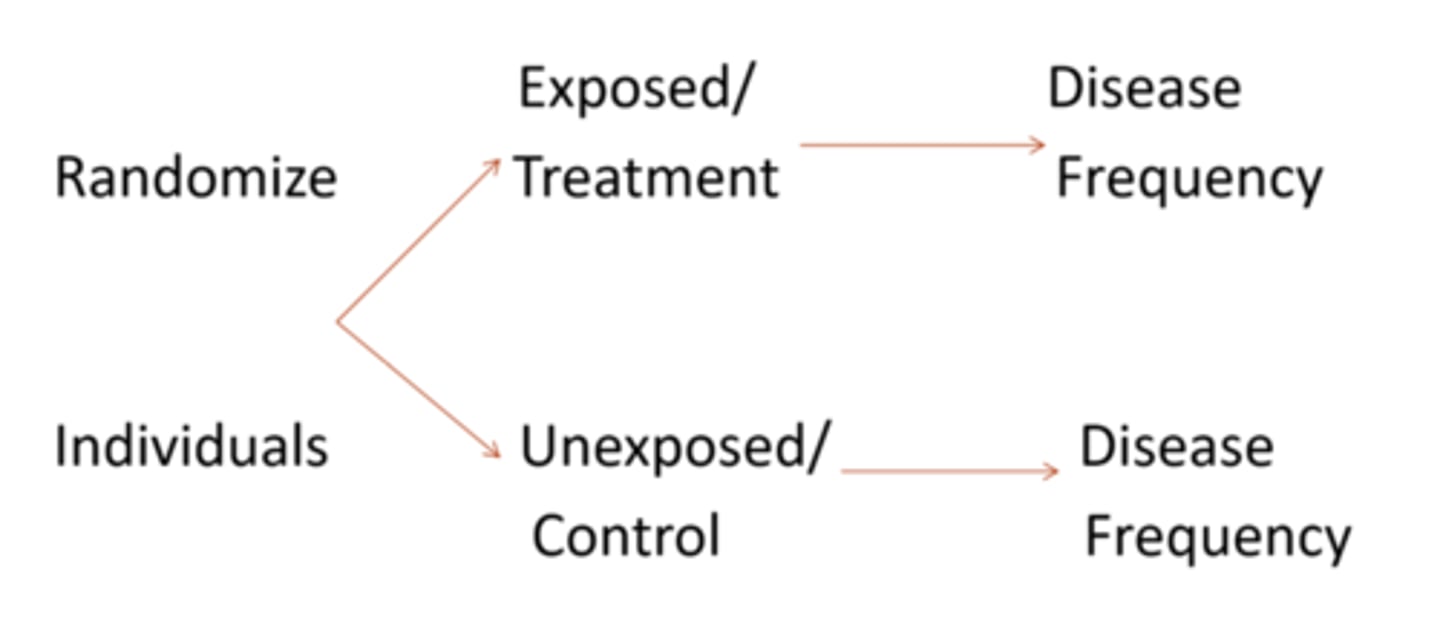
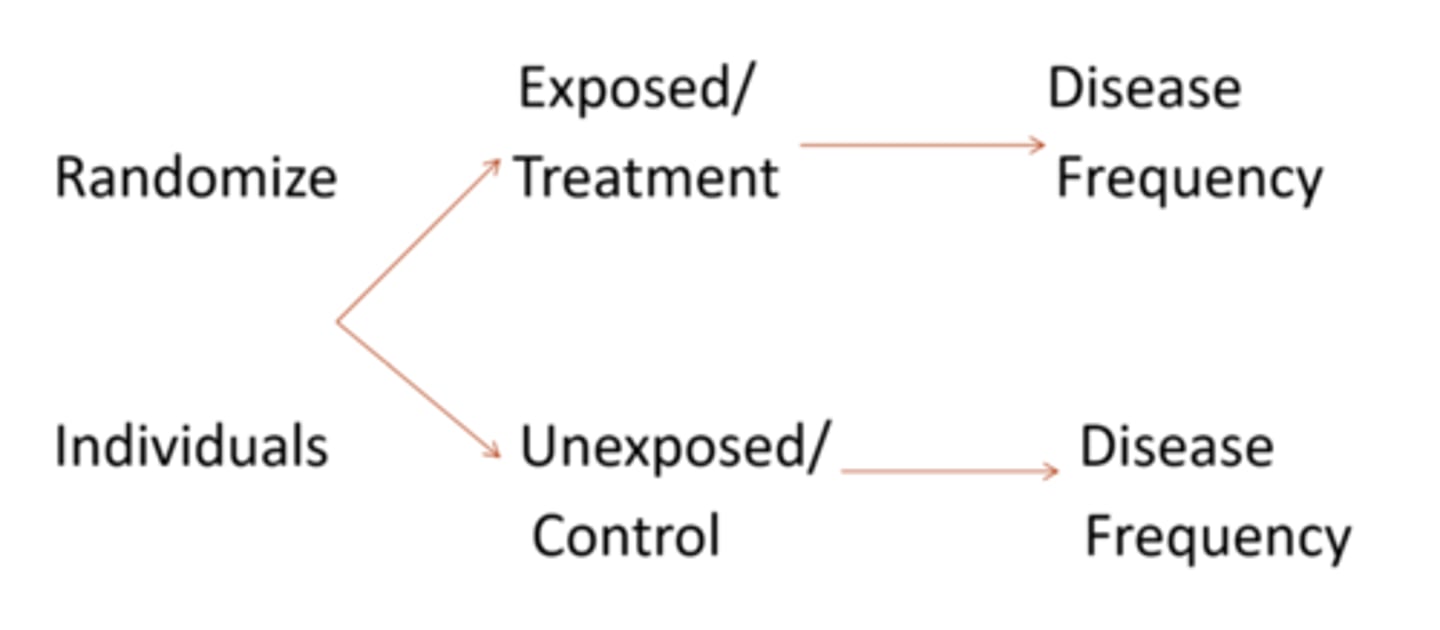
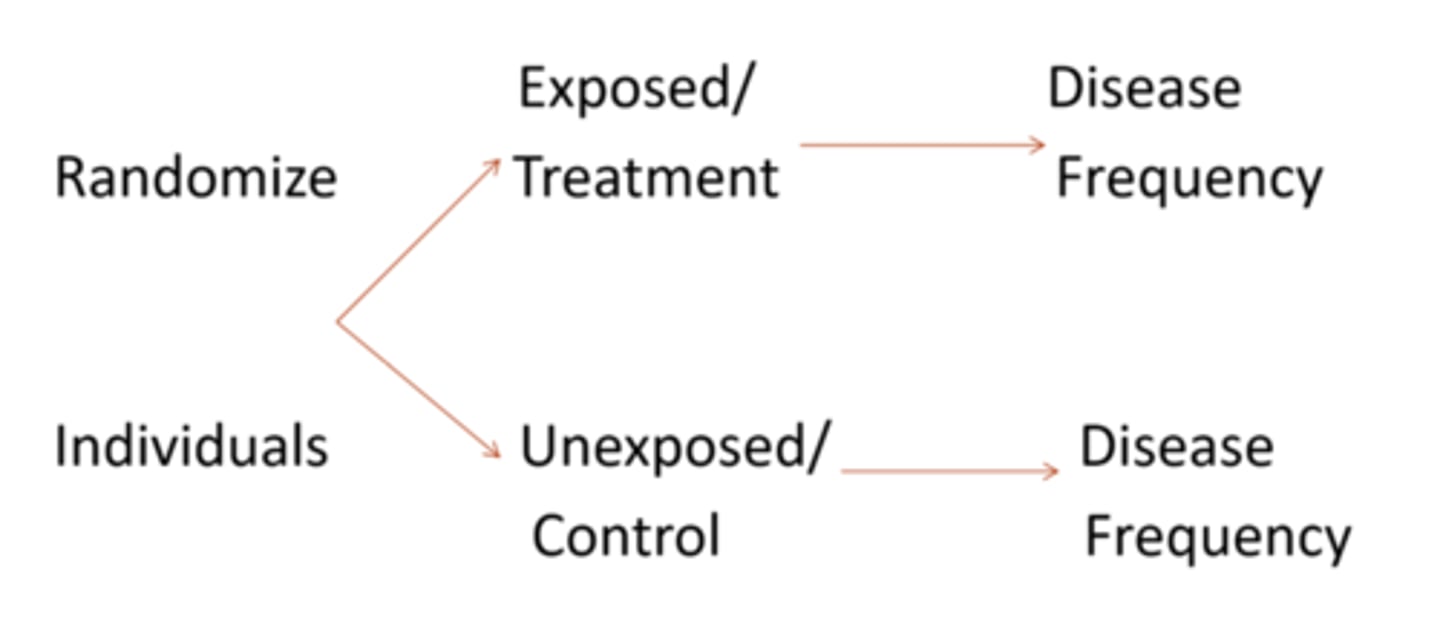
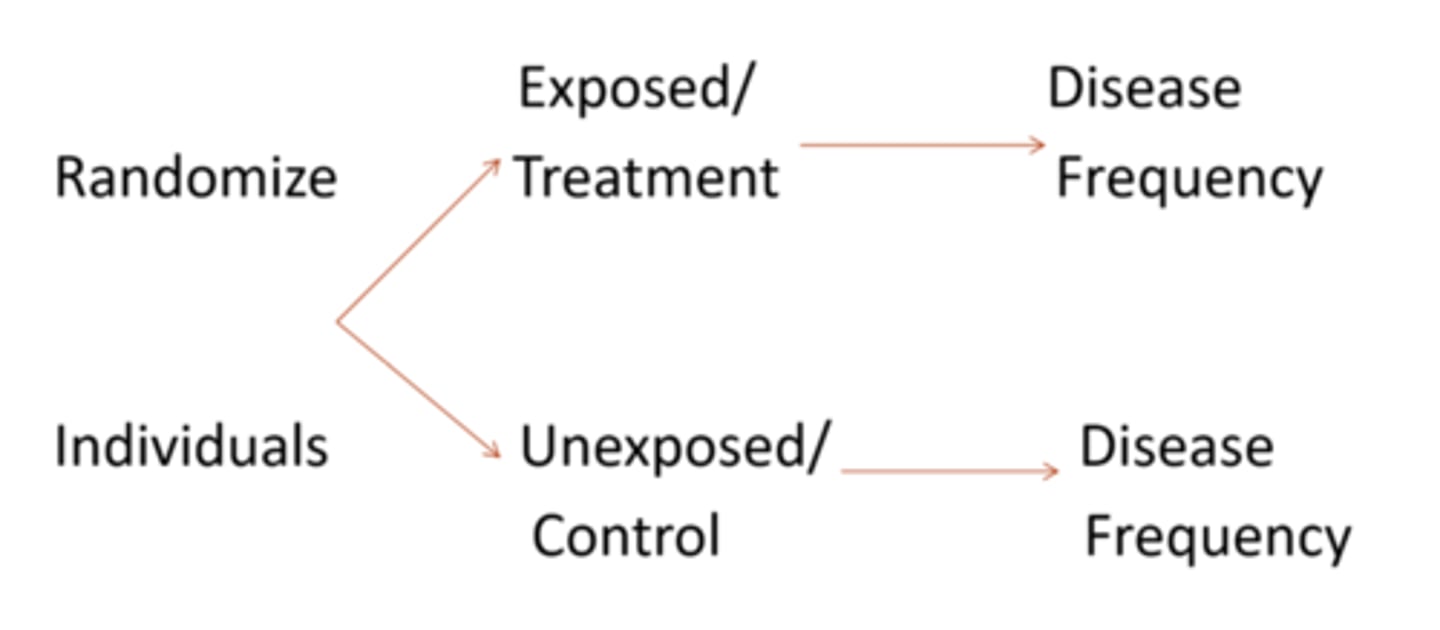
What is a randomized controlled trial experimental study?
1 group of very similar people without outcome are randomly assigned either a treatment/exposure or placebo, then outcome is compared after
What does it mean if a RCT is double or triple blinded?
double = subject and examiner do not know who belongs to what group
triple = statistician also does not know
What are some advantages of a RCT experimental study?
standard approach to test new treatments (gold standard)
prospective = we look to see how things progress temporally
exposure is assigned
What are some disadvantages of a RCT experimental study?
time-consuming
expensive
same effect in real world?
non-compliance
ethical issues (life-threatening conditions, who gets the placebo)
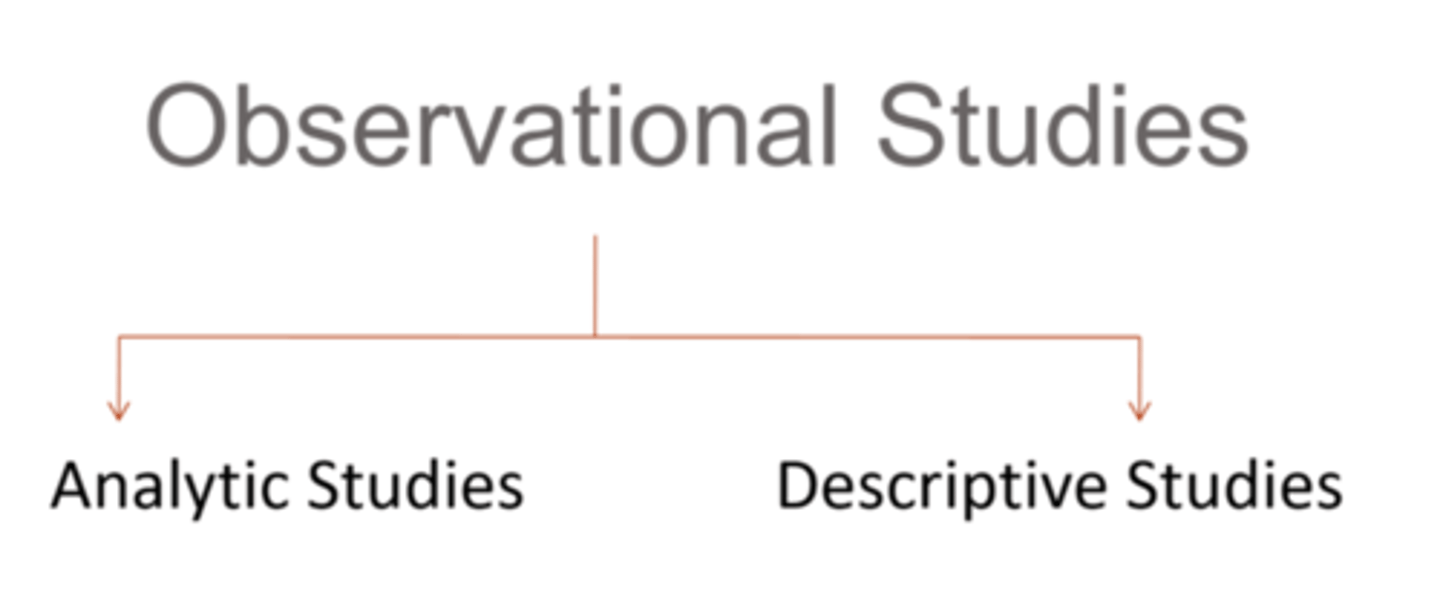
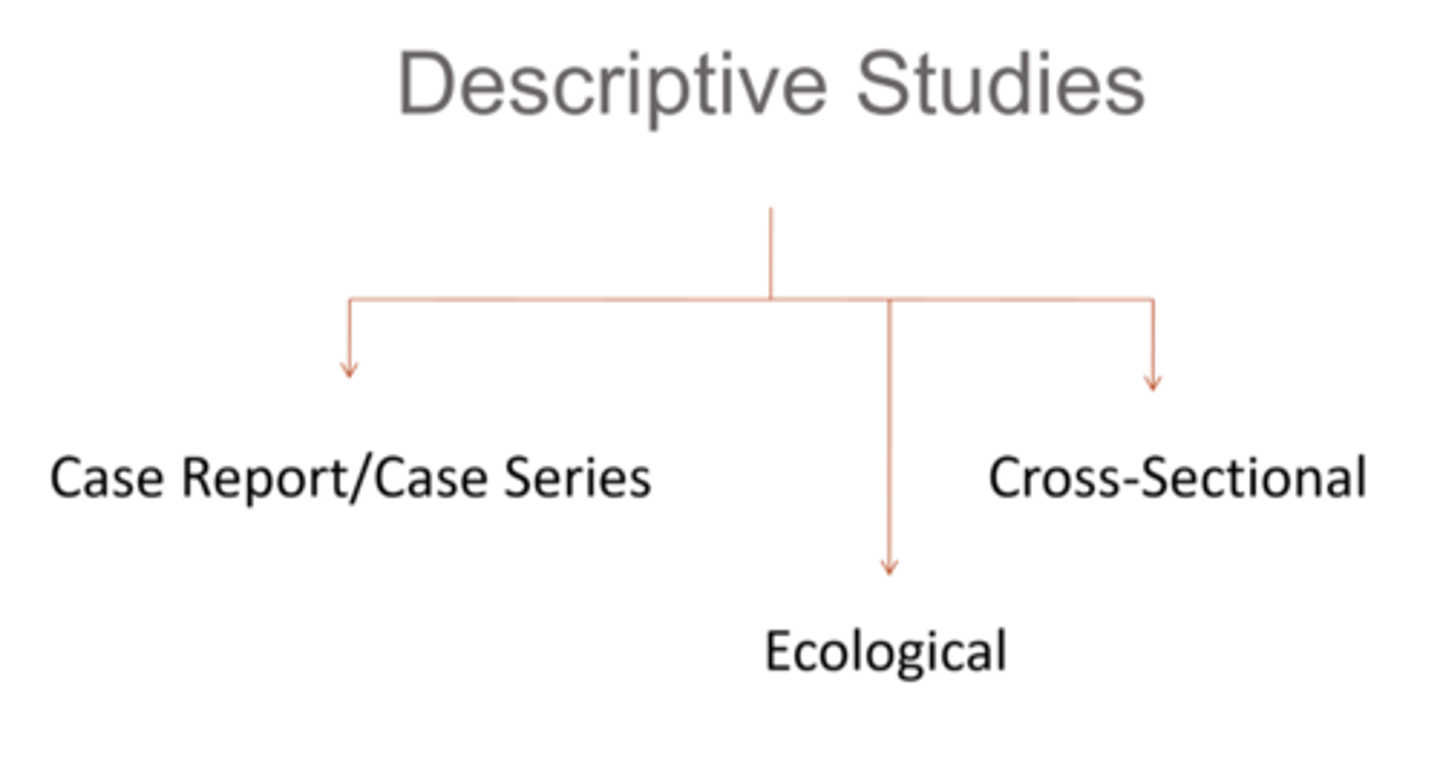
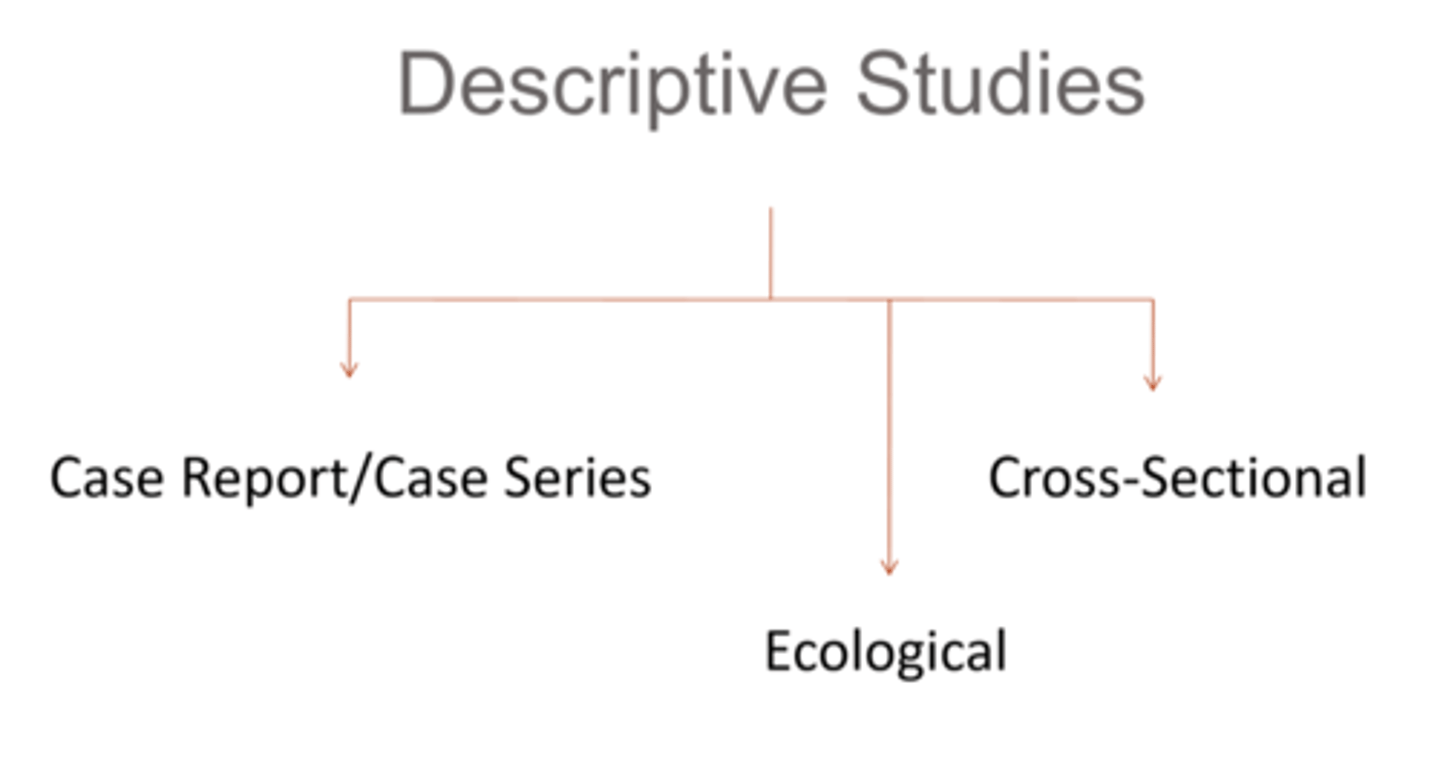
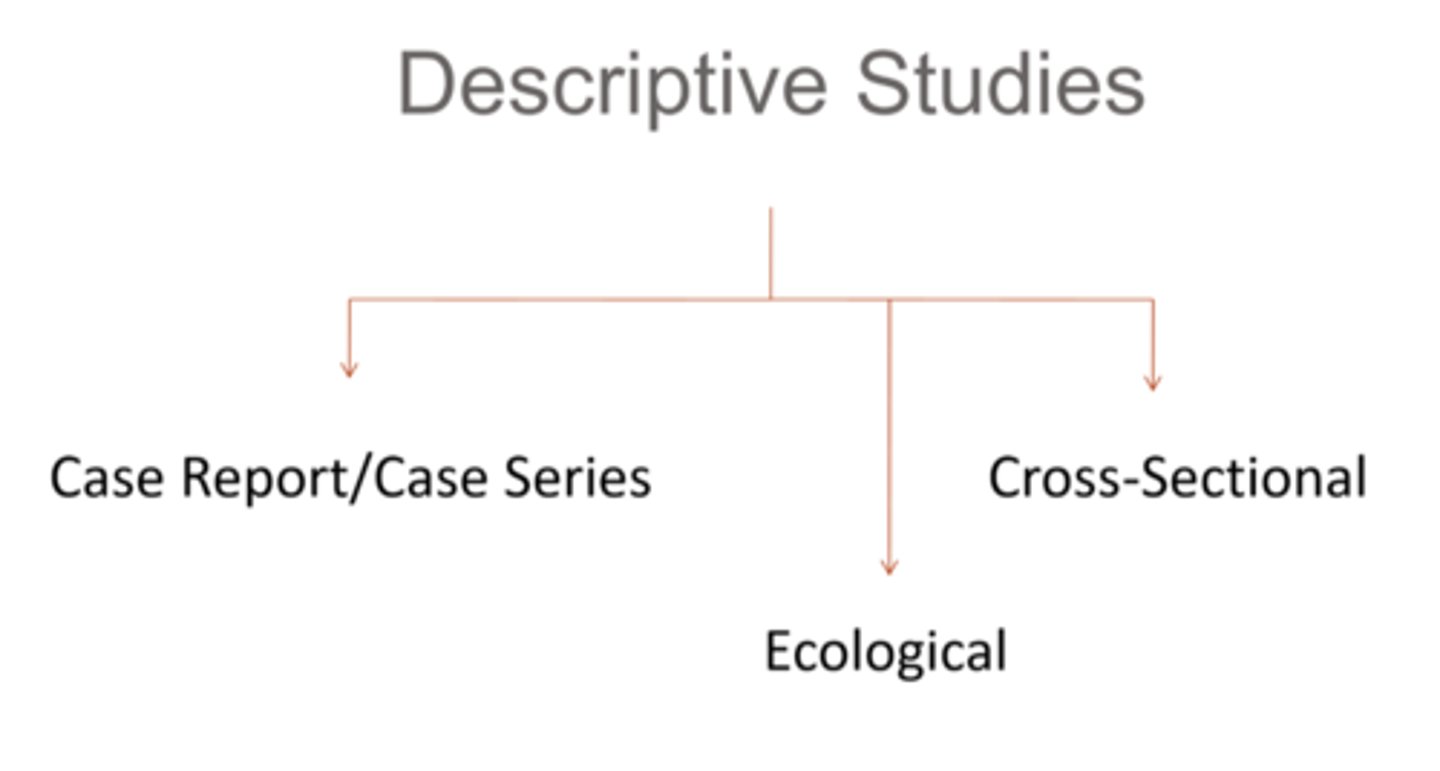
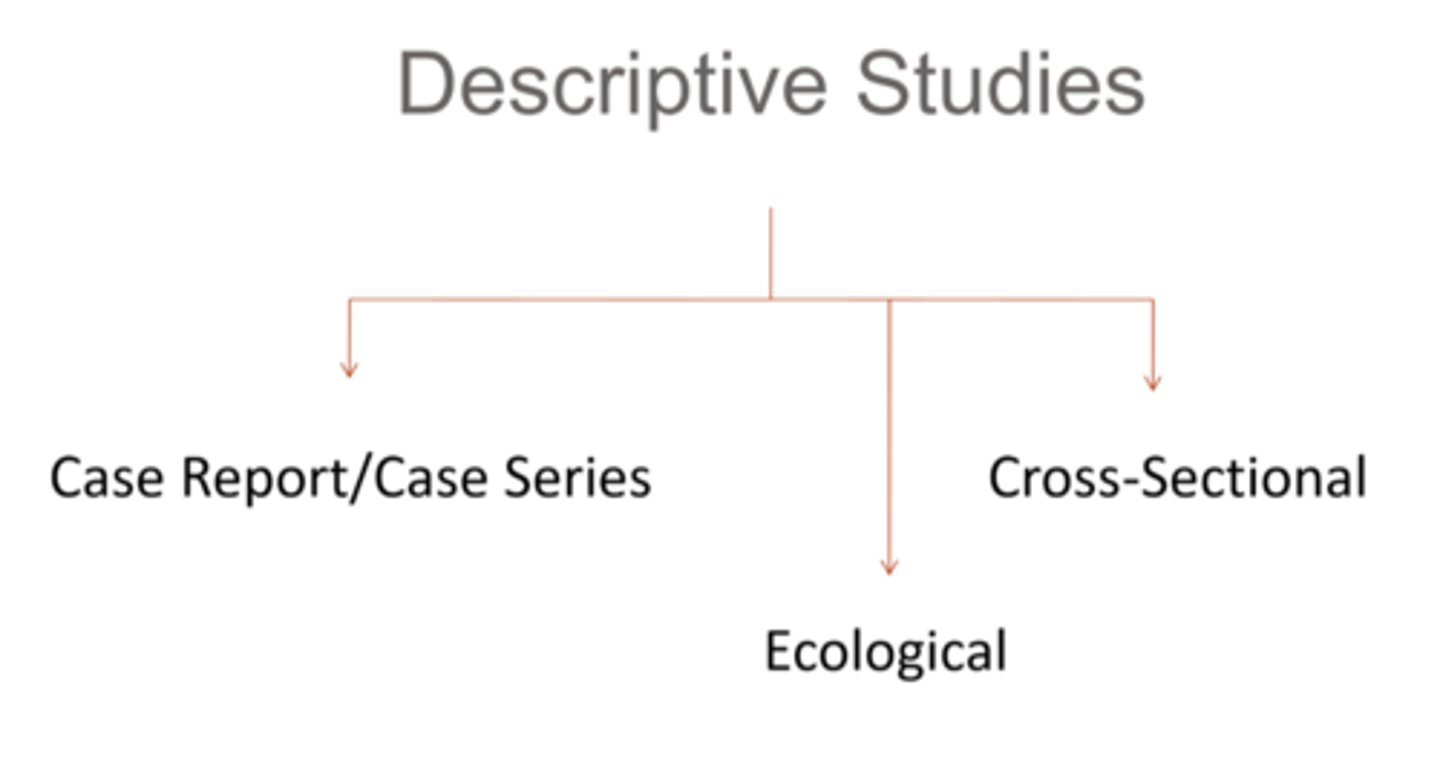
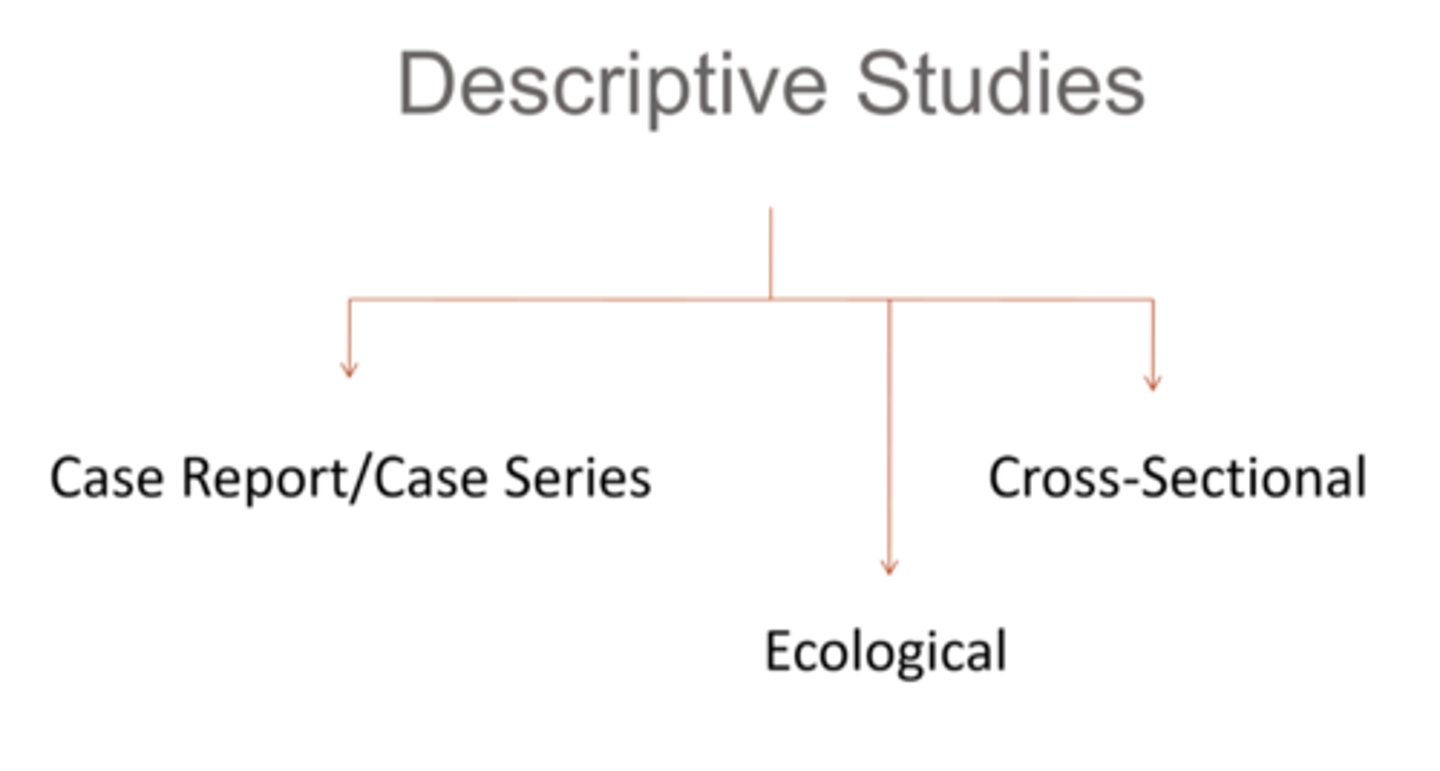
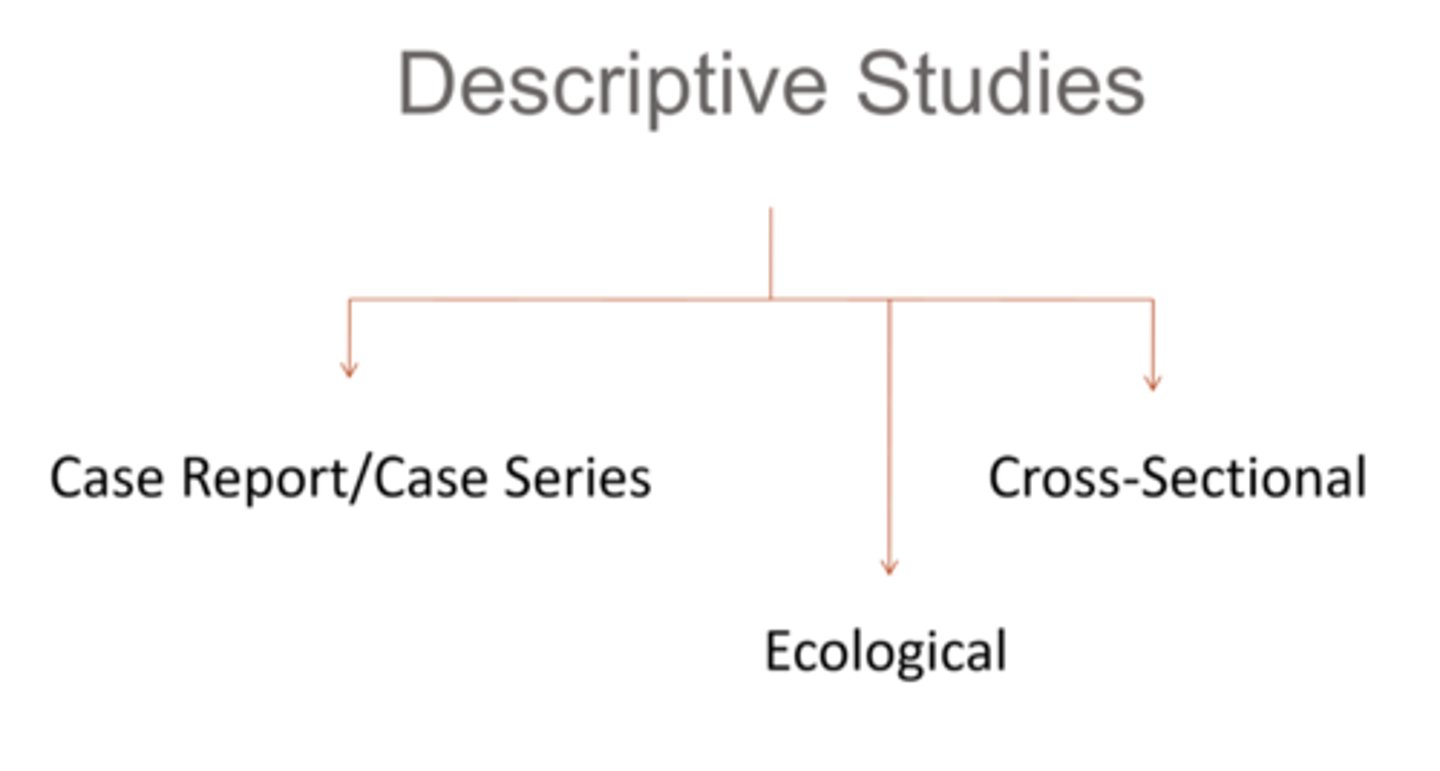
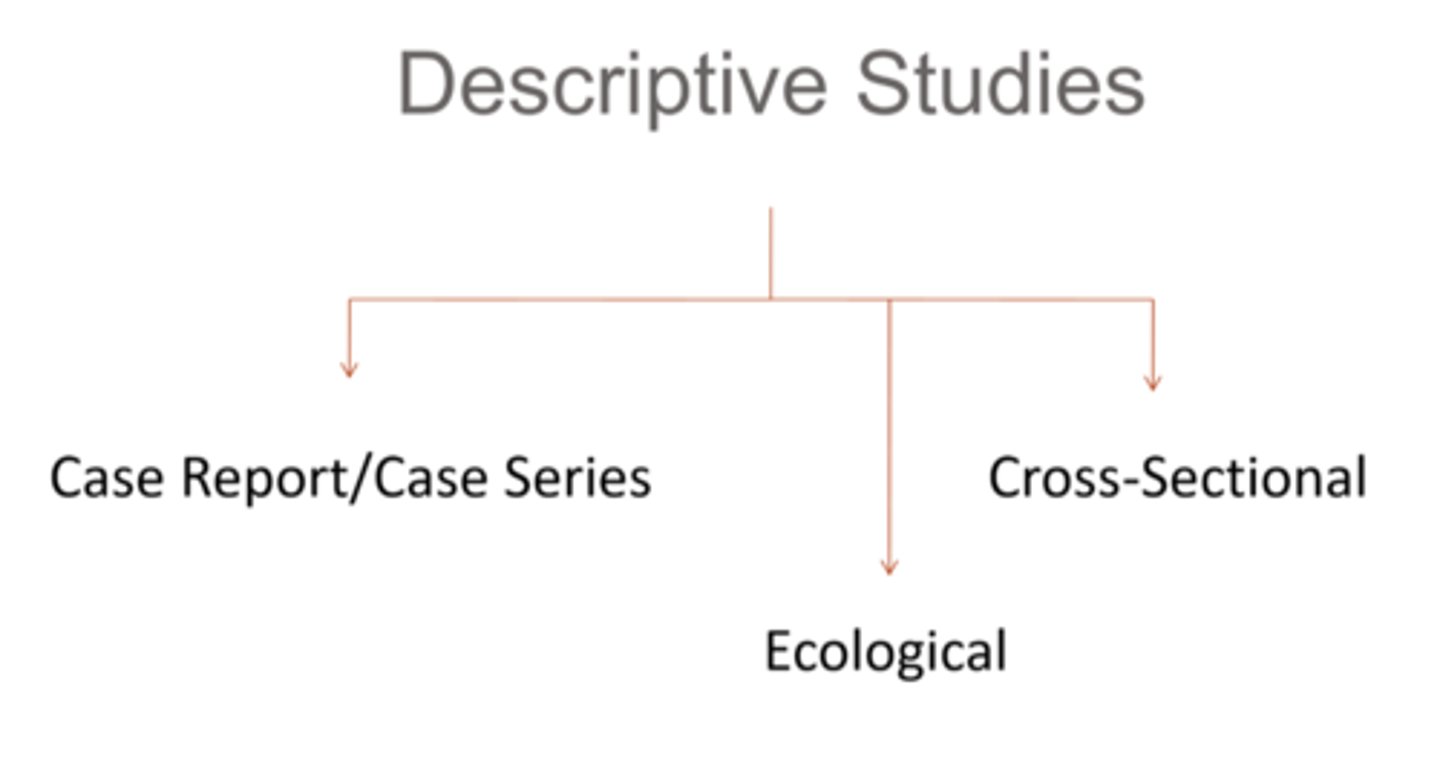
What is the difference between analytic vs descriptive observational studies?
analytic = WHAT, HOW, WHY = comparing groups helps establish cause or risk factors of exposure and outcomes
descriptive = WHERE, WHEN, WHO = identifies patterns in cases and populations, including rates and risk
What is incidence rate?
# of new cases that develop in a population at risk during a given person-time period at risk = expressed as a rate (comparing 2 quantities with different units)
How do we calculate incidence rate?
# new cases / person-time at risk
What is cumulative incidence?
risk of acquiring disease within a defined time period, expressed as a percent
How do we calculate cumulative incidence?
= # new cases / total population at risk x 100
NOTE: longer time period = higher CI
What is prevalence?
# of current cases that are present in a population at risk at a given time point / snapshot = expressed as a proportion (comparing 2 quantities of the same thing, parts of a whole)
How do we calculate prevalence?
= incidence rate x disease duration
What is a population study?
analyzes and predicts populations trends and challenges = often used to establish risk of an individual in a population getting a disease
What is a cohort analytic (observational) study?
observe a population of people with and without a certain exposure, and monitor them over time prospectively to see if exposed vs non-exposed develop the outcome
What are some advantages of a cohort analytic (observational) study?
prospective with a comparison group
info on multiple exposures and/or multiple outcomes
suitable/efficient for studying rare exposures
temporality = exposure before outcome
calculation of outcome incidence in exposed and unexposed subjects
allow for calculation of risk
What are some disadvantages of a cohort analytic (observational) study?
relatively expensive
time consuming = study subject drop-out, prolonged follow-up
not suitable/efficient for studying rare (or very “delayed”) outcomes
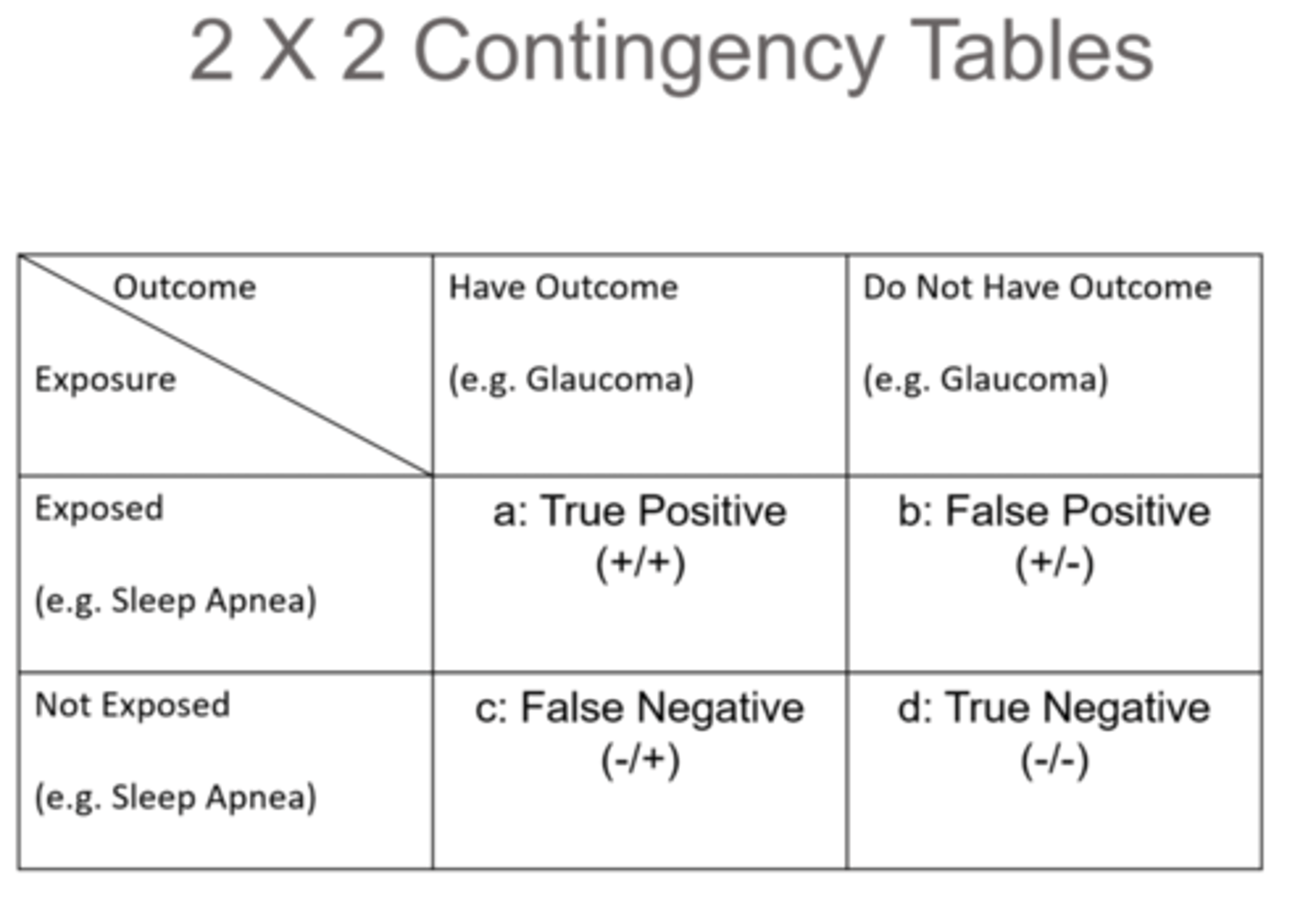
What is a true positive?
(+)exposure
(+)outcome
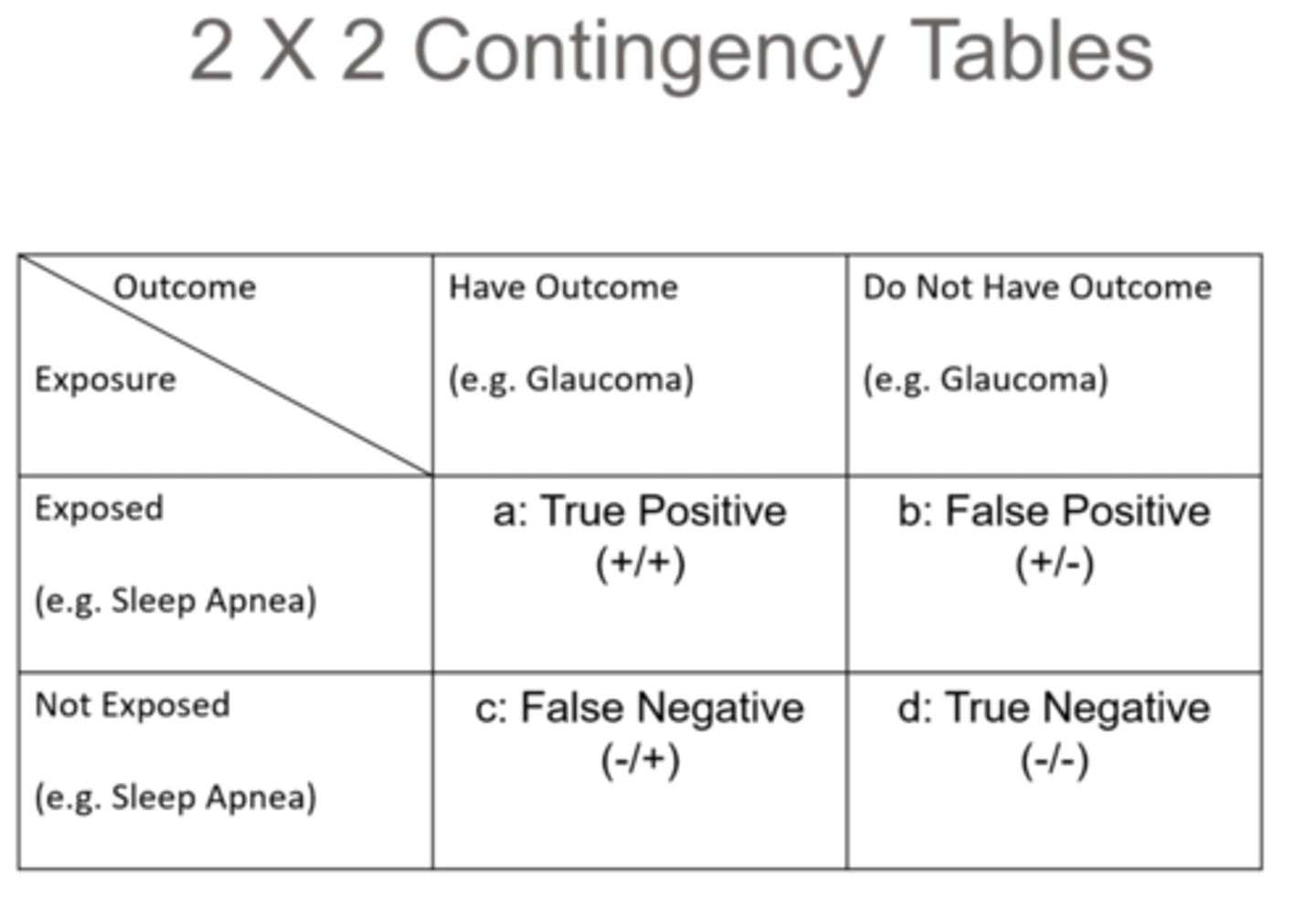
What is a false positive?
(+)exposure
(-)outcome
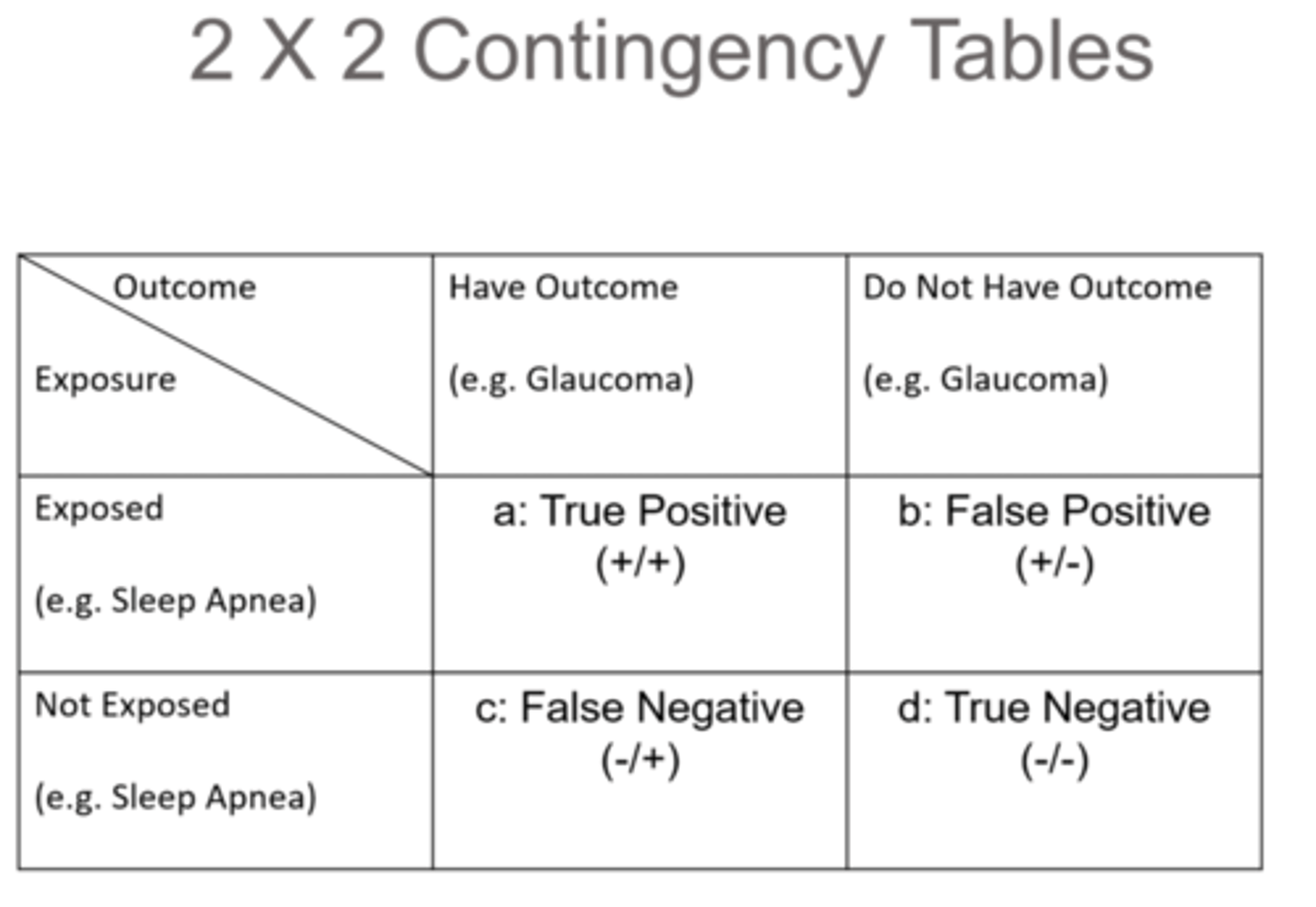
What is a true negative?
(-)exposure
(-)outcome
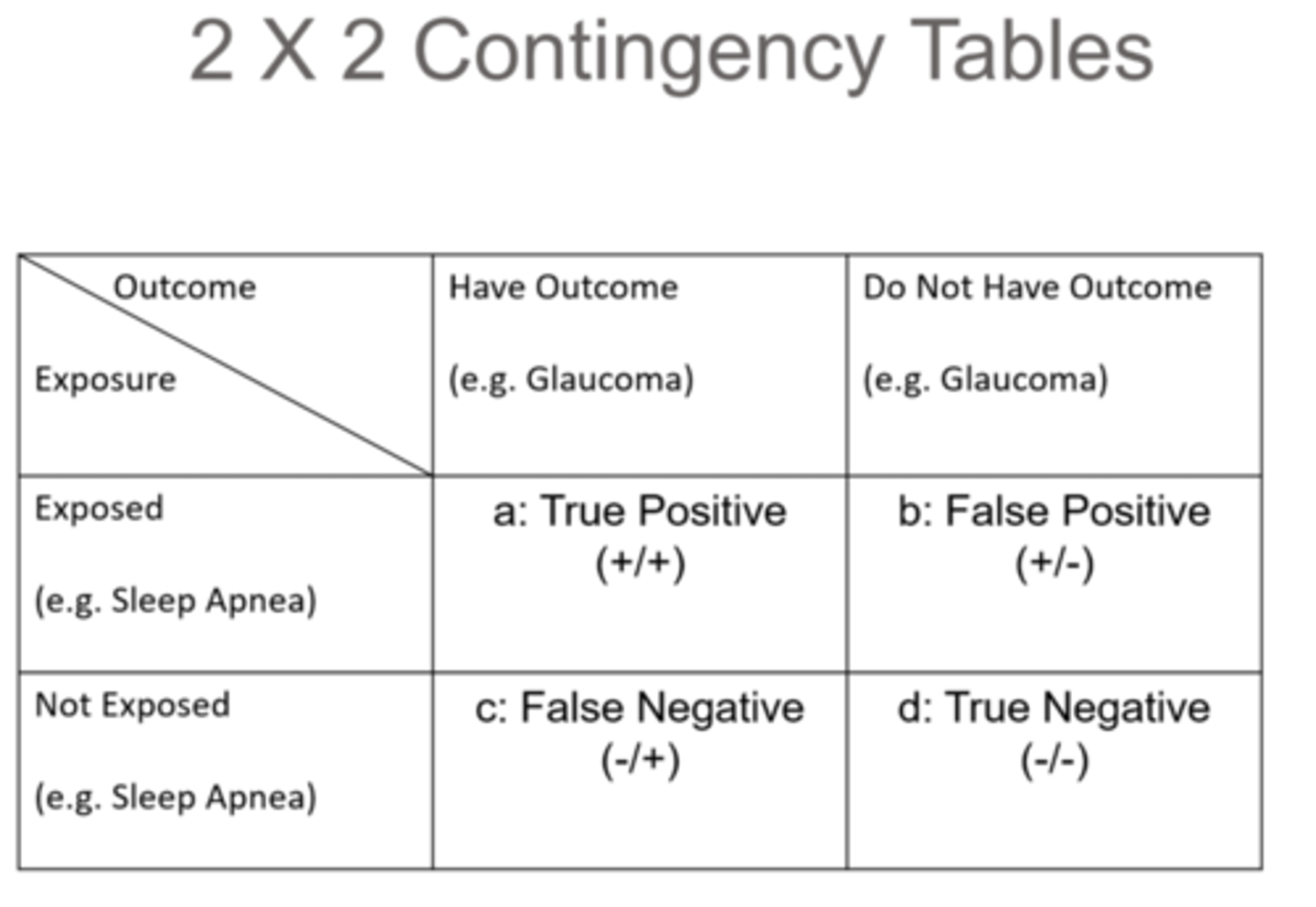
What is a false negative?
(-)exposure
(+)outcome
What is a case-control analytic (observational) study?
retrospective analysis of people with and without an outcome (cases and controls) to check for exposure in each group
What are some advantages of a case-control analytic (observational) study?
comparison group
relatively inexpensive
quick = already have data
very suitable/efficient for studying rare (or very “delayed”) outcomes bc easy to find cases that already exist
can study outcomes with long latency
can test multiple exposures for a single outcome
generate exposure “odds ratio”
What are some disadvantages of a case-control analytic (observational) study?
retrospective
control selection can be troublesome
exposure may be difficult to measure
subject to bias (e.g. recall)
temporality may be equivocal
cannot study multiple outcomes (diseases)
cannot directly determine incidence or risk
What is a cross-sectional desriptive (observational) study?
assess exposure and outcome simultaneously at a snapshot in time = compares subjects with exposure and subjects with exposure and outcome
What are some advantages of a cross-sectional desriptive (observational) study?
relatively inexpensive
quick (e.g. surveys)
practical for outcomes (diseases) of long duration and/or prolonged, progressive onset
practical for biological characteristics that do not change over time
establish prevalence
What are some disadvantages of a cross-sectional desriptive (observational) study?
no cause and effect
no temporality
can miss rare exposures/outcomes (diseases)
can miss outcomes (diseases) of short duration and/or having sporadic manifestations
not useful for rapidly emerging outcomes (diseases)
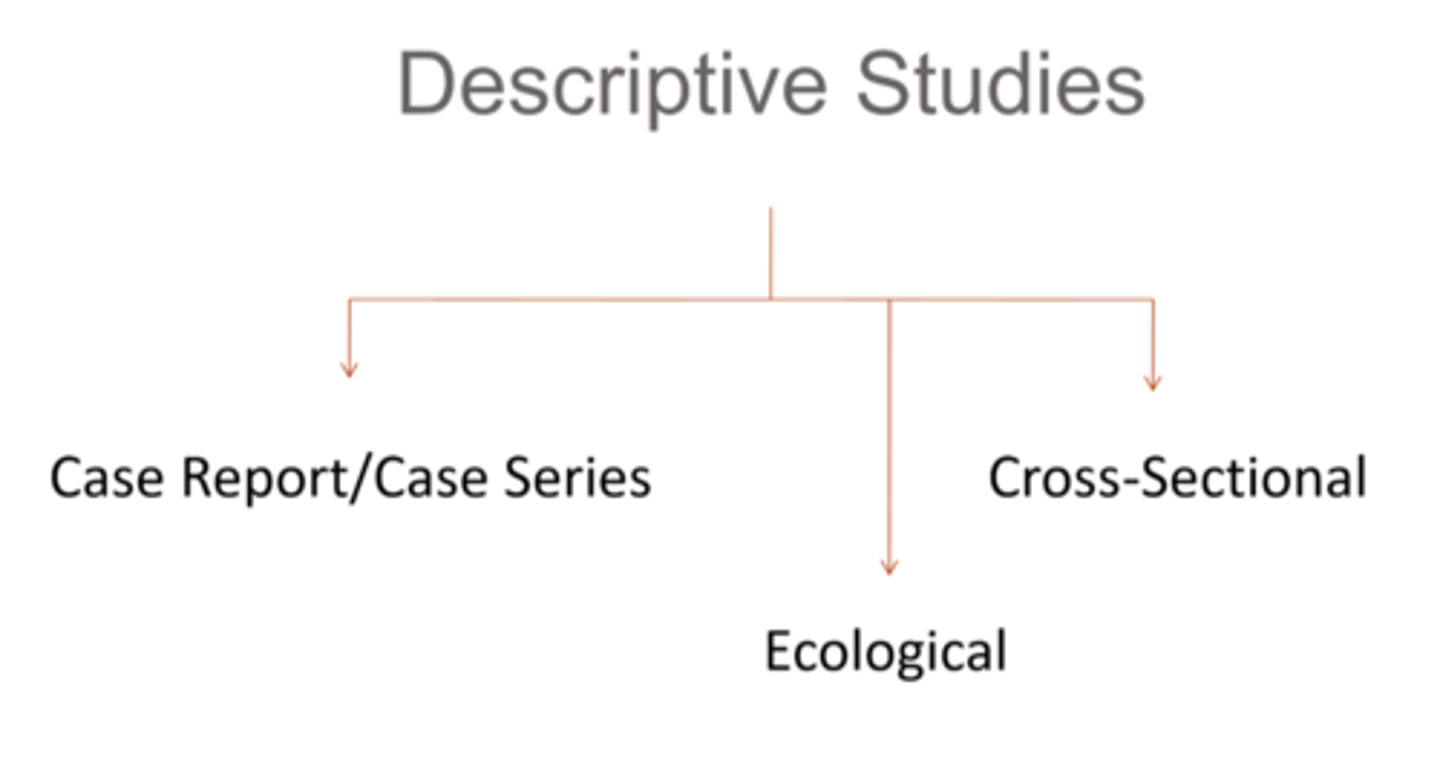
What is an ecological desriptive (observational) study?
analyzes groups/populations rather than individuals, trying to determine relationship between exposure and outcome
What are some advantages of an ecological desriptive (observational) study?
relatively inexpensive
quick (can sometimes use existing data)
big picture (population trends, broad social processes)
may detect previously unknown/unappreciated associations (as an exposure could be more variable across groups than within groups)
What are some disadvantages of an ecological desriptive (observational) study?
cannot establish causation
unable to control for confounding variables
ecological fallacy = trying to infer individual-level correlation/causation from group-level associations
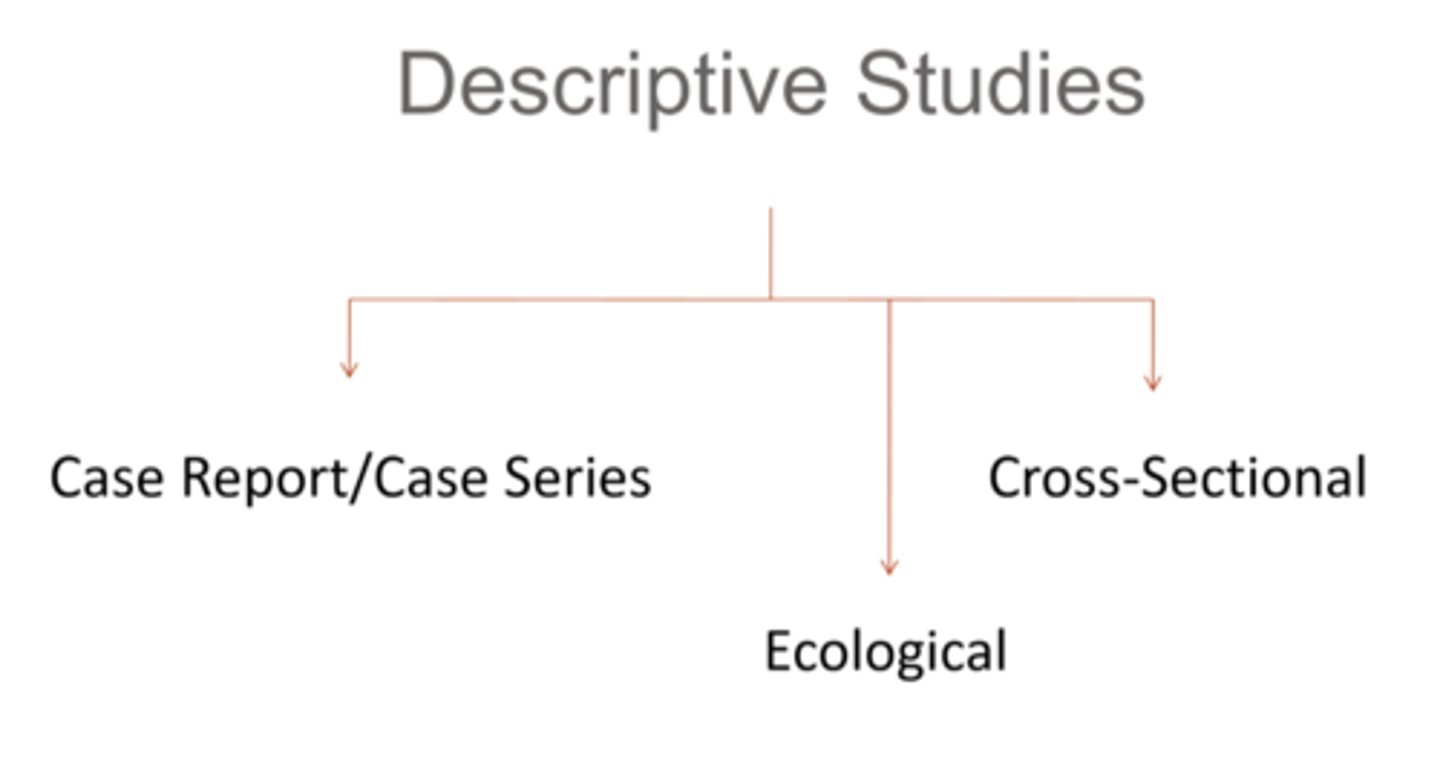
What is a case report/case series desriptive (observational) study?
documents one or a few unusual medical occurrences
What are some advantages of a case report/case series desriptive (observational) study?
piques interest and raises awareness for a potential problem
What are some disadvantages of a case report/case series desriptive (observational) study?
anecdotal and non-scientific
no comparison group
What is a meta-analysis / systematic review?
summarizes multiple studies (even if they are conflicting) to draw a deduction or determine an overall trend
How do we perform a meta-analysis?
1. decide exclusion and inclusion criteria for studies
2. find all relevant studies
3. extract required info
4. do the meta statistics
5. interpret results

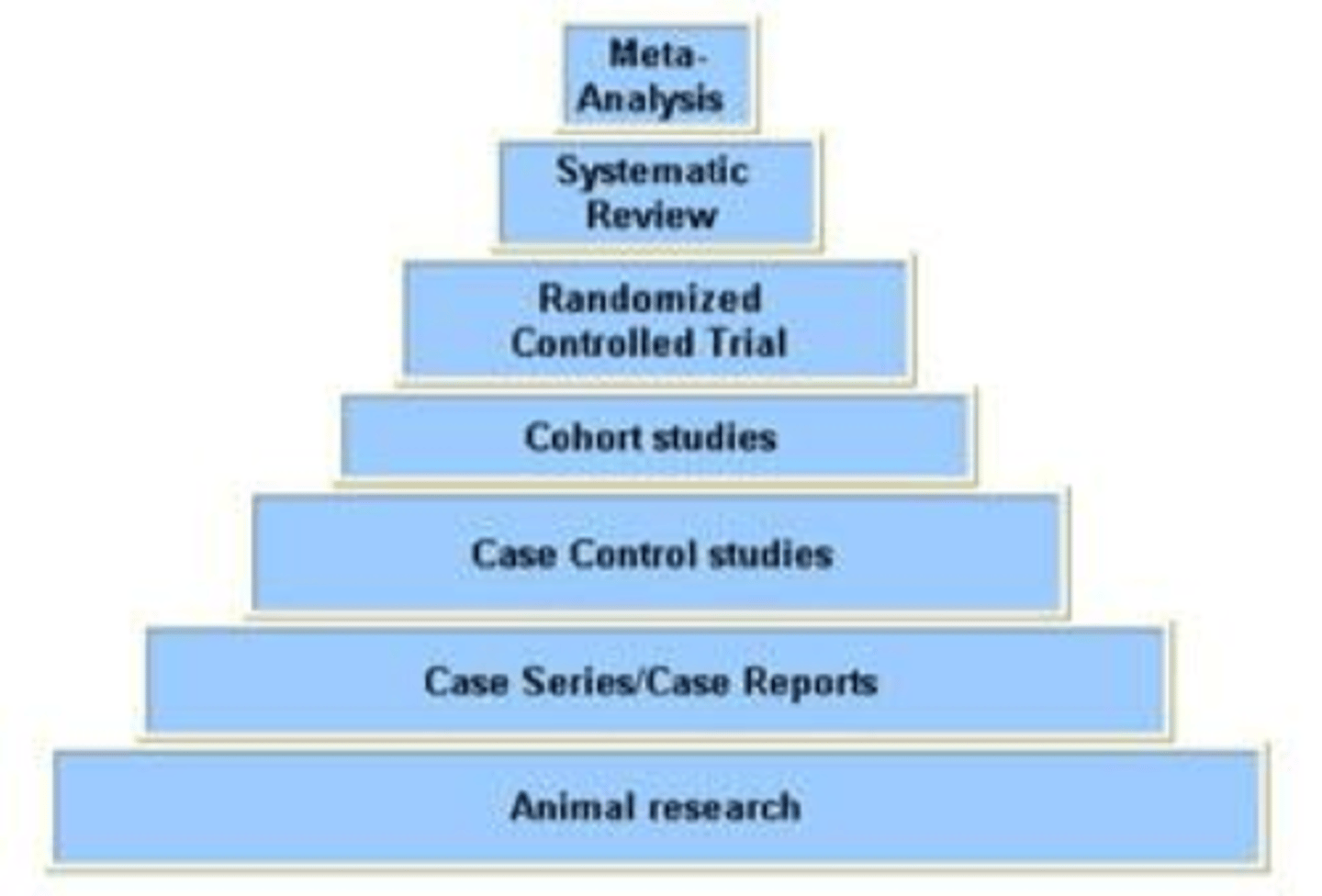
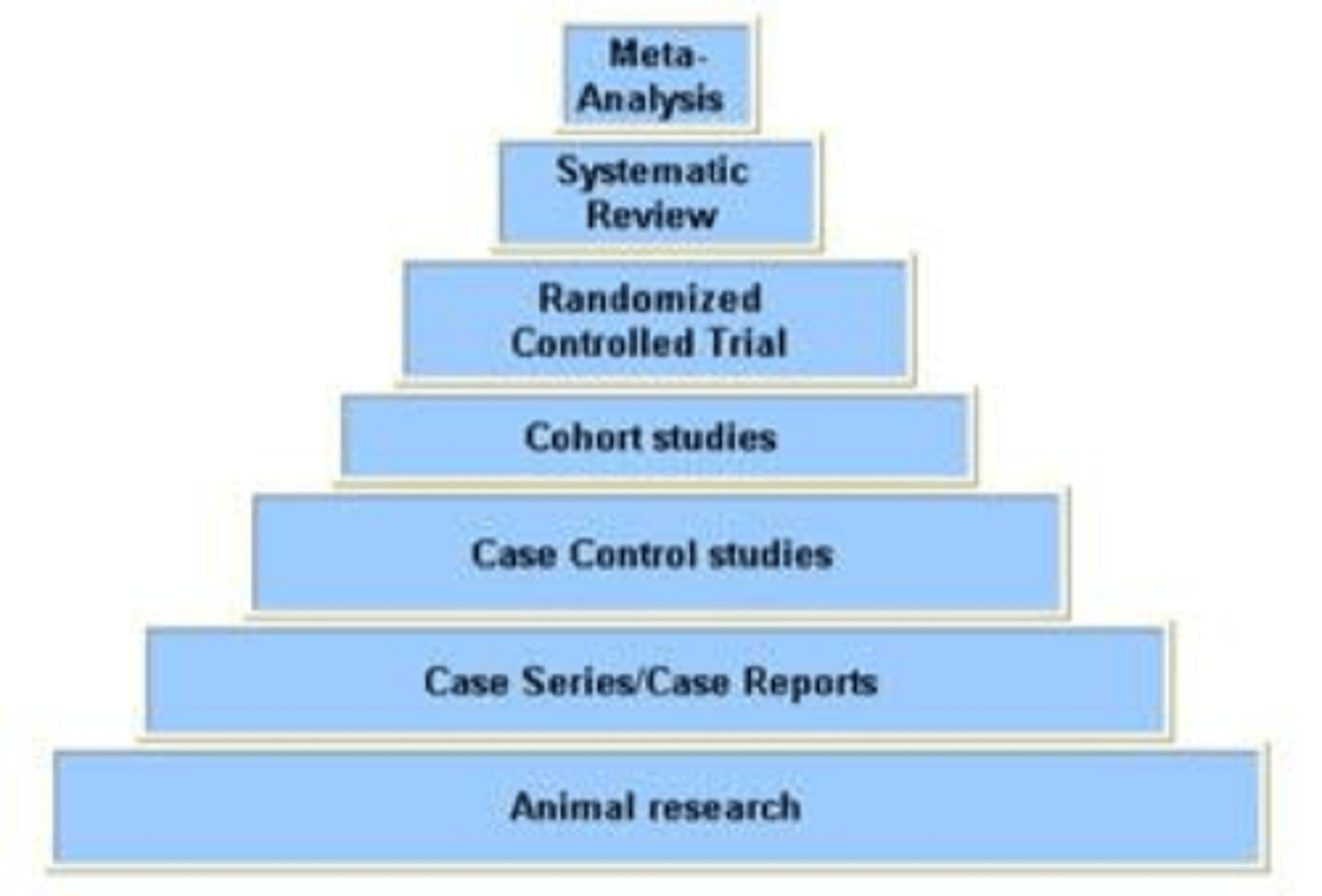
What is the hierarchy of study strength?
meta-analysis
systematic review
RCT
cohort studies
case control studies
case reports
animal research
What types of studies get a grade A for study design strength?
meta-analysis
systemiatic review
RCT
diagnostic studies that have a wide population, good reference standard, no case control studies
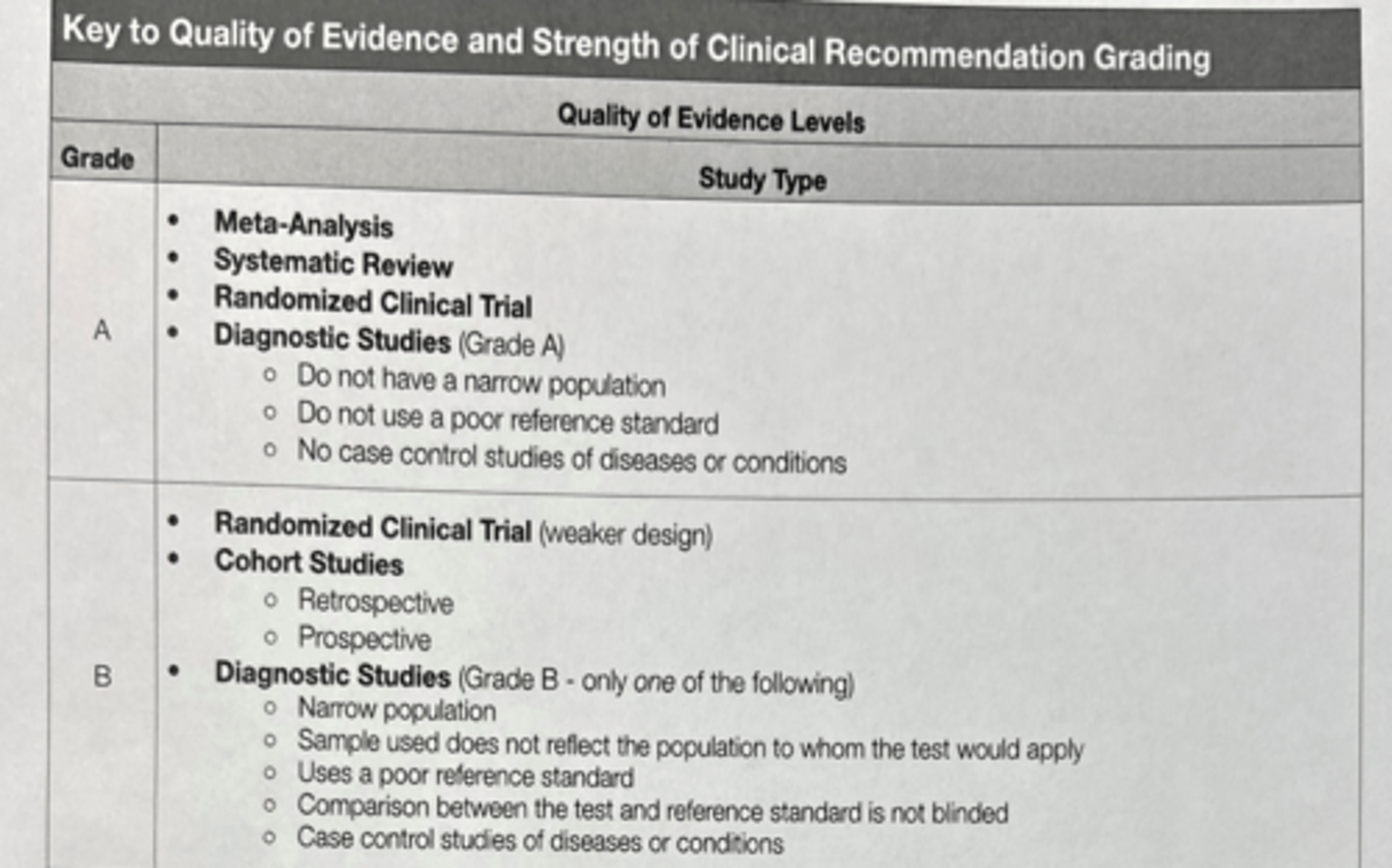
What types of studies get a grade B for study design strength?
RCT with weaker design
cohort studies (retrospective or prospective)
diagnostic studies that have ONE of narrow population, sample doesn't reflect population, poor reference standard, NOT blinded, may use case control studies
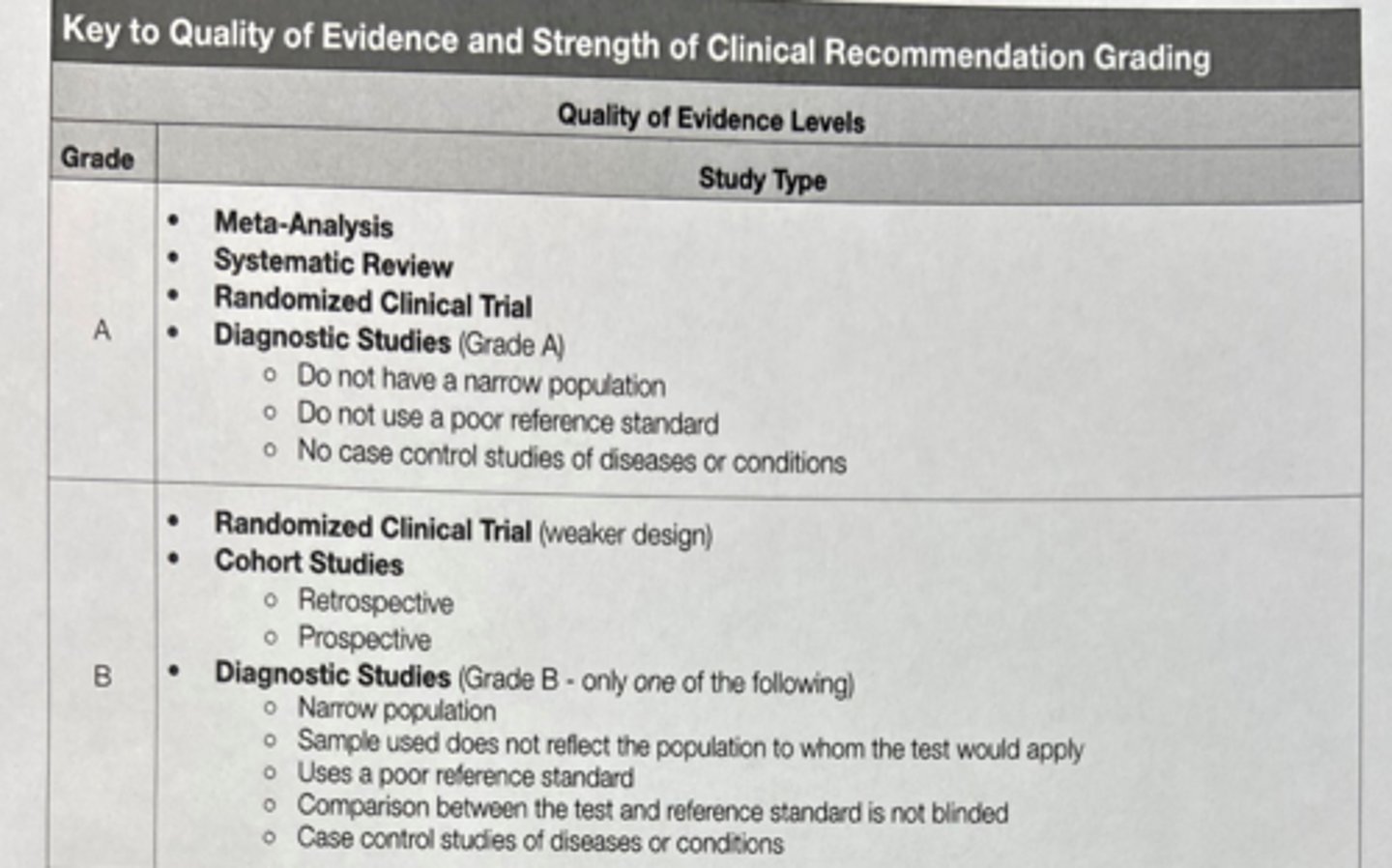
What types of studies get a grade C for study design strength?
case control studies (retrospective or prospective)
diagnostic studies that have TWO+ of narrow population, sample doesn't reflect population, poor reference standard, NOT blinded
strong study designs but with substantial uncertainty about conclusions or doubts about generalizations, bias, research design, sample size
nonrandomized trials
What types of studies get a grade D for study design strength?
cross sectional studies
case reports/series
reviews
position papers
expert opinion
reasoning from principle
What is absolute risk?
risk of a health event happening over a certain time period, reflecting the overall public health impact of the risk factor
How do we calculate absolute risk?
# of health events in a population / total populations at risk
What is relative risk?
risk of experiencing a health event based on group membership, reflecting how strong the association is between factor and disease
How do we calculate relative risk?
risk of population A / risk of population B
What does it mean if relative risk is 1 or >1?
RR > 1 = population A has a higher risk
RR = 1 = risk is equal between populations
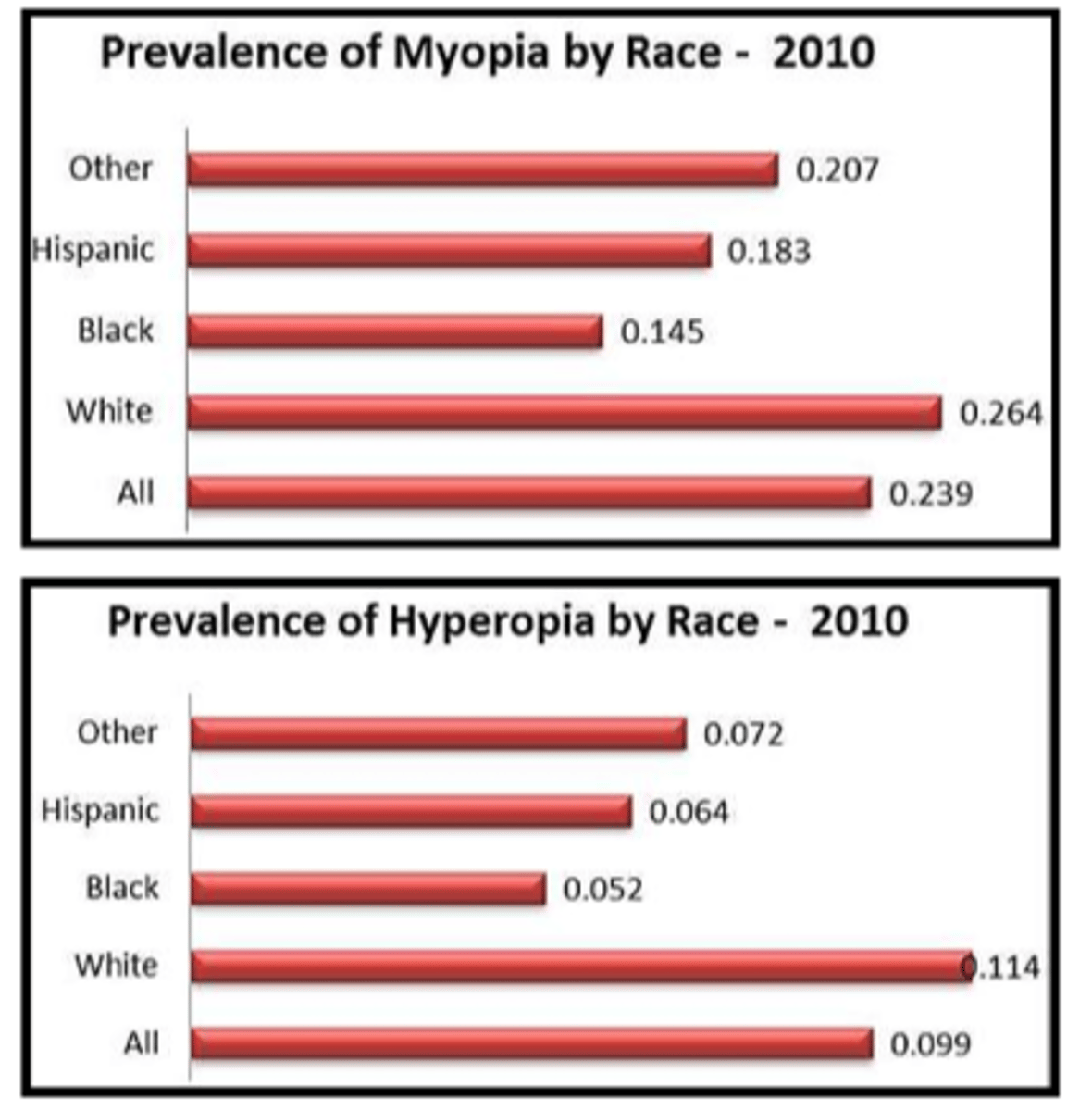
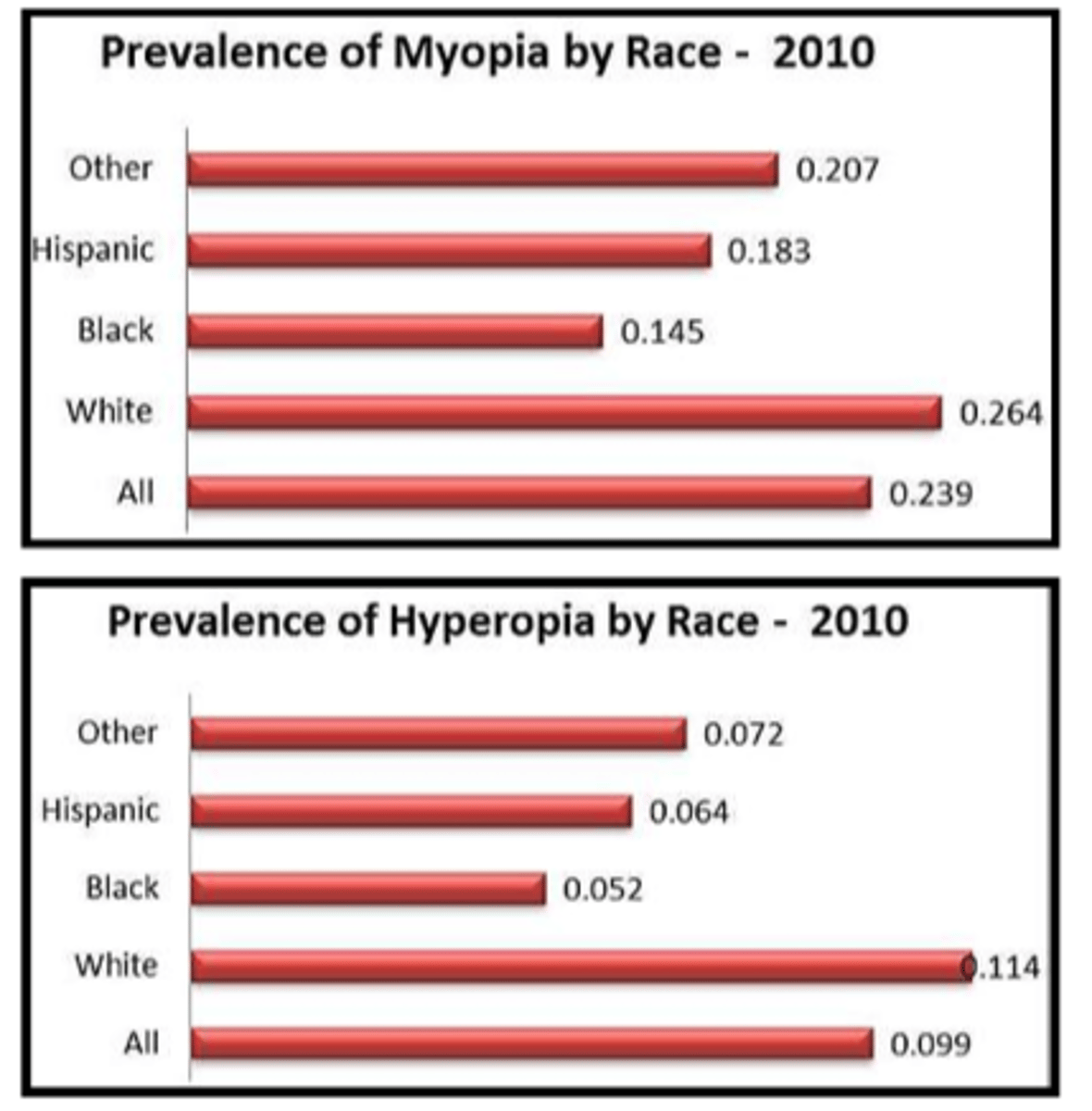
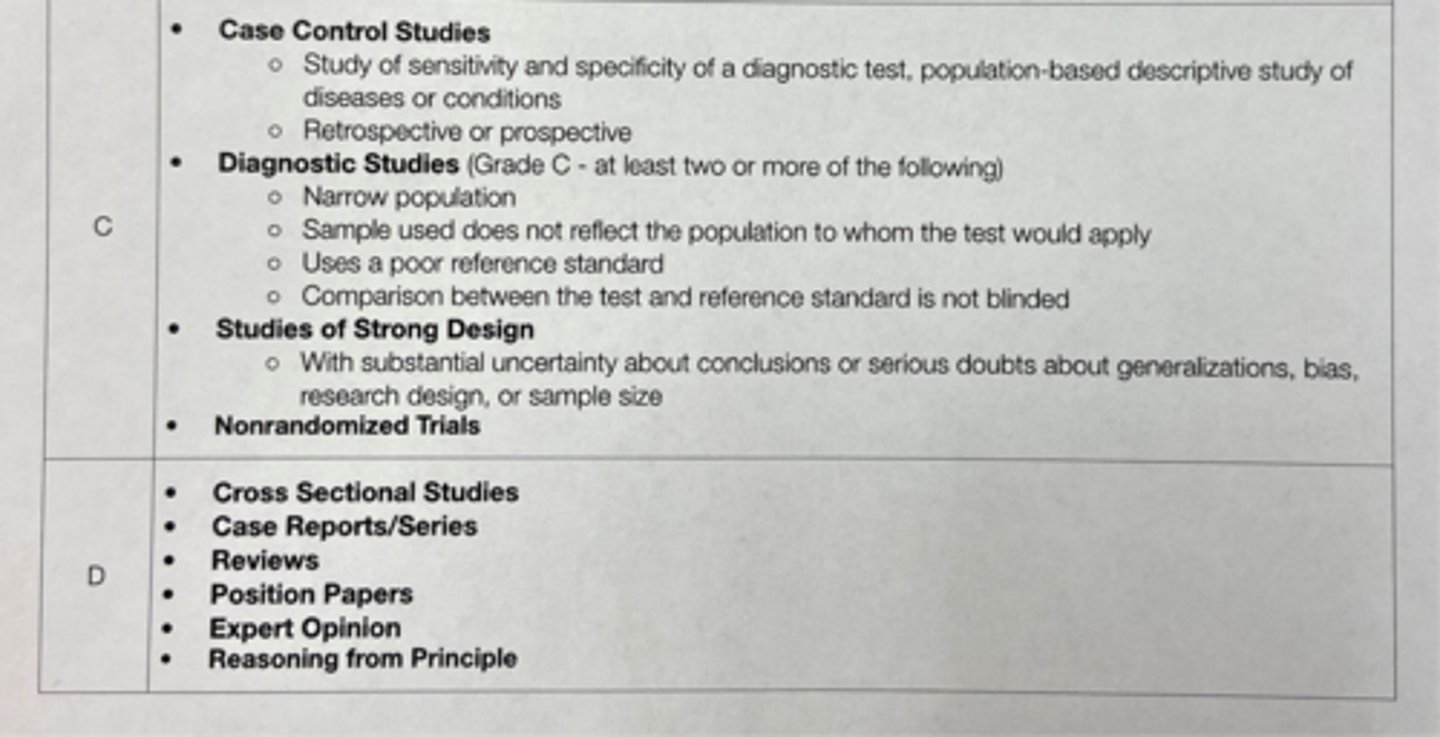
How do these graphs show the difference between prevalence and relative risk?
prevalence = most diabetic ret cases are in white people
relative risk = hispanic people have a higher relative risk of developing AMD
What is morbidity?
reported cases of disease, illness, and disability = shows current health status of population
What is mortality?
# of deaths in a population
What does sporadic mean?
occasional, irregular occurence such as...
food-borne disease
Creutzfeld-Jakob disease
Acanthamoeba keratitis
What does endemic mean?
disease frequency is maintained without external inputs such as...
cataracts
Rx
common cold
What does epidemic mean?
sudden increase in cases above endemic/baseline level = typically > 1.645 standard dev above seasonal baseline is considered threshold

What are the 2 types of epidemic?
common source = not transmissible like chlorine gas leak, obesity, diabetes, myopia
propogated = transmissible between people like COVID

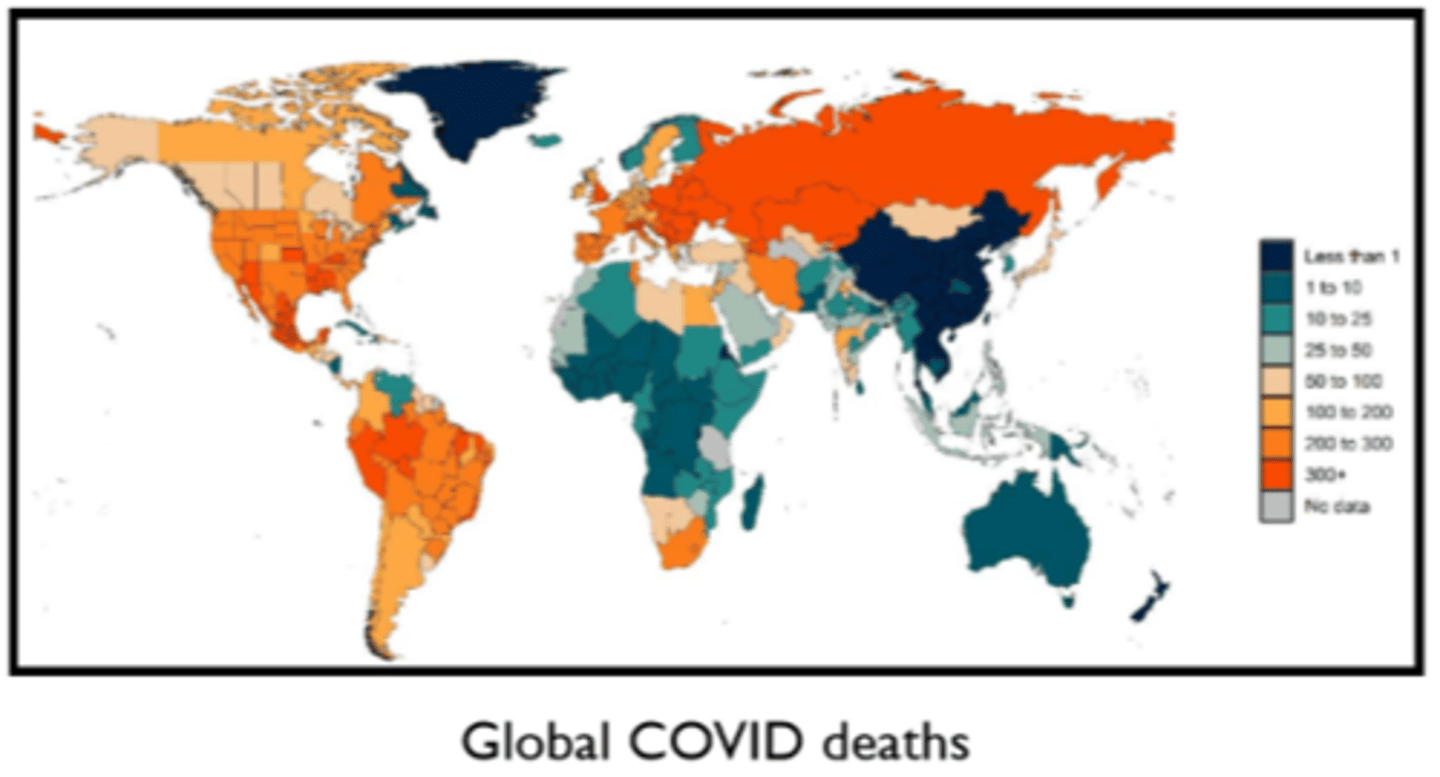
What does pandemic mean?
epidemic affecting a wide area, such as...
HIV
flu in 2009
COVID in 2019
Ex) the statement "14% of people develop PDR after a 20 year duration of DM" is an example of what type of public health measure?
cumulative incidence
Ex) the statement "8.6% of Americans > age 40 with DM have diabetic retinopathy" is an example of what type of public health measure?
prevalence
Ex) the statement "ambulatory eye injuries among US military personnel is 983/100,000 person-years" is an example of what type of public health measure?
incidence rate
Ex) the statement "the risk of retinal detachments in patients with lattice is < 1%" is an example of what type of public health measure?
absolute risk
Ex) the statement "10% of adults > age 60 in the US have ARMD" is an example of what type of public health measure?
prevalence
Ex) the statement "over a 15 year period, 8% of people > 75 years of age have late AMD" is an example of what type of public health measure?
cumulative incidence
Ex) the statement "2.5 million Americans suffer eye injuries annually" is an example of what type of public health measure?
incidence
Ex) the statement "AA are 3.29x more likely to be diagnosed with glaucoma than Caucasians" is an example of what type of public health measure?
relative risk
Ex) the statement "1 in 3 Americans have astigmatism" is an example of what type of public health measure?
prevalence
Ex) the statement "1.08 deaths per 100 million vehicle miles in the US in 2014" is an example of what type of public health measure?
incidence
What was the goal of the Orinda Vision Screening study (1954-1956)?
design the least expensive, least technical and most effective screening program for finding essentially all elementary-school children with vision problems
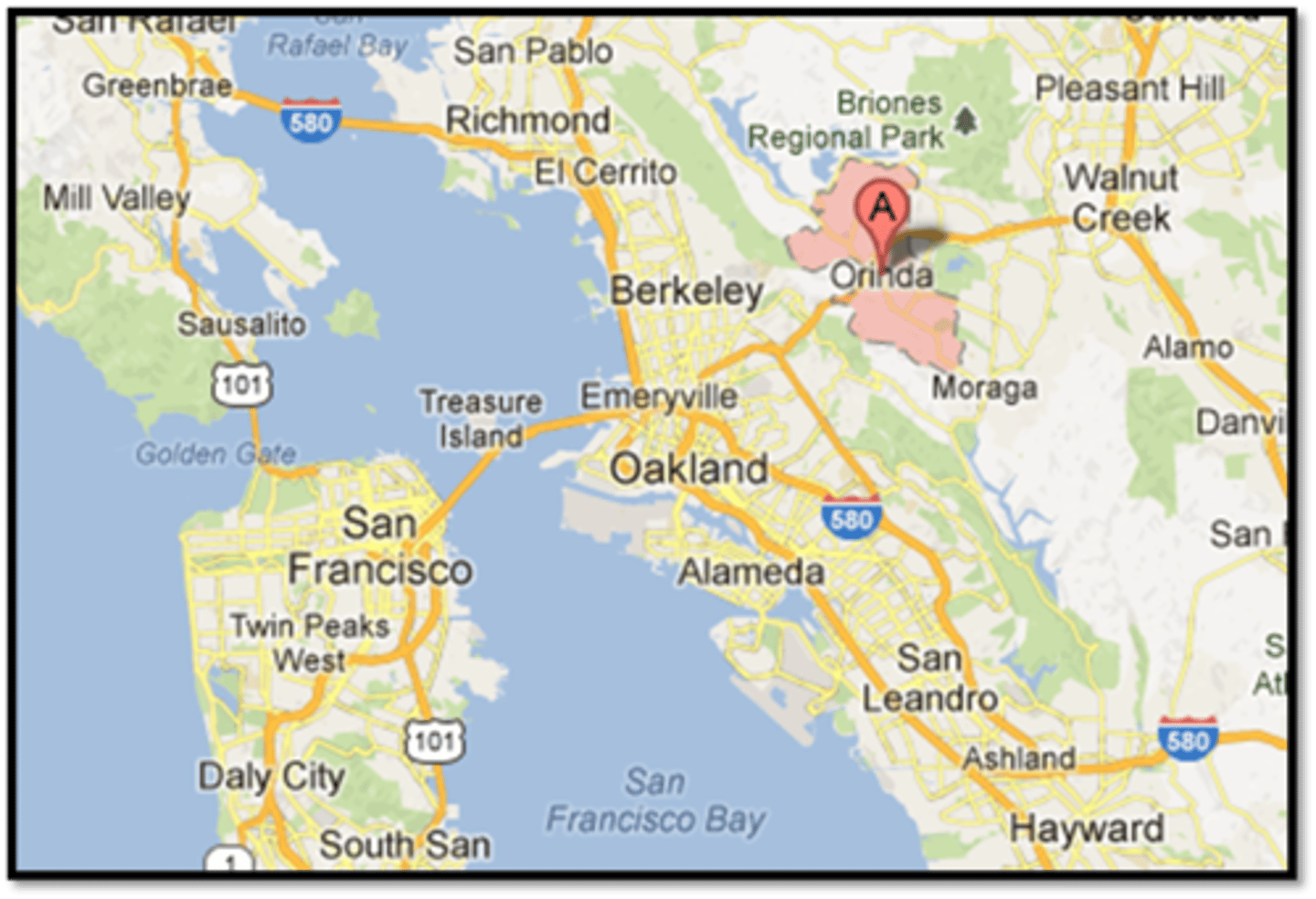
What was the study design of the Orinda Vision Screening study (1954-1956)?
hybrid study design = descriptive epidemiology + retrospective clinical trial
What were the 2 main outcomes of the Orinda Vision Screening study (1954-1956)?
modified clinical technique (MCT) = Snellen VA, retinoscopy with lens rack, CT, DO
>50% of children with previous eye care still failed the screening
What are some weaknesses of the Orinda Vision Screening study (1954-1956)?
not applicable to all populations
must be performed by clinicians, not laypeople
not the cheapest program
does not include visual skills testing
What was the goal of the Vision in Preschoolers study (1997)?
developing evidence-based guidelines for preschool vision screening tests to specificially target amblyopia, strabismus, significant Rx, unexplained reduced VA

What was the study design of the Vision in Preschoolers study (1997)?
experimental with 2 phases

What was phase I of the Vision in Preschoolers study (1997)?
eye care providers = refractive test (ret) and CT with crowded, linear Lea was best to assess strab

What was phase II of the Vision in Preschoolers study (1997)?
lay screeners and nurses = retinomax, suresight + stereo smile with single, crowded Lea was best for strab

What was the goal of the Framingham Eye Survey (1973)?
prevalence data gathered for common eye disease and disorders
What was the study design of the Framingham Eye Survey (1973)?
cross-sectional study with data taken from the original 1st generation heart study (which was a prospective cohort study)
What were the 3 main outcomes of the Framingham Eye Survey (1973)?
vision impairment is lower than initially thought
POAG prevalence is higher that initially thought
eye disease prevalence for other conditions such as CATs, DR, ARMD
What was the goal of the Baltimore Eye Survey (1985-1988)?
evaluation of glaucoma screening tests such as tonometry, VF, stereo fundus photos, PMHx, POHx
What was the study design of the Baltimore Eye Survey (1985-1988)?
prospective, cross-sectional study
What were the 2 main outcomes of the Baltimore Eye Survey (1985-1988)?
risk factors for POAG like race, IOP, HTN, perfusion pressure, FHx, ONH structure
visual impairment increases with age, black race, general health, and SES
What was the goal of the Beaver Dam Eye Study (1988-2008)?
prevalence and incidence of CATs, AMD, DR
What was the study design of the Beaver Dam Eye Study (1988-2008)?
prospective cohort study
What were the 3 main outcomes of the Beaver Dam Eye Study (1988-2008)?
cigarette smoking associated with CATs and AMD
retinal drusen and pigment associated with AMD progression
grading scale images
What was the goal of the Wisconsin Epidemiological Study of Diabetic Ret (1979)?
incidence and progression of diabetic complications
What was the study design of the Wisconsin Epidemiological Study of Diabetic Ret (1979)?
prospective cohort study

What were the 2 main outcomes of the Wisconsin Epidemiological Study of Diabetic Ret (1979)?
DR and kidney disease risk increases if HbA1c > 6.5%
higher BG, smoking, HTN associated with DM complications (retinopathy, nephropathy, neuropathy)

What was the goal of the Los Angeles Latino Eye Study (2000-2010)?
incidence and prevalence of DR, POAG, ARMD, CATs
What was the study design of the Los Angeles Latino Eye Study (2000-2010)?
prospective cohort study
What were the 2 main outcomes of the Los Angeles Latino Eye Study (2000-2010)?
60% of eye disease is undiagnosed in Latino populations
Latinos have highest risk of vision impairment, blindness, and developing DR
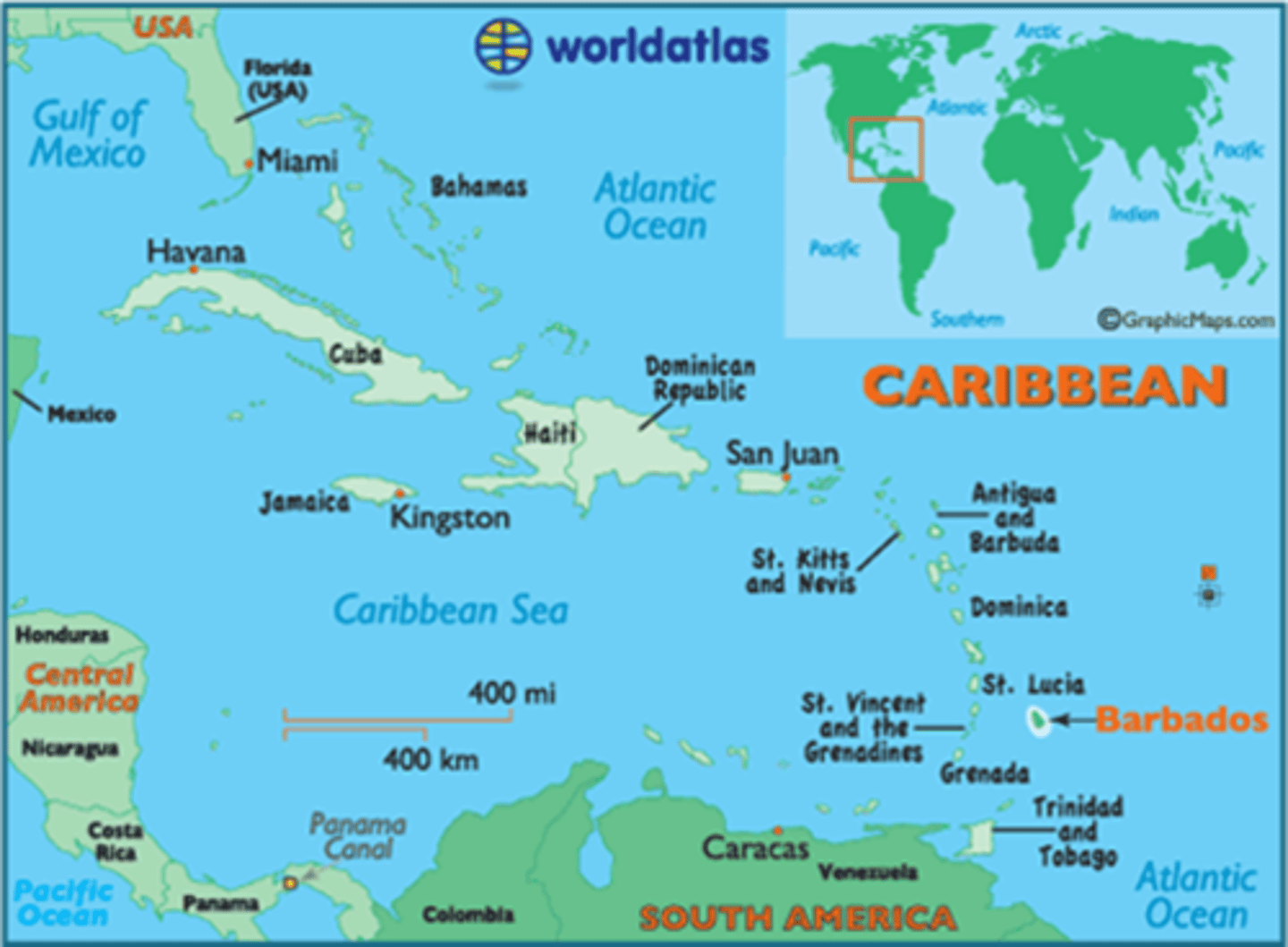
What was the goal of the Barbados Eye Studies (1986-2003)?
incidence, prevalence, and risk factors for POAG, CATs, DR, ARMD
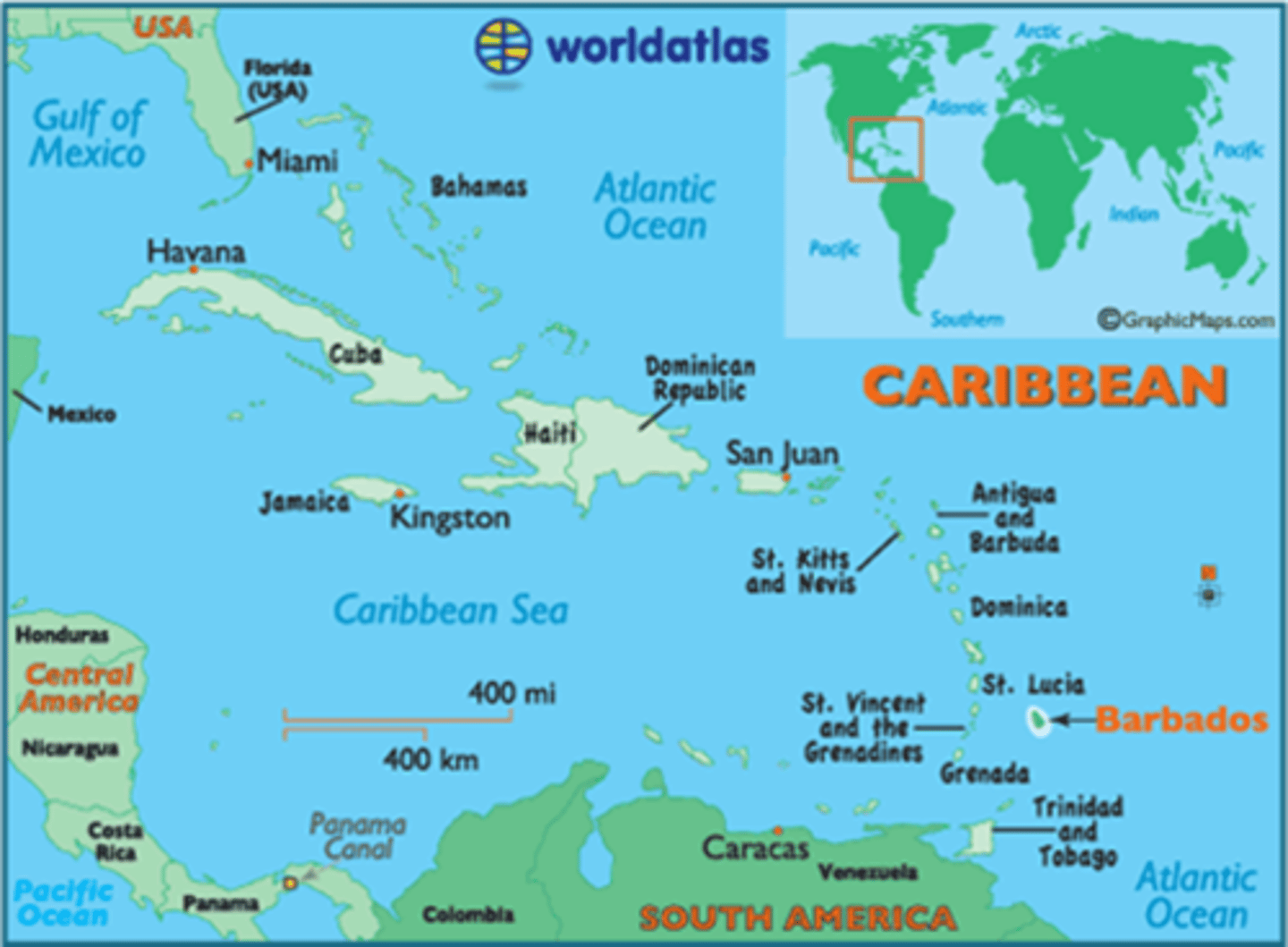
What was the study design of the Barbados Eye Studies (1986-2003)?
simple random sample
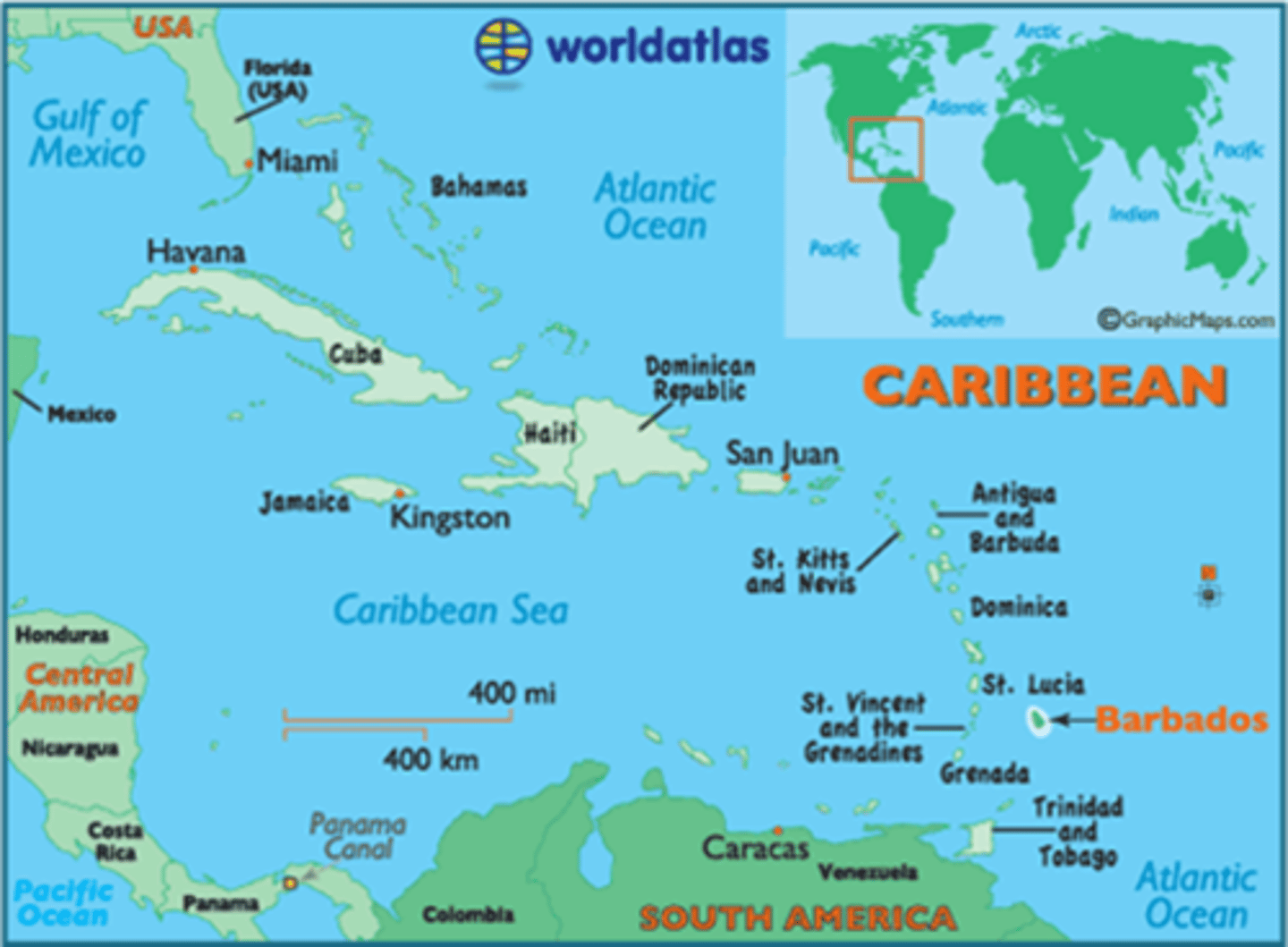
What were the 2 main outcomes of the Barbados Eye Studies (1986-2003)?
highest prevalence of low vision/blindness than elsewhere in the world, largerly due to CATs and POAG
POAG prevalence differed by race, age, gender = older, black, males more affected
What was the goal of the Multi-Ethnic Pediatric Eye Disease study (early 2000s)?
determine prevalence of Rx, strabismus, amblyopia in Baltimore and LA children

What was the study design of the Multi-Ethnic Pediatric Eye Disease study (early 2000s)?
cross-sectional study
