Leukemias and lymphomas 20 study document
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
I. Hematologic Malignancies Overview
Hematologic malignancies are cancers that affect the blood, bone marrow, and lymphatic system.
They include:
1. Leukemias
2. Lymphomas
3. Plasma cell disorders (e.g., multiple myeloma)
Key Diagnostic Tools:
• Clinical presentation
• Morphology
• Immunophenotyping
• Molecular studies
• Cytogenetics
• Bone marrow biopsy and aspiration
II. Leukemias
1. Definition:
• Malignancy of hematopoietic cells starting in the bone marrow
• Can spread to blood, lymph nodes, and organs
• Types by lineage:
o Myeloid
o Lymphoid
• Types by course:
o Acute
o Chronic
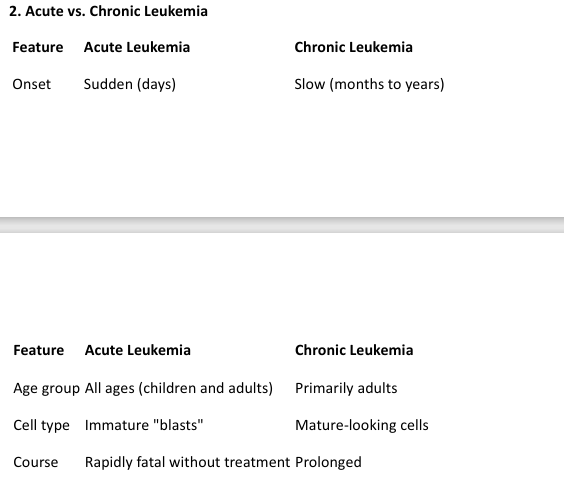
2. Acute vs. Chronic Leukemia A. Pathophysiology
III. Acute Leukemias
A. Pathophysiology
• Malignant clonal proliferation of immature myeloid or lymphoid cells
• Mechanisms:
o Clonal expansion
o Maturation arrest
• Consequences:
o Crowds out normal hematopoiesis
o Organ infiltration
III. Acute Leukemias B. Clinical Features
A. Pathophysiology
• Malignant clonal proliferation of immature myeloid or lymphoid cells
• Mechanisms:
o Clonal expansion
o Maturation arrest
• Consequences:
o Crowds out normal hematopoiesis
o Organ infiltration
III. Acute Leukemias C. Acute Myeloid Leukemia (AML)
• ≥ 20% blasts in marrow/blood for diagnosis
• Presence of Auer rods in cytoplasm of myeloblasts
• Multiple subtypes: M0-M7 (FAB classification)
Important Subtype:
• AML-M3 (Acute Promyelocytic Leukemia):
o Characterized by Faggot cells
o Associated with DIC
o Treated with ATRA (All-trans retinoic acid)
III. Acute Leukemias D. Acute Lymphoblastic Leukemia (ALL)
D. Acute Lymphoblastic Leukemia (ALL)
• Malignancy of lymphoid blasts
• More common in children
• Good prognosis in many pediatric cases
Classification by Immunophenotype:
• B-lineage (Better prognosis)
• T-lineage (Worse prognosis)
Prognostic Factors:
• Better:
o Age 1–10 years
o WBC < 10,000
o Hyperdiploidy
• Worse:
o T-cell origin
o Very high WBC
o <1 or >10 years of age
III. Acute Leukemias E. Treatment of Acute Leukemias
• Chemotherapy
• Bone marrow transplantation
• Prognosis varies:
o Worse in therapy-related AML
o Better in pediatric ALL with favorable cytogenetics
IV. Myelodysplastic Syndromes (MDS)
• Clonal stem cell disorders with ineffective hematopoiesis
• Dysplasia in one or more myeloid lineages
• Risk of progression to AML
• Common in elderly
• Blood findings: Macrocytic anemia, cytopenias
• Bone marrow: Hypercellular with dysplastic features
V. Chronic Leukemias A. Chronic Myeloid Leukemia (CML)
• Age: Adults (25–60 years)
• Genetics: t(9;22) Philadelphia chromosome → BCR-ABL fusion
• Peripheral blood:
o Very high TLC (>100,000/mm³)
o Myelocytes, basophilia, thrombocytosis
• Bone marrow: Hypercellular with granulocytic precursors
Clinical Course:
1. Chronic phase
2. Accelerated phase
3. Blast crisis → resembles acute leukemia
B. Chronic Lymphocytic Leukemia (CLL)
• Most common leukemia in adults in the West
• B-cell origin (CD19+, CD20+, CD23+)
• Smudge cells in peripheral smear
• Often asymptomatic; may present with:
o Fatigue, weight loss
o Recurrent infections
o Autoimmune phenomena: AIHA, ITP
• May transform into:
o Prolymphocytic leukemia
o Richter syndrome → Diffuse large B-cell lymphoma (DLBCL)
VI. Lymphomas A. General Features
VI. Lymphomas
A. General Features
• Malignancy of lymphoid cells, originating in lymph nodes
• May spread to blood, bone marrow, and extranodal sites
• Two broad categories:
1. Hodgkin Lymphoma (HL)
2. Non-Hodgkin Lymphoma (NHL)
VII. Hodgkin Lymphoma (HL)
A. Definition and Features
• Characterized by presence of Reed-Sternberg (RS) cells in a reactive inflammatory
background
• Arises in a single lymph node region, spreads contiguously
• Less commonly involves extranodal sites
• Associated with EBV in some subtypes
B. Subtypes (WHO Classification)
B. Subtypes (WHO Classification)
1. Nodular sclerosis (65–75%)
o Most common
o Features Lacunar cells
o Frequent in young adults, especially females
o Involves cervical, supraclavicular, and mediastinal nodes
o Excellent prognosis
2. Mixed cellularity (25%)
o Numerous classic RS cells, abundant inflammatory background
o More common in older males
o Often presents with B symptoms
o Intermediate prognosis
3. Lymphocyte-rich
o Many lymphocytes, few RS cells
o Good prognosis
4. Lymphocyte-depleted
o Few lymphocytes, many RS cells
o Worst prognosis
5. Lymphocyte-predominant (non-classical)
o "Popcorn" cells (L&H variants)
o Often in young males
o Indolent, good prognosis
C. Reed-Sternberg Cells
C. Reed-Sternberg Cells
• Classic RS: large (15–45 microns), binucleated or bilobed, "owl’s eye" nucleoli
• Variants:
o Mononuclear RS cell
o Lacunar RS cell (Nodular sclerosis)
o L&H cell (Lymphocyte predominant)
o Mummified RS cell (degenerative)
D. Spread and Staging
D. Spread and Staging
• Predictable spread pattern: lymph nodes → spleen → liver → marrow → extranodal sites
Ann Arbor Staging:
• I: One LN region or single extranodal site
• II: Two or more LN regions on same side of diaphragm
• III: LN regions on both sides of diaphragm ± spleen
• IV: Disseminated involvement (e.g., liver, marrow)
VIII. Non-Hodgkin Lymphoma (NHL)
VIII. Non-Hodgkin Lymphoma (NHL)
A. General Characteristics
• More heterogeneous than HL
• Often presents with multiple peripheral nodes, extranodal involvement
• Non-contiguous spread
• Higher association with immunodeficiency (e.g., AIDS)
VIII. Non-Hodgkin Lymphoma (NHL) B. Classification
B. Classification
• Origin:
o ~85% are B-cell lymphomas
o ~15% are T-cell/NK-cell lymphomas
• Based on:
o Cell of origin
o Morphology
o Immunophenotype
o Genetic abnormalities
C. Common B-cell NHL Subtypes:
C. Common B-cell NHL Subtypes:
1. Follicular lymphoma
o Most common indolent NHL in the U.S.
o Originates from germinal center B-cells
o t(14;18) → BCL2 overexpression
o Slow-growing; may transform to DLBCL
2. Diffuse large B-cell lymphoma (DLBCL)
o Most common aggressive NHL
o Rapidly enlarging mass
o Treatable with chemo (R-CHOP)
3. Mantle cell lymphoma
o Older males
o t(11;14) → Cyclin D1 overexpression
4. Marginal zone lymphoma
o Associated with chronic inflammation
▪ e.g., H. pylori (MALT lymphoma)
5. Burkitt lymphoma
o Highly aggressive
o t(8;14) → c-MYC activation
o Associated with EBV
o “Starry-sky” appearance
6. Small lymphocytic lymphoma (SLL)/CLL
o Same disease as CLL, but with low peripheral lymphocytosis
D. T-cell and NK-cell Lymphomas:
D. T-cell and NK-cell Lymphomas:
• Less common, often aggressive
• Examples:
o Adult T-cell leukemia/lymphoma (HTLV-1)
o Mycosis fungoides/Sezary syndrome
o Anaplastic large cell lymphoma
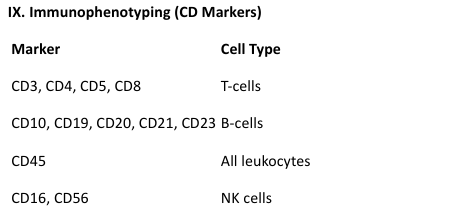
IX. Immunophenotyping (CD Markers)
X. Plasma Cell Neoplasms
X. Plasma Cell Neoplasms
A. Multiple Myeloma
• Malignancy of plasma cells in bone marrow
• Produces monoclonal immunoglobulin (M protein)
• Bone destruction → lytic lesions
Clinical Features: CRAB
• Calcium elevation (hypercalcemia)
• Renal insufficiency
• Anemia
• Bone pain, lytic lesions
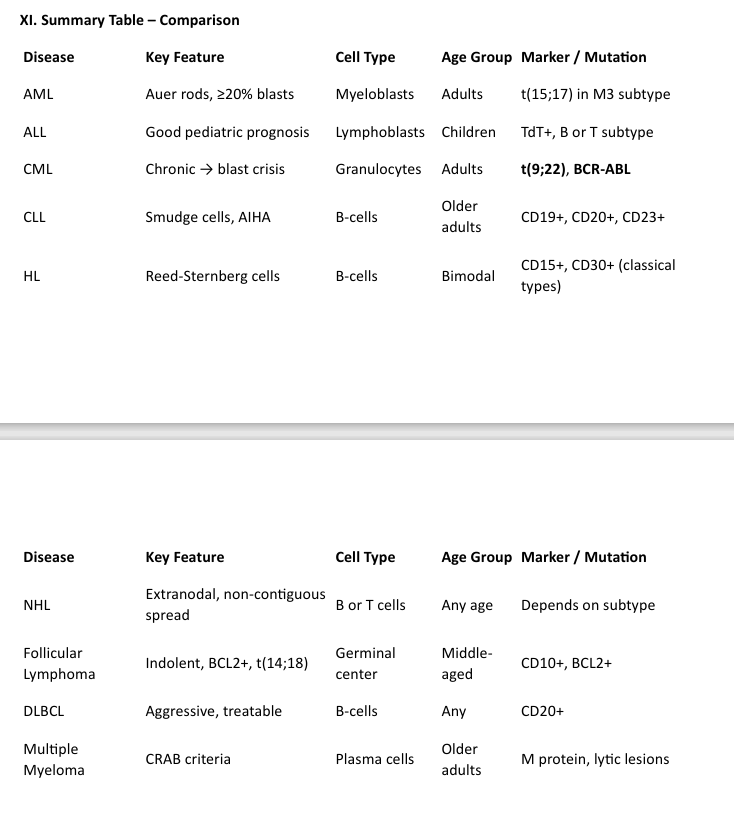
XI. Summary Table – Comparison of leukemias and lymphomas