Hemostasis: Laboratory Assessment
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
129 Terms
What type of tube is used for collecting specimens with sodium citrate as an anticoagulant?
A light blue top tube
What is the concentration of sodium citrate used in the light blue top tube?
3.2%.
What is the ideal blood to anticoagulant ratio in a blue top tube?
9:1
How much blood and anticoagulant should be in a standard light blue top tube?
It contains 2.7 mL of blood and 0.3 mL of sodium citrate.
What volume of blood and anticoagulant is used in a smaller light blue top tube?
A smaller tube contains 1.8 mL of blood and 0.2 mL of sodium citrate.
What hematocrit value is the 9:1 ratio based on?
on a normal hematocrit of 45%.
What happens if a sample is short (e.g., less than 2.7 mL in a standard tube)?
A short sample results in excess anticoagulant, which can prolong test results.
Why can a high hematocrit affect the test results when using a blue top tube?
A high hematocrit (greater than 55%) reduces plasma volume, leading to excess anticoagulant relative to plasma and potentially prolonging test results.
What can happen if a blue top tube is under-filled?
Under-filling a blue top tube can prolong both PT (Prothrombin Time) and APTT (Activated Partial Thromboplastin Time).
How much should a standard blue top tube be filled to avoid test inaccuracies?
It should be filled to at least 2.7 mL.
What is the minimum required volume for a smaller blue top tube?
At least 1.8 mL of blood is required.
What is the impact of under-filling on a long PT or APTT result?
A long PT or APTT can become significantly longer than the true value if the tube is under-filled.
How is a normal PT or APTT affected by under-filling?
A normal PT or APTT may be only slightly prolonged if the tube is under-filled.
How is the bleeding time test performed?
It is performed by making a small incision on the forearm and wicking away the blood while timing how long it takes for bleeding to stop.
What is the average bleeding time in control subjects?
Approximately 3.5 minutes, with a range of 2 to 9 minutes.
What does a prolonged bleeding time indicate?
It may indicate qualitative or quantitative platelet defects.
What are the different methods used for bleeding time tests?
Duke (earlobe), Ivy (forearm), and Mielke (forearm) methods.
Bleeding Time Test
It is widely used to diagnose hemostatic dysfunction, von Willebrand’s disease, and vascular disorders.
Why is the bleeding time test performed before surgery?
It is used to screen for platelet abnormalities that could increase the risk of bleeding during or after surgery.
How is the tourniquet test performed?
A blood pressure cuff is applied to the forearm and inflated to 80–100 mm Hg for 5 minutes to increase pressure in small vessels.
What indicates a positive or abnormal result in the tourniquet test?
The appearance of petechiae (small red or purple spots) indicates an abnormal result, suggesting fragile vessels.
What conditions are associated with abnormal tourniquet test results?
Abnormal results can be seen in vascular purpura (due to vessel weakness) and in platelet defects.
What is the normal range for petechiae on the forearm after the bleeding test?
Less than 10 petechiae on the forearm 5 minutes after the test is considered normal or negative.
How many petechiae on the anterior forearm correspond to a score of 1+?
few petechiae on the anterior forearm.
What score corresponds to having many petechiae on the anterior forearm?
A score of 2+
What does a score of 3+ represent in terms of the number of petechiae?
many petechiae on the whole arm and top of the hand.
What is the highest score on the scale, and what does it represent?
The highest score is 4+, and it represents confluent petechiae on all areas of the arm and top of the hand.
What is considered a positive result in the petechiae test?
More than 10 petechiae on the forearm is considered a positive result.
What is the purpose of adding an aggregating agent to platelet-rich plasma (PRP)?
to induce platelet shape change and aggregation.
What is used to measure platelet aggregation in an aggregation study?
An aggregometer, which works similarly to a spectrophotometer, is used to measure optical changes and plot the graph during platelet aggregation.
How does platelet aggregation affect light transmission in a platelet suspension?
Platelet aggregation allows more light to be transmitted through the suspension.
What causes immune thrombocytopenias?
antibodies against platelet antigens.
How is platelet retention tested using whole blood and glass beads?
Whole blood is passed through a column of glass beads, and normal platelets in the presence of von Willebrand factor (vWF) will adhere to the beads.
What happens to the platelet count in the platelet retention test?
The platelet count is reduced by about 75%
What is the role of aggregating agents in aggregation studies?
they cause different aggregation patterns in platelets.
What are some examples of aggregating agents used in platelet aggregation studies?
ADP, collagen, epinephrine, ristocetin, thrombin, thromboxane, and arachidonic acid.
How does ristocetin induce platelet aggregation?
Ristocetin, a glycopeptide antibiotic isolated from Nocardia lurida, induces platelet aggregation by initiating the binding of von Willebrand factor (vWF) to platelet glycoprotein Ib.
What causes the primary wave of platelet aggregation?
It is due to the direct action of the aggregating agent on the platelets.
What causes the secondary wave of platelet aggregation?
It is due to thromboxane A2 synthesis and secretion from platelets.
Which aggregating agents induce a monophasic curve (single wave of aggregation)?
Collagen, arachidonic acid, and ristocetin
What is the platelet aggregation pattern in Bernard Soulier syndrome?
the platelet aggregation is normal with ADP, epinephrine, collagen, and arachidonic acid but deficient with ristocetin.
What is the platelet aggregation pattern in Glanzmann's thrombastenia?
platelet aggregation is deficient with ADP, epinephrine, collagen, and arachidonic acid but normal with ristocetin.
How does the platelet aggregation pattern in Storage pool defect appear?
there is a primary wave with ADP and epinephrine, normal with arachidonic acid, deficient with collagen, and normal with ristocetin.
What is the platelet aggregation pattern in Aspirin-like defect?
there is a primary wave with ADP and epinephrine, deficient with arachidonic acid, deficient with collagen, and normal with ristocetin.
What is the platelet aggregation pattern in von Willebrand disease?
platelet aggregation is normal with ADP, epinephrine, collagen, and arachidonic acid but deficient with ristocetin.
What is the process of clot retraction?
Clot retraction is driven by outside-in signaling by platelet integrin αIIbβ3, which causes the contraction of the fibrin mesh. This results in the clot becoming smaller and excess fluid being extruded.
What is the function of fibrin in clot formation?
Fibrinogen is converted to fibrin at the injury site, forming fibrin threads that trap platelets and red blood cells to create a plug at the site of injury, consolidating the developing platelet thrombus.
How does clot retraction help in wound healing?
Clot retraction helps by drawing the edges of the damaged tissue together and forming a mechanically stable clot, which supports the healing process.
Under what conditions does clot retraction occur normally?
if platelet number and function are adequate, with the clot retracting from the test tube surface when incubated at 37°C.
What does a clot retracting from the surface of a test tube indicate?
that platelet number and function are normal.
Is the Clot Retraction Test a sensitive or insensitive test?
is a crude and insensitive test.
How can hemostasis laboratory tests be categorized?
Screening Tests and Diagnostic Tests.
What are screening tests in hemostasis testing?
functional end-point assays where a patient sample (plasma or whole blood) is incubated with exogenous reagents that activate the coagulation cascade. The time until clot formation is measured and compared to a standard clotting time to assess the patient's hemostatic status.
What is the purpose of screening tests in hemostasis?
The purpose of screening tests is to provide a standard measurement of the patient’s hemostatic status by comparing their clotting time to that of pooled normal plasma or whole blood.
What are some examples of screening tests in hemostasis?
Prothrombin Time Test (PT)
Activated Partial Thromboplastin Time Test (APTT)
Activated Clotting Time Test (ACT)
Thrombin Clotting Time Test
What does the clotting time measured in screening tests indicate?
how long it takes for clot formation to occur in the patient's sample, and this is compared to the clotting time of pooled normal plasma or whole blood to assess the patient's coagulation status.
What type of test is used for diagnostic purposes in hemostasis?
they are typically more complex and are used to investigate specific coagulation disorders, though the exact tests may vary depending on the condition being investigated.
What does Prothrombin Time (PT) measure
the tissue factor–induced coagulation time of blood or plasma.
Which coagulation pathways does the PT test evaluate?
the extrinsic and common coagulation pathways and is sensitive to coagulation factors I (fibrinogen), II (prothrombin), V, VII, and X.
How is the PT test performed?
by adding reagent thromboplastin and calcium (Ca2+) to a patient sample and measuring the time it takes for clot formation.
What is the normal range for Prothrombin Time (PT)?
10-14 seconds.
What could a prolonged PT indicate?
the presence of an inhibitor to, or a deficiency in one or more of the coagulation factors of the extrinsic or common pathway.
What conditions can cause a prolonged PT?
warfarin therapy, those with vitamin K deficiency, or individuals with liver dysfunction.
What is the primary use of PT in clinical practice?
to monitor oral anticoagulation therapy, such as warfarin therapy.
What is the purpose of the International Normalized Ratio (INR)?
calculated to standardize the Prothrombin Time (PT) across different reagents of varying sensitivity, ensuring consistency in results regardless of the thromboplastin used.
How is the INR calculated?
by taking the PT ratio (the ratio of patient PT to pooled normal PT) raised to the power of the International Sensitivity Index (ISI).
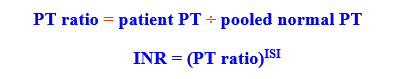
What is the role of the International Sensitivity Index (ISI) in INR calculation?
used to characterize the sensitivity of the thromboplastin used in the PT test. Sensitive thromboplastins have a low ISI, and the ISI is both instrument-dependent and reagent-dependent.
What does the PT ratio represent in the INR formula?
the ratio of the patient’s PT to the pooled normal PT.
Why is the ISI important in the INR calculation?
because it reflects the sensitivity of the thromboplastin, which can vary and affect the PT. It helps standardize the INR across different laboratories and reagents.
What is the relationship between the ISI and thromboplastin sensitivity?
Sensitive thromboplastins have a low ISI, while less sensitive thromboplastins have a higher ISI. The ISI affects the calculation of the INR.
Why must each laboratory calibrate the ISI for their own instruments and reagents?
because the sensitivity of thromboplastin can vary depending on the instrument and reagent, which can affect the accuracy and standardization of the INR.
How does an increase in the International Sensitivity Index (ISI) affect thromboplastin sensitivity?
An increase in the ISI from 1.0 to 2.0 decreases the sensitivity of the thromboplastin by more than half.
What is the ideal therapeutic range for INR?
2.0 and 3.0.
How can heparin therapy affect the INR?
It can falsely increase the INR, which may lead to inaccurate results.
What INR range is considered therapeutic for patients on warfarin sodium?
An INR range of 2.0 to 3.0
What does an INR value under 2.0 indicate?
minimal bleeding risk.
What are the potential risks associated with an INR of 3.0 to 4.5?
increased risk of excessive bleeding.
How often is the INR checked in patients on anticoagulation therapy?
every 4-6 weeks
What does the Activated Partial Thromboplastin Time (APTT) test evaluate?
the intrinsic coagulation pathway, which includes factors I, II, V, VIII, IX, X, XI, and XII.
How is the APTT test performed?
using a plasma sample, in which the intrinsic pathway is activated by the addition of phospholipid, an activator (such as ellagic acid, kaolin, or micronized silica), and calcium (Ca2+).
What complexes are formed during the APTT test?
Xase and prothrombinase complexes on the surface of the phospholipid enables prothrombin to be converted into thrombin, which leads to clot formation.
What does the APTT test measure?
measures the time (in seconds) required for clot formation after the activation of the intrinsic coagulation pathway.
What is the normal range for the APTT test?
26-38 seconds.
What are some uses of the APTT test?
used to assess the overall competence of a patient's coagulation system, as a preoperative screening test for bleeding tendencies, and as a routine test for monitoring heparin therapy.
What is the therapeutic range for APTT when monitoring heparin therapy?
1.5 to 2.0 times the normal APTT value, which corresponds to 38-76 seconds.
How is the Activated Clotting Time (ACT) test different from the APTT test?
The ACT test resembles the APTT test but is performed using fresh whole blood samples instead of plasma.
What is the primary use of the ACT test?
used to monitor heparin therapy, particularly in settings where immediate results are needed.
Where is the ACT test typically performed?
outside the core laboratory and is considered a point-of-care test.
What does the Thrombin Clotting Time (TCT) test measure?
measures the rate of a patient's clot formation compared to that of a normal plasma control.
How is the Thrombin Clotting Time (TCT) test performed?
by adding a standard amount of thrombin to a patient's plasma (which has been depleted of platelets) and measuring the time required for a clot to form.
What is the primary use of the Thrombin Clotting Time (TCT) test?
as an aid in the diagnosis of disseminated intravascular coagulation (DIC) and liver disease.
What is the normal range for the Thrombin Clotting Time (TCT) test?
15-22 seconds.
What does the Fletcher test (Prekallekrein, PK) evaluate?
the presence of a Prekallikrein (PK) deficiency.
How is the Fletcher test different from the standard aPTT test?
is a modified version of the aPTT, with a 60-minute incubation time instead of the typical 3-5 minutes used in a standard aPTT.
What happens in the Fletcher test if the patient is deficient in Prekallikrein (PK)?
If the patient is deficient in PK, the increased aPTT result will correct with the longer 60-minute incubation time, indicating PK deficiency.
What does the Reptilase test evaluate?
is used to assess fibrinogen (factor I) levels.
How does Reptilase work in the clotting process?
Reptilase mimics thrombin by cleaving fibrinogen to form fibrin.
Why is the Reptilase test useful in certain conditions?
It is not sensitive to heparin, making it useful to detect the presence of heparin in a specimen with a prolonged aPTT or thrombin time.
What is Protamine Sulfate (PS) and how is it used in testing?
It is a cationic protein extracted from salmon sperm. It is used to neutralize heparin (both unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH)) and can help in the management of anticoagulation after surgeries like heart surgery.
What is the primary use of Protamine Sulfate in clinical practice?
It is primarily used after heart surgery to neutralize heparin, which helps decrease the activated partial thromboplastin time (aPTT) and Activated Clotting Time (ACT), shortening the time to normal coagulation levels.