Clinical features of: – Degenerative diseases of the spinal cord of dogs • Intervertebral disc disease (IVDD) • Cervical spondylomyelopathy (CSM) • Degenerative lumbosacral stenosis (DLSS) (also known as cauda equina syndrome) • Canine degenerative myelopathy (DM) – Other types of disc disease • Acute non-compressive nucleus pulposus extrusion (ANNPE) • Hydrated nucleus pulposus extrusion (HNPE) • Fibrocartilaginous embolism (FCE
Degenerative diseases of the spinal cord of dogs includes 4
Intervertebral disc disease (IVDD)
Cervical spondylomyelopathy (CSM)
Degenerative lumbosacral stenosis (DLSS) (also known as cauda equina syndrome)
Canine degenerative myelopathy (DM)
Other types of disc disease
Acute non-compressive nucleus pulposus extrusion (ANNPE) • Hydrated nucleus pulposus extrusion (HNPE) • Fibrocartilaginous embolism (FCE)
Intervertebral disc – normal anatomy
Intervertebral disc : present between all vertebrae except C1-2. (C1-2 synovial joint instead)
2 components:
Nucleus pulposus: inner component, gelatinous in young normal animals
Annulus fibrosus: outer layer, fibrous, ventral portion thicker than dorsal
Intercapital ligament – between rib head on either side of vertebrae, T2 to T10
cover annulus fibrosus dorsally to reinforce, IVDD unusual in these locations
IVDD— normal anat
is the lack of IVD in C1/C2 normal?
No disc at C1-2 is normal as it is a synovial joint
IVDD - Pathogenesis
describe
3 main factors
what will genetic predispose animal to IVDD
Degeneration of the intervertebral disc (multifactorial)—> mineralisation/ whitening of nucleus propulus
Process of aging
Biomechanical strain & trauma
Genetic (FGF4 gene)
Chondrodystrophic breeds eg Dachshund, French Bulldog.
short limb phenotype FGF4
Stages of IVDD degeneration
Chondroid metaplasia
nucleus pulposus and then the annulus fibrosis
notocordal cells (NP) and spindle shaped fibroblasts (AF) replaced by chondrocytes
Dehydration of nucleus pulposus
loss of glycosaminoglycan from NP
Fissures in annulus fibrosus
tears and clefts form in AF, most commonly dorsal or dorsolateral regions
Necrosis and secondary calcification
mainly NP periphery and occasionally in AF
Types of degenerative intervertebral disc disease (IVDD)
Hansen type I : Intervertebral disc extrusion (IVDE)
Complete rupture of the annulus fibrosus
spilling-out of the nucleus pulposus into the vertebral canal
Chondrodystrophic breeds : frenchies, daschund
early as < 1 year old
acute onset histological degenerative
Hansen type II: Intervertebral disc protrusion (IVDP)
Fissures form in the annulus fibrosus
bulging of the annulus fibrosus and nucleus pulposus
Non-chondrodystrophic breeds
Older > 5 years
Chronic, more slowly progressive onset
Neurological examination includes 6
name an extra one if patient is paralysed
Mentation/Behaviour
Gait – ambulatory, non-ambulatory; paretic or plegic
Posture – kyphosis, lordosis or scoliosis
Proprioception – e.g. paw replacement and hopping
Muscle tone and muscle mass – limbs and bladder tone
Spinal reflexes e.g. Withdrawal reflexes, patellar reflex, perineal reflex and cutaneous trunci reflex
not indicative of degree of leision
(Sensation or pain perception Important only test in paralysed patients.)
if motor ability ok sensation will be ok
name this posture
Kyphosis
name the posture
Lordosis
name the posture
Scoliosis (DV view)
Neurolocalisation clasificaiton
dogs
C1-C5 = cervical
C6-T2 = cervical intumescence
T3-L3= thoracolumbar
L4-S3 = lumbosacral intumescence
Split into L4-S1 and S1-S3
Grading of dysfunction: name from least significant to most 5
1. Pain or hyperaesthesia
2. Proprioceptive ataxia and ambulatory paresis
3. Non-ambulatory paresis (not able to walk but still see movemetn when moving ox)
4. Plegia
5. Plegia with loss of pain perception
Paresis (para, tetra)
weakness, voluntary movement present
Plegia or paralysis
loss of voluntary movement
Effect when motor neuron s affected: Upper and lower motor neuron
Upper motor neuron (UMN):
Increased muscle tone
normal or increased spinal reflexes
Lower motor neuron (LMN)
Decreased muscle tone
decreased or absent spinal reflexes
when intumescences are affected
muscle mass and bladder effect: in each location of the spincal cord
where is the UMN of baldder and where is LMN)
For bladder
Upper motor neuron (UMN) (C1-S1)
When referring to the bladder, increased bladder wall (detrusor muscle) tone
difficult to express due to increased tone in urinary sphincters
Lower motor neuron (LMN) (S1-S3)
When referring to the bladder, decreased bladder wall (detrusor muscle) tone
easy to express due to loss of tone in urinary sphincters
Cervical IVDD (C1-5, C6-T2)
Clinical Signs 5
describe 4 types of gait presentation
Pain/Hyperaesthesia
Reluctance to move, reduced range of movement in the neck
Posture – Low head carriage
Gait
Single thoracic limb lameness = ‘nerve root signature’ (see pic)
Ambulatory hemi- or tetra-paresis and proprioceptive ataxia
Non-ambulatory tetraparesis
Tetraplegia
Respiratory arrest (C5-7, phrenic nerve)
Horner's syndrome (T1-3, sympathetic innervation to the eye)
describe Ambulatory tetraparesis, generalized proprioceptive ataxia— gait
3
Gait in all 4 limbs uncoordinated and unsteady
Long strides in all 4 limbs
Wide based in pelvic limbs
cervical IVDD causes resp arrest via
(C5-7, phrenic nerve)
cervical IVDD causes horner syndrome via
(T1-3, sympathetic innervation to the eye)
cervical IVDD if frequent in these location:
small breed
large breed
small breed, C5-6
large breed, C6-7
Thoracolumbar IVDD
Clinical Signs 4
2 posaible gait
most frequent in
Pain/Hyperaesthesia – reluctance to move
Posture – Kyphosis
Gait – Pelvic limb lameness = ‘nerve root signature’
Ambulatory mono- or para-paresis and proprioceptive ataxia
Non-ambulatory paraparesis – Paraplegia Loss of pain perception
Urinary and faecal incontinence
Most frequent between T11-12 to L3-4.
Thoracolumbar IVDD most common location is between ______ and ___
it is especially common in____ and ____
between T11-12 to L3-4.
Especially T12-13 and T13-L1
Ambulatory paraparesis and proprioceptive ataxia gait discription 2
Pelvic limb gait uncoordinated and unsteady
Varies between narrow based and wide based
gait describe— Non-ambulatory paraparesis and proprioceptive ataxia 2
lift/ sling neeeded
not relaly moving HL
Lumbosacral IVDD
Clinical Signs 4
gait possibility 3 /4
what is nerve root signiture for lumbosacral
Pain/Hyperaesthesia (reluctance to move)
Posture
Crouched stance in pelvic limbs • Low tail carriage
Gait
Pelvic limb lameness = ‘nerve root signature’
Ambulatory mono or paraparesis and proprioceptive ataxia
Non-ambulatory paraparesis
Paraplegia with or without deep pain perception
Urinary and faecal incontinence
Radiography IVDD: px positioning and sensitivtiy
– lateral and ventrodorsal, patient under sedation
sensitivity of 50-60% in the thoracolumbar region, 35% in the cervical region o
Radiographic changes supportive of IVD extrusion (hanson type1) 4
Narrowing of the disc space
Narrowing of the articular facets
Narrowing and/or increased opacity of the intervertebral foramen
Presence of mineralized disc material within the vertebral canal
radiographic evidence supportive of intervertebral disc degeneration but not disc extrusion 1
what would you remind O if dog is under 2 y/o 2
Mineralisation (or calcification) of the disc space in situ
disc calcification at 2 years old is a significant predictor of disc herniation later in life
risk factor for recurrent herniation following surgery.
Computed Tomopgraphy for IVDD diagnosis
3D image free from superimposition o Wider availability, less costly and much faster – vs. MRI o Characteristics compatible with acute intervertebral disc extrusion in CT: hyperattenuating (white) material within the vertebral canal, loss of epidural fat and distortion of the spinal cord o Soft tissue structures have similar appearance – spinal cord, cerebrospinal fluid and meninges o 82-100% sensitivity in the thoracolumbar region
CT myelography
Contrast injected into the subarachnoid space o Delineates compressive lesions not visible on non-contrast CTs
MRI IVDD
Gold standard o Can differentiate anatomical structures of vertebral column better to CT, including supporting ligamentous structures, synovial joints, bone marrow, nerve roots, spinal cord parenchyma, cerebrospinal fluid, epidural fat and the layers of the intervertebral disc o Characteristics of IVDE include extradural compression of the spinal cord centred over or near the intervertebral disc space ▪ Compression and/or displacement of the spinal cord = displacement or loss of the hyperintense (white/bright) signal associated with subarachnoid and epidural spaces on T2W images ▪ Extruded nucleus pulposus typically = hypointense (black/dark) mass within the epidural space on T2W images o Requires GA whereas CT can be done under sedation o Sensitivity 98.5%
Conservative treatmentI VDD tx
onservative treatment o Indications:
First episode of spinal hyperaesthesia with mild or no neurological deficits ▪ Chronic but mild neurological deficits ▪ Financial limitations
EXERCISE RESTRICTION
Analgesia – discuss risks of analgesia if strict rest is not implemented (patients feel better and more mobile which can lead to further disc material extruding)
Monitor urination and defecation
Rehabilitation / physiotherapy if required
IVDD Surgical treatment disc removal indication
Indications: ▪ Significant neurological deficits – inability to walk to loss of pain perception ▪ Pain or mild neurological deficits unresponsive to rest and analgesia ▪ Frequent recurrence of pain or neurological deficits following medical management
wil nver fully heal dc
IVDD sx In the cervical vertebral column
t commonly a ventral slot procedure is performed ▪ Section of the intervertebral disc and 2 adjacent ventral bodies is removed to access the vertebral canal from the ventral aspect
IVDD sx In the thoracolumbar vertebral column
hemilaminectomy procedure is performed o The articular facet joint and lamina of 2 (or more) adjacent vertebrae is removed to access the vertebral canal from the dorsolateral aspect (blue arrow) o Additionally a fenestration may be performed. A section of the lateral aspect of the annulus fibrosus is removed and the nucleus pulposus is curetted (scooped) out (yellow arrow)
Prognosis • Intervertebral disc extrusion
Prognosis: cervical
prognosis • Intervertebral disc protrusion
Surgery: 75% improve o Medical: 40% improve o Chronic presentation, likely to have permanent neurological deficits due to irreversible spinal cord damage
Cervical spondylomyelopathy (CSM)
Causes vertebral canal stenosis (narrowing) ▪ Combination of static and dynamic compression ▪ Static – compression always present ▪ Dynamic – compression improves or worsens with different positions of the cervical vertebral column o 2 forms with different pathophysiology ▪ Disc-associated CSM ▪ Osseous-associated CSM o Signalment: ▪ All canine breeds ▪ 60-70% Doberman and Great Dane
Disc-associated CSM
Signalment: Middle-aged large breed dogs (primarily Dobermans) o History: Typically chronic o Clinical signs: As for cervical IVDD o Pathogenesis: ▪ Degenerative (with likely genetic component, although unproven) ▪ Intervertebral disc protrusion and ligament hypertrophy (dorsal and ventral to the spinal cord) leads to narrowing of the vertebral canal and spinal cord compression ▪ C5-6 and C6-7 most commonly affected o Diagnosis: MRI
thickening of ligament (dorsal) and extrucion in ventral
• Osseous-associated CSM
Young, giant breed dogs
History: Typically chronic o Clinical signs: As for Cervical IVDD o Pathogenesis: ▪ Unknown aetiology, suspected combination of genetic, conformational and nutritional ▪ Vertebral malformation + degenerative osseous change ▪ Leading to osseous proliferation of vertebral arch, articular processes (osteoarthritis) and pedicles. ▪ Most giant breed dogs have osseous compression, can have disc protrusion, especially in older dogs ▪ C4-5, C5-6 and C6-7 o Diagnosis: MRI or CT
CSM Conservative treatment
▪ Exercise restriction, body harness rather than collar ▪ Anti-inflammatories (NSAIDs or corticosteroids) and analgesia
CSM Surgical treatment:: lots of types
Ventral slot for disc decompression +/- stabilisation ▪ >> Dorsal laminectomy to address osseous compression +/- stabilisation
CSM Prognosis
Surgery 70-90% improvement ▪ Conservative 14-54% ▪ However, progression of disease with both treatment strategies
spinal cord end l5
3. Degenerative lumbosacral stenosis (DLSS)
Lumbosacral junction = L7-S1 Cauda equina = L7, S1-3, Cd1-5 nerve roots
DLSS Signalment/Histor
Medium to large dogs of middle to older age o Especially German Shepherd dogs o Variable - acute or chronic and may be persistent or episodic
DLSS clins gin
Pelvic limb hypometria (short strided, reduced stride height) o Lumbosacral pain, pain on elevation of the tail o Lameness (‘nerve root signature’) – unilateral or bilateral o Urinary or faecal incontinence o Tail weakness o Reduced perineal and pelvic limb withdrawal reflexes
normal anatomy
sc end sat L5
DLSS Pathogenesis
= multifactorial: o Congenital vertebral malformation o L7-S1 intervertebral disc degeneration ▪ Protrusion ▪ Collapsed disc space o Hypertrophy of ligaments of lumbosacral joint (caused by instability) o Degenerative joint disease of articular processes o Spondylosis deformans • Collectively lead to narrowing of the vertebral canal and intervertebral foramen and nerve impingement
DLSS dx
which on egold stamdard
o Radiography – able to identify the osseous changes o CT – able to identify the osseous changes o MRI – better for assessing nerves of cauda equina and intervertebral disc changes
DLSS tx: Conservative treatment:
Exercise restriction and analgesia ▪ Epidural steroid injections – Variable response, may provide long lasting resolution of clinical signs
DLSS tx: Surgical treatment:
Dorsal laminectomy +/- foraminotomy ▪ +/- spinal distraction-stabilisation if instability
DLSS Prognosis: Usually good (but what if urine inconinuence)
Chronic cases likely to require long-term analgesia ▪ Poor prognosis in dogs presenting with chronic urinary incontinence
Canine Degenerative Myelopathy (CDM) Signalment
Middle age to older dogs, usually large breed o German Shepherd Dogs (GSD), Boxer, Pembroke Welsh Corgis (PWC) , Bernese Mountain Dog, Chesapeake Bay Retrievers, Rhodesian Ridgebacks, and other breeds o GSD median age onset 9 years, PWC 11 years
CDM • History and clin sign
Slowly progressive clinical sign o Non-painful
Initially: asymmetrical T3-L3 myelopathy o Progresses to involve L4-S3 and C6-T2 spinal cord segments and eventually involves the brainstem
CDM staging
not in slides
CDM pathogenesis
Concurrent axonal and myelin degeneration of the spinal cord o Multifactorial: Immunological, metabolic or nutritional, oxidative stress, excitotoxicity and genetic mechanisms o CDM has genetic and clinical similarities with amyotrophic lateral sclerosis (ALS) in humans
CDM dx
defin dx
reported breed, supportive neuro sign
Exclusion of other conditions
E.g., Intervertebral disc protrusion, neoplasia
Genetic test
SOD1 gene o Positive result to support pre-existing clinical suspicion, not diagnostic o See: http://www.offa.org/dnatesting/dmexplanation.html
Definitive diagnosis can only be achieved with post-mortem evaluation of the spinal cord
Other types of intervertebral disc disease
• Acute non-compressive nucleus pulposus extrusion (ANNPE)
Hydrated nucleus pulposus extrusion (HNPE)
Fibrocartilaginous embolism (FCE) —> ** Vascular myelopathy
Acute non-compressive nucleus pulposus extrusion (ANNPE)
non compressive—> contrindication for sx
brighter, bruising but nothing else
History: associated with a trauma or high-impact activity
Clinical signs:
acute onset, lateralised neurological deficits
Non progressive after first 24 hours
Often vocalize at onset and may be painful in first 24h
Neurological signs depend on location and degree of spinal cord damage
Pathogenesis: Sudden extrusion of small volume of disc material, impacts spinal cord with force
Diagnosis: MRI
Treatment: Conservative
Prognosis: Recovery of ambulation excellent, variable recovery of continences
Hydrated nucleus pulposus extrusion (HNPE)
Signalment: o Any breed, chondrodystrophic and non-chondrodystrophic o Typically middle aged or older
History: o Spontaneous, without inciting cause
Clinical signs: o Acute onset, non-progressive, symmetrical neurological deficits o Cervical location more common – tetraparesis, tetraplegia, respiratory compromise also possible o Typically non-painful
Pathogenesis: o Partially or non-degenerate disc extrudes, varying degree of compression
Diagnosis: MRI
Treatment: o Conservative (see earlier slide) – surgery if not improving( and dryspnoea) • Prognosis: o usually excellent, same conservative vs. surgical
Fibrocartilaginous embolism (FCE)
Signalment: o Most common in medium to large breed o Typically nonchondrodystrophic o Miniature Schnauzer o Rare in cats
History: o Typically spontaneous o Inciting cause of exercise or trauma in 30%
Clinical signs: o Peracute onset of nonpainful, lateralising clinical signs Dewey, 2015 o Majority of cases clinical signs don’t progress beyond first 24 hours
Pathogenesis: o Ischaemic infarct secondary to occlusion of artery/vein supplying the spinal cord o Caused by fragment of fibrocartilage thought to come from intervertebral disc • Diagnosis: MRI
Treatment: Conservative (see earlier slide) • Prognosis: usually excellent, but depends on response in the first 2 weeks of treatment and MRI findings
02
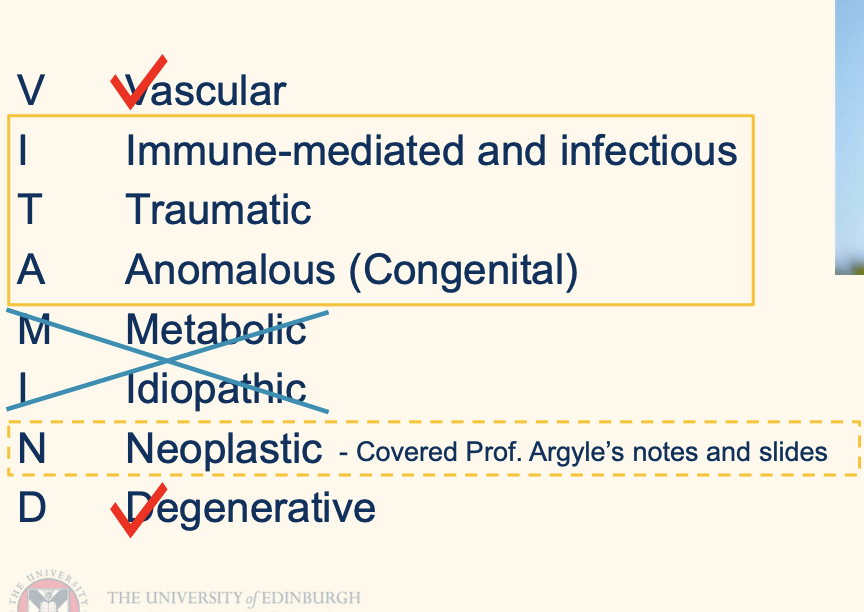
Clinical features of: – Steroid responsive meningitis-arteritis (immune mediated) – Discospondylitis (infectious) – Congenital or anomalous diseases • Chiari-like malformation and syringomyelia • Atlanto-axial subluxation • Hemivertebrae • Spinal arachnoid diverticula Clinical features and management of acute spinal cord trauma
Immune mediated diseases of the spinal cord
Steroid responsive meningitis-arteritis (SRMA)
Meningomyelitis of unknown origin also known as Granulomatous meningoencephalomyelitis (GME) - see notes on vestibular disease
Steroid responsive meningitis-arteritis
Signalment:
Young (< 2 years of age) dogs
Medium and large-breed dogs most often (but any breed can be affected)
predisposition in Boxers, Beagles, Bernese Mountain dogs, vizlaw, Golden retrievers, German Short-haired Pointers, and others
History: Acute onset, recurrent episodes, wax/waning
Clinical signs:
severe neck pain, low carriage head and neck
pyrexia (systemic; vs memningial myelitis main difference)
exercise intolerance and stiff gait (some cases develop concurrent polyarthritis)
Steroid responsive meningitis-arteritis (SRMA): pathogenesis and dx
Immune-mediated inflammation of the meninges and associated blood vessels
Cerebrospinal fluid (CSF) analysis:
neutrophilic pleocytosis (non-degenerate) +/- haemorrhage
can be normal if on/recently had anti-inflammatories
Elevated serum C-reactive protein (crp) supports clinical suspicion, but not diagnostic
Rule out infectious causes:
Imaging (radiographs, CT or MRI)
CSF bacterial culture
PCR/serology for protozoal and tick-borne diseases
red erythrocyte; neutrophil even if lack of bacteria
Steroid responsive meningitis-arteritis (SRMA) • Treatment:
Immunosuppressive doses: corticosteroids (prednisolone)
Slow tapering over 4-6 months to prevenbt relapse
relapse desribed
Check serum C-reactive protein prior to reducing dose
Regular monitoring for side effects of chronic steroid treatment
physical examination, haematology and biochemistry
Concurrent antibiotics may be necessary whilst pending infectious disease results
Steroid responsive meningitis-arteritis (SRMA): Prognosis
Good to excellent for cases with prompt diagnosis and treatment – Recurrence common (16-48%) – can re-start prednisolone tapering protocol or add another immunosuppressive drug – If severe side effects from prednisolone can use another immunosuppressive drug and taper prednisolone quicker
Infectious diseases of the spinal cord
Discospondylitis – infection of the intervertebral disc (IVD) and adjacent vertebral body endplates
Distemper myelitis - notes on forebrain disease
Feline infectious peritonitis (FIP) – See Prof. Gunn-Moore’s slides and notes
Dry form of FIP may involve the central nervous system (CNS)
Can cause multifocal CNS signs including signs of spinal cord disease
Discospondylitis signalment
Large breed, GSDs and Dobermans over-represented ▪ But can occur in any age/breed o Male (intact or castrated) dogs o Reported in cats
Discospondylitis hx
y: o Subacute or chronic, typically >72 hours duration o **Can present acutely with pathological vertebral fracture/luxation o Recent corticosteroid use or surgery (any region) are risk factors
discospondylitis Clinical signs
Vague spinal pain - focal or multifocal o Lameness, pyrexia (8%), lethargy, anorexia, abdominal pain and weight loss o ±Neurological deficits range from mild ataxia to plegia ▪ Caused by secondary IVDD, pathological vertebral fracture/luxation, or empyema (pus in vertebral canal)
± defi
Discospondylitis pathogenesis
Bacterial or fungal infections:
Staph. intermedius most common ▪
. coli, Bacteroides, Strep., and others
Brucella canis (zoonotic, notifiable disease) ▪
spergillus, Actinomyces o Route of infection
Haematogenous spread = most common ▪
Migrating foreign body (grass awn) ▪ Iatrogenic – surgery or epidural injection complication o L7-S1 most commonly affected site, but can occur anywhere along the vertebral column o Multifocal in over a third of cases
dc
Discospondylitis• Diagnosis
Bloodwork: ▪ Haematology ▪ C-reactive protein o Radiographs ▪ Radiographic changes can lag 2 weeks behind clinical signs ▪ Radiographic findings suggestive of discospondylitis • Collapsed IVD space • Lysis of vertebral end plates and adjacent vertebral bodies • Sclerosis of vertebral end plates • Bony proliferation adjacent to IVD space o CT or MRI with contrast – MRI most sensitive o Blood culture: only successful in 27-50% of cases o Urine culture
Intervertebral disc culture – surgical approach or image-guided ▪ Screen for Brucella canis in entire dogs / those with travel history
Intervertebral disc culture – surgical approach or image-guided
indication
Indications: negative urine or blood cultures, or lack of clinical response to broad spectrum antimicrobial therapy ▪ Complications – rare based on currently available literature • For surgical approach: haemorrhage, vertebral destabilization, postoperative neurological worsening and those associated with prolonged general anaesthesia. • For percutaneous approach: inadvertent damage to the spinal cord, spinal nerves, or large vessels, worsening pain, progression of neurological deficits, and seeding of bacteria from the disc into the epidural space, subarachnoid space or both o
Treatment
o Minimum 6-8 weeks antibiotics (median duration 16 weeks)
Cave if SRMA was suspected... steroids
Empirical treatment pending culture and sensitivity
Potentiated amoxicillin, cephalosporin
Negative culture: treat for Staph. intermedius
No improvement in 1 week: re-evaluate therapy
Biopsy and/or surgery in medically refractory cases
Antifungal agents e.g. itraconazole
Analgesia - NSAIDs, paracetamol, gabapentin
Surgery – decompressive or stabilisation
Discospondylitis: Follow up and Prognosi
Response to treatment monitored by serial imaging, usually every 6-8 weeks
Continue antibiotic/antifungal treatment until no evidence of lesion progression
Relapse in 12% o Progressive neurological dysfunction in 12% ▪ More likely if have pre-existing steroid treatment o Good prognosis if the organism is bacterial and it is identified early in the course of the disease when neurological deficits are not present o Guarded to poor with significant neurological deficits and/or fungal infection
Anomalous (Congenital) diseases of the spinal cord
Syringomyelia (+ Chiari-like malformation)
Vertebral malformations a. Hemivertebrae b. Block vertebrae, transitional vertebrae and Spina bifida c. Atlanto-axial subluxation
Dermoid sinus
Spinal arachnoid diverticulum
Chiari-like Malformation and Syringomyelia (CLM/SM): • Signalment:
Cavalier King Charles Spaniels, Griffon Bruxellois, other toy and small breeds o Also described in brachycephalic cats o Broad age range, typically < 4 years old
Chiari-like Malformation and Syringomyelia (CLM/SM) hx and clin sign
History: typically chronic, insidious
Clinical signs: o ‘Phantom-scratching’ neck/shoulder/flank area o Spinal pain (cervical or thoracolumbar) and/or allodynia (pain triggered by stimuli that don't normally cause pain, e.g. touch) o Chronic cases may develop ataxia and paresis o (Cerebellovestibular dysfunction)
Chiari-like Malformation and Syringomyelia (CLM/SM) pathogenesis
CLM = congenital malformation of small-breed dogs similar to Chiari type I malformation in humans o Causes a mismatch between the volume available in the caudal fossa and the brain parenchyma located in this space, resulting in herniation of the cerebellum into the foramen magnum ▪ Caudal fossa contains cerebellum, pons and medulla
CLM is associated with progressive formation of syringomyelia (SM), however, SM pathophysiology is still not clear
Syringomyelia = fluid filled cavity within the spinal cord
One hypothesis is that CLM leads to increased pressure difference between cranial and spinal compartments o CLM and SM are often associated but they can occur independently of the other
caudal fossa
intracranial space between tentorium cerebelli and occipital bone (green)
CLM/SM: Diagnosis
vMRI best modality to show effect of cranial malformation on brain tissue and also changes within the spinal cord
CLM/SM: medical tx
▪ Analgesia - gabapentin, pregabalin, tramadol, NSAIDs
Drugs that may reduce CSF productio
all evidence is anecdotal (omeprazole, acetazolamide, furosemide) ▪ Corticosteroids –
anti-inflammatory effects, decreased CSF production and decreased substance P expression.
Taper to lowest effective doseresponse ok to gaba
CLM/SM: sirg tx
Foramen magnum decompression and cranioplasty
• Prognosis:
Medical: 50-75% patients improve but resolution unlikely and disease will progress
Surgical: 80% short term improvement but relapse in 25-50%, typically due to excess scar tissue formation
Vertebral malformation a. Hemivertebrae
Signalment: Frequently reported in screw-tailed brachycephalic breeds o French bulldog, English bulldog, Boston Terriers, Pugs • History: typically, chronic and slowly progressive • Clinical signs: variable o Subclinical: Commonly found in neurological normal dogs ▪ 78% of French Bulldogs o Depends on site and degree of spinal cord compression ▪ Thoracic vertebral column most common site >>> paraparesis and proprioceptive ataxia o Abnormal angulation – kyphosis, lordosis, scoliosis o More likely to be associated with neurological deficits in Pugs
Hemivertebrae pathoenesis
pathgenesis: o Failure of vertebrae to form properly, usually vertebral body o Typically wedge shaped o Vertebral column instability and spinal cord compression
Vertebral malformation dx, tx, px
Diagnosis: o Radiographs, plain CT o MRI or CT myelogram to assess effect on spinal cord • Treatment: o Conservative: exercise restriction, anti-inflammatories and pain relief ▪ Likely to continue to progress o Surgical stabilisation
Prognosis: variable depending on degree of spinal cord compression, aim of surgery it to limit progression
not exmaminablle —block junction
Atlanto-axial subluxation: signalment and hx
o Anomalous: Toy or small-breed dogs less than 2 years old, occasionally cats ▪ Yorkshire terriers, miniature or Toy Poodles, Chihuahua and Pekingese o Traumatic: Any age/breed
hx Acute or chronic
Acute or chronic vc. Atlanto-axial subluxation
Clinical signs: Variable – Mild cases: neck pain alone (avoid neck flexion) – Moderate: ataxia and tetraparesis – Severe: tetraplegia and respiratory difficulties • Pathogenesis (for anomalous): – Congenital malformation of the dens (agenesis or hypoplasia) or abnormal ligaments – AA joint is unstable, leading to luxation/subluxation and cervical spinal cord compression
AA subluxation: diag tx, px
Diagnosis o Radiographs and MRI o CT scan • Treatment o Conservative: Rest and neck brace o Surgery: Fixation e.g. with pins or screws with bone cement (Polymethylmethacrylate, PMMA) • Prognosis o Depends on severity of neurological deficits o High rate of complications with surgery o 0-30% complication rate, 5-10% in more recent publications
. Spinal arachnoid diverticulum:
effect special part og thoraloccolubar
Signalment: o Congenital: Rottweilers in cervical region o Acquired: Pugs and French Bulldogs ▪ Male pugs predisposed o Also reported in cats o Age of onset variable • History: Typically chronic, slowly progressive • Clinical signs: Depend on site o Tetra- or paraparesis and proprioceptive ataxia o Typically, no associated with pain (present in ~20%) o Urinary and faecal incontinence (typically with thoracolumbar site)
4. Spinal arachnoid diverticulum
Signalment: o Congenital: Rottweilers in cervical region o Acquired: Pugs and French Bulldogs ▪ Male pugs predisposed o Also reported in cats o Age of onset variable • History: Typically chronic, slowly progressive • Clinical signs: Depend on site o Tetra- or paraparesis and proprioceptive ataxia o Typically, no associated with pain (present in ~20%) o Urinary and faecal incontinence (typically with thoracolumbar site)