PTE 742: midterm and final exams
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
chronic pain
pain that lasts beyond (persists) the normal tissue healing time of 3-6 months
what is chronic pain according to G. Lorimer Moseley?
“pain is a multiple system output activated by an individual-specific pain neuromatrix. the pain neuromatrix is activated whenever the brain concludes that body tissue is in danger and action is required.”
pain is considered an ____ and is very _____ with an “n= 1”
output
individualized
list the groups of individuals persistent pain is highest amongst.
women
older adults
unemployed
rural adults
those in poverty or on public health insurance
describe the Cartesian Model of pain.
“it hurts…ouch”; fire burns —> signal travels to brain—> realizes that hurts
tissue damage = pain
doesn’t explain complexities of pain
may induce fear/anxiety

what pain paradigm is described in this picture?
Cartesian Model
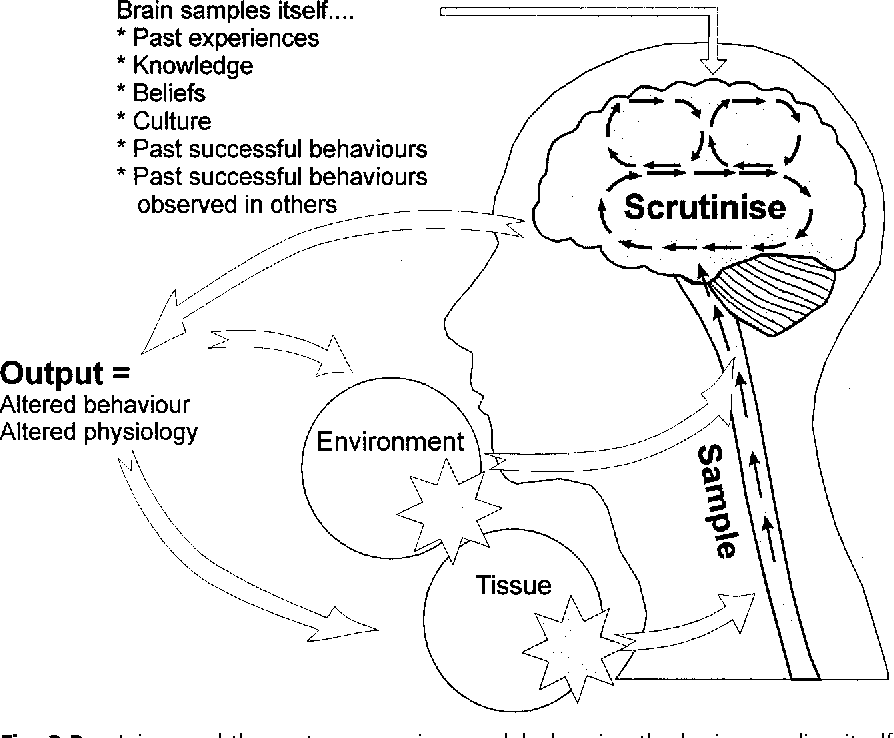
what pain paradigm is described in this picture?
Mature Organism Model (MOM)
describe the Mature Organism Model of pain.
“I think… it hurts… ouch”
multi-dimensional input
explains complexities; de-mystifies pain experience
biopsychosoical model
what are nociceptors stimulated by?
potentially harmful stimuli, including extreme temperatures (heat or cold), intense mechanical pressure, and chemical signals indicating tissue damage
what are the three types of pain?
nociceptive pain
neuropathic pain
nociplastic pain
nociceptive pain
pain that arises from actual or threatened damage to non-neural tissue (obvious tissue issue) and is due to the activation of nociceptors
neuropathic pain
pain caused by a lesion or disease of the somatosensory nervous system (actual nerve issue within the peripheral or central systems)
nociplastic pain
pain that arises from altered nociception despite NO clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system
what populations might be susceptible to neuropathic pain?
individuals with MS, spinal cord injury, diabetes, or nerve root compression/irritation
what population might be more susceptible to nociplastic pain?
individuals with phantom limb syndrome
what is sensitization?
increased responsiveness of nociceptive neurons to their normal input, and/or recruitment of a response to normally subthreshold inputs
what are the two types of sensitization?
hyperalgesia
allodynia
hyperalgesia
increased pain from a stimulus that normally provokes pain
longer a tissue issue occurs —> leads to sensitization —> heightens reaction
allodynia
pain due to a stimulus that does not normally provoke pain
what is the general rule when performing a skilled exam?
the more sensitized a person is, the more general the exam should be
exclude red flags, identify urgent issues, and assess functional limitations
list some examples of red flags.
cauda equina
severe and worsening pain
history of significant trauma
weight changes (cancer or other)
fevers
use of IV drugs or steroids
what is a yellow flag?
any psychosocial barriers to recovery
list some examples of yellow flags.
belief that all pain is harmful
catastrophizing
social withdrawal- negative moods
work or relationship problems
overprotective relationships or lack of support system
what are the three main characteristics of those who may benefit from Pain Neuroscience Education (PNE)?
high fear avoidance
high pain catastrophization
presence of central sensitization
what are the “3 Ps” patients want to know?
problem
prognosis
plan
what are the four pillars for dealing with persistent pain?
pain education
aerobic exercise
sleep hygiene
goal setting
what are some ways to calm the nervous system?
alter nocicpetion via medical, modalities, movement, or relaxation techniques
alter faulty cognitions and beliefs via PNE or coping strategies
decrease fear/anxiety
PNE can help normalize pain experiences associated with:
misbeliefs and faulty thought patterns associated with pain experience
fear-avoidance and pain catastrophizing behaviors
what is phase 1 of intervention with PNE?
education patients about pain using simple content with graphics that is personalized to the patient’s situation; avoid causing fear and anxiety
what is phase 2 of intervention with PNE?
focus on function with persistent pain
smart goal setting
graded exposure
patient empowerment
we should approach patients with persistent pain with a ______ approach.
biopsychosocial
T or F: it is possible to have pain and not know about it.
F
T or F: when part of your body is injured, special pain receptors convey the pain message to your brain.
F
T or F: pain only occurs when you are injured or at risk of being injured.
F
T or F: when you are injured, special receptors convey the danger message to your spinal cord.
T
T or F: special nerves in your spinal cord convey danger messages to your brain.
T
T or F: nerves adapt by increasing their resting level of excitement.
T
T or F: chronic pain means that an injury hasn’t healed properly.
F
T or F: worse injuries always result in worse pain.
F
T or F: descending neurons are always inhibitory.
F
T or F: pain occurs whenever you are injured.
F
T or F: when you injure yourself, the environment that you are in will not affect the amount of pain you experience, as long as the injury is exactly the same.
F
T or F: the brain decides when you will experience pain.
T
what is the gate control theory of pain?
pain signals can be modulated at the spinal cord, where a metaphorical "gate" can open or close to allow or restrict the transmission of pain signals to the brain, meaning that non-painful sensations can effectively "close the gate" and reduce the perception of pain
according to the gate control theory of pain, stimulus (input) from a small fiber ____ the gate.
opens
according to the gate control theory of pain, stimulus (input) from a large fiber ____ the gate.
closes
describe the nociceptive nerve fibers.
A: thick, fast, myelinated fibers; motor and cutaneous
B: medium, myelinated fibers; preganglionic ANS efferent
C: thin, unmyelinated, slow fibers; postganglionic ANS efferent
what are the two input mechanisms for the Mature Organism Model?
environment
peripheral neurogenic
what are the gatekeepers of the central nervous system?
interneurons
what are the two processing mechanisms of the Mature Organism Model?
spinal cord
brain
interneurons control what type of messages?
danger messages (via C fibers)
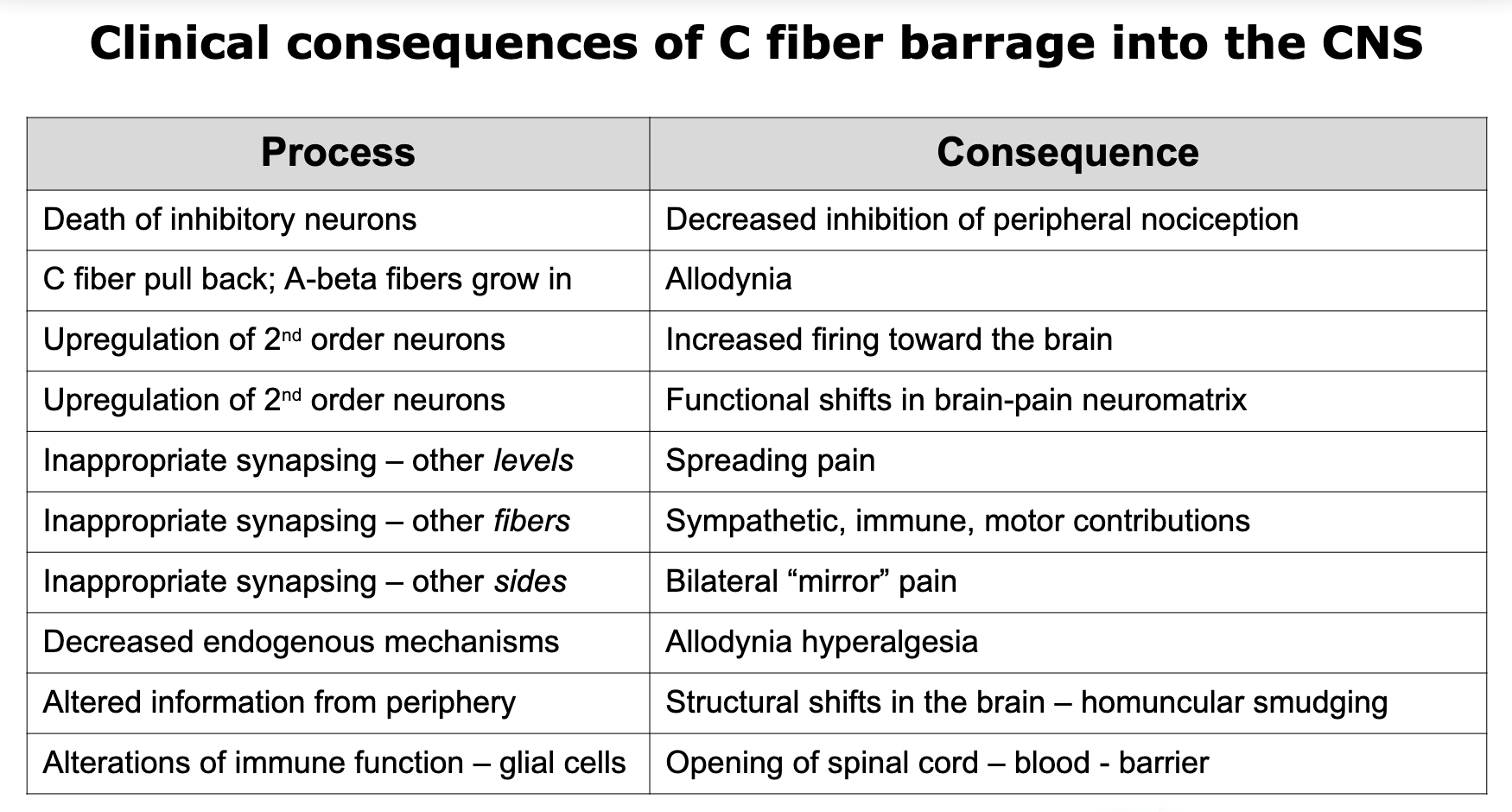
with persistent input from the periphery, changes to the spinal cord second-order neurons and brain pathways, lead to _____ ____.
heightened sensitivity
what happens if the interneurons die?
decreased ability to modulate incoming info, thresholds are easily met for nociceptive specific second-order neurons, increasing the firing to the brain
“action potential windup”
what are endogenous chemcials?
naturally occurring substances produced within the body, primarily "endorphins," which act as the body's natural painkillers
what does CRPS stand for?
complex regional pain syndrome
what are some symptoms of CRPS?
pain and increased pain sensitivity
changes in skin temp
decreased function
changes in skin color and texture
swelling
rapid or no hair and nail growth
describe the two types of CRPS.
no identifiable nerve injury
known nerve injury
why is determining the types of CRPS important?
they determine treatment plans
know these!
what are some techniques to not “lead a patient to pain”?
use softer language
ask what they are experiencing
ache vs. pain, tenderness vs. pain
T or F: persistent pain patients usually lack control over various aspects of their lives.
T
know this chart!
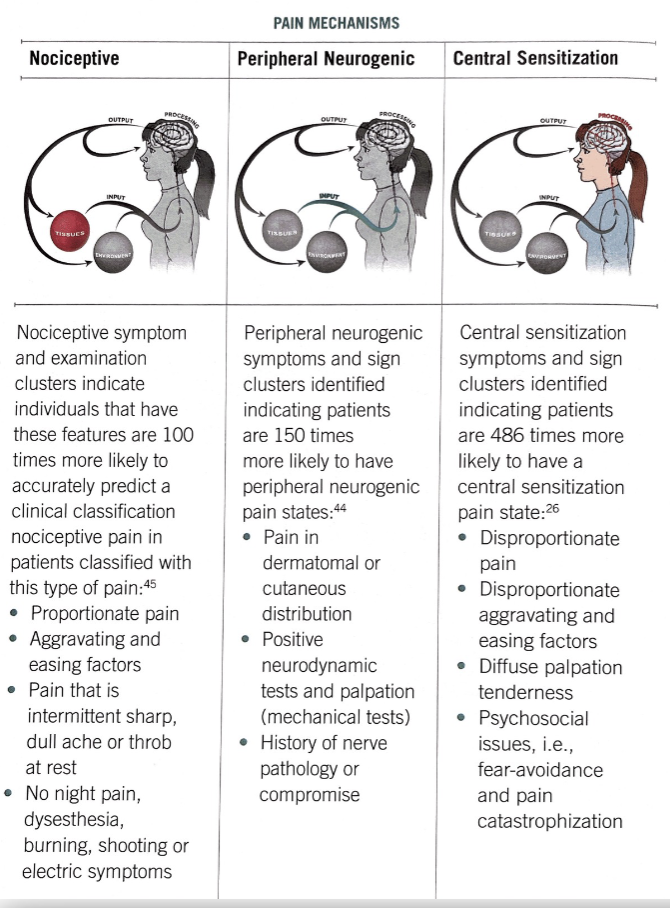
how do you know where your patient falls within the previous chart?
look for subjective exam clues: patient’s attitude, responses, and complaints (follow the M.O.M.)
T or F: we want patients to progress through the previous chart from nociceptive pain to central sensitization.
F; we want them to improve to nociceptive pain or no pain at all
if a patient presents with nociceptive pain, where should the therapist start?
looking for/addressing the pain generators, tissue issues, or any possible dysfunctions
what are the general treatment options for patients experiencing peripheral neurogenic symptoms?
avoid stretching, perform nerve glides, and proceed with “gentle work”
what are the general treatment options for patients experiencing central sensitization?
do laterality testing, fill out fear avoidance questionnaire, and educate via PNE
what are some other objective measures?
pressure pain threshold testing
thermal, vibration, and neural tension testing
joint end feel
two-point discrimination
graphesthesia testing
laterality and mirror testing
T or F: it is okay to start PNE education on the initial evaluation.
T; also good to build a rapport with patient beforehand
when is it appropriate to schedule persistent pain patients?
mid morning to early afternoon appointments
what are three main types of treatment for persistent pain patients?
PNE- education and knowledge are powerful
aerobic exercise (aka any movement is good)
medication
why is it a good idea to give patients pre-visit paperwork to fill out?
patients might be more honest when filling out before session in the comfort of their home
what are the percentages associated with PNE and behavioral changes?
20%: no way
35%: I get it
45%: yes, yes I get it
what should therapists do with the 20% (no way) patients?
focus on planting seeds about change
describe the 45% (yes, yes I get it) patients.
chronic patients; they keep coming back but not getting any better
they talk the talk but can’t walk the walk with PNE and behavioral changes
describe the 35% (I get it) patients.
life-long patients who progress but have episodes that keeps them coming back occasionally
good to their words and actions