Lecture 21 & 22 (Equine Viral Diseases)
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
Rabies
-neurotropic virus
-enveloped ssRNA
-transmitted by saliva of an infected animal - usually a bite or contaminated wound (also droplet inhalation or oral exposure)

yes
is rabies in horses zoonotic?
a) Rabies
pathogenesis:
-virus infects monocytes locally
-incubation can be days up to a year
-virus replicates in spinal nerve and ganglion of that nerve
-once in CNS spreads rapidly in neural tissue and glial cells of CNS → from there it spreads centrifugally along nerves → arrives in the salivary glands
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
a) Rabies
clinical signs:
-various neurological symptoms
-horses can present with a wide variety of signs
-death 5-10 days after onset of clinical signs
-abnormal vocalization
-depression // obscure lameness
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
there are no treatments
what is the treatment for Rabies in horses
-VACCINATION: very efficacious
-foals from vaccinated mares should not be vaccinated until 6 months of age (4 moths if dam is unvaccinated)
what is the prevention for Rabies in horses?
a) Cerebral
furious form of rabies
a) Cerebral
b) Brainstem
c) Spinal
b) Brainstem
dumb form of rabies
a) Cerebral
b) Brainstem
c) Spinal
c) Spinal
paralytic form of rabies
a) Cerebral
b) Brainstem
c) Spinal
false
t/f: clinical signs of Rabies in horses are pathognomic
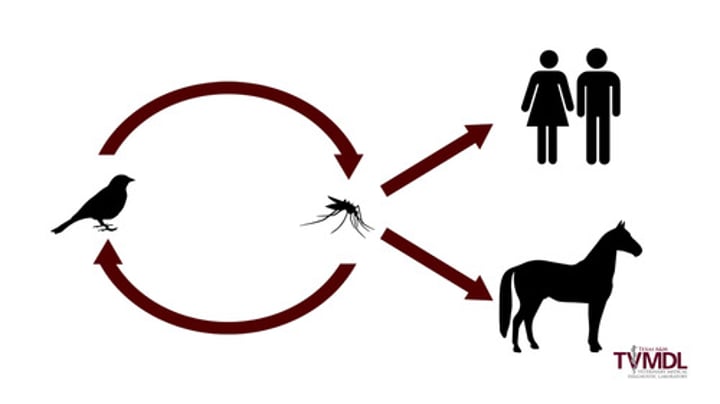
West Nile Virus
-single stranded RNA virus of the Flaviridae family
-transmitted mostly by Culex spp. mosquitoes
-not seen in the USA before 1999
-40% of infected horses died prior to the development of a vaccine
b) West Nile Virus
pathogenesis:
-this virus has a predilection for nervous tissue resulting in inflammation of the spinal cord and/or brain
-results in the clinical signs which can be variable and diverse
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
-hematology and clinical chemistry
-elevated muscle enzymes due to muscle damage
-diagnosis of WNV is supported by IgM antibodies
how do you diagnose West Nile Virus in horses
b) West Nile Virus
clinical signs:
-fever // anorexia // depression
-no clinical signs are pathognomonic
-muzzle fasciculation's // colic // apparent impaired vision
-circling/aimless wandering
-inability to swallow // muscle contractions
-gait abnormalities // trembling
-lack of coordination // weakness
-some cases will develop paralysis and/or convulsions which may lead to death
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
characteristic of a specific disease
what does pathognomonic mean?
birds
what is the primary host for West Nile Virus?
because they do not become sufficiently viremic to transmit to feeding mosquitoes
why are horses and humans considered dead-end-host for West Nile Virus?
true
is West Nile Virus zoonotic
-vaccination
-reducing exposure to mosquitoes
-eliminating mosquito breeding grounds such as pools/areas of stagnant water
how do you prevent West Nile virus in horses?
Japanese Encephalitis
-this is of the same family of WNV
-some strains have high fatality in horses
-foreign disease in the USA
-Culex spp. of mosquitoes are the main vectors
c) Hendra Virus
-not seen in the USA
-Paramyxovirdae family virus that closely resembles Nipah Virus
-a BSL4 agent
-recent emergence of this virus in Australia
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
c) Hendra Virus
-tropism for endothelial cells leads to respiratory distress and interstitial pneumonia
-flying foxes are the reservoir host
-urine and reproductive tract fluids may be the source of contamination
-infection leads to acute onset of high fevers and rapid progression to death
-respiratory or neurological disease
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses

d) Vesicular Stomatitis
-Rhabdovirus endemic in North, Central, and South America
-vesicles develop int he mouth and on the lips which rupture
-painful erosions on the lips cause anorexia // salivation
-fever is common
-lesions and fluid in vesicles can infect other animals directly (including humans)
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses

Yes
is Hendra Virus zoonotic?
yes
is Vesicular Stomatitis zoonotic?
Henipavirus
Hendra Virus (HeV) is a prototype of a new genus of viruses, ____________
e) Equine Encephalitis Viruses
-ssRNA enveloped viruses of the Alphavirus family
-viruses are zoonotic
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses
yes
are Equine Encephalitis Viruses zoonotic?
a) Eastern Equine Encephalitis
-first identified in MA in 1831
-infected horses are a low risk for infecting a human
-do not become viremic enough to infect biting mosquitoes
-this Encephalitis Virus is more likely to progress to severe disease and be fatal to the horse
a) Eastern Equine Encephalitis
b) Western Equine Encephalitis
c) Venezuelan Equine Encephalitis
b) Western Equine Encephalitis
-found predominantly in the western 2/3 of North America, Central America and most of South America
-horses infected are typically not contagious to other animals or people
a) Eastern Equine Encephalitis
b) Western Equine Encephalitis
c) Venezuelan Equine Encephalitis
c) Venezuelan Equine Encephalitis
-predominantly found in central and the north half of South America
-rodents are the natural host
-horses can become viremic enough to infect biting mosquitoes
-ocular and nasal secretions from infected horses can be sources of virus infection
a) Eastern Equine Encephalitis
b) Western Equine Encephalitis
c) Venezuelan Equine Encephalitis
from horses being bitten by infected mosquitoes mostly of the Aedes spp. and Culex spp.
*once a horse is bitten by an infected mosquito, the virus enters the lymphatic circulation replicating in macrophages and neutrophils
how is Equine Encephalitis transmitted?
e) Equine Encephalitis Viruses
clinical signs:
-pyrexia // stiffness // anorexia
-mild depression during the viremic stage
-signs of cerebral disease include propulsive walking, aggression, hyperesthesia, somnolence, and excitability
a) Rabies
b) West Nile Virus
c) Hendra Virus
d) Vesicular Stomatitis
e) Equine Encephalitis Viruses

a) Eastern Equine Encephalitis
_______ is more likely to progress to severe neurologic disease with mortality rates of 75-100% reported
a) Eastern Equine Encephalitis
b) Western Equine Encephalitis
c) Venezuelan Equine Encephalitis
c) Venezuelan Equine Encephalitis
neurological signs in ______ disease tend to develop over a shorter period of time, approximately 4 days after infection, and can include abortion, pulmonary hemorrhage, oral ulceration, and diarrhea
a) Eastern Equine Encephalitis
b) Western Equine Encephalitis
c) Venezuelan Equine Encephalitis
-EEE and WEE can be diagnosed by the presence of antibodies in an IgM antibody-capture ELISA
-VEE can be diagnosed by virus isolation or serology
how do you diagnose Equine Encephalitis Viruses?
-vaccinate against WEE and EEE annually
-horses should not be vaccinated against VEE since it is a foreign animal disease
-control of mosquitoes is important
how do you prevent a horse from getting Equine Encephalitis Viruses?
a) Equine Influenza Virus
-ssRNA enveloped virus belonging to the Orthomyxoviridae family
-viruses are typically classified into types A, B, C, and D
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

A
type ____ Influenza affects many species and is the EIV group that affects horses
neuraminidase and hemagglutination
Influenza type A is classified based on _______ and ________ antigens
a) neuraminidase
controls release of virus from infected host cells
a) neuraminidase
b) hemagglutination
b) hemagglutination
involved in binding to cells
a) neuraminidase
b) hemagglutination
a) equine-1 influenza
H7N7
a) equine-1 influenza
b) equine-2 influenza
b) equine-2 influenza
H3N8
a) equine-1 influenza
b) equine-2 influenza
b) H3N8
Equine Influenza Virus ______ has undergone antigenic drift and two lineages have develop
a) H7N7
b) H3N8
b) H3N8
Equine Influenza Virus _______ jumped species and was identified as a cause of acute respiratory distress in dogs in 2004
a) H7N7
b) H3N8
true
t/f: Equine Influenza Virus is considered more antigenically stable than human influenza virus
a) Equine Influenza Virus
-highly contagious and spreads quickly through naive horses through aerosol and contaminated fomites
-short incubation period of 1-3 days
-younger horses are typically more vulnerable
-common disease found in large equine facilities such as racetracks
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness
a) Equine Influenza Virus
pathogenesis:
-infects and replicates in respiratory epithelium
-healthy respiratory epithelium is ciliated and protected by a mucus layer
-mucus layer captures particulate matter but also contains antibodies
-cilia then waft the mucus layer up and out of the respiratory tract
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness
a) Equine Influenza Virus
Clinical Signs:
-appear in 3-5d post-infection
-severity related to strain and immune status
-sudden onset fever, often biphasic
-lethargy, anorexia, cough, serous-purulent nasal discharge
-occasionally myalgia, myositis, limb edema, +/- lymphadenopathy
-often minimal changes to thoracic auscultation
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

-clinical signs and detection of antigen or rising antibody titer levels
-detection of infection by virus isolation
-nasopharyngeal swab samples soon after onset of illness
A qPCR test that detects both H3N8 and H7N7 strains in a nasal swab or nasal wash is the most commonly used modality at present
how do you diagnose a horse with Equine Influenza Virus?
3-6 days
horses with Equine Influenza Virus remain infective for ____-____ days after cessation of clinical signs. young animals can become extremely sick with life-threatening disease
-vaccination programs are the mainstay of prevention with herd immunity being critical to prevent epidemics
-vaccination should be repeated every 6 months to yearly depending on age and other risk factors
-Broodmares should also be vaccinated 4-6 weeks prior to their expected sure date
how do you prevent Equine Influenza
a) Alpha Herpesvirus
EHV-1, EHV-3 and EHV-4
a) Alpha Herpesvirus
b) Gamma Herpesvirus
b) Gamma Herpesvirus
EHV-2 and EHV-5
a) Alpha Herpesvirus
b) Gamma Herpesvirus
a) N752
"wild type" of Equine Herpes Virus 1
a) N752
b) D752
b) D752
"neurotropic" type of Equine Herpes Virus 1
a) N752
b) D752
b) Equine Herpes Viruses
-enveloped dsDNA viruses characterized by their ability to establish lifelong infection by a state of latency
-the virus can reactivate (or recrudesce) at any time
-often associated with stress or immunosuppression
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

a) EHV 1
-infection causes respiratory disease, neurological disease, abortion in pregnant mares and neonatal deaths
-fever // rhinopneumonitis // cough // nasal discharge
-depression // respiratory distress
a) EHV 1
b) EHV 2
c) EHV 3
d) EHV 4
e) EHV 5
Equine Herpes Myeloencephalopathy (EHM)
-an uncommon manifestation of EHV-1 infection but usually occurs in an EHV-1 outbreak
-often have a history of fever, +/- respiratory disease signs, +/- limb edema in their recent history
-horses show ataxia // stiffness
-often an atonic bladder, urine dribbling and poor anal tone
-knuckling, toe dragging, clumsiness, stumbling and limb circumduction
b) EHV 2
-endemic slow replicating virus that develops latency in lymphoid and neural tissue as well as B- lymphocytes
-not typically considered a primary pathogen but may play a role in respiratory disease in foals
-foals are exposed in the first few weeks of life and develop a serological response
a) EHV 1
b) EHV 2
c) EHV 3
d) EHV 4
e) EHV 5
c) EHV 3 - Equine Herpes Coital Exanthema
-uncommon contagious venereal disease transmitted by coitus, insects, fomites and inhalation
-papules and bullae develop on the male and female genital tracts and sometimes lips, nostrils, mouth
-lesions become painful and pruritic but do heal with no lasting effect on fertility
-disease can recur due to virus recrudescence
-no vaccine or specific treatment
a) EHV 1
b) EHV 2
c) EHV 3
d) EHV 4
e) EHV 5
d) EHV 4
causes respiratory disease but is capable of causing neurological disease (termed abortion, and neonatal death but does so much more rarely)
a) EHV 1
b) EHV 2
c) EHV 3
d) EHV 4
e) EHV 5
e) EHV 5
-widespread virus and closely related to EHV-2
-implicated in self-limiting respiratory disease in young horses
a) EHV 1
b) EHV 2
c) EHV 3
d) EHV 4
e) EHV 5
-virus isolation from semen or necropsy specimens of dead foals
-PCR testing, virus isolation, virus neutralizing antibody paired titers or change from seronegative to seropositive
how do you diagnose Equine Viral Arteritis
c) Equine Viral Arteritis
-ssRNA virus that has a worldwide distribution
-can cause pneumonia, enteritis, fever, limb and ventral abdominal wall edema, sporadic sudden death in foals, abortion in mares, and mild and subclinical infections in horses
-bloodwork can show leukopenia, lymphopenia, and thrombocytopenia
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

c) Equine Viral Arteritis
-infection is often asymptomatic
-infection is by inhalation and more importantly by venereal transmission
-Stallions maintain the virus by being short- or long-term carriers where testosterone seems to be vital to long term carrier status
-the virus is shed in fluids of the reproductive tract such as semen
-the virus is maintained in the reproductive tract
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness
d) Equine Infectious Anemia
-largely worldwide retrovirus that results in infected horses becoming infected for life
-horses become infected usually through a bite from an infected fly (Stomoxys spp., Tabanus spp. Hybomitra spp. and Chrysops spp)
-infected horses show intermittent pyrexia, anemia, limb edema, weight loss and progressive weakness
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

"Swamp Fever"
what is Equine Infectious Anemia also known as?
-infected horses are quarantined from flies and other horses for the remainder of their life and freeze branded to identify them as EIAV positive → if this option is not pursued they are euthanized
-horses must have a valid negative Coggins test and Health Certificate completed by an accredited lab and accredited veterinarian to travel, cross states lines and travel internationally
how do you control and prevent Equine Infectious Anemia?
Rotaviruses
___________ are a large group of non-enveloped dsRNA viruses responsible for diarrhea in many species
e) Equine Rotavirus
-causes diarrhea in foals and typically is not seen in horse over 6 months of age
-the virus passes to the foal via a feco-oral route and following ingestion
-the virus damage also results in inflammation of the damaged gut wall
-decreased digestive capacity resulting in a maldigestion and malabsorption (osmotic) diarrhea
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

PCR testing of feces for Equine Rotavirus A and B is now available and should be performed on chilled feces from affected foals
how do you diagnose Equine Rotavirus?
A; B
Rotavirus Group ____ was considered the only Rotavirus to infect horses until 2021 when the University of Kentucky discovered a novel Rotavirus ___ in an outbreak of neonatal foal diarrhea
-two commonly used serological tests are the agar gel immunodiffusion (AGID or 'Coggins') test and enzyme-linked immunosorbent assays (ELISAs)
-ELISA tests can detect antibodies earlier than the AGID test, but false positives can occur
how would you diagnose Equine Infectious Anemia?
-diarrheic foals shed huge number of virus particles in their diarrhea and can shed for 3 days after cessation of diarrhea
-biosecurity is of paramount importance
A conditional Equine Rotavirus Group A vaccine is available for vaccination of pregnant mares in months 8, 9 and 10 of their gestation (this provides the foal with protective passive immunity via colostrum)
-currently there is no Equine Rotavirus B vaccine
talk about prevention and control of Equine Rotavirus
f) African Horse Sickness
-highly fatal arthropod-borne disease of equids that is currently foreign to the US (reportable)
-mortality rates in horses are up to 95%
-Zebra can be asymptomatic and are thought to be the reservoir host
-transmission is by biting insects such as Culicoides spp. midges, Stomoxys spp. and Tabanus spp. flies.
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

f) African Horse Sickness
Clinical signs:
Include fever and are as seen in four roughly grouped presentations: peracute (pulmonary) form, subacute edematous (cardiac) form, acute (mixed) form, and horse sickness fever (persistent cyclic fevers)
a) Equine Influenza Virus
b) Equine Herpes Viruses
c) Equine Viral Arteritis
d) Equine Infectious Anemia
e) Equine Rotavirus
f) African Horse Sickness

a) Equine Coronavirus
this virus can cause respiratory and gastrointestinal disease
a) Equine Coronavirus
b) Equine adenoviruses
c) Equine Rhinitis Viruses
b) Equine adenoviruses
Non enveloped viruses terms EADV1 and EADV2. EADV1 is endemic in horse populations and may cause conjunctivitis, rhinitis and bronchopneumonia in young stock. EADV2 has been isolated from foals with respiratory tract disease and diarrhea
a) Equine Coronavirus
b) Equine adenoviruses
c) Equine Rhinitis Viruses
c) Equine Rhinitis Viruses
these viruses cause fever, coughing, rhinitis, anorexia, submandibular lymphadenitis
a) Equine Coronavirus
b) Equine adenoviruses
c) Equine Rhinitis Viruses