Skin/Burns and F&E
1/81
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
Differences Between Infant Skin and Adult Skin
Thinner
Loses heat more readily
Contains more water
Bacteria can access more easily
Infants are less pigmented, placing them at risk of skin damage from UV radiation.

Differences in Dark-Skinned Children
Children tend to have more pronounced cutaneous reactions.
Hypopigmentation or hyperpigmentation can affect areas of healing.
This change in pigmentation may be temporary (a few months following a superficial skin disorder) or permanent (following a more involved skin condition).
Dark-skinned children tend to have more prominent:
Papules (rounded, non-pustular elevations of the skin)
Follicular Responses
Lichenification (thickened, rough skin)
Vesicular or Bullous reactions.
Hypertrophic scarring and keloid formation occur more often.

What are the Causes of Integumentary Disorders?
Exposure to Infectious Microorganisms
Hypersensitivity Reactions
Hormonal Influences
Genetic Predisposition
Injuries
What are terms to describe skin findings?
Macule — Flat, reddened areas.
Papule — Rounded, non-pustular elevation on the skin.
Annular — Ring-shaped with central clearing.
Vesicle — Fluid-filled lesions.
Pustule — Pus-filled lesion.
Scaling — Dry, flaky skin.
Plaques — Raised, flat-topped lesions.
Hypopigmented/Hyperpigmented — Areas of decreased or increased pigmentation.
Erythematous — Reddened skin.
Pictures of some skin findings

Integumentary Assessment
Health History:
Determine the chief complaint.
Document HPI, including location, duration, onset, and characteristics.
Note the child’s general health and discuss recent changes.
Use terms such as pruritus (itching) and scaling (dry, flaking skin).
Discuss chronic skin conditions.
Assess outdoor exposures.
Review skin care routines.
Physical Exam:
Perform a complete examination, noting abnormalities.
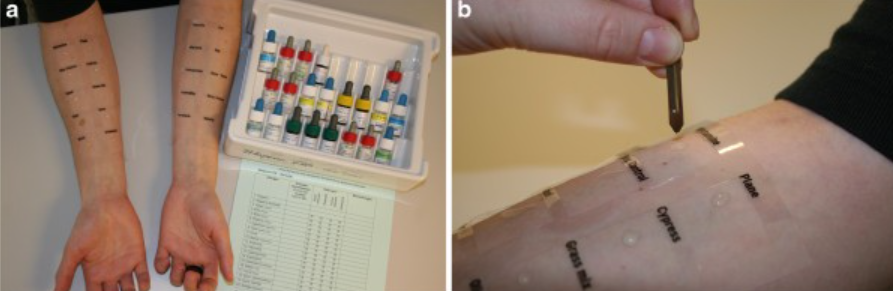
Laboratory Testing:
Testing is used to diagnose a disorder.
Most common tests include:
CBC with differential: Evaluates H&H, WBC count, and platelet count. Indicated for infections or inflammatory processes.
Erythrocyte Sedimentation Rate (ESR): A non-specific test used to detect the presence of infection or inflammation.
Potassium Hydroxide (KOH) Prep: Reveals branching hyphae (fungus) when viewed under a microscope. Used to identify fungal infections.
Immunoglobulin E (IgE): Measures serum IgE levels. Indicated for atopic dermatitis.
Patch or Skin Testing: A needle prick test with allergens. Indicated for atopic or contact dermatitis.
Wood Lamp
Impetigo
Bacterial Infection:
Epidermal, contagious
Papules progressing to vesicles, then painless pustules with a narrow erythematous border.
Honey-colored crusting/exudate when the vesicles or pustules rupture.
Cause: Staphylococcus or Streptococcus getting under the skin.
Most Common Sites:
Face
Mouth
Hands
Nursing Care:
Removal of crust (wound care)
Antibiotics (oral or topical)
Hygiene (just keep it clean!)

C) Impetigo
A 4-year-old child presents to the pediatric clinic with red sores on their face, especially around the nose and mouth. The sores have a honey-colored crust. The child has had a mild fever and is irritable. The mother reports that the child has been scratching at the lesions, which seem to be spreading. Upon examination, the lesions are non-tender, and there is no swelling of the lymph nodes. What is the most likely diagnosis for this child?
A) Tinea pedis
B) Acne vulgaris
C) Impetigo
D) Atopic dermatitis
Folliculitis
Bacterial Infection:
Infection of the hair follicle, often due to follicle occlusion.
Appearance: Red pustule-like, raised hair follicles.
Causes:
Poor hygiene
Contact with contaminated water
Maceration
Moist environment
Use of occlusive emollient products
Treatment:
Aggressive hygiene and warm compresses
Topical Mupirocin and occasionally oral antibiotics

Cellulitus
Bacterial Infection:
Localized infection and inflammation of the skin and subcutaneous tissues, usually preceded by skin trauma.
Cause: Streptococcus or Staphylococcus bacteria may enter via an abrasion, laceration, insect bite, foreign body, or infected lesion.
Localized Reactions:
Erythema
Pain
Edema
Warmth at the site of skin disruption
Education:
Mark around the border to see if it getting worse → sepsis.
Treatment:
Mild cases treated with Cephalexin or Augmentin
More severe cases of orbital cellulitis may require IV management.

A) Cellulitis
A 6-year-old child presents to the clinic with a red, swollen, and tender area on the lower leg. The child’s mother mentions that the child had a small cut on the leg a few days ago, which has now become infected. Upon examination, you notice diffuse erythema, warmth, and swelling extending beyond the wound. There is no history of fever, but the child has been complaining of pain in the area. What is the most likely diagnosis for this child?
A) Cellulitis
B) Impetigo
C) Folliculitis
D) Tinea pedis
Risk Factors for MRSA
Turf burns
Towel sharing
Participation in team sports
Attendance at daycare or outdoor camps
Tinea Capitis
Fungal Infection:
Affects the scalp.
Patches of scaling with central hair loss.

B) Tinea capitis
A 5-year-old child is brought to the clinic with red, itchy patches on their scalp. The child has been scratching the scalp frequently and complains of hair loss in the affected area. Upon examination, you observe circular, erythematous, and scaly patches on the scalp. There is also broken hair in the affected areas. The child has no fever or systemic symptoms. What is the most likely diagnosis for this child?
A) Tinea pedis
B) Tinea capitis
C) Tinea cruris
D) Acne vulgaris
Tinea Cruris
Fungal Infection:
Affects the groin.
Erythema, scaling, maceration in the inguinal creases or inner thighs (penis/scrotum spared).

B) Tinea cruris
A 4-year-old child presents with a red, itchy rash on the inner thighs and groin area. The rash appears as circular, erythematous patches with a scaly border, and some areas show small blisters. The child’s mother reports that the child has recently been playing in a public pool. The child has no fever or other systemic symptoms. What is the most likely diagnosis for this child?
A) Tinea corporis
B) Tinea cruris
C) Contact dermatitis
D) Diaper dermatitis
Tinea Pedis
Fungal Infection:
Affects the feet
“Athlete’s Foot”
Red, scaling on the soles and between the toes

C) Tinea pedis
A 9-year-old child presents with itching and redness between the toes, along with peeling skin on the soles of the feet. The child’s mother reports that the child frequently wears tight shoes and plays sports, which results in sweaty feet. Upon examination, you notice erythema and scaling between the toes, as well as some blisters on the feet. The child has no fever or other systemic symptoms. What is the most likely diagnosis for this child?
A) Contact dermatitis
B) Diaper dermatitis
C) Tinea pedis
D) Psoriasis
Tinea Corporis
Fungal Infection:
Affects any part of the body.
“Ringworm”—type of dermatophytosis…
Annular lesion with raised peripheral scaling and central clearing (looks like a ring!)

A) Tinea corporis
A 5-year-old child presents with a red, itchy rash on the arms and legs. The mother reports that the child has been scratching the rash for the past week. Upon examination, you observe circular, well-defined, erythematous patches with raised, scaly borders and clear centers. The child has no fever or other systemic symptoms. What is the most likely diagnosis for this child?
A) Tinea corporis
B) Eczema
C) Impetigo
D) Psoriasis
Tinea Versicolor
Fungal Infection:
Presents as hypopigmented lesions on the upper body.
Superficial tan or hypopigmented oval scaly lesions, especially on the upper back, chest, and proximal arms.

B) Tinea versicolor
A 12-year-old child presents with multiple small, discolored patches on the back and chest. The mother reports that the child’s skin appears lighter in some areas and darker in others, and that the patches do not tan well in the sun. Upon examination, you notice oval-shaped, hypopigmented or hyperpigmented patches with fine scales, especially on the upper back, chest, and shoulders. The child has no fever or systemic symptoms. What is the most likely diagnosis for this child?
A) Psoriasis
B) Tinea versicolor
C) Vitiligo
D) Eczema
Oral Candidiasis
Fungal Infection
Sources:
Breastfeeding infant
Corticosteroids
Antibiotics
Immunocompromised
Treatment:
Nystatin or Clotrimazole (for adults)
Nursing Care:
Apply medication with a swab or use "swish and swallow" technique.
Sterilize bottles, nipples, pacifiers, etc.

A) Oral candidiasis
A 9-month-old infant is brought to the clinic with white, patchy lesions on the inside of the mouth, including the tongue and the roof of the mouth. The mother reports that the baby has been more fussy than usual while feeding and seems to have difficulty sucking. Upon examination, you observe white, curd-like patches that can be scraped off, leaving behind a reddened surface underneath. The infant has no fever. What is the most likely diagnosis for this infant?
A) Oral candidiasis
B) Herpes simplex virus infection
C) Teething rash
D) Hand, foot, and mouth disease
Dermatophytoses
Fungal Infection
Common Sites:
Hands
Skin
Nails
Dry, Scaly Patches:
May be circular with a central clearing.
Often seen in immunocompromised individuals.
Treatment:
Keep the area clean and dry.
Oral antifungals such as Griseofulvin.—monitor liver enzymes.
Check pets and family members for infection.

Acne Vulgarius
Inflammatory:
It affects about 85% of adolescents between the ages of 7-16.
This occurs most frequently on the face, chest, and back.
Risk Factors:
Pre- or adolescent age
Male gender (due to androgens)
Oily complexion
Management:
Focuses on reducing Propionibacterium acnes, sebum production, normalizing skin shedding, and eliminating inflammation.
Medications:
Benzoyl peroxide
Salicylic acid
Retinoids
Topical or oral antibiotics
In girls, oral contraceptives may help lessen acne by decreasing the effects of androgens on the sebaceous glands.
Other Treatments:
Diode laser or blue UV light therapy
CO2 laser and dermabrasion may be used to treat pitted scarring.

A) Acne vulgaris
A 10-year-old child comes to the clinic with small, itchy bumps on the face and back. The child has been experiencing breakouts for the past few weeks, with the lesions appearing mostly on the forehead, chin, and shoulders. On examination, you observe comedones (blackheads), pustules, and papules. The child’s mother reports that the child is stressed due to schoolwork and has recently noticed the condition worsening. What is the most likely diagnosis for this child?
A) Acne vulgaris
B) Atopic dermatitis
C) Tinea corporis
D) Contact dermatitis
Acne Vulgarius: Classifications of Acne
Mild:
Primarily non-inflammatory lesions (comedones).
Moderate:
Comedones plus inflammatory lesions such as papules or pustules (localized to face or back).
Severe:
Lesions, similar to moderate acne, but more widespread, and/or presence of cysts.
Associated more frequently with scarring.

Atopic Dermatitis
Inflammatory Genetic immune disorder; also called eczema.
Characterized by lichenification, extreme itching and inflamed, reddened, and swollen skin, scaly.
Erythematous patches:
Vesicles, crusts.
Pruritus.
Nursing Care:
Wet (moist) dressings for oozing.
Occlusive for moisture.
Assess environment (moisture, dust mites, and cat dander).
Medications: Antihistamines, corticosteroids, antibiotics (treating secondary infection), immunomodulators (blunting their immune system so they aren’t as sensitive).

A) Atopic dermatitis
A 2-year-old child is brought to the clinic with a red, scaly rash on the cheeks and forehead. The mother mentions that the rash has been present for about a week and seems to be getting worse. The child is also scratching the area frequently, and the skin appears dry and cracked in some spots. The mother reports that the child has a history of asthma and seasonal allergies. The child has no fever. What is the most likely diagnosis for this child?
A) Atopic dermatitis
B) Seborrheic dermatitis
C) Impetigo
D) Contact dermatitis
Contact Dermatits
Inflammatory
Causes:
Antigenic substance exposure.
Allergy to nickel or cobalt in clothing, hardware, or dyes.
Exposure to highly allergenic plants:
Poison ivy, oak, and sumac.
Complications:
Secondary bacterial infections.
Lichenification or hyperpigmentation, particularly in dark-skinned people.
Medications:
Antihistamines, corticosteroids, antibiotics.

C) Contact dermatitis
A 3-year-old child is brought to the clinic with red, inflamed patches around the mouth and chin. The mother mentions that the child has been drooling more than usual due to teething and has been wiping the mouth frequently. On examination, you observe erythematous, scaly lesions around the mouth and chin area, with some crusting and mild excoriation from scratching. The child does not have any signs of fever or systemic infection. What is the most likely diagnosis for this child?
A) Impetigo
B) Diaper dermatitis
C) Contact dermatitis
D) Oral candidiasis
Diaper Dermatitis
Inflammatory reaction of the skin in the diaper area:
This is a non-immunologic response to a skin irritant.
Prolonged exposure to urine and feces may lead to skin breakdown.
Diaper wearing increases the skin’s pH, activating fecal enzymes that further contribute to skin maceration.
Nursing Care:
Prevention is key to management.
Frequent diaper changes.
Topical agents such as Vitamin A, D, E; zinc oxide, nystatin, or petroleum.

A) Diaper dermatitis
A 3-year-old child presents to the clinic with a red, inflamed rash in the diaper area. The rash appears as shiny, red patches with well-defined borders. The mother reports that the child has been having more frequent bowel movements than usual. The child has not had any fever or systemic symptoms, and the rash has not improved with regular diaper cream. What is the most likely diagnosis for this child?
A) Diaper dermatitis
B) Atopic dermatitis
C) Contact dermatitis
D) Oral candidiasis
Seborrheic Dermatitis
Inflammatory dermatitis that occurs on the skin or scalp.
In infants, it most often occurs on the scalp, and it's called Cradle Cap.
This usually resolves over weeks or months.
In adolescents, it typically develops on the scalp, eyebrows, eyelashes, behind the ears, and between the shoulder blades.
Nursing Care:
Medications: Anti-dandruff shampoos containing selenium sulfate, ketoconazole, and corticosteroids.

A) Seborrheic dermatitis
A 6-month-old infant is brought to the clinic with yellow, greasy, scaly patches on the scalp. The mother mentions that the baby’s scalp has been flaky for several weeks and that the patches seem to be getting worse. Upon examination, you notice well-demarcated, yellowish scales around the hairline and behind the ears. The baby does not appear to be in any pain, and there is no sign of redness or irritation elsewhere on the skin. What is the most likely diagnosis for this infant?
A) Seborrheic dermatitis
B) Atopic dermatitis
C) Psoriasis
D) Impetigo
Pediculosis
Infestation:
Transmitted from human hair.
Nits are attached to the hair shaft.
Nursing Management:
Assess with a bright light and magnifying glass.
Nit removal/pediculicide shampoo.
Prevention and environmental control.

A) Pediculosis
A 7-year-old child is brought to the clinic with complaints of intense itching on the scalp. The mother reports that the child has been scratching the scalp frequently, especially behind the ears and at the nape of the neck. Upon examination, you notice small, red bumps on the scalp, as well as tiny white eggs (nits) attached to the hair shafts close to the scalp. The child has no fever or systemic symptoms. What is the most likely diagnosis for this child?
A) Pediculosis
B) Tinea capitis
C) Atopic dermatitis
D) Scabies
Scabies
Infestation:
Transmitted through skin-to-skin contact.
Mites burrow into the epidermis.
Presents as papules, pustules, and burrows.
Causes intense pruritus (itching).
Nursing Management:
Apply scabicide lotion as prescribed.
Emphasize prevention and environmental control (wash bedding/clothes, vacuum, and treat close contacts to avoid reinfestation.)
Treatment:
Step 1: Initial Treatment → Kills live mites but not eggs.
Step 2: Follow-Up (10–14 days later) → Kills newly hatched mites before they mature.

A) Scabies
A 7-year-old child is brought in with complaints of intense itching and red, raised bumps on their body. Upon examination, you notice small, fluid-filled blisters located in the spaces between the fingers, on the wrists, and along the waistline. Additionally, you observe linear, grayish burrows in the skin, particularly around the wrists and between the fingers. The child’s mother mentions that the child has been scratching the areas for several days and has noticed that the rash appears to worsen at night. What is the most likely diagnosis for this child?
A) Scabies
B) Pediculosis
C) Erythema multiforme
D) Folliculitis
Erythema Multiforme
Acute, Self-Limiting Hypersensitivity Reaction
May occur in response to viral infections (e.g., Adenovirus, Epstein-Barr virus), Mycoplasma pneumoniae infection, or a drug (e.g., sulfa drugs, penicillins, immunizations) or food reaction.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are the most severe forms.
Nursing Care:
Management is generally supportive, as it resolves on its own.

A) Erythema multiforme
A 12-year-old child is brought to the clinic with a red, target-shaped rash on the arms, legs, and torso. The child’s mother reports that the rash developed suddenly a few days after the child was prescribed an antibiotic for a recent upper respiratory infection. The child also developed mild flu-like symptoms before the rash appeared. Upon examination, you notice raised, red lesions with a central area of pallor and concentric rings, resembling a target. The child has no fever, but the rash appears to be spreading. What is the most likely diagnosis for this child?
A) Erythema multiforme
B) Scarlet fever
C) Acute urticaria
D) Viral exanthem
Viral Rashes
Viral Exanthem:
Ex: Hand, foot, and mouth disease.
A rash.
Can look serious; if you rub or wipe the baby's back, the rash will fade and then reappear.
Bothers others more than the baby.
Herpes Simplex:
Pearly, clustered lesions.

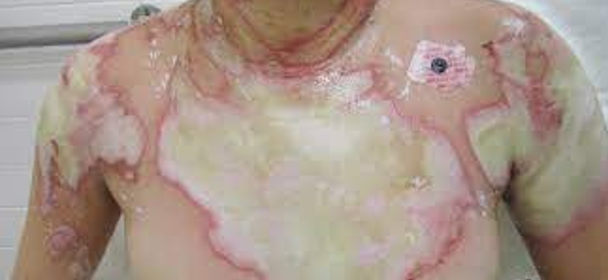
Burns are the…
3rd leading cause of accidental death in U.S. children.
Most are preventable.
High-Risk Groups:
Children under 4 years old
Working males
Elderly over 70 years
Burn Assessment: Age Groups
Risks Associated with Age:
Infant: Thermal burns
Accidental or abuse
Toddler: Thermal, electrical, contact
Exploration of the environment
Preschool: Scalding, contact
Hot appliances
School-Age and Adolescent: All types
Experimentation/Risk taking
Factors Affecting Burn Severity
Depth
Size
Location
Age of Person
Medical History
Cause
Children
Which population is more at risk for a higher body surface area involvement burn?
Adult vs. Children
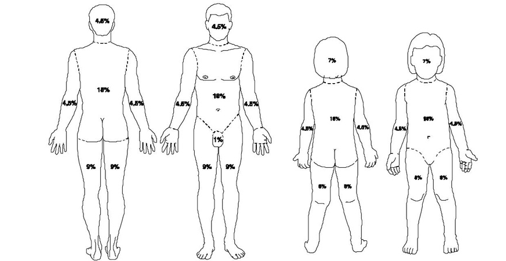
Assessing Burns in Children: Body Surface Area and Proportions
In children, the head is larger in proportion to other body parts or surface area, and they have a greater body surface area.
The head proportion decreases as they grow.

Location of Burns & What They Mean
Head and Neck:
Smoke inhalation, lung damage, alteration in respirations.
Circumferential:
Circular occlusion of the chest or extremity (compartment syndrome).
Electrical:
Cause of deep damage; electrical conduction can affect the heart. (rx for arrhythmias)
Perineal:
High risk of contamination.
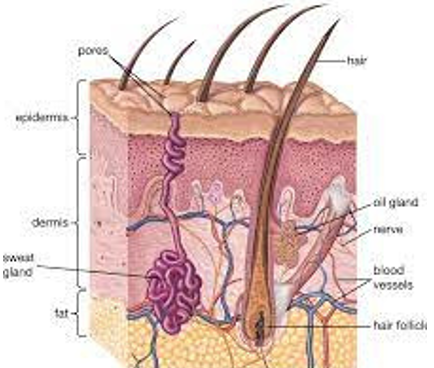
1st Degree Burn
Superficial Partial Thickness
Epidermis only, quick healing.

2nd Degree Burn
Partial Thickness
Epidermis + upper dermis
10-14 days healing
Very painful

3rd Degree Burn
Full Thickness
All layers
Grafting required
Affects underlying structures
No pain because nerves are destroyed

Intracellular Dehydration, Extracellular Edema-Hemovolemic Stage
Burn Response:
Increased capillary permeability → plasma leaks, causing edema.
Occurs within the first 24 hours after the initial burn.
Causes increased heart rate, decreased blood flow, and decreased urine.
Increased HCT
Fluid shifts → dehydration & swelling.
Increased epinephrine, ADH, and aldosterone.
Interventions:
Monitor vital signs & I&O.
Encourage PO fluids and IV fluids; give blood replacement as ordered.
Watch for metabolic acidosis.
Full-Thickness Burn: Initial Care
Assess Airway: Elevate head of bed (HOB), monitor pulse ox.
Maintain Fluids: Prevent hypovolemic shock from third spacing.
Promote Tissue Perfusion: Assess eschar carefully.
Control Pain: Medicate before dressing changes.
Prevent Infection: Use gown, gloves, and mask for protection.

Full-Thickness Burn: Special Care Needs
Escharotomy: Surgical incision to relieve pressure and improve circulation.
Debridement: Removal of dead tissue to promote healing.
Grafting:
Autograft: Skin from patient's own body.
Xenograft: Skin from another species (e.g., pig).
Homograft: Skin from a human donor.
Special Areas:
Eye, Lip, Hand Damage: Attention to these areas in children to preserve function and appearance. (vision, airway, and dexterity—PT needed)
Perineal Area: High risk for infection, manage carefully.

Full-Thickness Burn: Later Care
Control Pain (nerve endings start coming back)
Prevent Infection
Promote Physical Mobility
Monitor for GI Alterations
Ensure Adequate Nutrition and Fluid Balance
Provide Anxiety Management
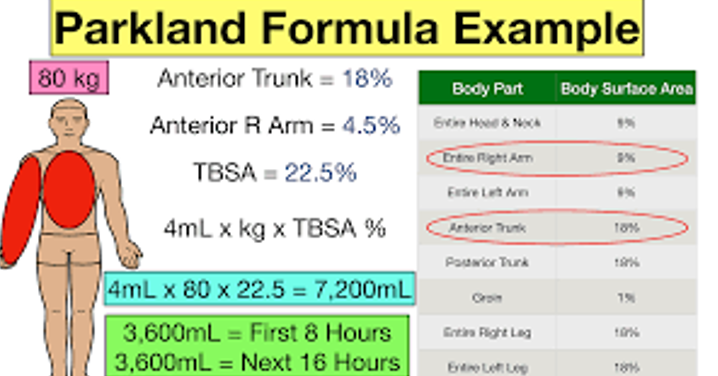
Restoring and Maintaing Fluid Volume: Parkland Formula
A fluid calculation based on the body surface area burned. (Restoration)
Use of a crystalloid (Lactated Ringers) during the first 24 hours (dextrose might be added for smaller children).
During the first 8 hours, half of the calculated fluid volume is given.
For the next 16 hours, the remaining half is given.
Monitor:
Cap Refill
Daily Weights
Urine Output (at least 1 mL/kg/hr)
Electrolytes (sodium and potassium).
Burns: Family & Psychological Support
Support Groups
Counseling
Camps
Ameriburn.org (American Burn Association)
Burns: Child Abuse
Inconsistent history given when caregivers are interviewed separately.
Delay in seeking treatment by the caregiver.
Uniform appearance of the burn, with clear delineation of the burned and non-burned areas (as with a hot object applied to the skin, e.g., cigarette burns).
In the case of scald-induced burns, lack of patterning of water but evidence of so-called “porcelain-contact sparing,” where the portion of the child’s skin that was in contact with the tub or sink is not burned (commonly seen with forced immersion in extremely hot water used as punishment).
Flexor-sparing burns or burns that involve the dorsum of the hand.
A stocking/glove pattern on the hands or feet (circumferential ring appearing around the extremity, resulting from a caregiver forcefully holding the child under extremely hot water).

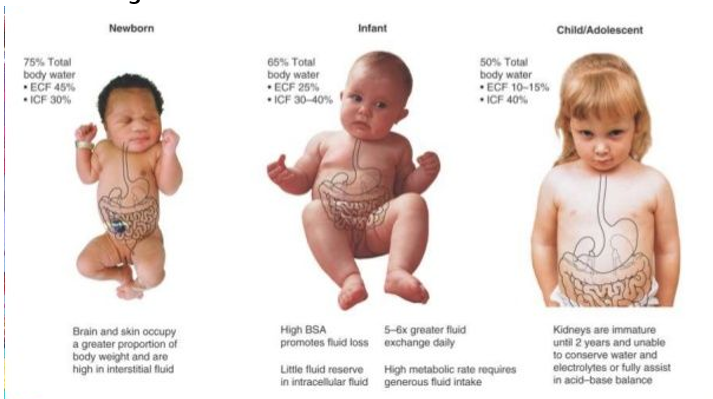
Fluid Balance: Pediatric Considerations
Have a proportionally greater amount of body water than adults.
Infants/toddlers have more extracellular fluid, so water loss occurs more rapidly.
More insensible water loss with fevers.
More body surface area.
Infants may have more difficulty concentrating their urine.
Fluid Changes in Children
Newborn:
Brain & skin occupy a greater proportion of body weight & are high in interstitial fluid.
Infant:
High body surface area promotes fluid loss, 5-6x greater fluid exchange daily, little fluid reserve in intracellular fluid, & high metabolic rate requires high fluid intake.
Child/Adolescent:
Kidneys are immature until 2 yr old & unable to conserve water & electrolytes or fully assist in acid-base balance.
3 Types of Dehydration
Isotonic
Hypotonic
Hypertonic
Isotonic Dehydration
The same amount of salt inside and outside the cell.
Ex: Diarrhea and vomiting

Hypotonic Dehydration
Less salt outside of the cell. The body pulls more water into the cell to compensate.
Ex: Renal disease
Hypertonic Dehydration
More salt outside of the cell. Caused by losing more water than sodium. The body pulls more water out of the cell.
Ex: Diabetes Insipidus, tube feeding with high electrolytes
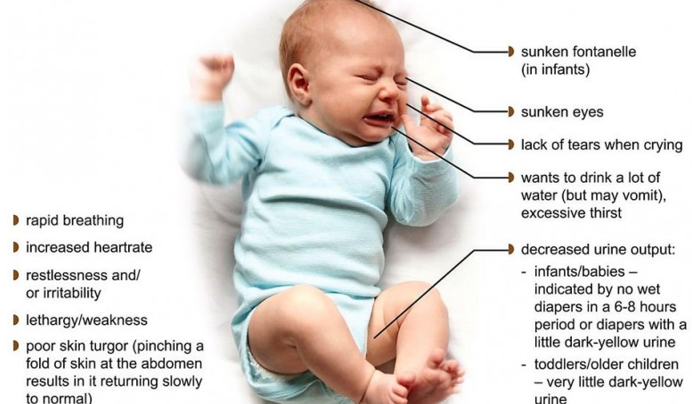
Signs of Dehydration
Dry skin, mucous membranes
Poor turgor
Sunken fontanelle
Poor perfusion
Weight loss
Tachycardia
Tachypnea
High urine specific gravity (may not be seen in younger)
High hematocrit, BUN, and serum osmolality
Urine less than 1 mL/kg/hour
What is the normal urine output for a child?
1 mL/kg/hr
Daily Weight Change
1 kg change = 1000 mL fluid change
Weight Loss Indication of Dehydration
5% loss = MILD—irritable, normal vitals, skin & fontanelle normal, dry mucous membranes, low urine.
6-9% loss = MODERATE—restless, high HR, pulse faint, turgor poor, mucous membranes dry, sunken fontanelles, low output.
10% + loss = SEVERE—lethargic-comatose, low BP, increased HR, impalpable pulse, skin cool, mottled, cyanotic, urine low to none.
Nursing Care for Extracellular Fluid Volume Deficit
Prevent Dehydration (small frequent sips)
Close Assessment
Daily Weights
Strict I&O
Oral Rehydration Therapy (recommended)
IV Therapy
Family Teaching
Maintenance Fluid Needs for Children
< 10 kg: 100 mL/kg of weight = # mL for 24 hours. [total max = 1,000]
11-20 kg: 1000 mL (for the first 10 kg) + (50 mL/kg for the next 10 kg) = # of mL for 24 hours. [total max = 500]
> 20 kg: (10 × 100 = 1,000) + (10 × 50 = 500) + (20 × # kg above 20) = # of mL for 24 hours.
So, 1500 mL + 20 x ( # of kg above 20)
**Remember!! Make sure to calculate the patient’s orginal weight before the weight loss. The whole point is to rehydrate the patient, not keep them dehydrated!**
![<ul><li><p><strong><u><</u> 10 kg</strong>: 100 mL/kg of weight = # mL for 24 hours. [total max = 1,000]</p></li><li><p><strong>11-20 kg</strong>: 1000 mL (for the first 10 kg) + <u>(50 mL/kg for the next 10 kg)</u> = # of mL for 24 hours. [total max = 500]</p></li><li><p><strong>> 20 kg</strong>: (10 × 100 = 1,000) + (10 × 50 = 500) + <u>(20 × # kg above 20)</u> = # of mL for 24 hours.</p><ul><li><p> So, 1500 mL + 20 x ( # of kg above 20)</p></li></ul></li></ul><p><strong><u>**Remember!! Make sure to calculate the patient’s orginal weight before the weight loss. The whole point is to rehydrate the patient, not keep them dehydrated!**</u></strong></p><p></p>](https://knowt-user-attachments.s3.amazonaws.com/b9b00b16-67bb-4138-88cf-076563dbc3e3.png)
Maintenance:
1500 mL + 20 mL/10kg/24 hr →
1500 mL + 200 mL = 1700 mL/day
10 year old Alex is admitted for severe dehydration. His normal weight is 30 kg but today he weighs 27 kg. Calculate his maintenance and replacement fluid needs for the next 24 hours.
False; The patient was admitted for hyperkalemia. Potassium should not be added to his IVF's until his levels have normalized.
Cameron is a 15kg, 4yo, who presented with hyperkalemia and dehydration after having an AGE. Dr. Brown ordered maintenance IV fluids after receiving a 20 ml/kg NS bolus in the ED. Is this the correct rate?
D5 1/2 NS with 20 KCL @ 50 ml/hr
Extracellular Fluid Excess
Common Causes:
Excessive isotonic IV fluids
Diseases like CHF or Renal Disease
Medications like Prednisone
Symptoms:
Weight Gain
Edema
Respiratory Crackles
Respiratory Distress
Nursing Care for Extracellular Fluid Excess
Strict I&O
Daily Weights
Fluid Restrictions
Frequent respiratory assessment
Elevate edematous body parts
Diuretics
Measure abdominal girth
Meticulous skin care
Types of Electrolyte Imbalances
Hyponatremia
Hypernatremia
Hypokalemia
Hyperkalemia
Sodium helps with…
Fluid balance in the body, blood pressure, muscle and nerve function, cellular homeostasis, and nutrient transport through plasma membranes.
Potassium helps with…
Muscle contraction, nerve transmission (nerve impulses), kidney function (prevents stones), lowers blood pressure, bone health, potassium helps reduce calcium loss in urine, and helps maintain intracellular fluid.
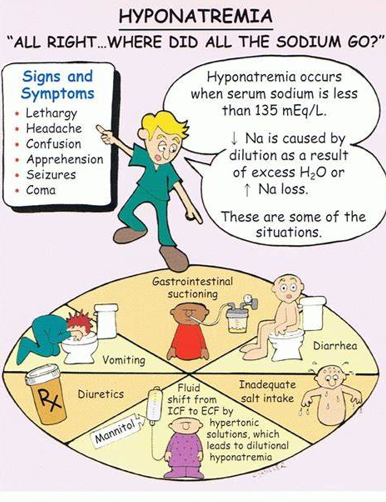
Hyponatremia
Serum Na below 135 mmol/L
Causes:
Excessive water intake
Excessive ADH
Excessive hypotonic IV fluids (D5W)
Irrigation with water instead of NS
Symptoms:
May lead to cerebral edema
Seizures or coma
Management:
Isotonic (0.9% NS) or Hypertonic (D5LR) IVF may be given.
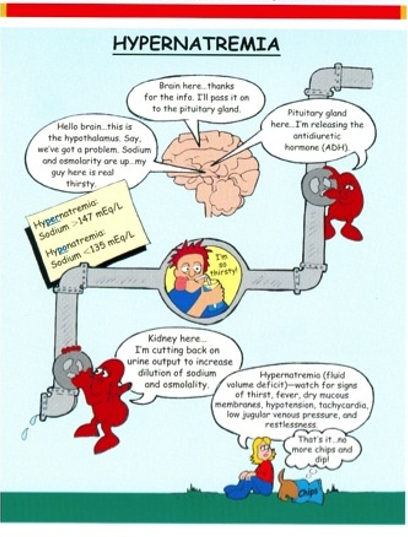
Hypernatremia
Serum Na greater than 148 mmol/L
Causes:
Not drinking enough water
Undiluted formula
Diarrhea or vomiting
Symptoms:
Symptoms from shrinking of brain cells: confusion, seizures, coma.
Management:
Hypotonic IV fluids
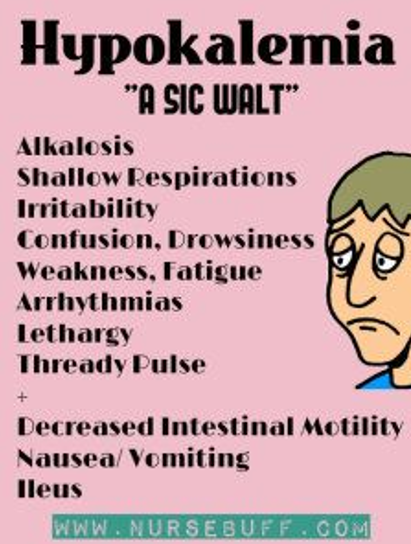
Hypokalemia
Serum K+ below 3.5 mmol/L
Causes:
No potassium in IVF
Loss of gastric secretions
Diuretics
Low potassium diet
Symptoms:
Muscle weakness
Respiratory distress
Decreased cardiac output
Management:
High potassium diet
IVF with potassium
Monitor urine output, cardiac, and respiratory function.
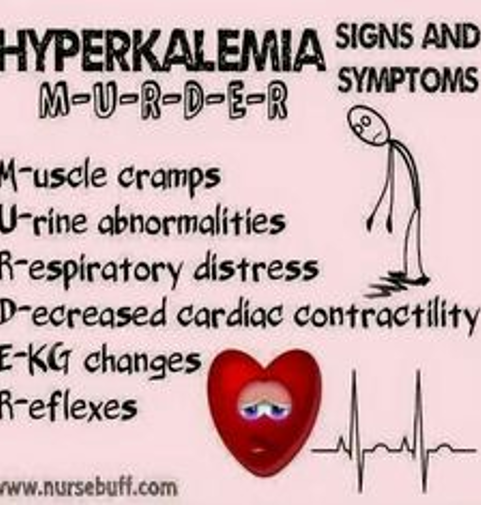
Hyperkalemia
Serum K+ greater than 5.8 mmol/L
Causes:
Renal insufficiency
Too much potassium in IVF
Blood transfusions
Symptoms:
Weakness
Increased GI motility
Tachycardia/Arrhythmias
Oliguria/Anuria
Management:
Prevention
IVF
Monitor cardiac, musculature, renal, and GI systems