Neuro/Degenerative Disorders
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
133 Terms
Neurologic Dysfunction Disorders
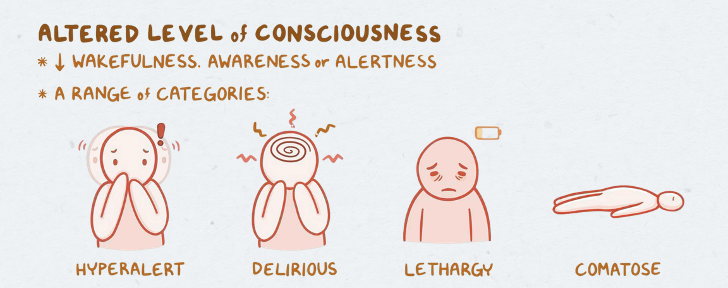
Altered Level of Consciousness
Delirium
Dementia
Seizures
Headaches
Altered Level of Consciousness: Etiology
Result of multiple pathophysiologic phenomena
Neurologic (head injury, stroke)
Toxicologic (drug overdose, alcohol intoxication)
Metabolic (hepatic or kidney injury, DKA)
Disruption of cells, neurotransmitters, or brain anatomy → dysfunction in how the CNS communicates & coordinates function
Altered Level of Consciousness: Clinical Manifestations
Changes in alertness & consciousness → alterations in pupillary response, eye opening, verbal response & motor response
Behavioral changes: restlessness, anxiety
Comatose:
Pupils responsive to light? → Possible toxic or metabolic etiology
Altered Level of Consciousness: Range of Categories (image + info)
Coma = state of unarousable unresponsiveness to internal and external stimuli, but can be responsive painful stimuli & brain stem reflexes may be present ---- presentation varies
Akinetic mutism: not responsive to environment through voluntary movement
Vegetative state: unresponsive but resumes sleep-wake cycles after coma; cognitive or affective mental function absent
Minimally conscious state: similar to vegetative but they have some reproducible signs of awareness
Locked-in syndrome: paralysis & inability to speak but are aware of environment; vertical eye movements & lid elevation intact
Altered Level of Consciousness: Assessment + Diagnostics
Assessment:
Altered LOC can affect other body systems
Evaluation of:
Mental status
Cranial nerve function
Cerebellar function (balance & coordination)
Reflexes
Motor & sensory function
Glasgow Coma Scale (GCS):
Score of 3 = severe impairment of neuro function
Score of 15 = fully responsive
Diagnostics:
Imaging:
CT, PCT
MRI/MRS
MRI = better at showing tumor size and blood vessel location
MRS = compares the chemical composition of the normal brain tissue w/ the abnormal
EEG
PET/SPECT
3D images of the head that help w/ assessing tumors and how responsive they are to treatment
Laboratory Tests:
Blood glucose
Comprehensive Metabolic Panel (CMP) - electrolytes, serum ammonia, liver function tests
Calcium level
Blood urea nitrogen (BUN)
Serum osmolality
Partial thromboplastin (PT) & prothrombin times (PTT)
Serum ketones
Alcohol & drug concentrations
Arterial blood gases
Altered Level of Consciousness: Management
Obtain & maintain a patent airway:
Oral or nasal intubation
Tracheostomy
Mechanical ventilation may be required until patient’s ability to breathe on their own is clear
Monitor circulatory status (blood pressure & heart rate)
Obtain intravenous (IV) catheter for fluids & meds
Nutritional support—via feeding tube or gastrostomy tube (G-tube)
Determine and treat underlying cause of altered LOC
Pharmacological management (depending on cause)
Prevent further complications
Delirium
Acute confusional state that starts with disorientation that can progress to changes in level of consciousness, irreversible brain damage, and sometimes death.
Delirium: Background
Can be considered a medical emergency d/t alteration in LOC
Also known as acute confusional state
Often mistaken for dementia
Acute & unexpected onset
Up to 80% of ICU patients affected
Risk factors:
Use of benzodiazepines
Administration of blood transfusions
Age
Presence of dementia
Prior coma
Recent emergency surgery or trauma
Delirium: Clinical Manifestations
Disorientation, confusion
Agitation, restlessness, aggressive behavior
Lethargy, withdrawn behavior
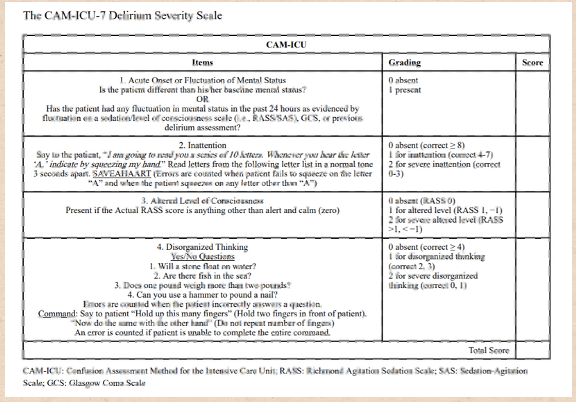
Delirium: Assessment + Diagnostics
Ongoing mental status assessments
Routine screening for all critically ill patients (for better recognition):
The Confusion Assessment Model (CAM) & Delirium Index (DI)
CAM = questions about acute onset, inattention, disorganized thinking, altered LOC, disorientation, memory impairment, perceptual disturbances, psychomotor agitation, psychomotor slowing, altered sleep-wake cycle
Patient’s baseline mental status - onset of change
Lab tests & imaging to rule out other causes—NO definitive lab tests or diagnostic procedure to diagnose
Delirium: Management
Prevention is most effective
Treat the underlying cause
Minimize use of psychoactive drugs
Delirium: Nursing Interventions
Assess for changes to cognition, memory, judgment and personality
Providing therapeutic activities for cognitive impairment:
Safe, quiet, & calm environment
Provide familiar environmental cues to reorient
Alternative communication methods
Maintain oxygen levels and fluid & electrolyte balance – Monitor I&Os carefully
Include the family in care, if appropriate
Ensure early, safe mobilization
Pain control
Notify provider about any nonessential meds that can be discontinued
Promote proper sleep hygiene
Encourage use of eyeglasses & hearing aids
Understand the patient’s usual mental status
Provide toileting schedule
Provide finger foods
Patient & family support:
Can be very disturbing for families
Dementia
Multiple cognitive, functional, and behavioral changes that destroy a person’s ability to function over time.
Dementia: Background
Onset: subtle, but progresses slowly over time
Usually cause from neurodegeneration
Most common: Alzheimer’s disease (AD)
After diagnosis, average survival is ~10 years
Risk factors:
Advanced age, chemical imbalances, family history, previous head injury, assigned female at birth, ethnicity/race
AA & Hispanic people at increased risk
Dementia: Clinical Manifestations
Memory problems
Personality changes
Loss of awareness, wandering behavior
Disrupted sleep/wake cycle
Decline in cognition
Ataxia
Progression different for each person
Dementia: Assessment + Diagnostics
Health history (family as historian typically)
Lab testing to rule out other causes
MRI, CT/CAT, PET, EEG
LP/CSF evaluation
Dementia: Nuring Interventions + Management
Assess for changes in cognition, memory, judgment and personality
Establish schedule for bowel & bladder program
Family education about home safety measures:
Rugs, door locks & alarms, place mattress on the floor, shower chairs, medical ID bracelets
Sundowning: phenomenon among patients with dementia experience increased agitation, confusion in late afternoon & early evening; more wandering, restlessness, etc.
Unknown cause – possible fatigue, circadian rhythm disturbances
Keep a consistent routine
Calm environment
Address triggers: hunger, pain, etc.
Promote safe, quiet & calm environment
Frequent walks
Weekly skin checks
Encourage cognitive stimulation & memory training
Medications to target behavioral & emotional issues
AD meds: donepezil, memantine, cholinesterase, pimavanserin
Seizures
Paroxysmal transient disturbance of brain, leading to discharge of abnormal electrical activity
Seizures: Pathophysiology
Electrical disturbance (arrhythmia) in nerve cells in one part of the brain
Episodes of abnormal motor, sensory, autonomic or psychic activity (or a combo of these)
Abnormal, recurring uncontrolled electrical discharge
Seizures: Background
Causes:
Allergies, brain tumor, cerebrovascular disease, CNS infections, drug & alcohol withdrawal, childhood fever, head injury, hypertension, hypoxemia of any cause
Metabolic & toxic condition: kidney injury, hyponatremia, hypocalcemia, hypoglycemia, pesticide exposure
Genetic etiology: structural & metabolic abnormalities
Epilepsy: more than one unprovoked seizure
Seizures: Clinical Manifestations
Varies depending on the location of discharging neurons:
Epileptic cry—contraction of diaphragm & chest muscles
Limb shaking
Mouth jerking
Dizziness
Speak unintelligibly
Unusual sensations
Postictal state—may be confused, lethargic, agitated
Seizures: Assessment + Diagnostics
Assessment:
During:
What happened before - consider type of stimuli, disturbances, sleep, hyperventilation
Presence of an aura
Characteristics of the episode - what does the episode look like?
Size & reactivity of pupils
Incontinence of urine or stool
Time of onset & duration of each phase
After:
Any obvious paralysis or weakness of arms or legs after seizure?
Movements after? Is the patient sleepy? Able to talk?
Cognitive status - confused?
Diagnostics:
Aim = to determine type of seizure, frequency & severity and factors that trigger them
Physical & neurologic exams
MRI
EEG (sometimes with video)
Telemetry & pulse oximetry
SPECT
Seizures: Medical Management
Pharmacologic Therapy:
Control > cure
Anticonvulsants
Monitor for drug toxicity
Surgical Management:
EEGs with depth electrodes
Hemostasis
Reduction surgery
Vagus nerve stimulator
Seizures: Nursing Interventions
Protect the patient’s airway:
Risk for hypoxia, vomiting, & aspiration
Perform suctioning as needed
Ongoing assessments of respiratory & cardiac function:
Monitor responsiveness
Provide privacy & maintain safety
Ease to floor & protect head
Place in side-lying position
Loosen constrictive clothing, remove glasses
Avoid restraining or prying jaw open
Maintain seizure precautions:
Place bed in lowest position
Raise 2-3 side rails & displace pillows
Suction, O2, padded side rails
Note the time of onset, duration, characteristics
Reorient the patient to the environment:
Guide to bed or chair if wandering
Keep distance but able to visualize if agitated
Seizures: Forms of Presentation
Tonic-clonic: full body stiffening & jerking w/ intermittent relaxing; loss of consciousness
Tonic: loss of consciousness, hypertonia
Clonic: rhythmic jerking & relaxing; last minutes
Absence: blinking, loss of consciousness; last seconds
Myoclonic: brief jerking & stiffening; last seconds
Atonic/akinetic: loss of muscle tone + confusion; few seconds
Complex partial: unconsciousness behaviors (lip smacking)
Simple partial: conscious; unusual sensations
Unknown: idiopathic; doesn’t fit into other categories
Status Epilepticus
Medical Emergency!
Lasts ≥ 5 minutes without full recovery
Stop seizures ASAP to ensure cerebral oxygenation
Vigorous muscular contractions → heavy metabolic demand → irregular respirations
Seizures: Special Considerations
Women:
↑ frequency during menses d/t ↑ sex hormones → affecting excitability of neurons in cerebral cortex
Family planning
Pregnancy:
↑ risk of congenital fetal anomaly 2-3x higher
Maternal seizures, anticonvulsants, genetic predisposition - possible malformations
Anticonvulsants - need careful monitoring
High risk pregnancies - higher risk of epilepsy
Damage to fetus during pregnancy or delivery
Bone loss r/t long-term use of anticonvulsant meds:
Assess for low bone mass & osteoporosis
Older Adults:
Altered pharmacokinetics
New onset epilepsy
Leading cause: CV disease
Treatment depends on cause
Polypharmacy & interactions
Monitor closely for adverse reactions & toxicity
At risk for osteoporosis
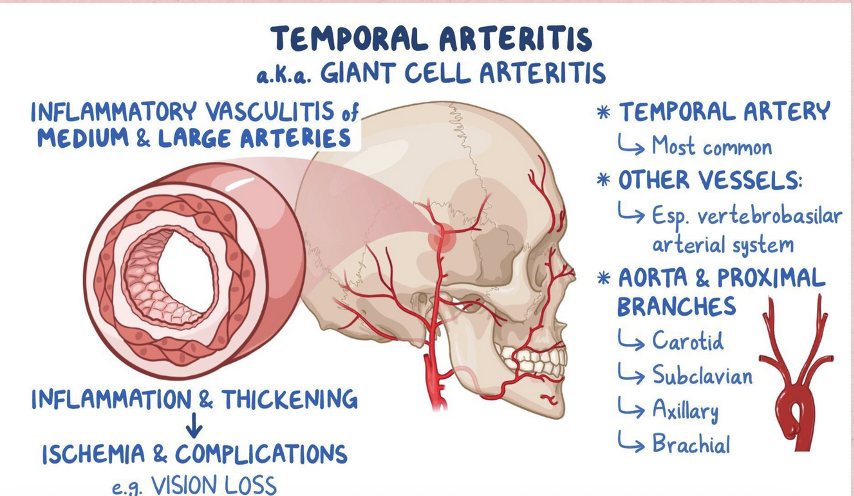
Headaches: Cranial Arteritis—Background + Clinical Manifestations
Background:
Common in elderly (older adults)
Inflammation of cranial arteries
Localized around temporal arteries
Clinical Manifestations:
Fatigue, malaise
Weight loss
Fever
Heat, redness, swelling, tenderness or pain over involved artery
Vision issues
Headaches: Tension—Background + Clinical Manifestations
Background:
Chronic, less severe
Very common
Stress → contraction of neck & scalp muscles
Patho unclear
Possibly dilation of orbital & adjacent extracranial arteries
Biopsy of artery to confirm
Clinical Manifestations:
Constant, band-like pressure on forehead, temple, and/or back of neck
“a weight on top of my head”

Headaches: Cluster—Background + Clinical Manifestations
Background:
Pretty uncommon
More frequent in men than woman
Triggered by cough, exertion, and sexual activity
Type of trigeminal autonomic cephalalgias
Clinical Manifestations:
Unilateral, migrating pain around eye and orbit that comes in episodes
Trigeminal autonomic cephalalgias—noted by pain on one side of the head with autonomic symptoms
Tearing, redness, nasal congestion on same side
Rhinorrhea, watery eyes
Pain described as penetrating, varying intensity

Headaches: Migraine—Background
Marked by periodic, recurrent attacks of severe headaches lasting from hours to days
Cause still unclear…
With or without aura (warning sensation)
What are some migraine headache triggers?
Menses
Bright lights
Stress
Depression
Sleep deprivation
Fatigue
Odors
Cheese, red wine, beer, chocolate (tyramine)
Monosodium glutamate (MSG)
Oral contraceptives for some
Headaches: Migraine—Pathophysiology (theory)
Stimulation → vascular changes, inflammation and continued pain signal stimulation
Hyper-excitable brain that’s more vulnerable to a wave of depolarization over the cerebral cortex, cerebellum, & hippocampus →
Inflammatory neuropeptides & other neurotransmitters activating →
Stimulation of meningeal nociceptors
Headaches: Migraine—Clinical Manifestations
Premonitory:
Depression, irritability
Feeling cold, light & sound sensitivity
Change in activity level
Food cravings, anorexia
Aura:
Vision disturbances
Slight extremity weakness
Mild confusion; drowsiness, dizziness
Numbness and tinging of lips, face or hands
Headache:
Pain, light & sound sensitivity
Nausea/vomiting
Cognitive difficulties & mood changes
Postdrome:
Fatigue, weakness
Headaches: Assessment + Diagnostics
Assessment: OLDCARTS
Detailed history:
**Purpose of hx - assess headache while considering possible factors that were precipitating or provoking the episode (different person to person!)
**Have the patient describe headache in their own words
Medications
Prescribed, OTC; complete hx
Anti-HTN, diuretics, anti-inflammatory agents, MAO inhibitors - known to provoke headaches
Family history
Triggers: stress, poor sleep habits, food
Occupational history
Toxins?
Medical & surgical history of all body systems
Physical assessment with focus on head & neck:
Frequency, location, quality, duration
Persistent headaches warrant investigation because it can be serious (brain tumors, subarachnoid hemorrhages, strokes, severe hypertension, meningitis, head injuries)
Neck stiffness— meningitis? spinal injury?
Thorough neurologic assessment
Diagnostics:
Usually not helpful due to lack of objective findings
CT
Cerebral angiography
MRI—to detect possible causes like tumors or aneurysm
Electromyography (EMG)—sustained contraction of neck, scalp, or facial muscles
CBC
Erythrocyte sedimentation rate (ESR)
Electrolytes
Glucose
Creatinine
Thyroid hormones
Headaches: Interventions
Goal: to relieve pain & provide comfort
Cranial arteritis:
Corticosteroids—prevent loss of vision d/t vascular occlusion or rupture --- DO NOT d/c
Migraine: abortive & preventative approaches
**Abortive = relieving or limit a headache at onset or while it's in progress
**Preventive = used for pts with more frequent episodes at regular or predictable intervals & might have medical condition that makes abortive therapies ineffective
**Migraine cocktail
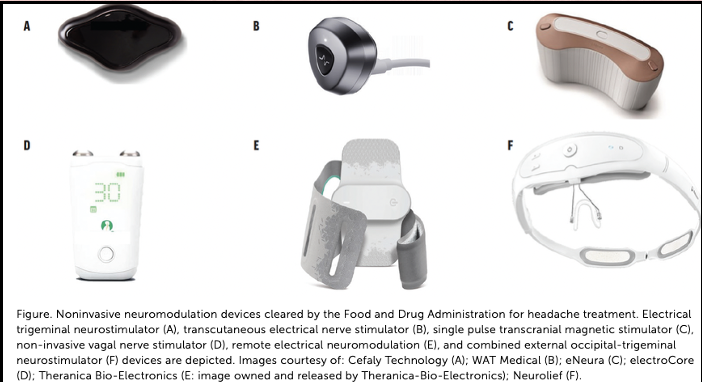
Non-invasive neuromodulation devices
Triptans (serotonin receptor agonists)
NSAIDs, antispasmodic agents, neuroleptics
Anti-emetics
Prophylaxis:
Beta-blockers, antiepileptics, antidepressants, ACE inhibitors, ARBs
Cluster:
100% O2 by facemask for 15 minutes
Sumatriptan (subcutaneous) & Zolmitriptan (nasal)
Vasoconstriction, anti-inflammatory, reduce pain
Tension:
Local heat or massage
Analgesics, antidepressants, muscle relaxants
Headaches: Prevention
Avoid specific triggers:
Alcohol—vasodilation of blood vessels
Nitrites, vasodilators, histamines
Foods with tyramine - chocolate, cheese, coffee, dairy products
Long periods between meals
Adhering to medication regimen
Regular sleep
Stress management—meditation, exercise, biofeedback
Environment:
Dark, quiet room
Elevating HOB to 30°
Cold compress
Headache diary
Hormonal fluctuations from menstrual cycle pattern can also affect migraines
Symptom management
Infections of the Nervous System
Meningitis
Herpes Simplex Encephalitis
Creutzfeldt-Jakob disease (CJD) & Variant CJD
Meningitis
Inflammation of the meninges, which cover and protect the brain & spinal cord
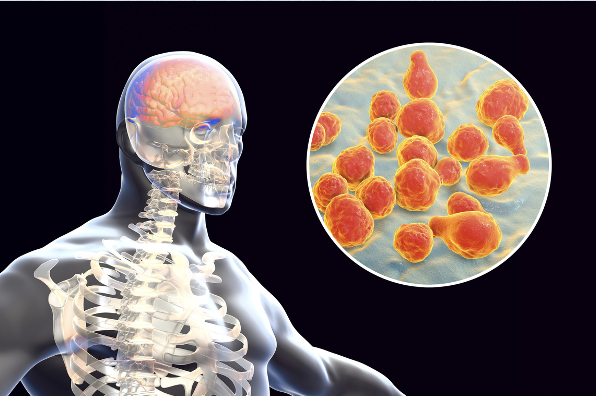
Meningitis: Background
Main types: bacterial (septic) & viral (aseptic)
Streptococcus pneumoniae and Neisseria meningitidis
Aseptic - secondary to cancer or r/t immunosuppression
Commonly due to enteroviruses
Immunization:
Haemophilus influenzae type B (Hib) vaccine
Pneumococcal polysaccharide vaccine (PPSV)
Meningococcal vaccine (MCV4): 1st year college students & members of the military
No vaccine for viral meningitis
Meningitis: Risk Factors
Bacterial: bacterial-based infections (otitis media, pneumonia, sinusitis) caused by N. meningitidis, S. pneumoniae, or H. influenzae
Viral: mumps, measles, herpes, arboviruses
Immunosuppression
Direct contamination of spinal fluid
Invasive procedures, skull fractures, or penetrating wounds
Environment—living in close quarters
Pathogen can travel through nose & throat, crossing blood-brain-barrier → bloodstream → CSF:
Head trauma, sinusitis → abscess, or organism just enters the bloodstream due to another infection
Can pass through the endothelial membrane to the subarachnoid space
Consequence of infection can be devastating → vascular necrosis and endothelial damage → neurological deficits, organ failure, seizures, etc.
Meningitis: Cause
Pathogen travels into bloodstream
↓
Crosses blood brain barrier
↓
Multiplies in CSF
↓
Host immune response
↓
Inflammation of subarachnoid space & pia mater
↓
↑ intracranial pressure
↓
Inflammatory materials circulates via CSF
↓
Endothelial damage & vascular necrosis
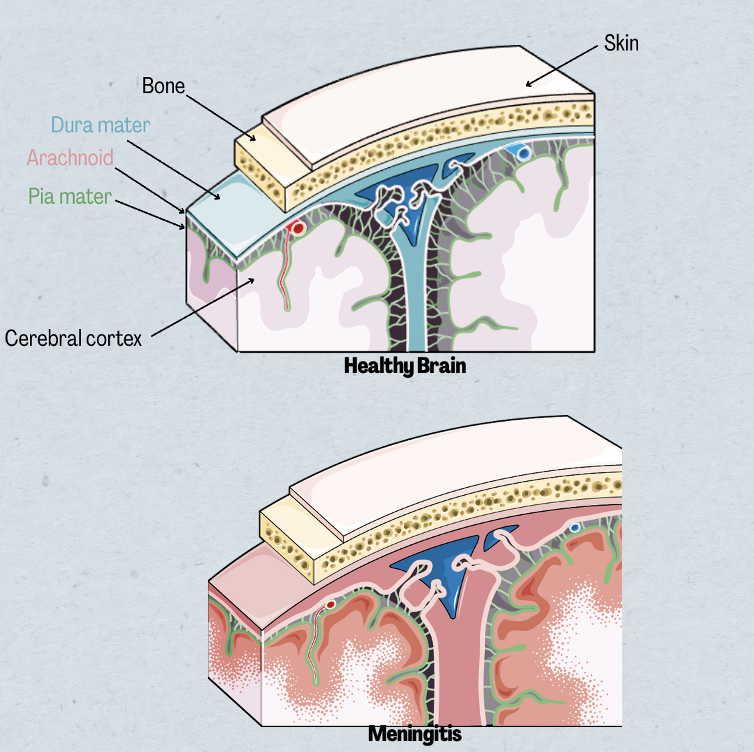
Meningitis: Clinical Manifestations
Fever & chills
Steady, throbbing headache
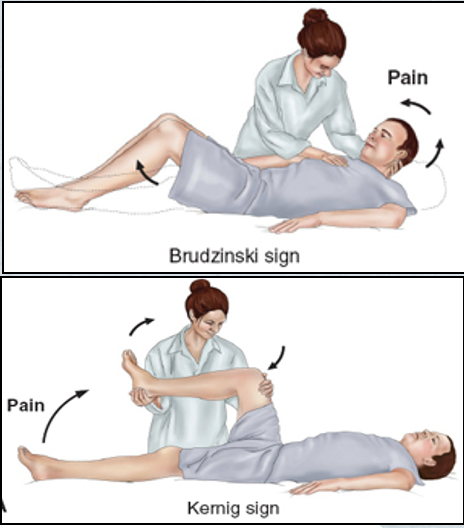
Nuchal rigidity:
Neck immobility—an early sign!
Trying to flex the neck causes spasms…
Positive Kernig sign:
Patient lying down with thigh flexed on abdomen, leg cannot be extended
If bilateral: meningeal irritation
Positive Brudzinski sign:
Patient's neck flexed → knees & hips flexed too
Lower extremity of one side is passively flexed, the same thing happens on the opposite extremity
Brudzinski > Kernig when indicating meningitis
Photophobia
Rash:
Common feature with meningococcal meningitidis (half of patients present with rash)
Skin lesions that have develop into varying degrees of petechiae, lesions and bruising
Disorientation & memory impairment
Seizures
Mental status changes
Irritability
Hyperactive DTRs
**Older adults - have more behavior changes & focal neurologic deficits
Meningitis: Assessment + Diagnostics
CT
MRI
Lumbar puncture & CSF analysis:
Glucose, ↑WBCs, ↑ protein, pressure
CBC
Urine, throat, nose, & blood culture & sensitivity
CT/MRI before LP
Rule out other conditions, especially those that may cause herniation from LP (altered LOC, papilledema, hx of CNS disease, being immunocompromised)
Specimen cultured and gram stained + blood culture
Gram staining → quick ID of causative bacteria à quickly starts on correct ABX therapy
CSF - assessment starts at appearance
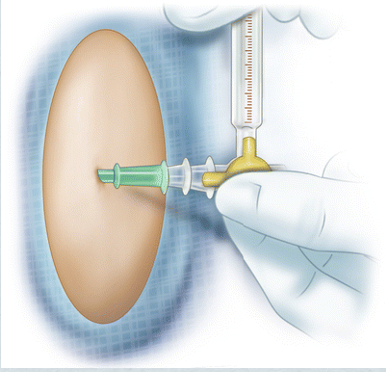
Measure pressure with manometer (looks like a giant traditional glass thermometer)
Cloudy (bacterial) & clear (viral)
↓ glucose (bacterial)
Collected before ABX!!!
Symptom driven: throat & nose cultures less common (not definitive for meningitis)
Meningitis: Treatment + Complications
Treatment:
Early administration of ABX
Penicillin G + cephalosporin IV
ABX → cross BBB into subarachnoid space → halt bacteria multiplication
Dexamethasone
Acute bacterial meningitis & pneumococcal if given with ABX & every 6 hrs for next 4 days
Fluid volume expanders
Shock & dehydration
Shown to improve outcomes in adults, no increased risk of GI bleed
Anticonvulsants
Treatment for ICP, if indicated
Also consider vaccine + ABX prophylaxis for anyone living with meningococcal infection
2 vaccines = recommended for children and adults who are at-risk
Exposed individuals:
Those exposed – 3 ABX
Rifampin, ciprofloxacin, or ceftriaxone
Started within 24 hours post exposure
Vaccine + ABX chemoprophylaxis
H. influenzae & S. pneumoniae vaccines
Complications:
Increased ICP:
Inflammation possibly to point of herniation
Monitor for s/sx
SIADH:
d/t abnormal simulation of area near hypothalamus → excess secretion of ADH
Concentrated urine (high osmolality) with lots of sodium
Low SERUM sodium
Daily weights
Septic emboli:
Forms during infection & moves to other parts of body → causing gangrene → DIC or stroke
Skin assessment + neurovascular assessments
Fever management
Meningitis: Interventions
Prevention!
Meningococcal conjugated vaccine
Isolate the patient immediately!
Droplet until 24 hrs post ABX
Report meningococcal infections to public health department
Supportive care
Manage fever
Neuro assessments & vital signs continually
Hydration
Monitor for early signs of shock
Seizure precautions
Prevent secondary complications
Family support
Rehabilitation
Health promotion
***Tell patient to try to avoid coughing and sneezing – could increase ICP
Herpes Simplex Encephalitis
Acute inflammatory process of brain tissue
Herpes Simplex Encephalitis: Background
Caused by herpes simplex virus (HSV) —most common (acute) cause of encephalitis
Marked by hemorrhagic tissue death → edema
Progressive deterioration of nerve cell bodies
Herpes Simplex Encephalitis: Clinical Manifestations
Initial symptoms of HSV: Fever, headache, confusion & hallucinations
Behavioral changes
Focal seizures
Dysphasia
Hemiparesis
Altered LOC
Herpes Simplex Encephalitis: Assessment + Diagnostics
EEG: diffuse slowing or focal changes in temporal lobe for most
CSF analysis (LP): high opening pressure, ↑ protein
MRI: detect inflammation = hypertense (bright) area
Polymerase chain reaction (PCR)*: early diagnostic test for HSV; very sensitive to genetic material of HSV

Herpes Simplex Encephalitis: Interventions
Antiviral agent: IV acyclovir for up to 3 weeks
Slow administration over 1 hour*—Admin slow d/t crystallization of med in urine
Early administration → improves prognosis
Inhibits viral DNA replication
↓ dose with pt hx of renal insufficiency
Ongoing neuro assessment
Supportive care—dim lights, limit noise, cluster care
Opioids ⚠—mask neuro symptoms!
Injury prevention & safety—monitor for sx & changes in LOC
Family support—help ease anxiety
Monitor blood chemistries & UOP—watching for renal complications r/t antiviral therapy
Creutzfeldt-Jakob disease (CJD) & Variant CJD
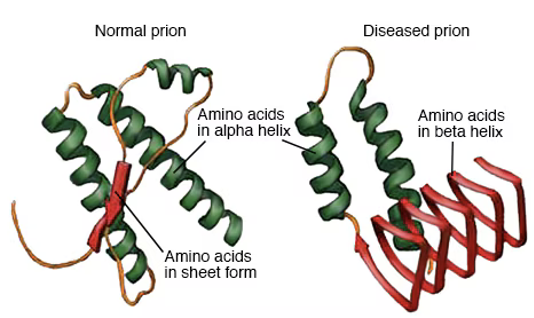
Rare, degenerative and fatal disorder caused by abnormal proteins (prions) resulting in rapid cognitive & neurological deterioration
Creutzfeldt-Jakob disease (CJD) & Variant CJD: Background
Transmissible spongiform encephalopathies (TSE): group of degenerative, infectious neurologic disorders
TSE = broader term for CJD, vCJD and other prion diseases
Rare with unknown cause
CJD: mostly sporadic; can be caused by mutation, hereditary, or iatrogenic
vCJD = human variant of bovine spongiform encephalopathy (BSE) (mad cow disease)
Result of ingesting prion-infested meat
Prions → TSEs
Shared characteristic of CJD & vCJD = lack of CNS inflammation
No definitive treatment
Fatal outcomes within 1 year of symptom onset
Mostly in UK; risk low in US:
Risk low in US d/t cattle fed mainly with soy-derived feed vs. animal-containing feed
Creutzfeldt-Jakob disease (CJD) & Variant CJD: Pathophysiology
Prions crosses BBB → deposits in & breaks down brain tissue → cell death → spongiform changes proliferation
Prions—in lymphoid tissue & blood:
American Red Cross & UK donations
Creutzfeldt-Jakob disease (CJD) & Variant CJD: Clinical Manifestations
CJD:
Mental deterioration, ataxia, visual disturbances
Memory loss, involuntary movement, paralysis, mutism
Late: psychiatric symptoms
Mean age of onset: 65 years
Survival after presentation: < 1 year
vCJD:
Early: Psychiatric symptoms
Behavior changes, sensory disturbances, limb pain
Muscle spasms & rigidity, dysarthria (difficulty speaking), incoordination, cognitive impairment & sleep disturbances
Mean age of onset: 27 years
Survival after presentation: ~14 months
Creutzfeldt-Jakob disease (CJD) & Variant CJD: Assessment + Diagnostics
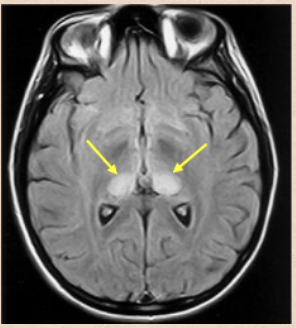
Immunologic assessment + EEG + MRI
Confirm by brain biopsy - NOT recommended
Post-mortem is preferred
Detection of protein kinase inhibitor (14-3-3)
EEG: starts with periodic activity; then periodic spikes alternating with slow periods
MRI: symmetric or unilateral hyperintense signals from basal ganglia
Creutzfeldt-Jakob disease (CJD) & Variant CJD: Management
No effective treatment for CJD & vCJD
Supportive & palliative:
Prevention r/t immobility & dementia, promotion of patient comfort, provision of support & education for family
Patient & family support:
Grief & loss
Hospice services – at home or inpatient
Transmission prevention:
Standard isolation precautions—no specific patient isolation
⚠ Handling of brain, spinal cord, pituitary gland and eye tissue
Careful handling of specimens
Disposable surgical instruments:
Sterilizations doesn’t kill prions
Bleach & extended sterilization time if not disposable
Autoimmune Nervous Disorders
Multiple Sclerosis
Myasthenia Gravis
Gullian-Barré Syndrome
Multiple Sclerosis
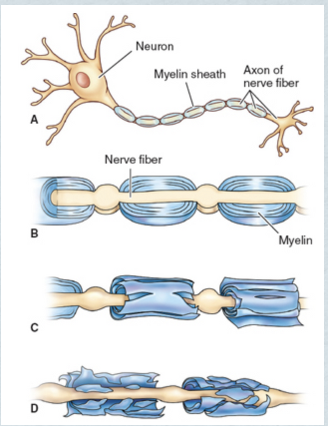
Immune-mediated, progressive demyelinating disease of the CNS
Multiple Sclerosis: Background
Demyelination = destruction of the fatty & protein material that encapsulates certain nerve fibers in brain and spinal cord ⟶ impaired transmission of nerve impulses
Affects 400,000 people in US
Can occur at any age:
Most common between age 20-50
More common in women > men
Cause unknown; ongoing research:
Autoimmune activity—demyelination but not clear about specific sensitized antigen
Environmental factors—obesity, ↓ Vit D exposure, high salt diet in teens
Geographical relationship:
More frequent in northern colder latitudes
↑ prevalence in Europe, New Zealand, southern Australia, northern US and southern Canada ---- less common in Asian populations
Genetic variations r/t MS—not necessarily hereditary – genetic variations
Infectious trigger
Other factors—physical injury, emotional stress, pregnancy, fatigue, overexertion, temperature extremes, hot shower/bath
4 main clinical forms:
Remitting-relapsing (RRMS):
Most common; patient reports development of new findings and function loss (relapse) --- symptoms mild to moderate & resolve within a few weeks to months (remission)
Secondary progressive (SPMS):
Starts as RRMS → continuously progressive
Primary progressive (PPMS):
MS with gradual & continuous reduction of CNS deterioration with remission
Progressive-relapsing (PRMS):
MS with frequent relapses with partial recovery w/o return to baseline
Multiple Sclerosis: Pathophysiology
Sensitized T & B lymphocytes cross BBB
↓
Sensitized T lymphocytes stay & promote infiltration of other agents
↓
Damage to immune system
↓
Inflammation
↓
Destruction of mostly white matter of CNS myelin & oligodendroglial cells; plaque formation
↓
Interrupted flow of nerve impulses
↓
Degeneration of axons
↓
Permanent & irreversible damage
Multiple Sclerosis: Clinical Manifestations
Dependent on area of CNS affected by demyelination
Fatigue—influenced by heat, depression, anemia, meds, etc
Weakness, numbness
Dysphagia
Difficulty in coordination, loss of balance
Spasticity
Pain: (lesions on sensory pathways)
Perimenopausal women: pain r/t osteoporosis—loss of estrogen, immobility and corticosteroids → osteoporosis
Bone mineral density testing recommended!
ALSO Pins & needles, abnormal sense of touch, proprioception loss
Visual disturbances
Cognitive & psychosocial difficulties:
Depression
Memory loss, emotional lability, ↓ concentration—Dementia in severe, rare cases
Ataxia, tremors
Bowel, bladder & sexual dysfunction
Exacerbations & remissions
Less severe forms:
RIS: no symptoms
CIS: uniliteral optic neuritis, focal symptoms or partial myelopathy
Main forms:
RRMS: complete recovery with each relapse but may occur over time → decline in function
Most RRMS cases → SPMS (can occur with or without relapses)
PPMS: disabling symptoms gradually increase + rare plateaus & temporary minor improvement
Quadriparesis, cognitive dysfunction, visual loss, brainstem syndromes
PRMS: relapses with continuous disabling progression b/t exacerbations
Multiple Sclerosis: Gerontologic Considerations
Life expectancy: 7-14 years shorter than average
Specific physical & psychosocial needs
Altered pharmakinetics due to age:
Monitor for adverse effects & toxicity
Might have chronic health problems + other medications that they’re taking → interactions
Osteoporosis ←→ corticosteroids
Cost of medications = chance for poor adherence, esp. for those on fixed income
Growing concerns:
Progressive disability
Family burden, marital concerns
Possibility of home nursing care
Immobility, physical challenges → loneliness & depression

Multiple Sclerosis: Assessment + Diagnostics
Based on clinical findings, imaging & lab findings
Neuropsychological testing—test for cognitive impairment
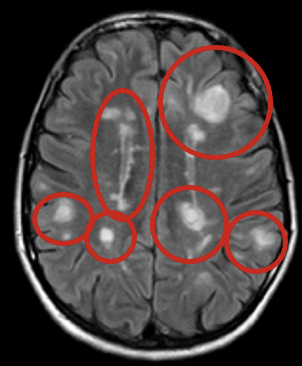
MRI: plaques in CNS distributed in different areas
LP/CSF analysis: presence of oligoclonal binding
Evoked potential studies—measure electrical activity in parts of CNS in response to stimuli
Urodynamics—– to diagnose underlying bladder dysfunction
Multiple Sclerosis: Management
Incurable
Goal: to delay progression of disease, manage chronic symptoms, treat acute exacerbations
Immunomodulators
Interferon beta-1a & interferon beta-1b
Glatiramer acetate
Teriflunomide, fingolimod, dimethyl furmarate
IV methylprednisolone
IV Mitoxantrone
Symptom management:
Treat spasticity: antrolene, baclofen, diazapam
Paresthesia: carbamazepine
Treat constipation: docusate sodium
Manage bladder dysfunction: anticholinergics
Ataxia: propranolol, clonazepam
Treat fatigue: amantadine, pemoline, dalfampridine, baclofen, tizanidine
Multiple Sclerosis: Nursing Interventions
Assess for changes in visual acuity, activity tolerance level, skin integrity, speech & swallowing abilities
Look out for cognitive changes
Monitor I&Os & encourage fluid intake
Promote physical mobility & independence when possible
Exercise, stretching, ROM exercises
Energy conservation—avoid overexertion
Reduce risk for injury
Coping strategies—stress management
Alternative therapies: yoga, meditation, aromatherapy, acupuncture, massage
Monitoring & managing complications
UTIs, constipation, pneumonia
Medication education
Outpatient management:
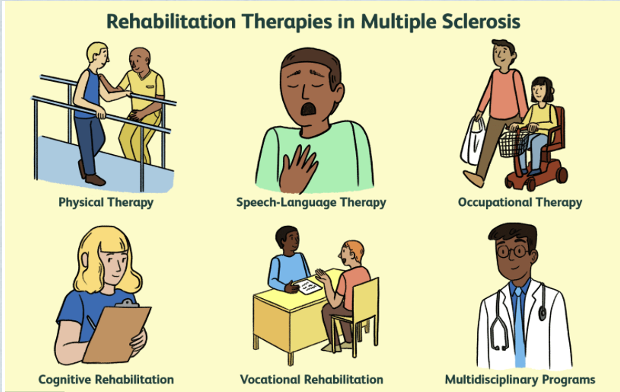
Interprofessional team: neurology, ophthalmology, physical therapy, OT, mental health provider, case management, social work
Myasthenia Gravis
Autoimmune disorder that affects myoneural junction
Myasthenia Gravis: Background
Characterized by varying degrees of weakness in voluntary muscles
Relatively uncommon but affects 9-30 in 1 million in US
More prevalent in women in 20-30s
But more common in men after age 50
Myasthenia Gravis: Pathophysiology
Antibodies targeting acetylcholine receptors
↓
Impaired impulse transmission
↓
Less receptors available for stimulation
↓
Voluntary muscle weakness that gets worse with ongoing activity
_____
**Normal: chemical impulse → release of acetylcholine from vesicles on nerve terminal myoneural junction → ACh attaches to receptor site on the motor endplate → muscle contraction
**Continuous binding of ACh receptor site REQUIRED for muscle contraction to be sustained
Myasthenia Gravis: Clinical Manifestations
Highly variable
Types: Ocular & Clinical
Diplopia
Ptosis—drooping of eyelids
Muscle weakness:
Face & throat (bulbar symptoms)
Respiratory
Dysphonia (voice impairment) & Dysphagia
Respiratory failure = myasthenic crisis
Myasthenia Gravis: Assessment + Diagnostics
Acetylcholinesterase inhibitor test:
Administer edrophonium chloride IV & give 30 sec → facial muscle weakness & ptosis resolved for 5 min.
Atropine for possible side effects—to control bradycardia, asystole, bronchoconstriction, sweating, cramping
Ice test:
Ice pack over eyes x 1 minute to temporarily resolve ptosis
Antibody testing—Multiple blood tests
Repetitive nerve stimulation (RNS)—↓ successive action potentials
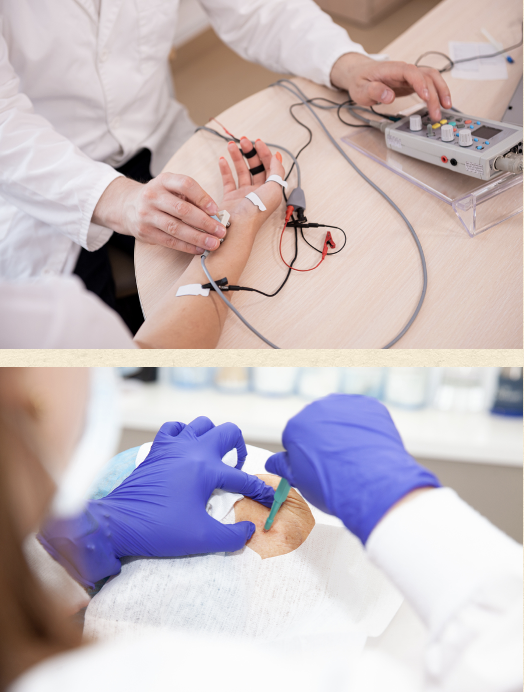
Single-fiber electromyography (EMG)—picks up on delay or failure of neuromuscular transmission; has 99% sensitivity
Enlarged thymus gland - can be identified with MRI:
thymus = site of acetylcholine receptor antibody production
Myasthenia Gravis: Management
Goal: To improve function & to reduce and remove circulating antibodies
Pyridostigmine bromide - 1st line of therapy**
PB = anticholinesterase —inhibits breakdown of neuromuscular junction → muscle strength & control fatigue
Dose gradually increase to a daily max, then given in divided doses (~4 x day)
Side effects: diarrhea, abdominal cramps, and/or excessive saliva
PB has fewer side effects than other anticholesterase meds
Immunosuppressive therapy:
Corticosteroids (Prednisone)
Cytotoxic meds (azathioprine)
Adverse Effects: leukopenia & hepatotoxicity → monthly liver enzymes & WBC checks
IVIG—for exacerbation but sometimes long-term basis (monthly infusions)
Pooled human gamma-globulin – lasts for ~4 weeks
Complications: headache, flu-like symptoms, aseptic meningitis
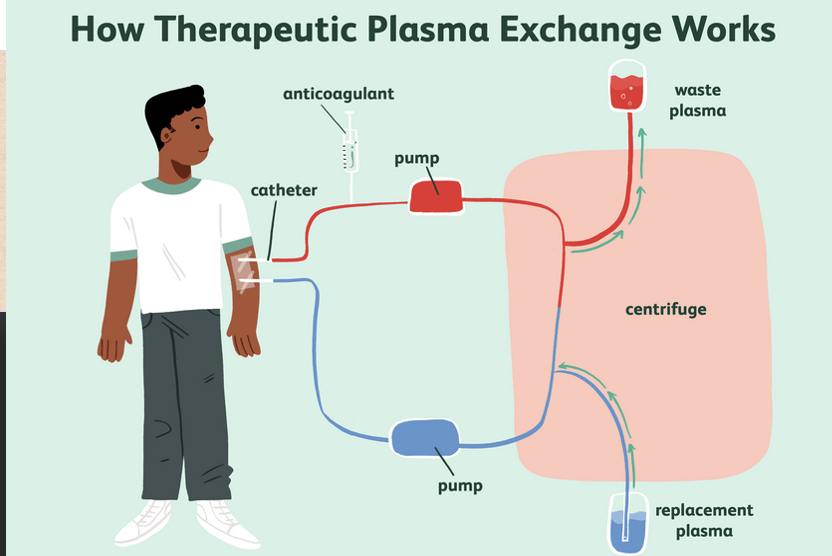
Plasmapheresis—(therapeutic plasma exchange)—helps treat exacerbation
Plasma & plasma contents removed through CVL, large-bore double lumen
Blood cells & antibody-containing plasma separated à cells and plasma substitute reinfused
Temporary reduction in antibodies in blood
Daily or alternating days
Thymectomy—removal of thymus gland (produces antigen-specific immunosuppression)
Only treatment for complete remission (only 35%)
Best for those under age 60 with a diagnosis of MG for 3 years
Plasmapheresis or pre-op IVIG → less time on the vent
~3 years post op to see benefit (circulating T cells have long life)
Myasthenia Gravis: Nursing Interventions
Education on outpatient self-care:
Energy conservation
Strategies for life with visual impairment
Prevention & management of complications:
Triggers
Medication management—lots of meds might be contraindicated for MG & could exacerbate symptoms
Procaine—should be avoided, notify dentist of diagnosis
Risk of choking & aspiration
Psychosocial support
Myasthenic Crisis
Exacerbation of disease characterized by severe generalized muscle weakness, respiratory and bulbar weakness → respiratory failure
Inadequate cough, impaired gag reflex → ineffective airway clearance
Most common trigger: respiratory infection
Worsening pulmonary function test—– 1st clinical sign of declining resp function
Negative inspiratory force & vital capacity
Respiratory support:
Intubation & mechanical ventilation
Noninvasive positive pressure ventilation (BiPAP, CPAP)
Chest physiotherapy
ABGs, serum electrolytes, I&Os, daily weights
Enteral feeds—if risk for aspiration
Temporarily stop cholinesterase inhibitors:
Cholinergic crisis = due to overmedication with cholinesterase inhibitors (rare)
Reason for temporarily stopping during myasthenic crisis – it could mimic or worsen the symptoms
Also results in resp. failure due to weakness of respiratory muscle & bulbar weakness
Gullian-Barré Syndrome
Autoimmune attack on the peripheral nerve myelin
Gullian-Barré Syndrome: Background
Acute idiopathic neuritis
Leads to acute, rapid sections of demyelinated peripheral nerves & some cranial nerves → ascending weakness with dyskinesia (inability to execute voluntary movements), hyporeflexia & paresthesias (sensation of numbness & tingling; “pins and needles”)
Usually preceded by a viral infection:
*Campylobacter jejuni
Cytomegalovirus
Epstein-Barr virus
Mycoplasma pneumoniae
H. influenzae
Zika virus
Several subtypes
1-2 per 100,000 people affected annually;
5-10% result in death from resp. failure, autonomic dysfunction, sepsis or pulmonary embolism
70% fully recover, remainder left with varied disability
Gullian-Barré Syndrome: Pathophysiology
Infectious organism has an amino acid that imitates that of peripheral nerve myelin protein
↓
Immune system can’t distinguish between the two; attacks & destroys peripheral myelin at GM1b
↓
↑ in macrophages & other immune-mediated agents to attack myelin
↓
Inflammation & destruction, interrupted nerve conduction & axonal loss
Gullian-Barré Syndrome: Clinical Manifestations
Symptoms typically show up 1-3 after preceding event
Typically beginning with leg weakness → progressing upward to neuromuscular resp. failure & bulbar weakness
Reaches peak around 2 weeks but doesn’t last longer 4 weeks
> 4 weeks = chronic inflammatory demyelinating polyneuropathy
__________________
Bilateral muscle weakness, hyporeflexia in lower extremities:
Could become tetraplegia
Bulbar weakness
Paresthesias of hands & feet
Pain
Blindness
Difficulty swallowing or clearing secretions
Autonomic dysfunction—tachy, brady, hypertension, hypotension --- resolve quickly!
Neuromuscular respiratory failure
***Does NOT affect cognition or level of consciousness
Gullian-Barré Syndrome: Assessment + Diagnostics
Health history, physical exam (if any recent viral illness)
Negative inspiratory force, vital capacity
Electrophysiology studies—measure nerve conduction velocity which can tell how much the disease has affected nerve conduction
Gullian-Barré Syndrome: Management
Medical Emergency!
Plasmapheresis (therapeutic plasma exchange)
IVIG
May require mechanical ventilation
IV fluids
Alpha-adrenergic blocking agents
Gullian-Barré Syndrome: Nursing Interventions
Monitor need for intubation - signs of respiratory failure
Suctioning as needed
Monitoring for autonomic dysfunction - ECG monitoring
Prevent complications from immobility:
Position changes, anticoagulants, SCDs, range-of-motion exercises
Administer IV fluids or parenteral nutrition
Reduce fatigue & maintaining independence
Rehabilitation
Psychological support to patient & family:
Identify support needs in preparation for discharge
Degenerative Disorders
Muscular Dystrophies
Huntington’s Disease
Amyotrophic Lateral Sclerosis
Degenerative Disc Disease
Muscular Dystrophies
Group of incurable muscle disorders marked by progressive weakening & wasting of skeletal or voluntary muscles

Muscular Dystrophies: Background
30 different types, mostly inherited:
Differentiated based on genetic pattern of inheritance, muscles involved, age at onset, rate of disease progression
Most common: Duchenne muscular dystrophy
Pathogenic features:
Degeneration & loss of muscle fibers
Variation in muscle fiber size
Phagocytosis and regeneration
Replacement of muscle wasting by connective tissue
Prognosis depends on type of dystrophy:
Unique needs for newly aging population
Muscular Dystrophies: Clinical Manifestations
Varying degrees of muscle weakness & wasting
Abnormal elevation of serum levels of muscle enzymes
Decreased respiratory reserve
Cardiomyopathy
Muscular Dystrophies: Management
Supportive care—to promote activity and optimal normal function & keeping functional deterioration at a minimum
Prevention of complications
Therapeutic exercise programs—–prevents muscle tightness, contractures, disuse atrophy
Night splints, stretching exercises—delays development of contractures of joints (ankles, knees & hips)
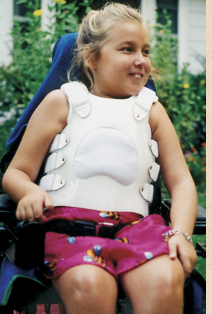
Braces—support body to compensate for weakness of muscles
Spinal deformity: muscle weakness & spinal collapse
Orthotic vest (to prevent)—improves stability when sitting and supports CV status
Spinal fusion, eventually
Pulmonary function—d/t disease progression or deformity of thorax secondary to severe scoliosis
URIs & fractures from falls – addressed promptly to avoid immobilization since contractures are a lot worse with inactivity
Other difficulties:
Dental hygiene
Speech & swallowing problems
GI issues—gastric dilation, rectal prolapse, fecal impaction
Cardiomyopathy
Genetic counseling—encouraged for parents & siblings of patients d/t strong genetic component
Muscular Dystrophies: Nursing Interventions
Goal: to maintain function at optimal levels & improve quality of life
Maintain home care routine when able
Consider your patient’s insight and knowledge when making decisions – they, along with family, know what strategies have worked for them to function at home
Try to promote home care routine during hospitalization as much as possible
Important component of caring for patient with chronic issues – helps them maintain some sense of normalcy
Transition from pediatric care to adult care (newly aging population – helping with transition into adulthood)
Promote independence as much as possible safely
Disease progression education
Rehabilitation programs
Range-of-motion exercises
Patient & family support:
End-of-life decisions
Mental health
Huntington’s Disease
Chronic, progressive herditary disease of nervous system that causes progressive involuntary choreiform movement & dementia
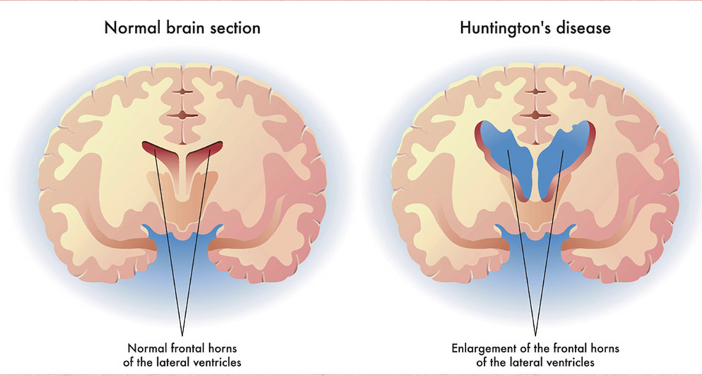
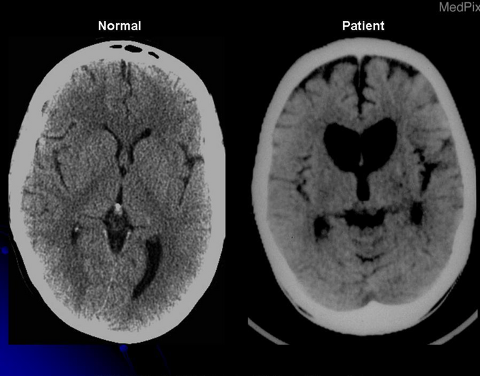
Huntington’s Disease: Etiology + Pathophysiology
Premature death of cells in:
Striatum of basal ganglia (involved in movement control) + Cortex (involved with thinking, memory, perception, judgment & behavior) + Cerebellum (voluntary muscle activity coordination)
Cause not known but possibly due to glutamine collecting in cell nucleus abnormally → cell death
Hereditary; passed on by autosomal dominant gene:
Each child of parent with disease have 50% chance of inheriting
Genetic testing:
Identify gene presence but not timing of onset
Everyone has the gene for Huntington Disease BUT the people with the expansion of the gene can develop the disease and pass it on
Affects 1 in 10,000 men and women at midlife—rare
Choreiform movements even when asleep
Huntington’s Disease: Clinical Manifestations
Characteristic triad:
*Motor dysfunction: (chorea - rapid, jerky, involuntary, purposeless movements); facial tics & grimaces
*Cognitive impairment: difficulties with attention & emotion recognition
*Behavioral features: apathy, blunted affect
Constant writing, twisting, uncontrollable movements of whole body (choreiform movements)
Disorganized gait
Other clinical manifestations: difficulties with chewing & swallowing, bladder & bowel incontinence
Huntington’s Disease: Assessment + Diagnostics
Clinical presentation of characteristic symptoms
Positive family history
Known presence of genetic marker cytosine-adenine-guanine (CAG) repeating on Huntington gene (HTT)
CT/MRI: symmetrical striatal atrophy prior to motor symptoms developing
Huntington’s Disease: Management
No curative or reversing treatment
Multidisciplinary: social work, occupational therapy, speech, physical therapy, palliative care
Goal: To optimize quality of life with supportive treatment
Ongoing assessment of motor signs to evaluate drug efficacy:
Akathisia (motor restlessness) with overmedication = DANGEROUS
Can be seen as restless fidgeting of illness & could be overlooked
Hypokinetic motor impairment -- resembles Parkinson's
Misleading symptoms
Tetrabenazine—manage chorea
Benzodiazepines & neuroleptic drugs
Antiparkinson (Levodopa)—manage rigidity sometimes
SSRIs, tricyclic antidepressants—psychiatric symptoms
Huntington’s Disease: Transitional Care
Coping with progression
Supportive care
Follow-up visits
Home care, day care centers
Respite care, skilled long-term care
End-of-life care planning

Amyotrophic Lateral Sclerosis
Loss of motor neurons in anterior horns of spinal cord & motor nuclei of lower brainstem
Amyotrophic Lateral Sclerosis: Etiology + Pathophysiology
Also known as Lou Gehrig disease
Cellular death of motor neurons → progressive weakness & atrophy of muscle fibers in extremities
Cause unknown:
Thought to be d/t overexcitation of nerve cells by glutamate → cell injury & neuronal degeneration
Risk factors: age, autoimmune diseases, environmental exposure to toxins, family hx, smoking, viral infections
Onset age: 40-60 years old
Affects men a little more often than women
10% of cases are familial; onset occurs 10 years earlier than average
Clinical presentation & prognosis dependent on area of CNS involved & speed of disease progression
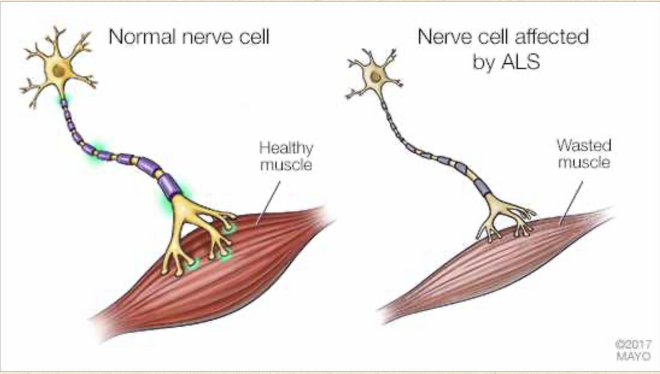
Amyotrophic Lateral Sclerosis: Clinical Manifestations
Fatigue
Progressive muscle weakness, cramps, twitching
Lack of coordination
Spasticity
Overactive deep tendon reflexes
Emotional lability, cognitive impairment
Soft palate & upper esophagus weakness → Difficulty with liquids
Posterior tongue & palate weakness → inability to laugh, cough, or blow nose
Bladder & anal sphincter intact d/t spinal nerves not affecting rectum & bladder
Death—usually from infection, respiratory insufficiency, or aspiration
Difficulty speaking, swallowing & eventually breathing
Amyotrophic Lateral Sclerosis: Assessment + Diagnostics
No ALS specific testing
Electromyography (EMG)
Muscle biopsy studies of affected muscles
MRI
Neuropsychological testing
**EMG & muscle biopsy studies of affected muscles - reduction in number of functioning motor units
**MRI - high signal intensity of corticospinal tracts
Amyotrophic Lateral Sclerosis: Management
No cure
Maintain or improve function, well-being, & quality of life
Riluzole & edaravone = ALS treatments but unsure how it works
Symptom management:
Baclofen, dantrolene sodium, diazepam (all—painful spasticity)
Modafinil—fatigue
Medications for pain, drooling, constipation
Depression & functional impairment
Rehabilitative measures
Clinical trials:
ALS registry
Life at home:
Hospitalizations
End-of-life issues
Mechanical ventilation:
Non-invasive positive pressure ventilation (NPPV)
Tracheotomy
PEG tube

Degenerative Disc Disease
Disorder that results from the breakdown of intervertebral discs in spine due to aging or injury, causing pain, stiffening or decreased mobility
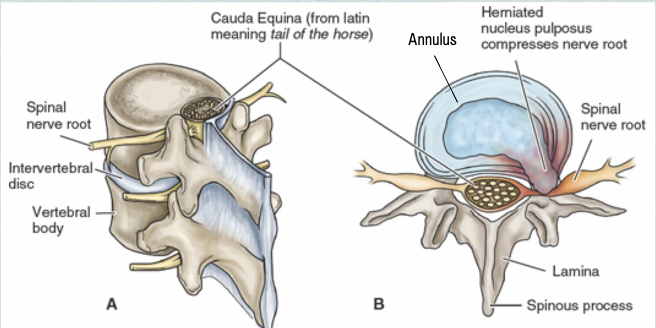
Degenerative Disc Disease: Background
Low back pain—2nd most common neurological disorder:
Migraines = most common
Most common reason for missed work & ↓ productivity
Commonly associated with depression, anxiety, smoking, alcohol abuse, obesity, stress
Most recover within 4-6 weeks
Acute pain < 3 months; chronic pain is > 3 months