Week 7 Tissue: Mechanics of Bone
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
45 Terms
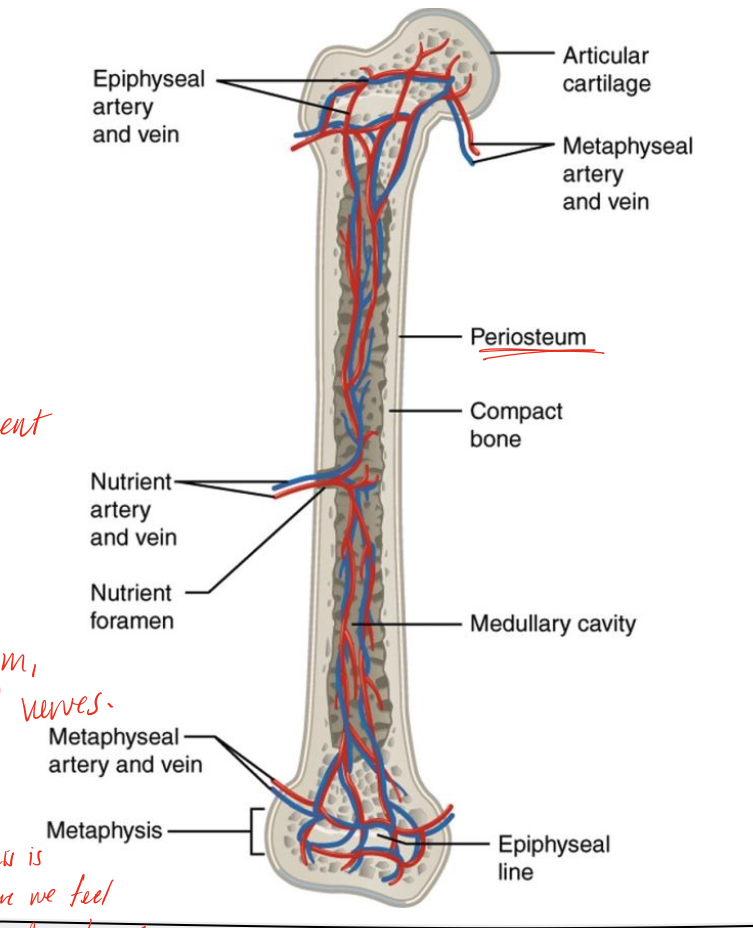
diaphysis
long shaft of bone
epiphysis
ends of bone
epiphyseal line/plate
growth plate, seals in females in teens, for males in mid 20s, a weak spot
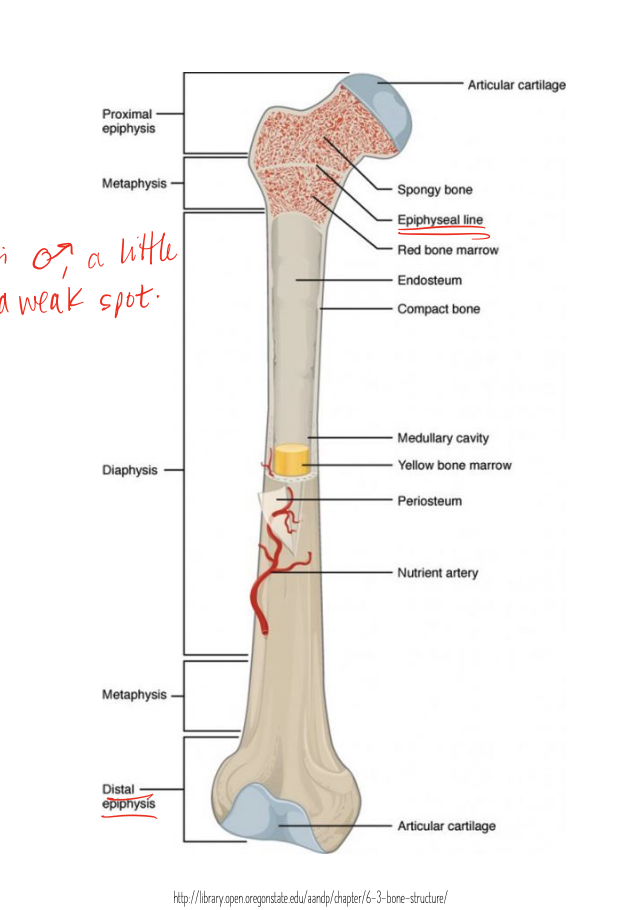
metaphysis
between the epiphysis and diaphysis
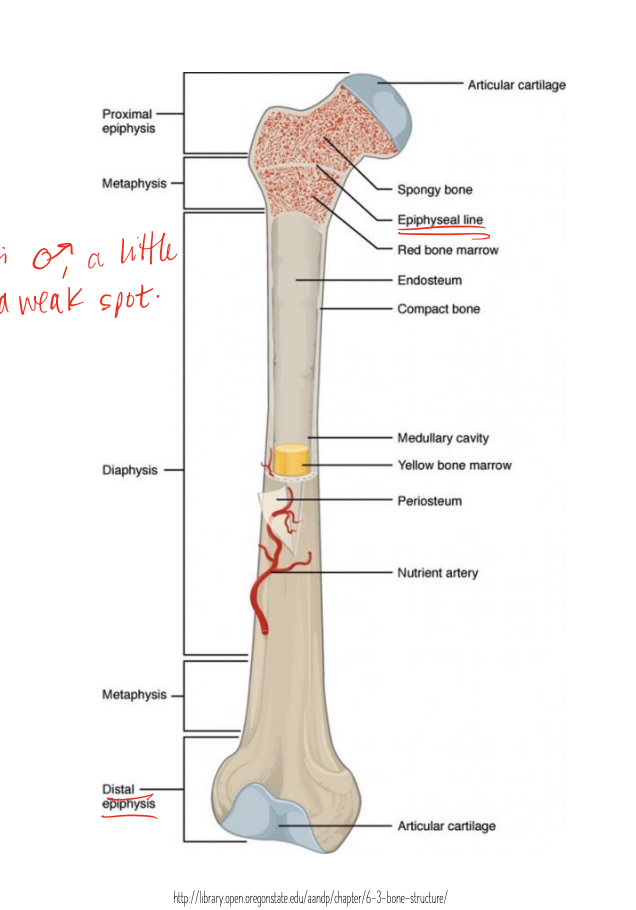
articular cartilage
covers the epiphysis on ends of the bone
periosteum
sheath-like bone covering attached by Sharpey’s fibers and contains nociceptors (pain)
medullary cavity
hollow chamber in bone, red marrow produces blood cells, yellow marrow is adipose
endosteum
thin layer lining the medullary cavity, important for blood transfer back and forth
cortical bone
aka compact, hard and dense, for protection adn stretgth, withstand force, example is mid femoral shaft
cancellous bone
spongy and trabecular, less dense with series of holes, femoral head is example, absorb force from different locations in femoral head
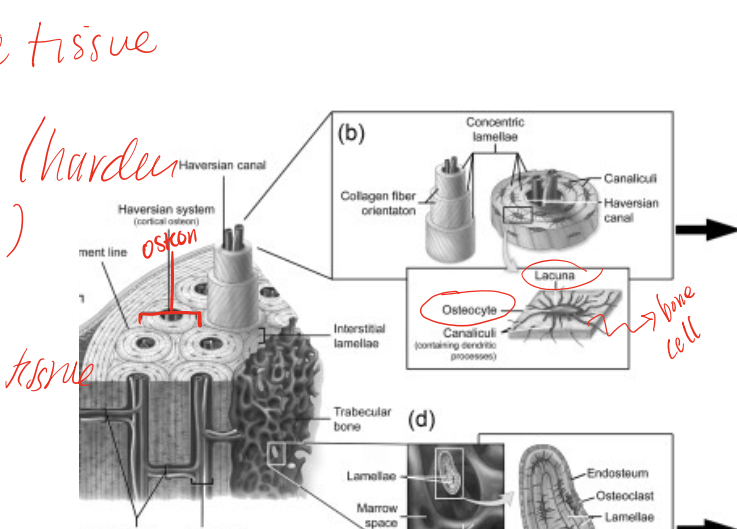
bone
specialized connective tissue, features osteon (haversian system) that secretes collagen and mineralized ground substance in concentric spirals, good blood supply that enables repair and remodeling
osteon
aka haversian system, subunit of bone that secretes collagen and mineralized ground substance in concentric spirals known as lamellae
blood supply of bones
nutrient arteries, periosteal arteries, epiphysial arteries, and metaphysial arteries
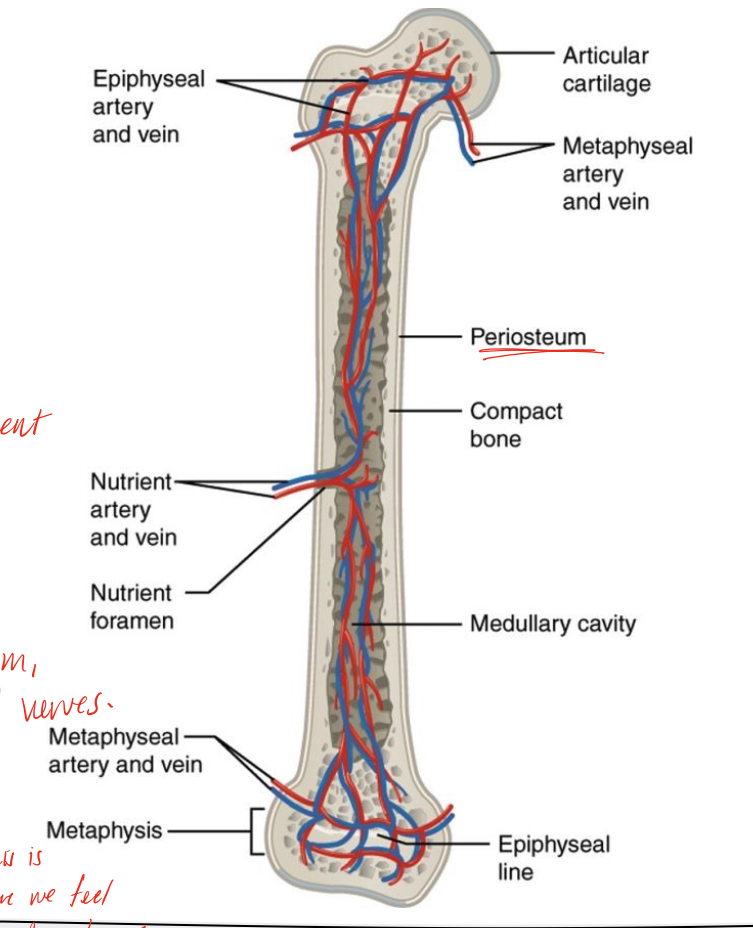
nerve supply of bones
run with the arteries and innervate bone, peristeal nerve is superficial on the periosteum, vaso-motor nerves go into the bones, not sensory
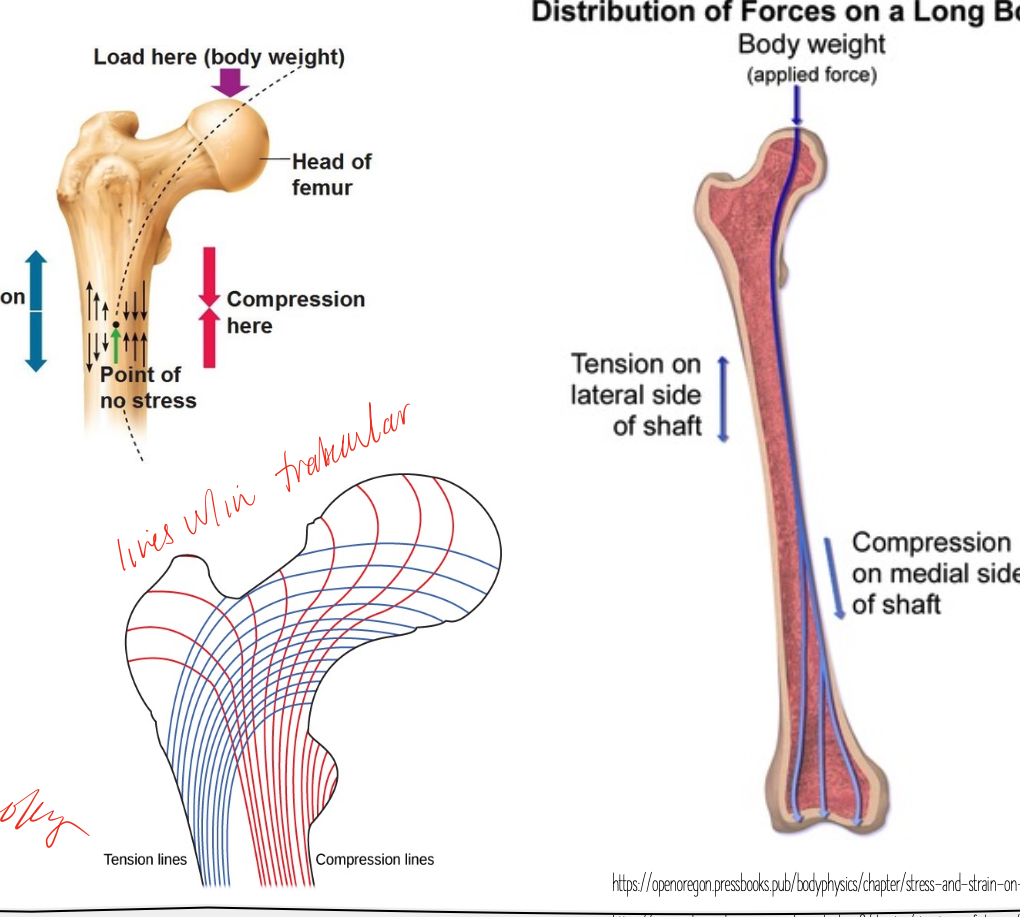
wolfe’s law (mechanotransduction)
physical characteristics of bone are based on what we do with them! bone is laid down in areas of high stress and reabsorbed in areas of low stress, mechanical properties vary and be based on function and structure, shows us the importance of loading the bone after injury to heal correctly (rehab implication)
structures of bones
hollow tube to resist compression, flat bone to serve at attachment point or protection
force distribution on the bone
can vary with the lines of force that act upon it, ie can be stiff in one direction and more flexible in others, cortical bone haversian systems align along lines of force, and similarly trabeculae align along lines of force
ultimate stress that cortical bone can withstand
compressive stress: 200 MPa
Tensile stress 125 MPa
Shear stress 50-75 MPa
ultimate stress that trabecular bone can withstand
compression 2.6 MPa
Tension 2.4 MPa
force bone is better at resisting
better at resisting compression than tension (and it’s brittle)
interpretation of the stress strain curves (young’s modulus is the slope)
the steeper the line, the stiffer the tissue, flatter line means more elastic
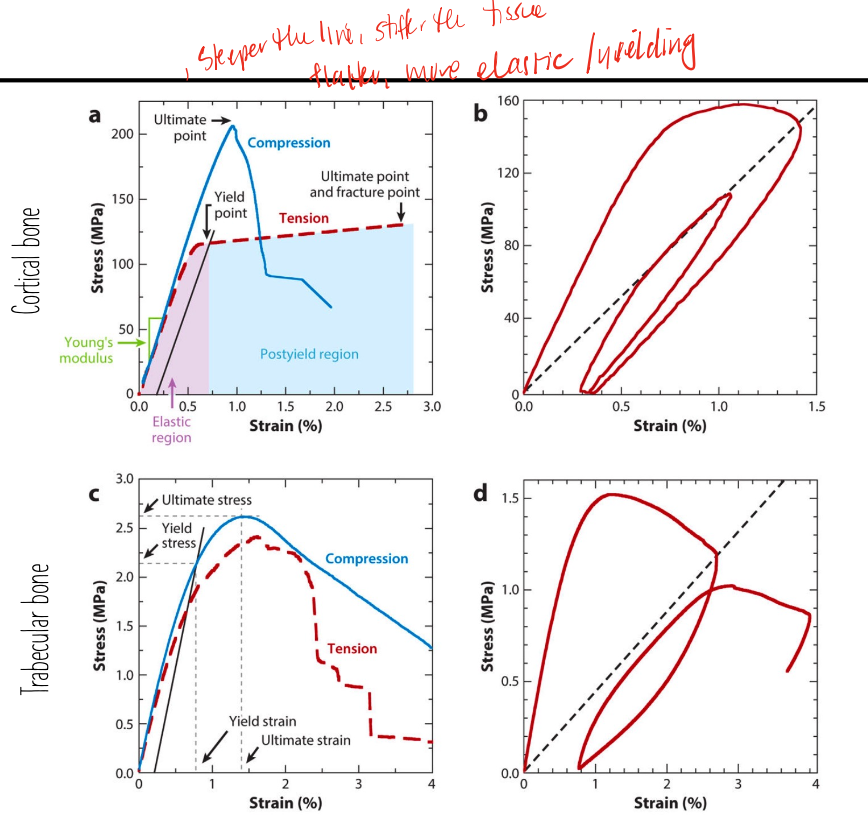
fracture toughness
measure of a bone’s ability to resist crack growth if a crack has been initiatied, rang efrom 3.3-6.4 MPa/m², low value indicated boen is brittle (like ceramics)
ductile
what a high fracture toughness would tell us about th ematerial, resists fracture well
bone will fail before metal
implications for metal implants in bone since metal is much more ductile
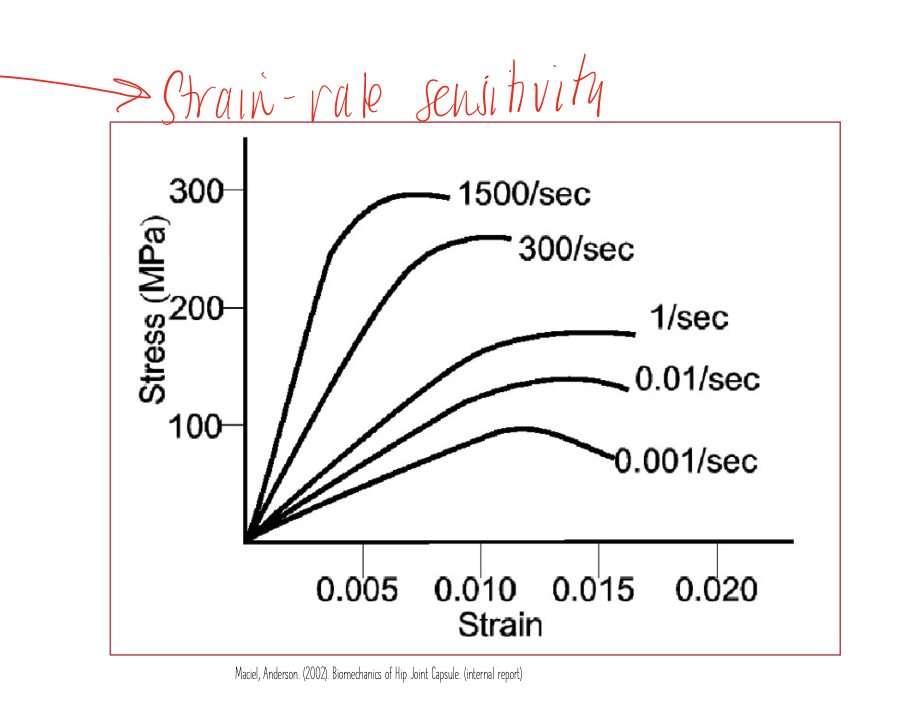
bone strain rate
stiffness increases with increase speed of loading, allows body to be protective against trauma, falls, jumps, etc
bone changes with activity and inactivity
increasing loading/activity- denser bone
decrease loading/activity- thinner bone, less remodeling
activities for increasing bone density (least to most)
swim, cycle
brisk walk
run, jog
jump, strength train
bone changes with age
decreased stiffness, fracture toughness, ultimate strength
due to changes in mineral composition, inactivity, and other things maybe
can lead to osteopenia and eventually osteoporosis
factors contributing to osteopenia
activity, level, hormonal changes, diet
osteopenia
precursor to osteoporosis, starting to lose bone density, can avoid progression if make the right changes
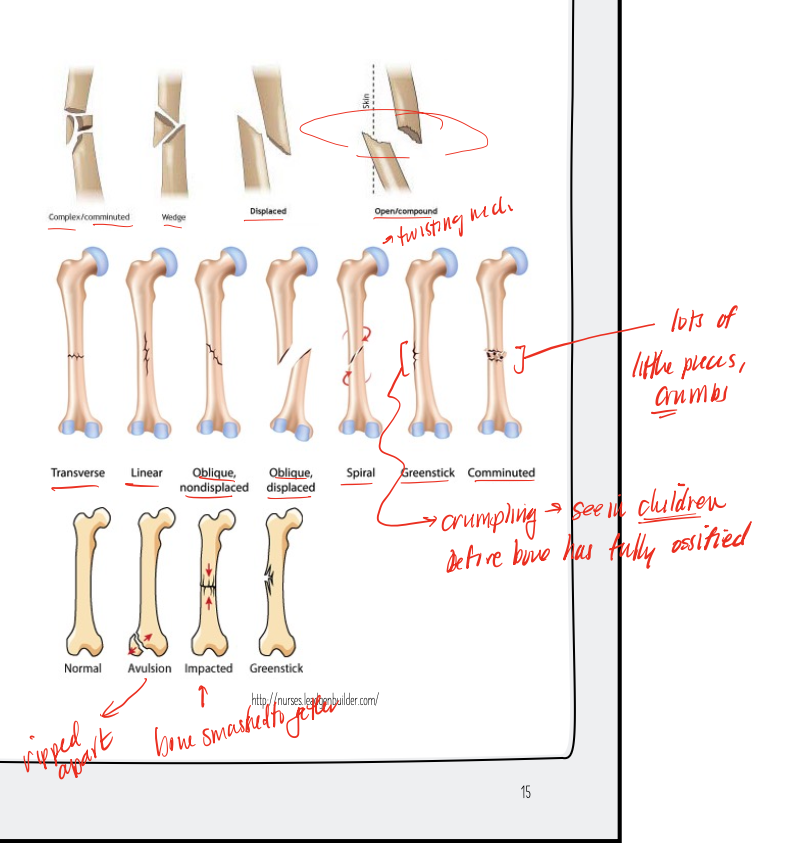
factors that bone fractures are classified by
position of the bone ends after fracture
completeness of the break
the orientation of the bone to the long axis
whether or not the bone ends penetrate the skin
types of bone fractures
transverse, linear, oblique, spiral, greenstick, comminuted, avulsion, impacted, open/compound
bone healing requirements
viable fragments with intact blood supply
mechanical rest (external mobilization like cast)
absence of infection
factors that promote recovery
stop smoking, don’t drink too much
balanced diet with sufficient calcium
adhere to activity restrictions
maintain strength and ROM of other joints and body regions
maintain fitness level with modified activity
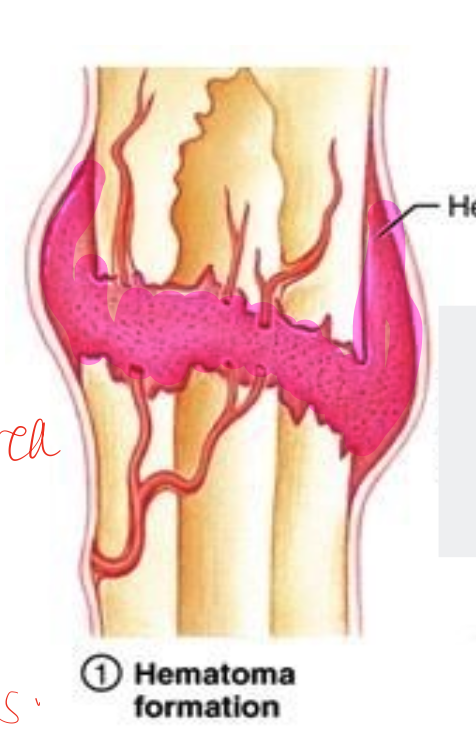
bone healing- inflammatory phase
first few days to week
local cell death due to ischemia
local swelling and warmth
inflammatory cells invade and release lysosomal enxymes
osteoblastic/osteoclastic activity is stimulated
hematoma develops
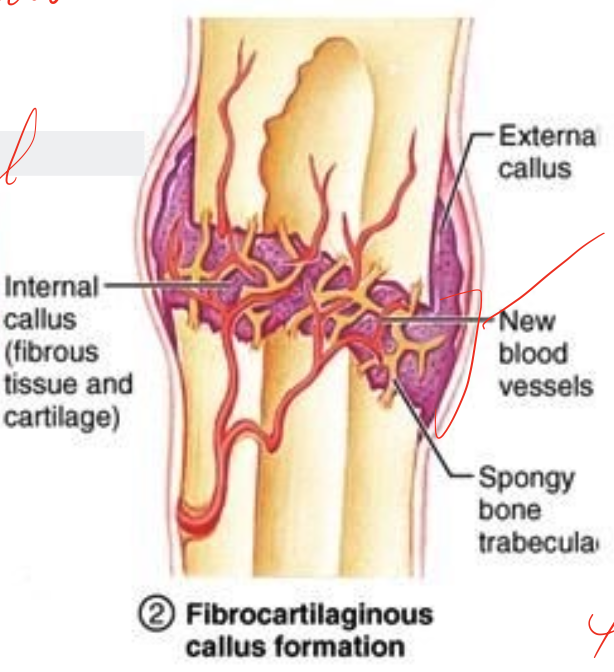
bone healing- early reparative phase
2-6 weeks
resorption of necrotic bone
characterized by differentiation of cells
fracture hematoma (invaded by chondroblasts and fibroblasts which lay down the matrix for the callus)
early soft callus composed of mainly fibrous tissue and cartilage with a very small amount of bone
increased vascularity
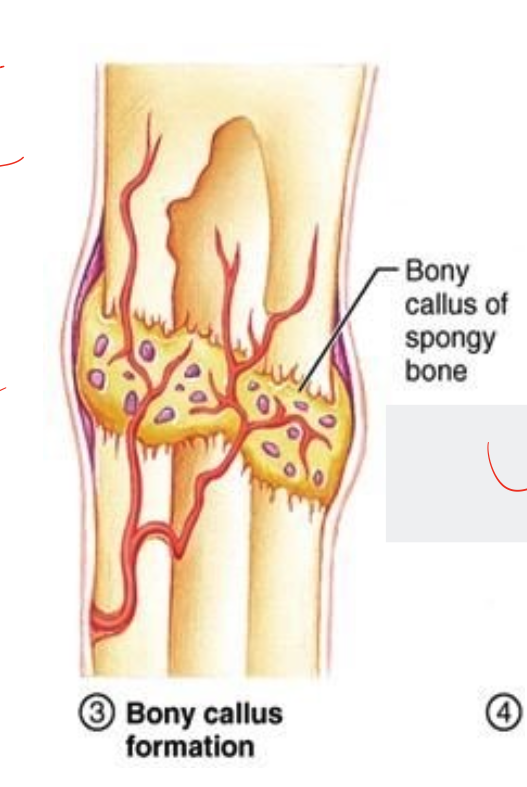
bone healing- Late reparative phase
8-12 weeks
osteoblasts minerlize the soft callus and from a hard callus of woven bone, increases stability
still immature and weak, bridging of the fracture
clinical and radiological healing during this phase
phase is complete when fracture is stable
bone healing- remodeling phase
months to years
bone is removed in tiny increments and then replaced by new bone
osteoblastic and osteoclastic activity
immature bone replaces bu mature bone
stability increases
adult skeleton continuously replaces itself at rate of 10- 18% per year (accelerated during fracture repair)
responds to loading characteristics according to wolfe’s law
factors that affect bone healing
severity of fracture
location of fracture
type of bone involved
soft tissue damage
type of fixation
extent of overall trauma
age
co-morbitities
etc
general timeline of bone healing for children
4-6 weeks (though depends on location and other factors)
general timeline of bone healing for adolescent
6-8 weeks (though depends on location and other factors)
general timeline of bone healing for adults
10-18 weeks (though depends on location and other factors)
bone implications for practice
goal during immobilization-
preserve function with ADs, slings, modifiications of activities, compensatory mechanisms for function
maintain strength and ROM of surrounding joints with home exercise program
goal after cast removal is to return to previous function
address factors that may have predisposed to injury
things to do after cast removal
strengthening and ROM
scar mobilization
functional training
education of timeline and return to prior functional level
home exercise program
percentage decrease of bone measures per 10 years after about 30 yo